Abstract
Objectives
To evaluate the incidence of snow-sports-related head injuries among children and adolescents reported to emergency departments (EDs), and to examine the trend from 1996 to 2010 in ED visits for snow-sports-related traumatic brain injury (TBI) among children and adolescents.
Methods
A retrospective, population-based cohort study was conducted using data from the National Electronic Injury Surveillance System for patients (aged ≤17 years) treated in EDs in the USA from 1996 to 2010, for TBIs associated with snow sports (defined as skiing or snowboarding). National estimates of snow sports participation were obtained from the National Ski Area Association and utilised to calculate incidence rates. Analyses were conducted separately for children (aged 4–12 years) and adolescents (aged 13–17 years).
Results
An estimated number of 78 538 (95% CI 66 350 to 90 727) snow sports-related head injuries among children and adolescents were treated in EDs during the 14-year study period. Among these, 77.2% were TBIs (intracranial injury, concussion or fracture). The annual average incidence rate of TBI was 2.24 per 10 000 resort visits for children compared with 3.13 per 10 000 visits for adolescents. The incidence of TBI increased from 1996 to 2010 among adolescents (p<0.003).
Conclusions
Given the increasing incidence of TBI among adolescents and the increased recognition of the importance of concussions, greater awareness efforts may be needed to ensure safety, especially helmet use, as youth engage in snow sports.
INTRODUCTION
In recent years, an increased focus on sports-related concussions among children and adolescents has driven legislative policies (such as the Zackery Lystedt law in Washington State) and generated position statements from youth sports organisations and paediatric societies.1,2 These efforts are fuelled by data showing an increasing incidence of reported sports-related and recreation-related traumatic brain injury (TBI) among young athletes in the last decade3,4 and research revealing the potential for substantial long-term sequelae of TBI.5-7 Among children and adolescents, even mild TBI, which does not present with operative lesions or abnormalities on routine imaging scans, can be associated with a range of negative consequences, including headaches, depression, memory problems and poor school performance.8-11 Mild TBI is also associated with increased healthcare costs in the years following injury.12
Head injuries constitute 16%–27% of injuries among children and adolescents engaged in snow sports (alpine skiing and snowboarding).13,14 Over half of these injuries may be classified as TBIs, including concussions, cerebral contusions and intracranial haemorrhages.14 Numerous regional and single-resort studies have described helmet use and its effectiveness in preventing snow-sports-related head injuries;15-20 however, little is known about the overall trend in these injuries. This study was conducted to evaluate the rates of snow-sports-related TBI among children and adolescents reporting to emergency departments (EDs) in the USA, and to examine the trend in ED visits for snow-sports-related TBIs among children and adolescents from 1996 to 2010.
METHODS
Data sources
Study data were obtained from several sources. The US Consumer Product Safety Commission (CPSC) maintains the National Electronic Injury Surveillance System (NEISS), which collects information on consumer-product-related injuries treated in the EDs of a probability sample of 100 US hospitals. The NEISS has been used previously to investigate head injuries in children and adolescents.3,4 Injury information includes age, sex, site of injury, body part, diagnosis, discharge disposition, consumer product(s) associated with injury and a 160-character narrative with additional detail on the injury and circumstances of its occurrence. Diagnosis codes are limited to the ‘most severe and specific diagnosis’, given by the attending physician. Helmet use was not consistently reported in narratives and therefore not used in this analysis. Patient outcomes other than ED disposition were not available.
Yearly estimates of snow sports participation were obtained from the annual National Ski Area Association (NSAA), Kottke National End of Season and Demographic Surveys. The Kottke Survey compiles information from US ski resorts to estimate the total number of youth skier and snow-boarder visits for the winter seasons of 1996–1997 through 2009–2010. For the purposes of this study, a ‘resort visit’ is defined as a one-day athletic exposure to downhill skiing or snowboarding within a resort. The Kottke Survey categorises young snow sports participants into two age groups: children (4–12 years old) and adolescents (13–17 years old).
Subjects
Study subjects included patients under 18 years old with head injuries reported in the NEISS database between 1996 and 2010, which involved activity, apparel or equipment associated with snow skiing (product code 3283) or snowboarding (product code 5031). Ski-related and snowboard-related injuries were combined to represent ‘snow-sports-related injuries’ because the data on snow sports participation are not available separately for skiing and snowboarding. Records were included for all head injuries (body part code 75), which were subcategorised as either ‘TBI’ or ‘other head injury’ based on the diagnosis codes.21 ‘TBI’ was assigned to subjects with intracranial injury (internal organ injury: diagnosis code 62) or concussion (diagnosis code 52), consistent with previous research.2 A study that used the Centers for Disease Control and Prevention standard definition of mild TBI to evaluate case ascertainment in the NEISS found that inclusion of skull fractures identified additional TBI cases.21 Therefore, our definition of ‘TBI’ also included skull fractures (diagnosis code 57). All other head injuries, including scalp lacerations and contusions, were categorised as ‘other head injury’. Narratives with missing diagnosis were reviewed by investigators (JMG, FPR) and assigned an injury category if possible. Narratives for subjects with haematoma (diagnosis code 58) or haemorrhage (diagnosis code 66) diagnoses were also reviewed to determine the eligibility for inclusion in the TBI group. Fatalities were excluded because the NEISS is not representative for deaths.
Two researchers (JMW, JOS) independently reviewed the narratives to identify ineligible cases based on the following criteria: subject not engaged in downhill snow skiing or snowboarding (eg, jumping into the swimming pool with snow-board), non-head injury, product other than a snowboard or ski was involved (eg, skateboard), injury occurred at a location other than a US ski resort (eg, home; in Argentina), injury occurred inadvertently and not directly due to snow sports activity (eg, equipment falling from the wall onto a person).
Statistical analysis
The NSAA reported estimates of snow sports participation by winter season, so injuries were also assigned to a winter season based on the date of injury occurrence. For example, winter season 1996–1997 includes injuries that took place between 1 July 1996 and 30 June 1997.
Analyses were conducted using Stata/SE v.11.2.22 National estimates of paediatric snow-sports-related head injuries were summarised by age group, sex, discharge disposition, NEISS diagnosis and injury category (TBI, other head injury), and product (ski, snowboard) for seasons 1996–1997 to 2009–2010 using svy commands in Stata statistical software to account for sampling variation.22 Patient characteristics were compared across injury categories using χ2 tests.
Injury incidence rates (per 10 000 resort visits) were calculated as the number of head injuries divided by snow sports participation estimates derived from annual NSAA surveys. We calculated separate rates for children (4–12 years old) and adolescents (13–17 years old). Yearly variation in the likelihood (relative risk, RR) of head injuries was calculated using annual incidence rates, with the first season (1996–1997) as reference. To assess whether the severity of reported head injuries changed over the study period, we used discharge disposition as a proxy for severity. The likelihood of being released from the ED versus admitted or transferred was compared for children and adolescent TBI cases over the study period, using the 1996–1997 season as reference.
The study protocol was deemed exempt from institutional review board review by the University of Washington Human Subjects Division.
RESULTS
From July 1996 to December 2010, there was an estimate of 671 112 (95% CI 310 423 to 1 031 808) injuries associated with skiing and snowboarding among participants aged 4–17 years. To generate the study sample of paediatric head injuries, we first excluded 2639 cases that were ineligible through narrative reviews. Common reasons for exclusion were injuries that occurred inadvertently and not directly due to snow sports activity (51%), and injuries among patients who were not engaged in downhill snow skiing or snowboarding (36%). Of the 1302 cases with missing NEISS diagnoses, most patients (90%) were able to be classified through narrative reviews; 27% were classified as concussions (‘TBI’) and 73% were classified as scalp lacerations, contusions or other (‘other head injury’). Eighty-one patients with haemorrhage or haematoma diagnoses were reclassified as TBI based on narrative reviews.
The final study sample consisted of 78 538 (95% CI 66 350 to 90 727) paediatric head injuries reported to EDs for snowboarding or skiing during winter seasons 1996–1997 to 2009–2010. Of these injuries, 33.8% were among children (4–12 years old) and 66.2% were among adolescents (13–17 years old). More head injuries were diagnosed as TBI among adolescents than children (82% vs 69%, respectively; p<0.01) (table 1). Concussions and intracranial injuries represented the majority of TBI cases, whereas most other head injuries were attributed to scalp lacerations or contusions/abrasions. Most patients with head injuries were treated and released from the ED. Among children, most TBIs were associated with skiing (55%), whereas for adolescents, the majority of TBIs were associated with snowboarding (62%) (p<0.01).
Table 1.
Paediatric ED visits for snow-sports-related head injuries, 1996–1997 to 2009–2010 seasons
| Children (aged 4-12 years) |
Adolescents (aged 13-17 years) |
|||||||
|---|---|---|---|---|---|---|---|---|
| TBI |
Other head injuries |
TBI |
Other head injury |
|||||
| N | % | N | % | N | % | N | % | |
| Sex | ||||||||
| Male | 13 766 | 76 | 6855 | 83 | 30 411 | 72 | 6396 | 67 |
| Female | 4462 | 24 | 1440 | 17 | 11 987 | 28 | 3221 | 33 |
| Diagnosis | ||||||||
| Concussion | 11 287 | 62 | – | – | 28 077 | 66 | – | – |
| Other intracranial injury* | 6731 | 37 | – | – | 14 050 | 33 | – | – |
| Fracture | 209 | 1 | – | – | 272 | 1 | – | – |
| Haematoma/haemorrhage (scalp) | – | – | 206 | 2 | – | – | 162 | 2 |
| Scalp laceration | – | – | 4827 | 58 | – | – | 4241 | 44 |
| Scalp contusion/abrasion | – | – | 3192 | 38 | – | – | 4978 | 52 |
| Puncture | – | – | 0 | 0 | – | – | 112 | 0 |
| Avulsion | – | – | 69 | 1 | – | – | 0 | 0 |
| Missing | – | – | 0 | 0 | – | – | 125 | 1 |
| ED discharge disposition | ||||||||
| Released | 16 830 | 92 | 8214 | 99 | 38 209 | 90 | 9376 | 97 |
| Transferred | 427 | 2 | 80 | 1 | 1096 | 3 | 203 | 2 |
| Admitted or held for observation | 965 | 5 | 0 | 0 | 3082 | 7 | 38 | 0 |
| Left without being seen | 5 | 0 | 0 | 0 | 6 | 0 | 0 | 0 |
| Missing | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 |
| Product/Sport | ||||||||
| Skis (alpine) | 10 051 | 55 | 3414 | 41 | 16 302 | 38 | 3640 | 38 |
| Snowboard | 8176 | 45 | 4881 | 59 | 26 097 | 62 | 5977 | 62 |
| Total | 18 227 | 69 | 8295 | 31 | 42 399 | 82 | 9618 | 18 |
Values are weighted and represent national estimates of snow-sports-related head injuries from 1996 to 2010 from the National Electronic Injury Surveillance System. Percentages may not sum to 100% due to rounding.
Includes internal organ injury and intracranial haematoma or haemorrhage.
ED, emergency department; TBI, traumatic brain injury.
Injury rates
The average incidence of all paediatric head injuries from 1996–1997 to 2009–2010 was 3.14 per 10 000 resort visits (95% CI 2.65 to 3.62). Over this time period, the average incidence of TBI was 2.42 per 10 000 visits (95% CI 1.92 to 2.93). The incidence of other head injuries was 0.72 per 10 000 visits (95% CI 0.53 to 0.90). For children, the average incidence of TBI was 1.59 per 10 000 visits (95% CI 1.20 to 2.93) compared with 3.13 per 10 000 visits (95% CI 2.85 to 3.41) for adolescents.
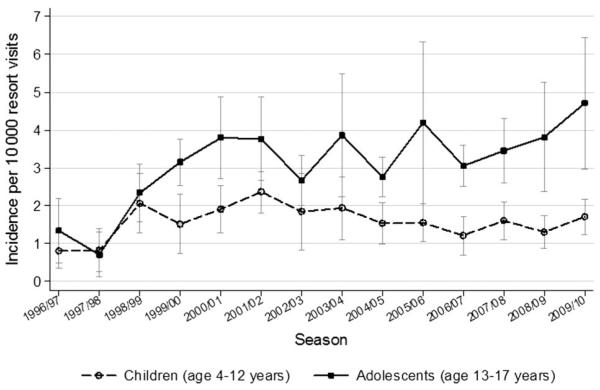
The average incidence of TBI and other head injuries among children did not vary significantly over the 14 seasons (change in the incidence for both TBI and other head injuries: 0.01 percentage points per year, p=0.64). In contrast, among adolescents, the TBI incidence increased to 0.19 percentage points per year (p<0.01), whereas the incidence of other head injuries did not vary significantly over time (change in incidence for other head injuries: −0.03 percentage points per year, p=0.09). For adolescents, graphical results demonstrate an increase in TBI incidence over the study period; this trend is not observed among children (figure 1).
Figure 1.
Incidence of emergency department-reported traumatic brain injuries associated with snow sports among children and adolescents from 1996–1997 to 2009–2010 seasons. Based on population-level estimates of snow-sports-related head injuries from the National Electronic Injury Surveillance System and national ski area participation data from the National Ski Area Association. Incidence values reported are per 10 000 ski or snowboard resort visits for each age group. Vertical bars indicate 95% CIs for incidence estimates.
RR of TBI
Compared with the 1996–1997 season, the RR of snow-sports-related TBI in recent seasons was higher for both children and adolescents (table 2). For example, the likelihood of TBI among children in 2009–2010 was 111% higher than that in 1996–1997 (RR 2.11, 95% CI 1.71 to 3.58). The likelihood of TBI among adolescents was 250% higher in 2009–2010 than 1996–1997 (RR 3.50, 95% CI 2.94 to 5.99).
Table 2.
Likelihood of ED-reported TBIs associated with snow sports among children and adolescents
| Season | Children (aged 4–12 years) |
Adolescents (aged 13–17 years) |
||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| 1996–1997 | 1.00 | Reference | 1.00 | Reference |
| 1997–1998 | 1.02 | 0.74 to 1.09 | 0.53 | 0.25 to 0.59 |
| 1998–1999 | 2.55 | 2.23 to 3.70 | 1.74 | 1.41 to 3.18 |
| 1999–2000 | 1.87 | 1.81 to 2.10 | 2.35 | 1.72 to 5.12 |
| 2000–2001 | 2.36 | 1.99 to 3.70 | 2.82 | 2.22 to 5.48 |
| 2001–2002 | 2.92 | 2.29 to 5.24 | 2.80 | 2.22 to 5.36 |
| 2002–2003 | 2.28 | 2.24 to 2.42 | 1.99 | 1.52 to 4.04 |
| 2003–2004 | 2.40 | 2.18 to 3.21 | 2.87 | 2.51 to 4.50 |
| 2004–2005 | 1.89 | 1.64 to 2.83 | 2.05 | 1.50 to 4.51 |
| 2005–2006 | 1.91 | 1.61 to 3.02 | 3.12 | 2.89 to 4.15 |
| 2006–2007 | 1.50 | 1.36 to 2.03 | 2.27 | 1.64 to 5.03 |
| 2007–2008 | 1.98 | 1.66 to 3.18 | 2.57 | 1.97 to 5.23 |
| 2008–2009 | 1.61 | 1.37 to 2.52 | 2.83 | 2.40 to 4.76 |
| 2009–2010 | 2.11 | 1.71 to 3.58 | 3.50 | 2.94 to 5.99 |
ED, emergency department; RR, relative risk; TBI, traumatic brain injury.
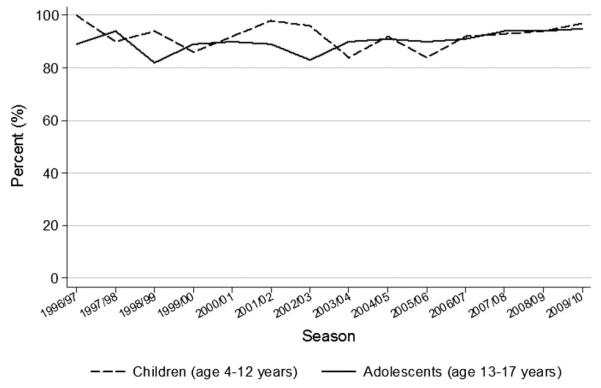
Severity
Among TBI cases, most children and adolescents were released after being seen in the ED, rather than being transferred, admitted or held for observation (table 1). The proportion of TBI cases treated and released did not vary substantially over time for children or adolescents (figure 2). Linear regression analyses evaluating the change in the proportion of TBI patients treated and released across all seasons indicated no significant trend over time for children (p=0.84) and adolescents (p=0.06).
Figure 2.
Percentage of patients ‘treated and released’ from the emergency department after seeking treatment for snow-sports-related traumatic brain injuries from 1996–1997 to 2009–2010.
DISCUSSION
This study found that from 1996 to 2010, TBIs constituted the majority of ED-reported head injuries from skiing and snowboarding among children and adolescents. Our study found higher rates of ED visits for snow sports-related TBI among adolescents than children and an increasing incidence of these injuries in adolescents over time.
Previous research supports the finding that adolescents have higher rates of ED visits and hospitalisations for concussions and TBIs than younger children, both generally and specifically to sports-related or recreation-related injuries.3,4,23,24 For skiing and snowboarding, resort-specific or regional case–control studies show adolescents constituting the majority of head injury cases.19,20 To our knowledge, this is the first study to use nationally representative data to examine snow-sports-related TBIs among children and adolescents.
The public health and medical literature has recently highlighted the importance of recognising trends in paediatric TBIs. From 2001 to 2009, Gilchrist et al.3 reported an increase in the rate of ED visits for non-fatal sports-related TBIs among children (less than 20 years old). However, that analysis did not include skiing or snowboarding injuries, and our data suggest that an increase in snow-sports-related TBIs among adolescents began even earlier (figure 1). Smaller studies have reported increases in snow-sports-related head injuries over time. A single-resort study in Vermont reported an increase in head injuries and concussions among adolescents from 1972–1973 to 1993–1994.25 A review of ski and snowboard injuries at 16 Canadian EDs demonstrated an increase in head injuries among 12–17 year olds from 1995 to 1999.26 The CPSC evaluated ED visits nationally and found an increase in snowboarding and skiing head injuries among children (aged ≤15 years) from 1993 to 1997.27 A review of the literature suggests that the incidence of medically treated head injuries, including TBIs, has increased among skiers and snowboarders of all ages from 1990 to 2004.26,28 Our study provides evidence of an increasing trend in snow-sports-related TBIs among adolescents, but not children, from 1996 to 2010.
Our results may have implications for targeted interventions involving helmet use in injury prevention. Previous research suggests that age is a strong predictor of helmet use in bicycling and skiing,29-31 and industry data suggest lower uptake of helmet use by teens than by younger children.32 Increased educational efforts and interventions may be warranted to generate injury awareness and minimise hazards associated with snow sports for adolescents.33 Mandatory helmet laws for minors at some ski areas have been enacted to improve compliance and ensure optimal safety.34 In Colorado, injury prevention efforts include provision of free helmets with ski or snowboard rentals.35 Insurance incentives for ski resorts may encourage implementation of safety measures to improve infrastructure. Furthermore, many resorts require an educational module for terrain park access, which can play an additional role in risk reduction and injury prevention. Terrain parks typically include jumps, half-pipes and harder surfaces that may contribute to head injury risk.
Given the retrospective and observational nature of this study, it is not possible to directly determine the reasons for the observed increase in the incidence of snow-sports-related TBIs among adolescents from 1996 to 2010. We speculate that increases may be attributed in part to changes in snow sports behaviour. The rise in the popularity of snowboarding over the study period may have contributed to the increase in TBI incidence; research suggests that the incidence of head injuries may be greater for snowboarding than skiing.28,36,37 Also, the recent proliferation of terrain parks in resorts and the rapid growth of extreme sports, which include freestyle snowboarding and skiing, may play a role in the increased head injury rates during later years.38,39 Alternatively, the trend may not be due to a true increase in TBI incidence, but instead due to improved recognition of the clinical symptoms of TBI and increased reporting to EDs for head injuries incurred while skiing or snowboarding. Both possibilities are relevant and important for future research, awareness and outreach efforts.
Several methodological limitations apply to our study, mainly due to the data sources used. The NEISS provides nationally representative estimates of patients treated in hospital EDs and does not capture untreated injuries or those treated elsewhere. Our study may therefore underestimate the incidence of snow-sports-related head injuries. Also, NEISS provides only limited information about the patients; for instance, reporting of helmet use is inconsistent. Other than evaluating discharge disposition, we were unable to determine TBI severity, so our analyses were restricted to a general definition of TBI.21 Because NEISS is generally not regarded as useful for studying fatal injuries, we evaluated the incidence of non-fatal head injuries only. In addition to NEISS data, we used national estimates of snow sports participation to calculate incidence rates, which also presented several challenges. First, these data consider only the in-bounds resort skiing, excluding estimates for skiers or snowboarders who engaged in skiing elsewhere. However, it is unlikely that children would be frequently engaging in back-country skiing, and we carefully reviewed all injury narratives to exclude any that occurred outside a resort or the USA. Second, because the participation data did not specify skiing or snowboarding, we were unable to provide separate head injury rates for each sport. Injury rates may differ by snowsport.28,36,37 Despite these limitations, this study provides updated national estimates of the incidence of paediatric head injuries from skiing and snowboarding over a 14-year period, which may inform future research and outreach efforts.
This study has several strengths. This is a large-scale, national study to evaluate the temporal trend in snow-sports-related head injury among children and adolescents. We used national estimates of resort visits to account for variation in sports participation over time, unlike studies that focus on specific resorts or compare the rate of head injuries to other snow-sports-related injuries without generating a national incidence rate. Furthermore, most studies of ski and snowboard injuries use data from regional, state or local sources for shorter periods of time; a substantial strength of this study is its large, nationally representative sample size over a 14-year period.
CONCLUSIONS
Snow-sports-related head injuries may be an important source of morbidity among children and adolescents. Our results suggest that adolescents have a higher incidence of snow-sports-related TBIs than children, and that the incidence of snow-sports-related TBIs has increased among adolescents. Additional efforts to understand the causes of this increase are warranted and will have implications for preventive interventions in the future.
What is already known on the subject.
-
▶
Traumatic brain injury (TBI) is a serious public health concern among children and adolescents.
-
▶
Sports-related TBIs occur frequently among young athletes and has been increasing over time.
What this study adds.
-
▶
Snow-sports-related TBIs treated in emergency departments (EDs) are more common among adolescents (aged 13–17 years) than children (aged 4–12 years).
-
▶
ED-treated TBIs associated with snow-sports increased from 1996 to 2010 among adolescents.
Acknowledgements
The authors thank David Byrd at the National Ski Area Association providing ski participation data. The authors appreciate the helpful comments and suggestions from Dr Patricia Ayoung-Chee.
Funding This research is supported in part by the Wilderness Medical Society Research-in-Training Award (Graves). JMG and JMW receive fellowship support from National Institute of Child Health and Human Development (T32 HD057822-01A2).
Footnotes
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The National Electronic Injury Surveillance Survey (NEISS) data used in this study are publicly available from the Consumer Product Safety Commission (http://www.cpsc.gov/cpscpub/pubs/3002.html).
Contributors JMG, JMW and FPR conceived of and designed the study. JMG acquired the data. JMG, JMW and JOS coded data and conducted the analyses. JMG led the writing of the article. JMW, JOS, MSV and FPR contributed data interpretation and critical manuscript revisions. All authors gave final approval of the version to be published.
REFERENCES
- 1.Halstead ME, Walter KD. American Academy of Pediatrics. Clinical report—sport-related concussion in children and adolescents. Pediatrics. 2010;126:597–615. doi: 10.1542/peds.2010-2005. [DOI] [PubMed] [Google Scholar]
- 2.State of Washington . Youth sports—Concussion and head injury guidelines—Injured athlete restrictions. RCW Title 28A: Chapter 600.190. [Google Scholar]
- 3.Gilchrist JTK, Xu L, McGuire LC, et al. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years—United States, 2001-2009. MMWR Morb Mortal Wkly Rep. 2011;60:1337–42. [PubMed] [Google Scholar]
- 4.Bakhos LL, Lockhart GR, Myers R, et al. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126:e550–6. doi: 10.1542/peds.2009-3101. [DOI] [PubMed] [Google Scholar]
- 5.Taylor HG, Yeates KO, Wade SL, et al. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 6.Anderson V, Brown S, Newitt H, et al. Long-term outcome from childhood traumatic brain injury: intellectual ability, personality, and quality of life. Neuropsychology. 2011;25:176–84. doi: 10.1037/a0021217. [DOI] [PubMed] [Google Scholar]
- 7.Todis B, Glang A, Bullis M, et al. Longitudinal investigation of the post-high school transition experiences of adolescents with traumatic brain injury. J Head Trauma Rehabil. 2011;26:138–49. doi: 10.1097/HTR.0b013e3181e5a87a. [DOI] [PubMed] [Google Scholar]
- 8.Ryan LM, Warden DL. Post concussion syndrome. Int Rev Psychiatry. 2003;15:310–16. doi: 10.1080/09540260310001606692. [DOI] [PubMed] [Google Scholar]
- 9.Blume HK, Vavilala MS, Jaffe KM, et al. Headache after pediatric traumatic brain injury: a cohort study. Pediatrics. 2011;129:e31–9. doi: 10.1542/peds.2011-1742. [DOI] [PubMed] [Google Scholar]
- 10.Bombardier CH, Fann JR, Temkin NR, et al. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA. 2010;303:1938–45. doi: 10.1001/jama.2010.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor SS, Zatzick DF, Wang J, et al. Association between posttraumatic stress, depression, and functional impairments in adolescents 24 months after traumatic brain injury. J Trauma Stress. 2012;25:264–71. doi: 10.1002/jts.21704. [DOI] [PubMed] [Google Scholar]
- 12.Rockhill CM, Jaffe K, Zhou C, et al. Health care costs associated with traumatic brain injury and psychiatric illness in adults. J Neurotrauma. 2012;29:1038–46. doi: 10.1089/neu.2010.1562. [DOI] [PubMed] [Google Scholar]
- 13.Xiang H, Kelleher K, Shields BJ, et al. Skiing- and snowboarding-related injuries treated in U.S. emergency departments, 2002. J Trauma. 2005;58:112–18. doi: 10.1097/01.ta.0000151270.26634.dd. [DOI] [PubMed] [Google Scholar]
- 14.Wasden CC, McIntosh SE, Keith DS, et al. An analysis of skiing and snowboarding injuries on Utah slopes. J Trauma. 2009;67:1022–6. doi: 10.1097/TA.0b013e3181b0d559. [DOI] [PubMed] [Google Scholar]
- 15.Burtscher M, Gatterer H, Flatz M, et al. Effects of modern ski equipment on the overall injury rate and the pattern of injury location in Alpine skiing. Clin J Sport Med. 2008;18:355–7. doi: 10.1097/MJT.0b013e31815fd0fe. [DOI] [PubMed] [Google Scholar]
- 16.Cusimano MD, Kwok J. The effectiveness of helmet wear in skiers and snowboarders: a systematic review. Br J Sports Med. 2010;44:781–6. doi: 10.1136/bjsm.2009.070573. [DOI] [PubMed] [Google Scholar]
- 17.Hagel BE, Pless IB, Goulet C, et al. Effectiveness of helmets in skiers and snowboarders: case-control and case crossover study. Br J Med. 2005;330:281. doi: 10.1136/bmj.38314.480035.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McBeth PB, Ball CG, Mulloy RH, et al. Alpine ski and snowboarding traumatic injuries: incidence, injury patterns, and risk factors for 10 years. Am J Surg. 2009;197:560–3. doi: 10.1016/j.amjsurg.2008.12.016. discussion 63-4. [DOI] [PubMed] [Google Scholar]
- 19.Mueller BA, Cummings P, Rivara FP, et al. Injuries of the head, face, and neck in relation to ski helmet use. Epidemiology. 2008;19:270–6. doi: 10.1097/EDE.0b013e318163567c. [DOI] [PubMed] [Google Scholar]
- 20.Sulheim S, Holme I, Ekeland A, et al. Helmet use and risk of head injuries in alpine skiers and snowboarders. JAMA. 2006;295:919–24. doi: 10.1001/jama.295.8.919. [DOI] [PubMed] [Google Scholar]
- 21.Xiang H, Sinclair SA, Yu S, et al. Case ascertainment in pediatric traumatic brain injury: challenges in using the NEISS. Brain Inj. 2007;21:293–9. doi: 10.1080/02699050701311034. [DOI] [PubMed] [Google Scholar]
- 22.Stata Statistics/Data Analysis Software . Special edition 11.2 (for Windows) [program] StataCorp LP; College Station, TX: 2011. [Google Scholar]
- 23.Faul MXL, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002-2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Atlanta, GA: 2010. [Google Scholar]
- 24.Yang J, Phillips G, Xiang H, et al. Hospitalisations for sport-related concussions in US children aged 5 to 18 years during 2000-2004. Br J Sports Med. 2008;42:664–9. doi: 10.1136/bjsm.2007.040923. [DOI] [PubMed] [Google Scholar]
- 25.Deibert MC, Aronsson DD, Johnson RJ, et al. Skiing injuries in children, adolescents, and adults. J Bone Joint Surg Am. 1998;80:25–32. [PubMed] [Google Scholar]
- 26.Hagel BE, Pless B, Platt RW. Trends in emergency department reported head and neck injuries among skiers and snowboarders. Can J Public Health. 2003;94:458–62. doi: 10.1007/BF03405085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Consumer Product Safety Commission . Skiing helmets, an evaluation of the potential to reduce head injury. US Consumer Product Safety Commission; Washington, DC: 1999. [Google Scholar]
- 28.Ackery A, Hagel BE, Provvidenza C, et al. An international review of head and spinal cord injuries in alpine skiing and snowboarding. Inj Prev. 2007;13:368–75. doi: 10.1136/ip.2007.017285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawrence L, Shaha S, Lillis K. Observational study of helmet use among children skiing and snowboarding. Pediatr Emerg Care. 2008;24:219–21. doi: 10.1097/PEC.0b013e31816a9f0a. [DOI] [PubMed] [Google Scholar]
- 30.Klein KS, Thompson D, Scheidt PC, et al. Factors associated with bicycle helmet use among young adolescents in a multinational sample. Inj Prev. 2005;11:288–93. doi: 10.1136/ip.2004.007013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harlos S, Warda L, Buchan N, et al. Urban and rural patterns of bicycle helmet use: factors predicting usage. Inj Prev. 1999;5:183–8. doi: 10.1136/ip.5.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Ski Area Association (NSAA) [accessed 17 Jan 2012];Study Shows Most Skiers and Riders Wearing Helmets on the Slopes. http://www.nsaa.org/nsaa/press/1011/helmet-usage.asp.
- 33.Cusimano MD, Kwok J. Skiers, snowboarders, and safety helmets. JAMA. 2010;303:661–62. doi: 10.1001/jama.2010.147. [DOI] [PubMed] [Google Scholar]
- 34.State of New Jersey . Helmet required for downhill skiers, snowboarders: violations, penalties. L.2011, c.41, s.1. [Google Scholar]
- 35.Levy AS, Hawkes AP, Rossie GV. Helmets for skiers and snowboarders: an injury prevention program. Health Promot Pract. 2007;8:257–65. doi: 10.1177/1524839906292178. [DOI] [PubMed] [Google Scholar]
- 36.Hentschel S, Hader W, Boyd M. Head injuries in skiers and snowboarders in British Columbia. Can J Neurol Sci. 2001;28:42–6. doi: 10.1017/s0317167100052537. [DOI] [PubMed] [Google Scholar]
- 37.Nakaguchi H, Fujimaki T, Ueki K, et al. Snowboard head injury: prospective study in Chino, Nagano, for two seasons from 1995 to 1997. J Trauma. 1999;46:1066–9. doi: 10.1097/00005373-199906000-00017. [DOI] [PubMed] [Google Scholar]
- 38.Brooks MA, Evans MD, Rivara FP. Evaluation of skiing and snowboarding injuries sustained in terrain parks versus traditional slopes. Inj Prev. 2010;16:119–22. doi: 10.1136/ip.2009.022608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goulet C, Hagel B, Hamel D, et al. Risk factors associated with serious ski patrol-reported injuries sustained by skiers and snowboarders in snow-parks and on other slopes. Can J Public Health. 2007;98:402–6. doi: 10.1007/BF03405428. [DOI] [PMC free article] [PubMed] [Google Scholar]