Abstract
Annona genus contains plants used in folk medicine for the treatment of diabetes. In the present study, an aqueous extract prepared from Annona macroprophyllata (Annonaceae, also known as A. diversifolia) leaves was evaluated on both the activity of yeast α-glucosidase (an in vitro assay) and sucrose tolerance in Wistar rats. The results have shown that the aqueous extract from A. macroprophyllata inhibits the yeast α-glucosidase with an IC50 = 1.18 mg/mL, in a competitive manner with a K i = 0.97 mg/mL, a similar value to that of acarbose (K i = 0.79 mg/mL). The inhibitory activity of A. macroprophyllata was reinforced by its antihyperglycemic effect, at doses of 100, 300, and 500 mg/kg in rats. Chromatographic analysis identified the flavonoids rutin and isoquercitrin in the most polar fractions of A. macroprophyllata crude extract, suggesting that these flavonoids are part of the active constituents in the plant. Our results support the use of A. macroprophyllata in Mexican folk medicine to control postprandial glycemia in people with diabetes mellitus, involving active constituents of flavonoid nature.
1. Introduction
Diabetes mellitus (DM) is a chronic disease associated with abnormal and constant high blood glucose (hyperglycemia) that results from defects in insulin secretion, action, or both. In type 2 diabetes mellitus (DM2), postprandial hyperglycemia is important in the development of the disease; it is associated with micro- and macrovascular complications, and it has been proposed as an independent risk factor for cardiovascular disease [1, 2]. The postprandial phase is characterized by a rapid and increased glycemia. These postprandial “hyperglycemic spikes” may be relevant to the pathophysiological conditions of late diabetes [3, 4].
One important factor that arises in postprandial hyperglycemia is the fast uptake of glucose in the intestine, in which α-glucosidases hydrolyze starch and oligosaccharides [5]. The α-glucosidases, exoglycosidases, found in the luminal surface of enterocytes contain maltase/glucoamylase and sucrose/isomaltase activities [6]. It is believed that inhibition of these enzymes can effectively control the postprandial elevation of blood glucose. Therefore, an important strategy for managing postprandial hyperglycemia is to inhibit α-glucosidase activity [7]. The α-glucosidase inhibitors, such as acarbose, have been used in the clinic to control blood glucose increase, especially postprandial, in DM2 [8]; these chemical drugs have strong inhibitory activity against α-glucosidases but have the disadvantage of undesirable side effects such as abdominal distention, flatulence, meteorism, and diarrhea [9]. Previous research indicates that side effects could be caused by excessive inhibition of pancreatic α-amylase, resulting in the abnormal bacterial fermentation of undigested carbohydrates in the colon. Therefore, more effective inhibitors for the enzymes should have strong inhibitory effect against α-glucosidase and mild inhibitory effect against α-amylase, which can be an effective therapy for managing postprandial hyperglycemia with minimal side effects [10].
Annonaceae is a family of plants consisting of 2300 to 2500 species included in more than 130 genera; in fact, it is the largest family of the order Magnoliales. Only four genera (Annona, Rollinia, Uvaria, and Asimina) produce edible fruits such as annona [11–13]. Annona macroprophyllata Donn. Sm. is a species belonging to the Annona genus; it is a common tree in central México known as “ilama” (States of Colima, Guerrero, and México); whereas in the southeast (Tehuantepec region and Yucatán) it is called “papauce” or “anona blanca” [14, 15]. The fruits of this plant are used as food, but its leaves are employed as anticonvulsant [16], as well as analgesic and anti-inflammatory agents in traditional Mexican medicine [17]. However, so far there are no scientific reports supporting its probable antihyperglycemic properties, even though other species of the genus are known to have those properties, that is, Annona squamosa, A. muricata, A. glabra, and A. cherimola [18–20]; then we have used a chemotaxonomic criterion in order that A. macroprophyllata, besides its described medicinal properties [14–17], was investigated to search for its likely antidiabetic properties.
2. Materials and Methods
2.1. Plant Material and Extract
Annona macroprophyllata Donn. Sm. specimens were collected in Tejupilco, Guerrero in September 2010. Dr. E. Cedillo-Portugal, botanist from the Universidad Autónoma de Chapingo (UACH), certified the authenticity of the plant, and a voucher specimen (AN9702) was deposited in the herbarium “Herbario de Plantas Útiles Efraím Hernández X” at the UACH, in the State of México, México, for future reference. Aqueous extract was obtained by using 50 g of dried and powdered leaves, in a process of infusion in 500 mL of boiling water. The aqueous extract was separated from the residues by gravity filtration; samples were frozen in liquid nitrogen and then lyophilized during 12 h using a Heto FD3 Lab lyophilizer to yield 1.11 g (2.22%).
2.2. HPLC Quantification of Flavonoids
An HPLC analysis was performed using an Agilent Technologies Chromatograph. The separation was performed on an ODS Hypersil C18 column (15 mm × 4 mm i.d. and 5 μm particle size). The samples were injected through a 20 μL loop. The column was thermostatically controlled at 30°C using a 1 mL/min flow rate. The mobile phase consisted of 15 : 85 acetonitrile-trifluoroacetic acid solution at pH 2.5. The detection was monitored at 350 nm wavelength, and the system was run for 15 min. Calibration curves were done for the standards: kaempferol, hesperidin, naringenin, naringin, rutin, isoquercitrin, and quercetin.
2.3. α-Glucosidase Assay In Vitro
α-Glucosidase inhibition was measured at pH 7.0 and 30°C using p-nitrophenyl-α-D-glucopyranoside (pNPG) as substrate and 0.75 IU/mL of yeast α-glucosidase in 0.1 M sodium phosphate buffer. Acarbose and aqueous extract were dissolved in phosphate buffer, and serial dilutions from 1.4 to 0.2 mg/mL were prepared. The increments in absorption at 405 nm, due to the hydrolysis of pNPG by the α-glucosidase, were determined on a microplate reader DTX 880 Multimode Detector from Beckman Coulter. Ten μL of acarbose or extract solution (in triplicate) were incubated during 5 min with 20 μL of enzyme stock. After incubation, 10 μL of substrate were added and further incubated for 35 min at 30°C. Finally, the reaction was stopped by adding 30 μL of 5 M Na2CO3. The concentration required to inhibit the enzyme activity by 50% (IC50) was calculated by regression analysis, using the following equation:
| (1) |
where v is the percentage of inhibition, A 100 is the maximum inhibition, I is the inhibitor concentration, IC50 is the concentration required to inhibit the enzyme activity by 50%, and s is the cooperative degree.
2.4. Enzyme Kinetics
The mode of inhibition for α-glucosidase was determined by the Lineweaver-Burk plots. All the results are expressed as the mean of at least three experiments ± SEM. Kinetic parameters such as V m, K m, and K i were evaluated by using the nonlinear regression method, based on the following inhibition equation:
| (2) |
where v is the initial velocity in either the Presence or absence of the inhibitor S and I are the concentrations of substrate and inhibitor, respectively; V m is the maximum velocity, K m is the Michaelis-Menten constant, K i is the competitive inhibition constant, and K i′ is the uncompetitive inhibition constant. The kinetic data were analyzed using a computer program for nonlinear regressions (Origin 8.0).
2.5. Experimental Animals
Male Wistar normoglycemic rats, weighing 200–250 g, were obtained from our animal facilities at Facultad de Estudios Superiores Iztacala, U.N.A.M. Procedures involving animals and their care fulfilled the Mexican Official Norm for Animal Care and Handling (NOM-062-ZOO-1999) and were in compliance with international rules on care and use of laboratory animals. Furthermore, clearance for conducting the studies was obtained from the Ethics Committee for the Use of Animals in Pharmacological and Toxicological Testing of Facultad de Estudios Superiores Iztacala, U.N.A.M. For the pharmacological studies, groups of four animals were used. All doses are in mg/kg of body weight. The rats were housed in groups of four under standard laboratory conditions (12 h light/dark cycle at 22 ± 1°C) and maintained on a standard pellet diet and water ad libitum.
2.6. Preparation of the Test Samples and Determination of Glycemia
All aqueous administrations were suspended in 0.9% saline solution and given by intragastrical route. Acarbose (Sigma-Aldrich Co., St. Louis, MO, USA) was used as antihyperglycemic drug. Sucrose (Reasol, Reactivos Analíticos, México) was used as carbohydrate to carry out the sucrose tolerance tests. The control rats received only vehicle (saline solution) in the same volume (0.5 mL of vehicle/100 g of body weight) by the same route. Blood samples were collected from the caudal vein by performing a small incision at the end of the tail. Blood glucose (mg/dL) was estimated using a commercial glucometer (Accu-Chek sensor, Roche, Mannheim, Germany). The variation of glycemia as percentage for each group was calculated with respect to the initial (0 h) level, according to the following equation:
| (3) |
where G i is the initial glycemia values and G t is the glycemia value after treatments administration [21].
2.7. Oral Sucrose Tolerance Test (OSTT)
Rats were fasted during 12 h before the experiment having free access to water. The crude extract of A. macroprophyllata was tested at the doses of 100, 300, and 500 mg/kg. Acarbose (5 mg/kg) was suspended in the same vehicle. Time 0 min was set before treatment with the extract; 30 min later a sucrose load (3 g/kg) was administered to the rats. Blood samples were obtained 15, 30, 60, 90, and 120 min after the carbohydrate load [21].
2.8. Statistical Analysis
Data represent the mean ± SEM of n = 4 rats for the OSTT and n = 3 assays for in vitro experiments. Differences were analyzed using Student's t-test (Sigma Stat version 3.0), and significant differences were considered at P < 0.05.
3. Results and Discussion
In México, it has been reported the use of A. muricata, A. glabra, and A. cherimola as antidiabetic species [18], which suggested to us that A. macroprophyllata is an interesting species to study, since it may have the same metabolic pathways that synthesize the compounds as the other members of the genus and thus may show their therapeutic properties. That is, we tested a chemotaxonomic criterion for the study.
Elution of A. macroprophyllata leaves aqueous extract yielded rutin (2.88 μg/mg of crude extract; RT 3.973 min) and isoquercitrin (0.71 μg/mg of crude extract; RT 6.872), as well as some traces of astragalin/isoquercitrin (0.03 μg/mg of crude extract) (Figure 1).
Figure 1.
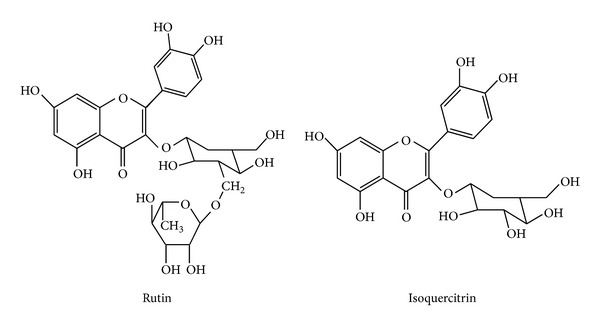
Structure of flavonoids rutin and isoquercitrin.
Annona macroprophyllata ethanolic extract has been investigated as antinociceptive, anti-inflammatory, and anticonvulsant agents [15–17]; however, the species has not been tested for antidiabetic actions, as their counterparts have done [19, 20, 22–25]. Our study found rutin as one of its components, as well as isoquercitrin; these two flavonoids, along with quercetin, have been tested on diabetic rats, that is, rutin decreased fasting plasma glucose, increased insulin levels, and improved the antioxidant status by decreasing lipid peroxidative products, and increasing enzymic and nonenzymic antioxidants [26]. Rutin has been associated with marked decrease of hepatic and cardiac levels of triglycerides and elevated glycogen which suggest that rutin can improve hyperglycemia and dyslipidemia, while inhibiting the progression of liver and heart dysfunction in STZ-induced diabetic rats [27], and rutin has hypoglycemic effect in normal and diabetic rats [28–30]. Rutin metabolites are capable of inhibiting α-glucosidase activity both in vivo and in vitro [31], and the formation of advanced glycation end products, formed via protein glycation which correlates with aging and diabetes complications [32].
To our knowledge, this is the first report that the aqueous extract from A. macroprophyllata inhibited the activity of yeast α-glucosidase, with a low IC50 (1.18 mg/mL), very similar to that of acarbose (0.27 mg/mL). This result agrees with that reported for rutin as inhibitor of α-glucosidase (IC50 = 0.196 mM), compared with acarbose (IC50 0.091 mM) [33]; therefore rutin might participate in the aqueous extract of A. macroprophyllata on the α-glucosidase inhibition and antihyperglycemic effects.
The next step was to determine the nature of the inhibition exerted by the aqueous extract of A. macroprophyllata, then a kinetic analysis of the inhibition of enzyme activity using different amounts of aqueous extract or acarbose was conducted. The results yielded a K i of 0.97 mg/mL and K i of 0.79 mg/mL to aqueous extract and acarbose, respectively. These values show that the extract inhibited the enzyme and could be used to control postprandial hyperglycemia. Lineweaver-Burk plots for α-glucosidase from yeast, in the presence of acarbose or A. macroprophyllata extract at different concentrations (Figure 2), revealed typical curves for competitive inhibitors implying binding to the catalytic site. Then, we suggest that disaccharidases are targets of flavonoids in the regulation of glucose release and consequently glucose absorption by the gut. This type of inhibitor has several advantages over others; that is, its inhibition is not permanent, and undesirable effects are easily attenuated with decreasing dose; therefore, the aqueous extract of A. macroprophyllata represents a good alternative to avoid hyperglycemia.
Figure 2.
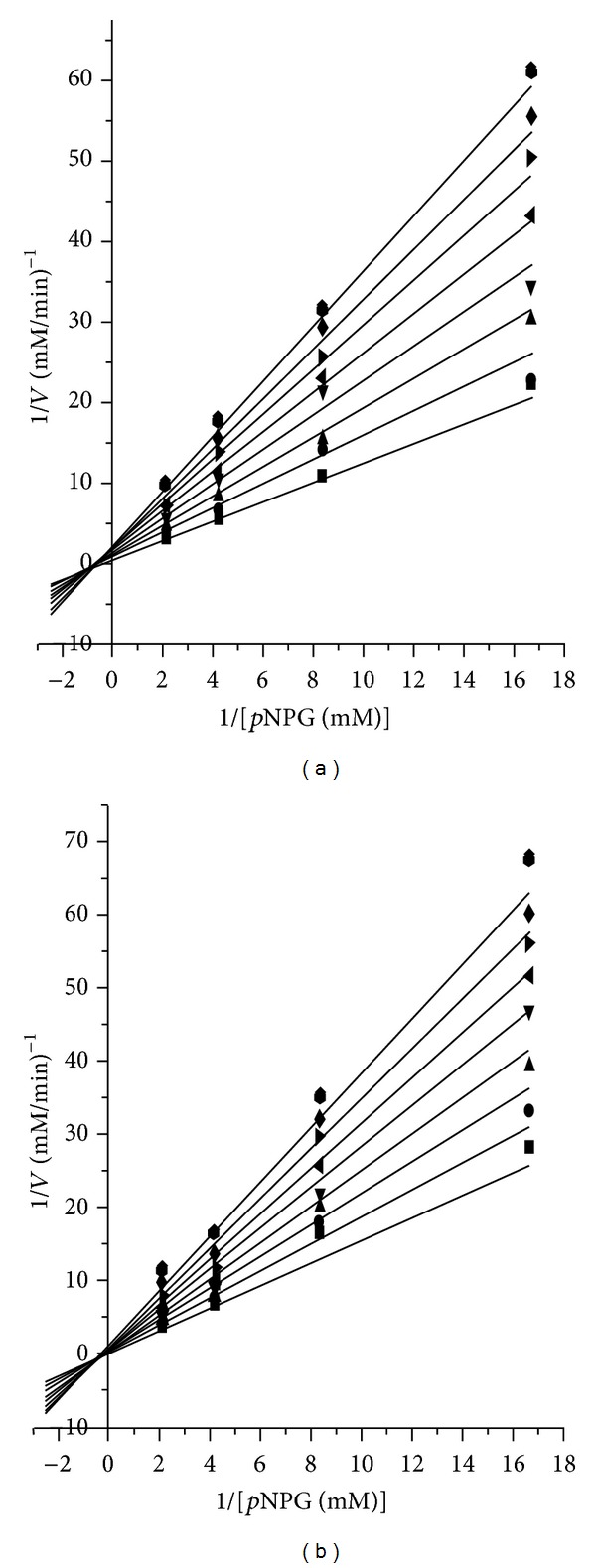
Lineweaver-Burk plots of α-glucosidase inhibition at different concentrations of (a) acarbose and (b) extract aqueous from A. macroprophyllata. 0.0 mg/mL (■), 0.2 mg/mL (⚫), 0.4 mg/mL (▲), 0.6 mg/mL (▼), 0.8 mg/mL (◂), 1.0 mg/mL (▸), 1.2 mg/mL (◆), 1.4 mg/mL (⬢).
On the other hand, to confirm whether our results in vitro could be reproduced in a whole organism, the response on glycemia after single oral sucrose ingestion was examined for A. macroprophyllata. As observed in Figure 3, the test extract significantly avoided the hyperglycemic response, at doses of 100, 300, and 500 mg/kg compared to control (P < 0.05). The postprandial blood glucose peak was diminished from 15 min in all three doses (100, 300, and 500 mg/kg); however, the highest activity was 300 > 500 > 100 mg/kg throughout the time-curve postingestion of sucrose. The glycemic lowering effect of A. macroprophyllata at doses of 100, 300, and 500 mg/kg was not greater than that with acarbose, a therapeutic drug used as positive control (5 mg/kg); however, maximum effect obtained at a dose of 300 mg/kg was not statistically different with acarbose dose from 60 min on, results in vivo that agree to the reported for other species of the genus Annona as is the case of A. squamosa, A. muricata, and A. cherimola, which also show antioxidant, hypoglycemic, antihyperglycemic, and hypolipidemic properties [19, 20, 22–25]. These data support the idea that this species synthesizes similar secondary metabolites that act as antidiabetic, directly by lowering glucose availability in the gut or indirectly by decreasing oxidative stress and/or lipids, attenuating the effect of these two factors in disease. Our results indicate that the control of postprandial glycemia showed by A. macroprophyllata involves an antihyperglycemic effect, mediated by the regulation of glucose uptake from the intestinal lumen, through the inhibition of carbohydrate digestion, putatively by inhibition of intestinal α-glucosidases complex, as observed in vitro for yeast α-glucosidase. In addition, the search for the active principle of the extract could generate a new α-glucosidase inhibitor, useful for the development of new antidiabetic or antiobesity agents.
Figure 3.
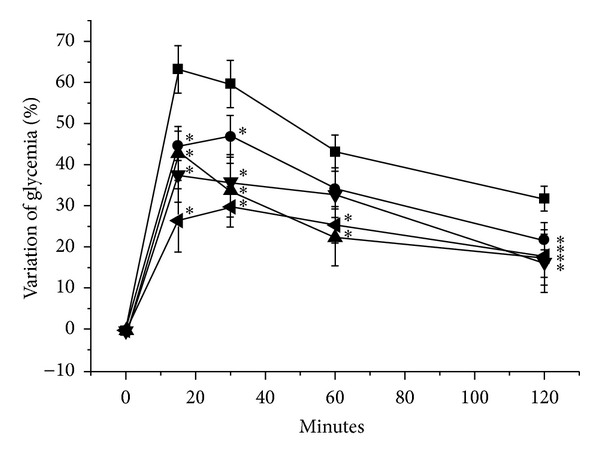
Effects of the crude extract of the leaves of A. macroprophyllata on blood glucose levels in rats on the OSTT. Vehicle (■), acarbose 5 mg/kg (◂), extract A. macroprophyllata 100 mg/kg (⚫), extract A. macroprophyllata 300 mg/kg (▲), and extract A. macroprophyllata 500 mg/kg (▼). Each value is the mean ± SEM for 4 rats in each group. *P < 0.05 is significantly different. t-test for comparison with respect to negative control values at the same time. Baseline glycemia 77 mg/dL.
In conclusion, our results indicate that A. macroprophyllata aqueous extract has potent antihyperglycemic effect, and according to the in vitro studies it acts as a competitive inhibitor of the α-glucosidase. Last but not least, this study provides scientific support to use A. macroprophyllata leaves in Mexican traditional medicine for the treatment of DM2.
Conflict of Interests
The authors declare no conflict of interests.
Acknowledgments
This work was supported by grants from PAPIIT, DGAPA, U.N.A.M. (IN214812), and INMEGEN (06/2012/l). F. Brindis acknowledges postdoctoral fellowship awarded by DGAPA-U.N.A.M.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Kerner W, Brückel J. Definition, classification, and diagnosis of diabetes mellitus. Diabetologie und Stoffwechsel. 2009;4(2):S115–S117. [Google Scholar]
- 3.Bonora E, Muggeo M. Postprandial blood glucose as a risk factor for cardiovascular disease in type II diabetes: the epidemiological evidence. Diabetologia. 2001;44(12):2107–2114. doi: 10.1007/s001250100020. [DOI] [PubMed] [Google Scholar]
- 4.Ceriello A. Postprandial hyperglycemia and diabetes complications: is it time to treat? Diabetes. 2005;54(1):1–7. doi: 10.2337/diabetes.54.1.1. [DOI] [PubMed] [Google Scholar]
- 5.Quezada-Calvillo R, Robayo-Torres CC, Opekun AR, et al. Contribution of mucosal maltase-glucoamylase activities to mouse small intestinal starch α-glucogenesis. Journal of Nutrition. 2007;137(7):1725–1733. doi: 10.1093/jn/137.7.1725. [DOI] [PubMed] [Google Scholar]
- 6.Krentz AJ, Bailey CJ. Oral antidiabetic agents. Drugs. 2005;65(3):385–411. doi: 10.2165/00003495-200565030-00005. [DOI] [PubMed] [Google Scholar]
- 7.Borges de Melo E, da Silveira Gomes A, Carvalho I. α- and β-glucosidase inhibitors: chemical structure and biological activity. Tetrahedron. 2006;62(44):10277–10302. [Google Scholar]
- 8.Bischoff H, Puls W, Krause HP, Schutt H, Thomas G. Pharmacological properties of the novel glucosidase inhibitors BAY m 1099 (miglitol) and BAY o 1248. Diabetes Research and Clinical Practice. 1985;1:53–62. [Google Scholar]
- 9.Horii A, Emi M, Tomita N, et al. Primary structure of human pancreatic α-amylase gene: its comparison with human salivary α-amylase gene. Gene. 1987;60(1):57–64. doi: 10.1016/0378-1119(87)90213-7. [DOI] [PubMed] [Google Scholar]
- 10.Kwon Y-I, Apostolidis E, Shetty K. In vitro studies of eggplant (Solanum melongena) phenolics as inhibitors of key enzymes relevant for type 2 diabetes and hypertension. Bioresource Technology. 2008;99(8):2981–2988. doi: 10.1016/j.biortech.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 11.Cañizares ZJ. Las Frutas Anonáceas. La Habana, Cuba: Ediciones Fruticus; 1966. [Google Scholar]
- 12.Ruiz SE, Morett AL. Las Anonas en el México Prehispánico. Memorias Congreso Internacional de Anonáceas. Chapingo, Estado de México, 169-186, 1997.
- 13.Popenoe W. Manual of Tropical and Sub-Tropical Fruits. New York, NY, USA: Hafner Press; 1920. [Google Scholar]
- 14.González-Trujano ME, Navarrete A, Reyes B, Hong E. Some pharmacological effects of the ethanol extract of leaves of Annona diversifolia on the central nervous system in mice. Phytotherapy Research. 1998;12:600–602. [Google Scholar]
- 15.González-Trujano ME, Navarrete A, Reyes B, Cedillo-Portugal E, Hong E. Anticonvulsant properties and bio-guided isolation of palmitone from leaves of Annona diversifolia . Planta Medica. 2001;67(2):136–141. doi: 10.1055/s-2001-11504. [DOI] [PubMed] [Google Scholar]
- 16.González-Trujano ME, Tapia E, López-Meraz L, Navarrete A, Reyes-Ramírez A, Martínez A. Anticonvulsant effect of Annona diversifolia Saff. and palmitone on penicillin-induced convulsive activity. A behavioral and EEG study in rats. Epilepsia. 2006;47(11):1810–1817. doi: 10.1111/j.1528-1167.2006.00827.x. [DOI] [PubMed] [Google Scholar]
- 17.Carballo AI, Martínez AL, González-Trujano ME, et al. Antinociceptive activity of Annona diversifolia Saff. leaf extracts and palmitone as a bioactive compound. Pharmacology Biochemistry and Behavior. 2010;95(1):6–12. doi: 10.1016/j.pbb.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 18.Andrade-Cetto A, Heinrich M. Mexican plants with hypoglycaemic effect used in the treatment of diabetes. Journal of Ethnopharmacology. 2005;99(3):325–348. doi: 10.1016/j.jep.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 19.Shirwaikar A, Rajendran K, Dinesh Kumar C, Bodla R. Antidiabetic activity of aqueous leaf extract of Annona squamosa in streptozotocin-nicotinamide type 2 diabetic rats. Journal of Ethnopharmacology. 2004;91(1):171–175. doi: 10.1016/j.jep.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Adeyemi DO, Komolafe OA, Adewole OS, et al. Anti hyperglycemic activities of Annona muricata (Linn) African Journal of Traditional, Complementary and Alternative Medicines. 2009;6(1):62–69. [PMC free article] [PubMed] [Google Scholar]
- 21.Cristians S, Guerrero-Analco JA, Pérez-Vásquez A, et al. Hypoglycemic activity of extracts and compounds from the leaves of Hintonia standleyana and H. latiflora: potential alternatives to the use of the stem bark of these species. Journal of Natural Products. 2009;72(3):408–413. doi: 10.1021/np800642d. [DOI] [PubMed] [Google Scholar]
- 22.Gupta RK, Kesari AN, Murthy PS, Chandra R, Tandon V, Watal G. Hypoglycemic and antidiabetic effect of ethanolic extract of leaves of Annona squamosa L. in experimental animals. Journal of Ethnopharmacology. 2005;99(1):75–81. doi: 10.1016/j.jep.2005.01.048. [DOI] [PubMed] [Google Scholar]
- 23.Gupta RK, Kesari AN, Diwakar S, et al. In vivo evaluation of anti-oxidant and anti-lipidimic potential of Annona squamosa aqueous extract in type 2 diabetic models. Journal of Ethnopharmacology. 2008;118(1):21–25. doi: 10.1016/j.jep.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Gupta-Elera G, Garrett AR, Martinez A, Robison RA, O’Neill KL. The antioxidant properties of the cherimoya (Annona cherimola) fruit. Food Research International. 2011;44(7):2205–2209. [Google Scholar]
- 25.Loizzo MR, Tundis R, Bonesi M, et al. Radical scavenging, antioxidant and metal chelating activities of Annona cherimola Mill. (cherimoya) peel and pulp in relation to their total phenolic and total flavonoid contents. Journal of Food Composition and Analysis. 2012;25(2):179–184. [Google Scholar]
- 26.Kamalakkannan N, Mainzen Prince PS. Rutin improves the antioxidant status in streptozotocin-induced diabetic rat tissues. Molecular and Cellular Biochemistry. 2006;293(1-2):211–219. doi: 10.1007/s11010-006-9244-1. [DOI] [PubMed] [Google Scholar]
- 27.Henrique Fernandes AA, Barbosa Novelli EL, Okoshi K, et al. Influence of rutin treatment on biochemical alterations in experimental diabetes. Biomedicine and Pharmacotherapy. 2010;64(3):214–219. doi: 10.1016/j.biopha.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 28.Hnatyszyn O, Miño J, Ferraro G, Acevedo C. The hypoglycemic effect of Phyllanthus sellowianus fractions in streptozotocin-induced diabetic mice. Phytomedicine. 2002;9(6):556–559. doi: 10.1078/09447110260573209. [DOI] [PubMed] [Google Scholar]
- 29.Ahmed OM, Moneim AA, Yazid IA, Mahmoud AM. Antihyperglycemic, antihyperlipidemic and antioxidant effects and the probable mechanisms of action of Ruta graveolens infusion and rutin in nicotinamide-streptozotocin-induced diabetic rats. Diabetologia Croatica. 2010;39(1):15–35. [Google Scholar]
- 30.Fontana Pereira D, Cazarolli LH, Lavado C, et al. Effects of flavonoids on α-glucosidase activity: potential targets for glucose homeostasis. Nutrition. 2011;27(11-12):1161–1167. doi: 10.1016/j.nut.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Adisakwattana S, Yibchok-Anun S, Charoenlertkul P, Wongsasiripat N. Cyanidin-3-rutinoside alleviates postprandial hyperglycemia and its synergism with acarbose by inhibition of intestinal α-glucosidase. Journal of Clinical Biochemistry and Nutrition. 2011;49(1):36–41. doi: 10.3164/jcbn.10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pashikanti S, de Alba DR, Boissonneault GA, Cervantes-Laurean D. Rutin metabolites: novel inhibitors of nonoxidative advanced glycation end products. Free Radical Biology and Medicine. 2010;48(5):656–663. doi: 10.1016/j.freeradbiomed.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 33.Qin Y, Chao F, Gao F, et al. Comparative evaluation of quercetin, isoquercetin and rutin as inhibitors of α-glucosidase. Journal of Agricultural and Food Chemistry. 2009;57(24):11463–11468. doi: 10.1021/jf903083h. [DOI] [PubMed] [Google Scholar]


