Abstract
This study examined patterns of movement for youth receiving services within a continuum of intensive and restrictive residentially-based programs. Data were collected for 701 completed episodes of care within a three-program residential continuum of care over a 5 year period, and examined time within program, movement between programs, in-program disruptive behavior, and discharge status. Results showed that most youth either remained in a stable placement in the least restrictive of the programs, or followed a pattern of placements that systematically moved them from more restrictive to less restrictive settings. Of note, transitions from more restrictive to less restrictive programs correspond to deescalating levels of problem behavior; and over 80% of the youth were stepped down to either family-based or independent living situations at the time of departure. Findings support the notion that a continuum of intensive residential services can serve the needs of youth with significant emotional and behavioral needs.
Keywords: Adolescent, Continuum of care, Emotional and behavior disorders, Residential care
1. Introduction
The out-of-home care options specifically designed to address the needs of youth with emotional and behavioral disorders who cannot be maintained in lower level family-based settings (e.g., non-relative foster care and relative foster care) range from treatment foster care, (therapeutic) group homes, and residential treatment centers to inpatient psychiatric care. These settings constitute a complex amalgamation of programs and services providing placement and services to children with a variety of needs from multiple service systems (Garland, Hough, Landsverk, & Brown, 2001).
Within this continuum of intensive and restrictive care services available, placement into all but treatment foster care is generally considered an adverse outcome by child service systems, policy makers and consumers (Dodge, 2006). Group homes, residential treatment and inpatient psychiatric care constitute forms of service delivery, which ideologically depart from system of care emphasis on community-based care, are the most costly and restrictive interventions available and have a comparably weak evidence base for their effectiveness (Burns, Hoagwood, & Mrazek, 1999; Butler & McPherson, 2007). As such, the placement of youth into any of these settings is theoretically intended as a last resort and as a response to treatment needs that cannot be addressed in less restrictive family-based care settings (Barth, 2002). In spite of the skepticism about their continued use (Dishion, Dodge, & Lansford, 2008), these settings have remained an integral component of the system of services for youth (Geller & Biebel, 2006; McCurdy & Mclntyre, 2004). This is supported by some research evidence that group homes and residential treatment centers care for children with greater treatment needs (Nash, Thompson, & Kim, 2006; Preyde, Adams, Cameron, & Frensch, 2009), and continue to be the most frequently utilized placements within the continuum of intensive and restrictive services available (James et al., 2006; McMillen et al., 2004).
Youth placed into intensive and restrictive settings tend to have complex needs that often require more intensive intervention than can be provided in foster care or standard outpatient mental health treatment (Ainsworth & Hansen, 2005; Davidson-Arad, 2005). These youth have been described as presenting with significant emotional and disruptive behaviors that frequently require psychopharmacological intervention (Breland-Noble et al., 2004). They are also considered at high risk for substance use and other health-risking behaviors (Trout et al., 2010; Weiner, Abraham, & Lyons, 2001). They frequently have lengthy placement histories, moving up and down the continuum of placements available, and are at risk of transitioning into other service systems, such as juvenile justice and mental health, and later on, adult service systems (Dore, 1999; James, Landsverk, & Slymen, 2004). Development of community-based treatments such as multidimensional treatment foster care (Chamberlain, 1998), multisystemic therapy (Henggeler, Schoenwald, Borduin, Rowland, & Cunningham, 1998), and wraparound services (Burchard, Bruns, & Burchard, 2002) has promised to bring diffusion of evidence-based and less costly interventions into service systems for children and adolescents and thus reduce the need for group home and residential care over time. However, the effective implementation of alternative evidence-based practices into real world service systems remains challenging, and effectively addressing the needs of youth in need of more intensive and restrictive services remains a priority for many service systems.
Given concerns about placement into the most costly and restrictive placement options, system of care philosophy and current policy mandate utilization of alternative community-based treatments whenever possible and movement into less restrictive placement options (Fields & Ogles, 2002). For the most part, researchers have found a high level of correspondence between youth problems and the restrictiveness of the setting in which they receive care (Handwerk, Friman, Mott, & Stairs, 1998; Nash et al., 2006), although this is not always the case (Fields & Ogles, 2004).
Unfortunately, children do not always neatly move up and down the continuum of care depending on their level of clinical severity but some move back and forth between settings of different levels of restrictiveness (Farmer, Wagner, Burns, & Richards, 2003; James et al., 2004). In fact, there are considerable similarities in the clinical needs of children served by different intensive and restrictive care settings (Breland-Noble, Farmer, Dubs, Potter, & Burns, 2005; Lyons, Libman-Mintzer, Kisiel, & Shallcross, 1998), raising questions about either the function of these settings or the ability of service systems to provide and effectively coordinate optimal levels of care for youth. Research has found that placing youth with more extreme behavioral problems in family-based services is associated with lack of clinical progress and placement instability (Davidson-Arad, 2005; James, 2004; Oosterman, Schuengel, Slot, Bullens, & Doreleijers, 2007; Wulczyn, Kogan, & Harden, 2003). About half of foster care youth experience one or more placement disruptions (Connell et al., 2006; Staff & Fein, 1995), with higher levels of placement disruption being associated with increasing levels of low inhibitory control and opposition behavior in youth (Lewis, Dozier, Ackerman, & Sepulveda-Kozakowski, 2007). While a child's clinical needs are an important consideration in the placement of a child, contextual factors such as policy mandates (James, 2004) and resource availability (Hurlburt et al., 2004; Pottick, Warner, & Yoder, 2005) have also been shown to regulate where and when a child is placed and what type of services are accessed. Correspondence between problems and level of care would be consistent with a rational system of care, in which youth step up to more restrictive settings or step down to less restrictive settings according to their clinical needs (Handwerk et al., 1998).
To date, little is known about the movement of youth within the continuum of intensive and restrictive placements available. The importance of studying movement or pathways through out-of-home care has previously been emphasized by child welfare and mental health researchers dealing primarily with foster care populations (Barth, Courtney, Berrick, & Albert, 1994; Farmer et al., 2003; Usher, Randolph, & Gogan, 1999; Wulczyn et al., 2003). Other research has examined the impact of type of placement and placement disruption on outcome for children in out-of-home placement (Benedict, Zuravin, & Stallings, 1996; Iglehart, 1994; Smith, Stormshak, Chamberlain, & Bridges Whaley, 2001; Usher et al., 1999; Webster, Barth, & Needell, 2000).
This paper examined the patterns of movement for youth receiving services within a residentially-based continuum of care providing a range of services with different levels of restrictiveness. This environment offers a unique opportunity to examine movement patterns within an integrated continuum of residential care programs, where our objective is to investigate the patterns and how youth disruptive behavior relates to transitions between levels of care.
2. Method
2.1. Setting
The setting for this study was a large, mid-western, residentially-based continuum of care for youth. The residential program has its theoretical roots in the Teaching-Family Model developed at the University of Kansas in the 1970s (Wolf et al., 1976). This approach is based on operant and social learning theories and emphasizes the acquisition of positive behaviors in family-style residential settings via modeling, prompting, reinforcement, and guided practice. The current model has evolved to include six core hallmarks: teaching life skills, using tested motivation systems, building trusting relationships with peers and adults, living in the most family-style setting possible, encouraging the development of moral and spiritual values, and making self-control and self-government the goal for every youth (Davis & Daly, 2003). The primary treatment agents are the people working closest to the children being served. Each youth has individualized treatment goals and attends on-site school. Some children additionally receive individualized or group therapy, depending on their treatment needs.
The intervention strategies developed for this family-style residential care have been used to develop a continuum of residential treatment programs to serve children with varying levels of need in mental health, juvenile justice, and child welfare systems. These programs include a locked, medically supervised Intensive Residential Treatment Center, and staff-secure therapeutic group homes with shift staff. Intervention methods had to be adapted for each of these different settings, but the same basic model of care was maintained.
2.2. The residential continuum
The continuum of residential care services examined in this study consisted of three programs. Each of the programs is described below, with Treatment Family Homes being the least restrictive and the Intensive Residential Treatment Center being the most restrictive of the three. Table 1 shows the differences in diagnostic rates for the three programs.
Table 1.
Youth race, sex, DSM diagnosis, and age at time of admission by residential continuum admission program.
| TFH |
STGH |
IRTC |
Total |
|
|---|---|---|---|---|
| n = 283 | n = 145 | n = 273 | n = 701 | |
| Race | ||||
| Caucasian | 53.4% | 78.6% | 66.1% | 63.9% |
| African-American | 15.9% | 10.1% | 15.1% | 14.4% |
| Hispanic | 19.1% | 1.3% | 3.8% | 9.0% |
| Native American | 6.7% | 5.0% | 4.1% | 5.3% |
| Other | 4.9% | 5.0% | 11.0% | 7.5% |
| Sex | ||||
| Female | 35.0% | 38.6% | 50.5% | 41.8% |
| Male | 65.0% | 61.4% | 49.5% | 58.2% |
| DSM IV diagnosis (% yes) | 55.0% | 100% | 100% | 81.5% |
| Age at time of admission (mean) | 14.8 | 14.6 | 14.4 | 14.6 |
Treatment Family Homes
(TFH; family-style, residential care provided by a specially trained married couple and an Assistant Family-Teacher). Treatment Family Homes are a family-style, community-based program that can serve six to eight males or females, usually ages 12 to 18. Married couples called Family-Teachers are the primary treatment agents. Family-Teachers are responsible for structured supervision of youth in daily living and treatment activities. The couple and their assistant work on both treatment and skill building in the home, and with community and family resources in the child's life. Clinical and medical supervision is an integral part of the program and professionals are available on a 24-h basis.
Seventy TFH homes are located on a 144 acre campus, and the program has the capacity of simultaneously treating 516 youth. Most youth in the TFH program have a history of two or more out-of-home placements prior to admission, and typically manifest low levels of aggression (1.4 daily acts per 100 youth) and experience very infrequent safety holds (restraints; .01 daily per 100 youth). Seclusions and PRN medication are not used in this program. TFH youth receive schooling in regular education classrooms in an on-site high school.
Specialized Treatment Group Home Services
(STGH; A medically directed and staff secure treatment program for youth ages 10 to 18). Specialized Treatment Group Homes provide treatment within a family-oriented environment for youth with psychiatric disorders. These homes are run by shift staff and have the capacity for 14 youth. This program is also Medicaid funded with all youth having a DSM IV diagnosis. The program offers support, care, and round-the-clock supervision to enable youth to progress in daily living skills and appropriate healthy socialization. The goal of the program is to help children successfully transition to a less restrictive level of care.
Four STGH homes are located on the same campus as the TFH program, with the capacity to provide treatment for 55 youth. Most STGH youth are admitted following a stay in a residential treatment program, and typically have moderate rates of aggression (19.1 daily acts per 100 youth) with infrequent safety holds (restraints; .2 daily per 100 youth). Seclusions and PRN medication are not used in this program. STGH youth receive schooling within self-contained special education (SPED) classroom in the on-site high school.
Intensive Residential Treatment Center Services
(IRTC; A 24-h residential treatment program for youth ages 7 to 18 with psychiatric disorders). The Intensive Residential Treatment Center is a long-term residential program specifically designed to offer medically directed care for more seriously troubled youth who require supervision, safety, and therapy but do not require inpatient psychiatric care. The program is Medicaid funded, and all youth have a DSM IV diagnosis. The Center provides round-the-clock supervision, locked/secure facilities, and numerous other safety and program features. For many of these high-risk youth, placements in traditional treatment programs have repeatedly failed and reunification with the family holds little promise without stabilizing intervention.
The IRTC consists of four secured units located within a research hospital setting that has the capacity to provide treatment for 47 youth. Most youth are admitted to the STGH following residence in a highly restrictive setting (e.g., inpatient hospitalization, juvenile justice detention). These youth manifest high rates of aggression (46.6 daily acts per 100 youth), which correspond to frequent safety holds (restraints; 8.5 daily per 100 youth). Seclusions are used (6.9 daily per 100 youth) and PRN medication also occurs, but infrequently (.5 daily per 100 youth). STGH youth receive schooling within a SPED classroom in the unit.
2.3. Participants
The sample consists of all completed episodes of care between October 2001 and October 2006. We defined an episode of care as period of time where a youth remains in care in one or more of these residential programs, with no time gaps between program transitions when they occur. Eligible cases were limited to youth who were at least 11 years old.1 There were 701 completed episodes of care for this period, of which 425 episodes entailed one or more moves between programs within the residential system of care.
Table 1 shows the race, sex, and average age for youth at the time of admission to the residential continuum of care. While the average age at the time of admission for youth decreased slightly with program restrictiveness, there was no significant difference across programs; F (2, 698)=2.2, p=.104.
Overall, 63.9% of the youth were Caucasian, 14.4% were African-American, 9.0% were Hispanic, 5.3% were Native American, and 7.5% other (i.e., Asian, multi-racial, other). There was a significant difference on racial proportions for the different programs; χ2 (8)=60.5, p<.0001. The IRTC had a lower rate of Hispanics, the STGH had a higher rate of Caucasians and a lower rate of Hispanics, and the TFH had a higher rate of Hispanics and a lower rate of Caucasians than expected based on examination of the standardized residuals.
Overall, 58.2% of the youth were male, and 41.8% were female. There was a significant difference for the ratio of males and females for the residential programs; χ2 (2)=14.6, p<.001. Standardized residuals indicated that there was a higher proportion of females in the IRTC than in the other programs.
There were significant differences in the prior living environment for youth admitted to the different programs in the residential care continuum; χ2 (12)=198.8, p<.0001. The left-hand section of Table 2 shows the percentages for the living environment immediately prior to admission to each program. Standardized residuals indicated that youth who were admitted to the TFH program were more likely to have come from home settings and less likely to have come from the IRTC and other more intensive treatment settings; youth admitted to the STGH were more likely to have come from more intensive RTC or corrections settings and less likely to have come from a Home setting; and youth admitted to the IRTC were more likely to have come from an intensive treatment setting and also less likely to have come from a Home setting.
Table 2.
Placement setting prior to entering and at the time of departure from the residential continuum.
| Prior placement by placement program |
Departure placement by departure program |
|||||||
|---|---|---|---|---|---|---|---|---|
| TFH |
STGH |
IRTC |
Total |
TFH |
STGH |
IRTC |
Total |
|
| 251 | 126 | 84 | 461 | 440 | 118 | 93 | 651 | |
| Independent living | - | - | - | - | 12.9% | - | - | 8.8% |
| Home | 60.6% | 20.6% | 14.3% | 41.2% | 69.8% | 46.6% | 11.8% | 57.3% |
| Foster care | 3.2% | 6.3% | 1.2% | 3.7% | 4.8% | 12.7% | 10.7% | 7.1% |
| Group home | 7.2% | 8.7% | 2.4% | 6.7% | 2.0% | 14.4% | 34.4% | 8.9% |
| Emergency shelter | 14.7% | 10.3% | 14.3% | 13.4% | 4.3% | 1.7% | - | 3.2% |
| RTC | 2.0% | 25.4% | 15.5% | 10.8% | .7% | 4.2% | 7.5% | 2.3% |
| Intensive treatment | 1.6% | 8.7% | 40.5% | 10.6% | .9% | 11.9% | 21.5% | 5.8% |
| Corrections | 10.8% | 19.8% | 11.9% | 13.4% | 4.5% | 8.5% | 14.0% | 6.6% |
2.4. Measures
The focus of this study was the patterns of movement across a limited continuum of residential services, both in terms of time within a program and movement between programs. Within this residential continuum, most children move from more to less restrictive settings, either during their stay within the continuum, or at the time of departure from the system. The most common patterns of movement were identified.
Discharge placements were categorized as either independent living/supervised independent living (IL/SIL; this latter included living in a dormitory, military service, and job corps), home (Home; home of parents, family, and friends), foster care (Foster; all types of foster care), group care (Group), shelter (Shelter), residential treatment center (RTC), intensive treatment (Int. Tx; includes inpatient psychiatric, drug and alcohol rehabilitation, and hospitalization), or corrections (Correc.; youth corrections, detention, and jail).
Behavioral Index
Two different measures of observed behavior are used by the programs. One is the Treatment Progress Checklist (TPC) and the other is the Daily Incident Report (DIR). Both of these measures are similar to the Parent Daily Report that has been developed and used in foster care and family intervention contexts (Chamberlain & Reid, 1987; Patterson, Reid, Jones, & Conger, 1975). The principal difference between these two measures is that they use slightly different lists of problem behavior, and that the TPC records the daily frequency for each problem behavior while the DIR simply records whether or not a given problem behavior occurred during the day. The IRTC and STGH programs use the TPC, and STGH and TGH programs use the DIR. While the two measures are scored differently, there are 15 items shared by both measures with identical definitions. A cross-walk behavioral index was created by scoring these 15 items as yes or no for a given day, and then summing the incidents during 7-day periods to obtain a weekly measure. Because the STGH program uses both measures, we were able to assess the convergence between the two measures. The correlation between the common TPC and DIR items for youth in the STGH program was r=.94. The Behavioral Index was used to track problem behaviors in youth as they moved through the residential continuum of care. Table 3 lists the behaviors used in the Behavioral Index. While this list of problem behaviors used in the Behavioral Index are important indices of challenges faced by youth in the continuum of care, it should not be understood that they reflect the sole consideration for why these youth were placed in treatment nor the overriding basis upon which treatment and movement decisions are made.
Table 3.
Behavioral Index items.
| Behavior | Definition (not full descriptions) |
|---|---|
| Inappropriate sexual behavior | Exposure of body, sexual advances, sexual intercourse, masturbating in front of others, and possessing pornography |
| Lying/cheating | Presenting false information, attempt to deceive, and cheating on school assignment |
| Physical aggression toward objects | Throwing or kicking objects, slamming doors, overturning furniture, slamming books, and tearing up point card |
| Physical assault toward adults | Intentional aggressive physical contact toward an adult, e.g., biting, kicking, punching, spitting at, and jumping on |
| Physical assault toward peers | Intentional aggressive physical contact toward a peer or sibling, e.g., biting, kicking, punching, spitting at, and jumping on |
| Property damage | Intentionally damaging property, e.g., breaking windows, tearing clothes, breaking furniture, and putting holes in walls |
| Runaway | Being absent without permission where police have been contacted and a runaway report has been filed |
| School misbehavior | Inappropriate school behavior, e.g., office referral, leaving the classroom without permission, and disrupting learning |
| Self-destructive behavior | Attempts to injury or place self in danger, e.g., cutting, head banging, choking self, and biting self; does not include suicidal behavior |
| Stealing | Steals or is suspected of stealing from others, does not include food taken |
| Substance abuse/possession | Use or suspected use of alcohol, marijuana, or other illegal drugs, in possession of drugs or drug paraphernalia |
| Suicide ideation | Making a verbalization suggesting thoughts of suicide, or indicating suicidal tendencies or thoughts |
| Verbal or symbolic threats | Attempts to intimidate others with spoken or figurative behavior, e.g., verbal threats, stares, aggressive stance, and clenched fists |
| Police contact | Arrest, reprimand, or detention by police about involvement in illegal acts, including assault, , vandalism, shoplifting, and status offenses |
| Physical restraint (Safety hold) | A staff member or other adult holds a youth to keep him or her from harming self or others |
2.5. Data analysis
Chi-square was used to test for differences between the identified patterns of movement. Additionally, a repeated measures ANOVA was used to examine differences in behavior for particular periods of time. Specifically, the level of disruptive behavior for the first four weeks was contrasted with the level of disruptive behavior for the last four weeks for youth in the IRTC and STGH programs in order to determine if the level of disruptive behavior was different for these two periods of time. A similar contrast was made examining disruptive behavior levels for the last four weeks at the higher level of care versus the level of disruptive behavior during the first four weeks after transitioning to a lower level of residential care.
3. Results
As can been seen in the right-hand section of Table 2, 82.7% of all youth who were discharged from the TFH program went back either to a Home setting (69.8%) or to Independent Living (12.9%). Just less than half of youth departing from the STGH program also ended up in Home settings (46.6%), with another 27.1% going to either Group Home (14.4%) or Foster Care settings (12.7%). At departure 56.9% of IRTC went to less restrictive settings: Group Home (34.4%), Home Settings (11.8%) or Foster Care (10.7%); but there was another 35.5% who went to more restrictive intensive treatment (21.5%) or corrections settings (14.0%).
The pattern of movement for each episode of care was identified. Specifically, to which program was the youth admitted, and if there was one or more moves to another program within the residential continuum, what was the sequence of programs for that movement? In total there were 44 unique sequences of program placements for the 701 episodes. The single greatest number of episodes involved a stay in only one program (n=276, 39.4%), only one move between two programs (n=242, 34.5%), or with two program moves (n=133, 19.0%). Smaller numbers of episodes involved four or more program moves, with two cases having six program moves.
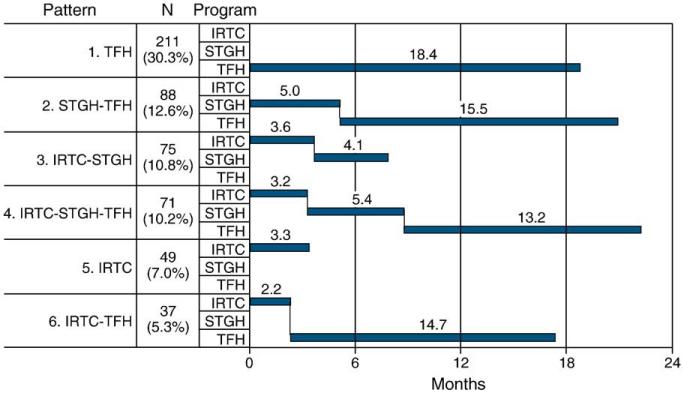
More than three-quarters (76.2%) of all episodes in the residential care continuum fell into one of 6 patterns. The patterns and average program lengths of stay are shown in Fig. 1, and the discharge placements for each of these patterns are shown in Table 4. For instance, the residential placement continuum pattern with the greatest frequency was for youth to enter and stay in the TFH program. There were 211 episodes of care that followed this pattern (30.1% of all episodes), and the average length of stay was 18.4 months, with 84.9% of youth departing from this pattern either going to an Independent Living or Home setting. Similarly, for the second most frequent pattern youth were admitted to the STGH and then stepped down to the TFH program. There were 88 episodes (12.6%) that followed this pattern, with an overall length of stay of 20.5 months and 85.0% of these youth going to independent living or home settings at the time of departure.
Fig. 1.
Pattern and average length of stay in programs in residential care continuum.
Table 4.
Discharge placement for the eight most common patterns of movement within the residential continuum, representing 80% of all episodes.
| Pattern | Discharge placement |
|||||||
|---|---|---|---|---|---|---|---|---|
| IL/SIL | Home | Foster | Group | Shelter | RTC | Int. Tx | Correc. | |
| 1. TFH | 27 | 148 | 4 | 4 | 15 | - | - | 8 |
| (211, 5 missing) | 13.1% | 71.8% | 1.9% | 1.9% | 7.3% | 0% | 0% | 3.8% |
| 2. STGH-TFH | 9 | 65 | 5 | 1 | 2 | 1 | 1 | 3 |
| (88, 1 missing) | 10.3% | 74.7% | 5.7% | 1.1% | 3.3% | 1.1% | 1.1% | 3.3% |
| 3. IRTC-STGH | - | 32 | 10 | 7 | 1 | 1 | 6 | 6 |
| (77,14 missing) | 0% | 50.0% | 14.7% | 11.5% | 1.1% | 1.1% | 6.9% | 6.9% |
| 4. IRTC-STGH-TFH | 8 | 42 | 7 | 2 | - | - | 1 | 6 |
| (71, 5 missing) | 12.1% | 63.6% | 10.6% | 3.0% | 0% | 0% | 1.5% | 9.1% |
| 5. IRTC | - | 4 | 5 | 7 | - | 2 | 19 | 7 |
| (50, 6 missing) | 0% | 9.1% | 11.4% | 15.9% | 0% | 4.5% | 43.2% | 15.9% |
| 6. IRTC-TFH | 5 | 23 | 3 | 1 | - | - | 1 | 1 |
| (37, 3 missing) | 14.7% | 67.6% | 8.8% | 2.9% | 0% | 0% | 2.9% | 2.9% |
Departure setting information was missing for 34 of these episodes (6.4%).
In general, it can be seen in Fig. 1 that most episodes of care can be represented by either stable placement in the least restrictive program (TFH) or placement in a more restrictive setting that is followed by stepping down to less restrictive programs. Consistent with what was shown in Table 2, the majority of episodes that end with a TFH stay (regardless of the pattern) result in placement in either Independent Living or Home settings (82.7%). This clearly contrasts with episodes that end with IRTC and STGH stays, where only just over half are stepped down to a Home or another less restrictive treatment setting. There is also an elevated risk for youth departing from the IRTC to be stepped up to a more restrictive intensive treatment or corrections setting.
A similar tendency was shown when the departure placements for the 6 most common patterns of movement are compared. There was a significant difference between the 6 most common patterns for the number of youth departing to IL/SIL and Home settings versus all other placements; χ2 (5)=128.8, p<.0001. Specifically, standardized residuals indicated that the number of youth departing to IL/SIL and Home settings from the 1st (TFH) and 2nd (STGH–TFH) patterns was significantly higher than expected. This contrasts with youth from the 3rd (IRTC–STGH) and 5th (IRTC) patterns, where significantly higher numbers of youth departed to all other placement types (i.e., foster care through corrections).
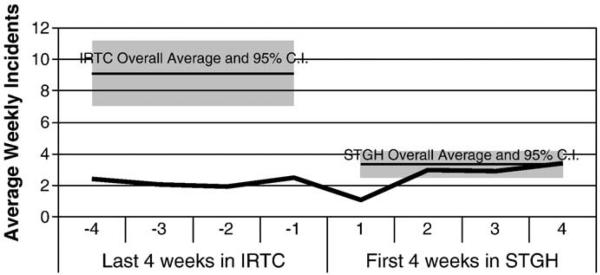
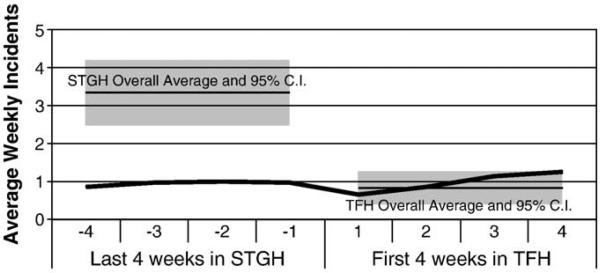
Patterns of movement are instructive, but are the transitions between programs related to changes in problem behavior? We used the Behavioral Index to examine problems for youth who moved from the IRTC to the STGH, or from the STGH to the TFH. Fig. 2 shows the Behavioral Index data for all youth who stepped down from the IRTC to the STGH at any point during an episode of care. Similarly, Fig. 3 shows the Behavioral Index data for youth who stepped down from the STGH to the TFH program at any point during an episode of care. As can be seen in these figures, prior to stepping down to a new program, youths’ Behavioral Index behaviors were far below the norm for youth in their current program and tended to fall within, or even a little lower than, the norm for youth within the program to which they would be transitioning. These figures also show that, at least in terms of the Behavioral Index, the IRTC, STGH, and TFH consist of unique populations, with clear non-overlapping differences between the Behavioral Index distributions for each program.
Fig. 2.
Behavior rate for those youth stepping down from IRTC to STGH (n=192).
Fig. 3.
Behavior rate for those youth stepping down from STGH to TFH (n=184).
A repeated measures ANOVA was used to compare the Behavioral Index for the last four weeks in the more intensive program with the first four weeks in the next program for youth stepping down from one level of care to another. There was a significant difference between these two periods for the IRTC to STGH transition, but non-significant for the STGH to TFH transition. The Behavioral Index increased from M=2.12 to M=3.39 for youth transitioning from the IRTC to the STGH; F (1, 103)=8.0, p<.01. The Behavioral Index also increased slightly from M=1.04 to M=1.13 for youth transitioning from the STGH to the TFH (n.s.).
Of interest, there was a significant Sex by transition interaction for both the IRTC–STGH and STGH–TFH stepdowns; F (1, 103)=9.79, p<.01, and F (1, 121)=5.3, p<.05 respectively. In both cases the Behavioral Index increased for girls while it decreased for boys during the transition. For the IRTC–STGH transition, the Behavioral Index increased from M=1.69 to M=4.36 for girls while it decreased from M=2.55 to M=2.42 for boys. For the STGH–TFH transition, the increase was M=.85 to M=1.47 for girls and the decrease M=1.22 to M=.78 for boys.
In response to the issue of whether youth who stepped down from one program to the next were always at a lower level of problem behavior, a repeated measures ANOVA was used to compare the Behavioral Index for the first four weeks in the IRTC with the last four weeks in the IRTC for youth transitioning to the STGH. There was a significant reduction in the Behavioral Index, with the average number of problem behavior types per week for the four-week periods going from M=8.25 to M=2.12; F (1, 103)=46.3, p<.001. There was a similar reduction in the Behavioral Index for youth transitioning from the STGH to the TFH, with the number of problem behaviors decreasing from M=1.69 to M=1.04; F (1, 121)=7.4, p<.01.
4. Discussion
Findings from this study show that the vast majority of youth who entered this residentially-based continuum of care either remained in a stable placement in the least restrictive of the settings, or followed a pattern of placements that systematically moved them from more restrictive to less restrictive settings. Overall, this movement corresponded with improvements in behavior functioning. Findings suggest that the service continuum functions as it was designed to; that is, 1) most youth are either stable in the least restrictive of the residential settings or stepping down from more restrictive to less restrictive programs; 2) the transitions from more restrictive to less restrictive programs correspond to deescalating levels of problem behavior; 3) at the time of departure from the residential continuum over 80% of the youth were stepped down to either family-based or independent living situations, which is the explicit objective of the overall program.
We further found that the Behavioral Index significantly differentiated between children in the various programs, with children with higher levels of behavioral problems being placed into more restrictive programs. This supports the need for different levels of treatment intensity for youth with varying levels of problems. The commensurate reduction of behavioral problems and level of restrictiveness further suggests that the continuum played a role in the improvement of these youth over time.
Findings from this study support the value of intensive and restrictive residential settings of varying degrees. The needs of some youth require more intensive treatment that may not be able to occur at lower level settings (Ainsworth, 2001). As such, the current stance of viewing all forms of group or residential care as “failure options” (Lieberman, 2004) may prevent some youth from receiving intensive treatment they need in order to meet their treatment needs. While the growing availability of alternative community-based and evidence-based treatments, such as Multidimensional Treatment Foster Care or Multisystemic Treatment are encouraging and should be supported, their implementation and adaptation into real world service systems remains an issue of investigation (Chamberlain et al., 2008; Schoenwald, Heiblum, Saldana, & Henggeler, 2008). The continued high utilization of group home and residential services compared to treatment foster care programs (most of which do not utilize the evidence-based MTFC model; James et al., 2006), might be an indication that the availability of alternative treatments is limited. Additionally, the finding that foster care parents are often ill equipped to meet the needs of more troubled youth (Ainsworth & Hansen, 2005), is also consistent with the continuing need for residential care programs for this population.
The majority of episodes that ended with a TFH stay (regardless of the pattern) resulted in placement in either Independent Living or Home settings (82.7%). This clearly contrasts with episodes that end with IRTC and STGH stays, where only just over half are stepped down to a home or another less restrictive treatment setting. There was also an elevated risk for a small number of youth departing from the IRTC to be stepped up to a more restrictive intensive treatment or corrections setting. This highlights the degree to which these youth are troubled and the challenges inherent in preparing them for less restrictive settings. Conversely, the low percentage of IRTC and STGH youth who transition back to home settings is consistent with the notion that the more troubled youth in these programs need an intermediary program before they are ready for less restrictive community-based type programs. It is also possible that youth who departed from the IRTC or STGH may not have had family members available for reunification. The relationship between the availability of family on actual reunification rates is a question that will have to be answered in future research.
There were significant sex by transition interactions for both the IRTC–STGH and STGH–TFH stepdowns. In both cases behavioral problems increased for girls while they decreased for boys during the transition. It is unclear why this should be the case, but one possibility is that the girls were more troubled by the placement disruption caused by the transition than were the boys. Some previous research has noted that in some out-of-home programs girls demonstrate higher levels of symptomatology and problem behavior at the time of admission (Connor, Doerfler, Toscano, Volungis, & Steingard, 2004; Handwerk et al., 2006; Weiss et al., 2005). A common explanation for this finding is that perhaps there is less willingness to place troubled girls in out-of-home treatment settings than there is for boys, and the threshold for behavior problems might be higher for girls to be considered for this type of placement. Perhaps the increase in girls’ disruptive behavior during program transition seen in this study indicates that placement disruption itself plays a role in these initially higher levels of symptomatology and problem behavior for girls.
It needs to be noted that in this study unlike many other service systems, a tremendous amount of continuity between the three programs exists because the underlying therapeutic model is the same for all three residential programs. This continuity may contribute to youth being able to move successfully from one program to the next with greater ease and therefore less disruption. This is a very important point: the disconnectedness of group homes from the regular service systems is perhaps one reason that this result has not be found in other systems (e.g., Bickman, Lambert, Andrade, & Penaloza, 2000). In contrast, the current study examined an integrated program with exceptional continuity between individual treatment programs. This integration likely allows the continuum to operate in a more functional manner, but the ultimate transition out of the continuum may not work as well if a similar level of coordination is not continued into aftercare. There is an increasing awareness of the important role aftercare plays in helping youth maintain treatment gains (Altschuler & Brash, 2004; Courtney et al., 2005; Trout et al., 2010).
The program also utilizes one of the few treatment models relevant to residential care (Teaching Family Model) that is considered to have a promising evidence base (Dodge, Dishion, & Lansford, 2006; Lipsey, 1999). TFM is manualized and well specified, and at this residential campus is tested for implementation fidelity across programs. In comparison, very little is generally known about usual care treatment models used in many residentially-based programs. There is evidence that many programs integrate behavioral components, but to date, there are few treatment models relevant for residential care that meet any standard of being evidence-based. The future challenge for residential care providers will be to build an evidence base about effective treatment models in group and residential care and to determine which children may indeed benefit from residential and other treatment services. Rigorous trials to test the effectiveness of these services are needed involving methods other than random assignment. Random assignment into group and residential settings is seldom feasible, and there is evidence that process and context variables may be powerful predictors of successful outcomes in group and residential treatment (Whittaker, 2004). Residential care providers are in a unique position to partner with academic researchers and funding agencies to contribute to the knowledge base about the implementation and outcome of services provided to children with mental health problems (Whittaker et al., 2006).
4.1. Study limitations
The differences in the DSM diagnoses rates (Table 1) and the average levels of disruptive behavior shown in the Behavioral Index (Figs. 2 and 3) give some indication of the initial differences for the youth in each of the residential programs. Each of the programs is designed to respond to different levels of disruptive behavior, so the evident selection process is quite appropriate. But there were also differences in race and gender proportions for each program that are not addressed by the data reported here. It is unclear at this point what might explain this disproportionality. Future studies should also determine how these differences might have impacted the findings.
Findings of this study might not be generalizable to other residential programs given the unique characteristics of the overall programs and continuum as previously described. The study also did not examine youth who do not follow the general pattern (i.e., demonstrated increasing behavioral problems), step up through the continuum, and ultimately experience an unsuccessful departure. Future analyses should examine whether these youth could be identified early and either provided with additional needed care or placed in a treatment setting more appropriate to meeting their needs. Finally, all patterns of movement studies have the inherent limitation that they ultimately provide little information about specific interventions and quality of services provided. Much more needs to be known about what youth experience individually as they experience treatment within the continuum.
5. Conclusion
The results of this study have several practical implications. The data reported here are the same data that are used by clinical staff in treatment planning and determining readiness for transitioning to a lower level of care. We argue in favor of using clinically relevant, real-time data in clinical decision making, as opposed to non-clinical factors (e.g., benefits running out, legislative mandate, etc.). Further, the clear differences in the levels of problem behavior for each of the programs, and the ability of these programs to ameliorate the problems, are consistent with keeping more intensive treatment settings available within an integrated continuum. The more restrictive levels of care allow youth with high levels of disruptive behavior to get the treatment intensity they need to improve. Finally, placement disruption often results in unfavorable outcomes for youth (Leathers, 2006; Price et al., 2008). The stability and systematic stepdown patterns seen in this study appear to successfully prepare youth for less restrictive levels of care, inclusive of returning back to home settings. A highly integrated continuum of care for troubled youth may thus minimize the extent of disruptive changes experienced by so many youth in out-of-home care.
Despite limitations, this study supports the notion that a continuum of intensive services with varying degrees of restrictiveness can serve the needs of youth with significant emotional and behavioral disorders. The continuity between individual programs and the use of a strong treatment model add to the strength of the overall program and are perhaps the primary reason that this system of care functions in a rational way for the majority of youth.
Footnotes
There is a specific program in the IRTC designed for children as young as 6-year-old, but there is no program that they can transition to within this residential system of care.
References
- Ainsworth F. After ideology: The effectiveness of residential programs for “at risk” adolescents. Children Australia. 2001;26:11–18. [Google Scholar]
- Ainsworth F, Hansen P. A dream come true – no more residential care: A corrective note. International Journal of Social Welfare. 2005;14:195–199. [Google Scholar]
- Altschuler DM, Brash R. Adolescent and teenage offenders confronting the challenges and opportunities of reentry. Youth Violence and Juvenile Justice. 2004;2:72–87. [Google Scholar]
- Barth RP. Institutions vs. foster homes: The empirical base for the second century of debate. Annie E. Casey Foundation, University of North Carolina, School of Social Work, Jordan Institute for Families; Chapel Hill, NC: 2002. [Google Scholar]
- Barth RP, Courtney M, Berrick JD, Albert V. From child abuse to permanency planning: Child welfare services pathways and placements. Aldine de Gruyter; Hawthorne: 1994. [Google Scholar]
- Benedict MI, Zuravin S, Stallings RY. Adult functioning of children who lived in kin versus nonrelative family foster homes. Child Welfare Journal. 1996;75:529–549. [PubMed] [Google Scholar]
- Bickman L, Lambert EW, Andrade AR, Penaloza RV. The Fort Bragg continuum of care for children and adolescents: Mental health outcomes over 5 years. Journal of Consulting & Clinical Psychology. 2000;68:710–716. [PubMed] [Google Scholar]
- Breland-Noble AM, Elbogen EB, Farmer EMZ, Dubs MS, Wagner HR, Burns BJ. Use of psychotropic medications by youths in therapeutic foster care and group homes. Psychiatric Services. 2004;55:706–708. doi: 10.1176/appi.ps.55.6.706. [DOI] [PubMed] [Google Scholar]
- Breland-Noble AM, Farmer EMZ, Dubs MS, Potter E, Burns BJ. Mental health and other service use by youth in therapeutic foster care and group homes. Journal of Child & Family Studies. 2005;14:167–180. [Google Scholar]
- Burchard JD, Bruns EJ, Burchard SN. The wraparound approach. In: Burns BJ, Hoagwood K, editors. Community treatment for youth: Evidence-based interventions for severe emotional and behavioral disorders. Oxford University Press; New York: 2002. pp. 69–91. [Google Scholar]
- Burns BJ, Hoagwood K, Mrazek PJ. Effective treatment for mental disorders in children and adolescents. Clinical Child & Family Psychology Review. 1999;2:199–254. doi: 10.1023/a:1021826216025. [DOI] [PubMed] [Google Scholar]
- Butler LS, McPherson PM. Is residential treatment misunderstood? Journal of Child and Family Studies. 2007;16:465–472. [Google Scholar]
- Chamberlain P. Treatment foster care. U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; Washington DC: 1998. [Google Scholar]
- Chamberlain P, Brown CH, Saldana L, Reid J, Wang W, Marsenich L, et al. Engaging and recruiting counties in an experiment on implementing evidence-based practice in California. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35:250–260. doi: 10.1007/s10488-008-0167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain P, Reid JB. Parent observation and report of child symptoms. Behavioral Assessment. 1987;9:97–109. [Google Scholar]
- Connell CM, Vanderploeg JJ, Flaspohler P, Katz KH, Saunders L, Tebes JK. Changes in placement among children in foster care: A longitudinal study of child and case influences. Social Service Review. 2006;80:398–418. doi: 10.1086/505554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor DF, Doerfler LA, Toscano PF, Volungis AM, Steingard RJ. Characteristics of children and adolescents admitted to a residential treatment center. Journal of Child and Family Studies. 2004;13:497–510. [Google Scholar]
- Courtney ME, Dworsky A, Ruth G, Keller T, Havlicek J, Bost N. Midwest evaluation of the adult functioning of former foster youth: Outcomes at age 19. Chapin Hall Center for Children; Chicago IL: 2005. [Google Scholar]
- Davidson-Arad B. Fifteen-month follow-up of children at risk: Comparison of the quality of life of children removed from home and children remaining at home. Children and Youth Services Review. 2005;27:1–20. [Google Scholar]
- Davis J, Daly DL. 4th ed. Father Flanagan's Boys’ Home; Boys Town, NE: 2003. Girls and Boys Town long-term residential program: Training manual. [Google Scholar]
- Dishion TJ, Dodge KA, Lansford JE. Deviant by design: Risks associated with aggregating deviant peers into group prevention and treatment programs. The Prevention Researcher. 2008;15:8–11. [Google Scholar]
- Dodge KA. Professionalizing the practice of public policy in the prevention of violence. Journal of Abnormal Child Psychology. 2006;34:475–479. doi: 10.1007/s10802-006-9040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Dishion TJ, Lansford JE. Deviant peer influences in intervention and public policy for youth. Social Policy Report. 2006;20:3–19. [Google Scholar]
- Dore MM. Emotionally and behaviorally disturbed children in the child welfare system: Points of preventive intervention. Children and Youth Services Review. 1999;21:7–29. [Google Scholar]
- Farmer EMZ, Wagner HR, Burns BJ, Richards JT. Treatment foster care in a system of care: Sequences and correlates of residential placements. Journal of Child and Family Studies. 2003;12:11–25. [Google Scholar]
- Fields SA, Ogles BM. The system of care for children and the least restrictive alternative: Legal origins and current concerns. Children's Services: Social Policy, Research, & Practice. 2002;5:75–93. [Google Scholar]
- Fields SA, Ogles BM. An empirical typology of youth with severe emotional disturbances. American Journal of Orthopsychiatry. 2004;72:250–261. doi: 10.1037/0002-9432.72.2.250. [DOI] [PubMed] [Google Scholar]
- Garland AF, Hough RL, Landsverk JA, Brown SA. Multi-sector complexity of systems of care for youth with mental health needs. Children's Services: Social Policy, Research, & Practice. 2001;4:123–140. [Google Scholar]
- Geller JL, Biebel K. The premature demise of public child and adolescent inpatient psychiatric beds: Part I: Overview and current conditions. Psychiatric Quarterly. 2006;77:251–271. doi: 10.1007/s11126-006-9012-0. [DOI] [PubMed] [Google Scholar]
- Handwerk ML, Clopton K, Huefner JC, Smith GL, Hoff KE, Lucas CP. Gender differences in adolescents in residential treatment. American Journal of Orthopsychiatry. 2006;76:312–324. doi: 10.1037/0002-9432.76.3.312. [DOI] [PubMed] [Google Scholar]
- Handwerk ML, Friman PC, Mott MA, Stairs JM. The relationship between program restrictiveness and youth behavior problems. Journal of Emotional & Behavioral Disorders. 1998;6:170–179. [Google Scholar]
- Henggeler SW, Schoenwald SK, Borduin CM, Rowland MD, Cunningham PB. Multisystemic treatment of antisocial behavior in children and adolescents. Guilford Press; New York, NY: 1998. [Google Scholar]
- Hurlburt MS, Leslie LK, Landsverk J, Barth RP, Burns BJ, Gibbons RD, et al. Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry. 2004;61:1217–1224. doi: 10.1001/archpsyc.61.12.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglehart AP. Adolescents in foster care: Predicting readiness for independent living. Children & Youth Services Review. 1994;16:159–169. [Google Scholar]
- James S. Why do foster care placements disrupt? An investigation of reasons for placement change in foster care. Social Service Review. 2004;78:601–627. [Google Scholar]
- James S, Landsverk J, Slymen DJ. Placement movement in out-of-home care: Patterns and predictors. Children and Youth Services Review. 2004;26:185–206. [Google Scholar]
- James S, Leslie LK, Hurlburt MS, Slymen DJ, Landsverk J, Davis I, et al. Children in out-of-home care: Entry into intensive or restrictive mental health and residential care placements. Journal of Emotional & Behavioral Disorders. 2006;14:196–208. [Google Scholar]
- Leathers SJ. Placement disruption and negative placement outcomes among adolescents in long-term foster care: The role of behavior problems. Child Abuse & Neglect. 2006;30:307–324. doi: 10.1016/j.chiabu.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Lewis EE, Dozier M, Ackerman J, Sepulveda-Kozakowski S. The effect of placement instability on adopted children's inhibitory control abilities and oppositional behavior. Developmental Psychology. 2007;43:1415–1427. doi: 10.1037/0012-1649.43.6.1415. [DOI] [PubMed] [Google Scholar]
- Lieberman RE. Future directions in residential treatment. Child and Adolescent Psychiatric Clinics of North America. 2004;13:279–294. doi: 10.1016/S1056-4993(03)00118-4. [DOI] [PubMed] [Google Scholar]
- Lipsey MW. Can intervention rehabilitate serious delinquents? Annals of the American Academy of Political & Social Science(s) 1999;564:142–199. [Google Scholar]
- Lyons JS, Libman-Mintzer LN, Kisiel CL, Shallcross H. Understanding the mental health needs of children and adolescents in residential treatment. Professional Psychology: Research & Practice. 1998;29:582–587. [Google Scholar]
- McCurdy BL, Mclntyre EK. ‘And what about residential...?’ Re-conceptualizing residential treatment as a stop-gap service for youth with emotional and behavioral disorders. Behavioral Interventions. 2004;19:137–158. [Google Scholar]
- McMillen JC, Scott LD, Zima BT, Ollie MT, Munson MR, Spitznagel E. Use of mental health services among older youths in foster care. Psychiatric Services. 2004;55:811–817. doi: 10.1176/appi.ps.55.7.811. [DOI] [PubMed] [Google Scholar]
- Nash JK, Thompson S, Kim JS. Residential trajectories of participants in North Carolina's Willie-M. Program: A semi-parametric group based model. Journal of Social Service Research. 2006;33:53–68. [Google Scholar]
- Oosterman M, Schuengel C, Slot NW, Bullens RAR, Doreleijers TAH. Disruptions in foster care: A review and meta-analysis. Children and Youth Services Review. 2007;29:53–76. [Google Scholar]
- Patterson GR, Reid JB, Jones RR, Conger RE. A social learning approach to family intervention. I. Castalia Publishing; Eugene, OR: 1975. [Google Scholar]
- Pottick KJ, Warner LA, Yoder KA. Youths living away from families in the US mental health system: Opportunities for targeted intervention. Journal of Behavioral Health Services & Research. 2005;32:264–281. doi: 10.1007/BF02291827. [DOI] [PubMed] [Google Scholar]
- Preyde M, Adams G, Cameron G, Frensch K. Outcomes of children participating in mental health residential and intensive family services: Preliminary findings. Residential Treatment for Children & Youth. 2009;26:1–20. [Google Scholar]
- Price JM, Chamberlain P, Landsverk J, Reid JB, Leve LD, Laurent H. Effects of a foster parent training intervention on placement changes of children in foster care. Child Maltreatment. 2008;13:64–75. doi: 10.1177/1077559507310612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenwald SK, Heiblum N, Saldana L, Henggeler SW. The international implementation of multisystemic therapy. Evaluation & the Health Professions. 2008;31:211–225. doi: 10.1177/0163278708315925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Stormshak E, Chamberlain P, Bridges Whaley R. Placement disruption in treatment foster care. Journal of Emotional & Behavioral Disorders. 2001;9:200–205. [Google Scholar]
- Staff I, Fein E. Stability and change: Initial findings in a study of treatment foster care placements. Children & Youth Services Review. 1995;17:379–389. [Google Scholar]
- Trout AL, Chmelka MB, Thompson RW, Epstein MH, Tyler P, Pick R. The departure status of youth from residential group care: Implications for aftercare. Journal of Child & Family Studies. 2010;19:67–78. [Google Scholar]
- Usher CL, Randolph KA, Gogan HC. Placement patterns in foster care. Social Service Review. 1999;73:22–36. [Google Scholar]
- Webster D, Barth RP, Needell B. Placement stability for chldren in out-of-home care: A longitudinal analysis. Child Welfare. 2000;79:614–632. [PubMed] [Google Scholar]
- Weiner DA, Abraham ME, Lyons J. Clinical characteristics of youths with substance use problems and implications for residential treatment. Psychiatric Services. 2001;52:793–799. doi: 10.1176/appi.ps.52.6.793. [DOI] [PubMed] [Google Scholar]
- Weiss B, Caron A, Ball S, Tapp J, Johnson M, Weisz JR. Iatrogenic effects of group treatment for antisocial youths. Journal of Consulting and Clinical Psychology. 2005;73:1036–1044. doi: 10.1037/0022-006X.73.6.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittaker JK. The re-invention of residential treatment: An agenda for research and practice. Child & Adolescent Psychiatric Clinics of North America. 2004;13:267–278. doi: 10.1016/S1056-4993(03)00117-2. [DOI] [PubMed] [Google Scholar]
- Whittaker JK, Greene K, Schubert D, Blum R, Cheng K, Blum K, et al. Integrating evidence-based practice in the child mental health agency: A template for clinical and organizational change. American Journal of Orthopsychiatry. 2006;76:194–201. doi: 10.1037/0002-9432.76.2.194. [DOI] [PubMed] [Google Scholar]
- Wolf MM, Phillips EL, Fixsen DL, Braukmann CJ, Kirigin KA, Willner AG, et al. Achievement place: The teaching-family model. Child Care Quarterly. 1976;5:92–103. [Google Scholar]
- Wulczyn F, Kogan J, Harden BJ. Placement stability and movement trajectories. Social Service Review. 2003;77:212–236. [Google Scholar]