Abstract
The opioid system is implicated in the hedonic and motivational processing of food, and in binge eating, a behaviour strongly linked to obesity. The aim of this study was to evaluate the effects of 4 weeks of treatment with the mu-opioid receptor antagonist GSK1521498 on eating behaviour in binge-eating obese subjects. Adults with body mass index ⩾30 kg m−2 and binge eating scale scores ⩾19 received 1-week single-blind placebo run-in, and were then randomized to 28 days with either 2 mg day−1 GSK1521498, 5 mg day−1 GSK1521498 or placebo (N=21 per arm) in a double-blind parallel group design. The outcome measures were body weight, fat mass, hedonic and consummatory eating behaviour during inpatient food challenges, safety and pharmacokinetics. The primary analysis was the comparison of change scores in the higher-dose treatment group versus placebo using analysis of covariance at each relevant time point. GSK1521498 (2 mg and 5 mg) was not different from placebo in its effects on weight, fat mass and binge eating scores. However, compared with placebo, GSK1521498 5 mg day−1 caused a significant reduction in hedonic responses to sweetened dairy products and reduced calorific intake, particularly of high-fat foods during ad libitum buffet meals, with some of these effects correlating with systemic exposure of GSK1521498. There were no significant effects of GSK1521498 2 mg day−1 on eating behaviour, indicating dose dependency of pharmacodynamics. GSK1521498 was generally well tolerated and no previously unidentified safety signals were detected. The potential for these findings to translate into clinically significant effects in the context of binge eating and weight regain prevention requires further investigation.
Keywords: binge eating, GSK1521498, obesity, opioid, OPRM1, pharmacogenetics
Introduction
The mu-opioid receptor (MOR), has a critical role in the hedonic and consummatory aspects of ingestive behaviour.1 In animals, MOR agonism enhances hedonic reactions to highly palatable foods and preferentially increases their consumption, whereas antagonism produces opposite effects.2, 3, 4, 5, 6, 7, 8, 9 In humans, MOR antagonism decreases food palatability and reduces short-term intake by 11–29%.10
Dysregulation of the MOR system has been implicated in the pathophysiology of binge eating,11 characterised by recurrent circumscribed episodes of disproportionate and compulsive food consumption.12 Binge eating is associated with craving, loss of control and persistence despite negative consequences and parallels have been suggested with substance addiction.13 Binge eating is seen in 23–46% of obese individuals seeking weight loss treatment14 and its severity relates to body mass index and predicts regain of lost weight.15, 16, 17 However, the relationship is not deterministic, not all binge eaters become obese and not all obese individuals binge eat. Nor does this association of binge eating with obesity define the direction of causality, though studies of binge-eating disorder15 suggest that binge eating may be a pathway to obesity.
There is a paucity of pharmacological treatments for binge eating and/or obesity.11, 18 Positive therapeutic effects on both weight and binge eating have been reported with topiramate (antiepileptic), atomoxetine (norepinephrine reuptake inhibitor), sibutramine (mixed monoamine reuptake inhibitor causing anorexia and thermogenesis), the stimulant phentermine, selective serotonin reuptake inhibitors and rimonabant (cannabinoid receptor 1 inverse agonist).19, 20, 21, 22, 23, 24, 25 However, safety concerns regarding psychiatric (rimonabant, topiramate) and cardiovascular risks (sibutramine, atomoxetine, phentermine) have hindered the clinical deployment of these treatments [26]. There is a need to explore novel pharmacological approaches, guided by the knowledge of the neurochemical systems implicated in the pathophysiology of abnormal eating. Given the role of the MOR system in ingestive behaviour and binge eating, centrally acting mu-opioid antagonists represent a potentially valuable approach for modulating eating behaviour for the treatment of obesity.11, 16, 27, 28, 29 Preliminary findings to date using MOR antagonists for the treatment of obesity and alcohol dependence have yielded some, though limited, therapeutic success.11, 30
GSK1521498 is a novel opioid antagonist being investigated as a candidate treatment for behavioural and substance addictions.31, 32, 33 It is centrally active and has 14–20-fold greater selectivity for mu versus kappa and delta opioid receptors.31 In rodents, GSK1521498 suppressed the intake of standard and palatable chow and caused weight loss in diet-induced obese rats.34 It also suppressed food seeking and binge eating showing superior efficacy to naltrexone.35 In a single dose (25 mg) phase 1 study in healthy overweight men, GSK1521498 reduced the pleasurable response to high-fat and high-sugar food samples and reduced calorie intake in an ad libitum eating experiment.31 The current study evaluated the effects of 28 days of GSK1521498 treatment on a range of parameters in binge-eating obese individuals. We hypothesised that, compared with placebo, treatment with GSK1521498 would cause significant reductions in hedonic responses to food and calorific intake, decrease binge-eating severity and consequently result in weight loss.
Subjects and methods
Participants
Sixty-three volunteers (n=28 (44%) males) aged 18–60 years (mean±s.d., 41.5±10.0 years) endorsing moderate-to-severe binge eating (Binge-Eating Scale (BES) scores ⩾19, mean 26.4±6.7)36, 37 and with body mass index ⩾30 kg m−2 (mean 37.3±4.76 kg m−2) were entered into the study after signed informed consent. The study (identification number EudraCT 2009-016663-11, ClinicalTrials.gov identifier NCT01195792) was approved by Berkshire Research Ethics Committee, United Kingdom.
Participants had no history of axis-I disorders (assessed by the Mini-International Neuropsychiatric Interview) and were excluded if they reported alcohol intake >14 units week−1, screened positive for illicit drugs on urine screen, had used nicotine in the past 3 months or taken any centrally active medications in the preceding 2 weeks. Subjects with Beck Depression Inventory II Scale total score >13 and/or suicidality questionnaire score >0 at screening were excluded.38, 39
Study design
This was a multi-centre double-blind placebo-controlled parallel group study. Subjects received 1-week single-blind placebo run-in, followed by 4-weeks treatment with either placebo, GSK1521498 2 mg day−1 or GSK1521498 5 mg day−1 capsules (all n=21). Treatment doses were selected on the basis of a previous positron emission tomography study33 and a 10-day repeat dose study of safety and pharmacokinetics (PK).32 We predicted that single daily doses of 2 mg day−1 and 5 mg day−1 would be well-tolerated with a favourable safety profile and produce average steady state MOR occupancies of 60.0% and 78.1%, respectively, over 24 h.
The sample size was calculated for the primary endpoint of weight change of 2.1 kg (s.e. 0.5 kg) from baseline based on a placebo-controlled study of sibutramine 10 mg day−1 for 28 days in obese individuals.40 Assuming a similar magnitude of effect with GSK1521498, it was determined a priori that the proposed sample size would yield ⩾95% power to detect this difference with an overall 5% type-I error risk.
Further details of the study design and the CONSORT chart are provided in the Supplementary Methods.
Procedures and measures
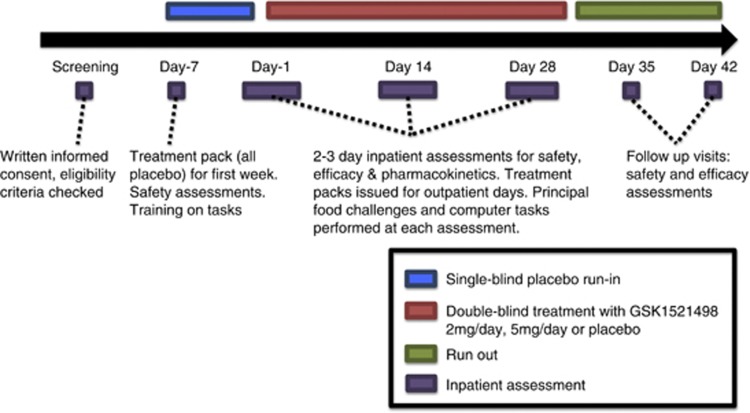
The study flow is summarised in Figure 1. Measures reported herein constitute a subset of a larger dataset including functional neuroimaging, some of which will be reported separately (see Supplementary Methods).
Figure 1.
Schematic representation of the study schedule.
Principal assessments and procedures during the study period related to (i) body weight, fat mass and BES score; (ii) hedonic responses and eating behaviour during inpatient food challenges; (iii) safety; and (iv) PK. The designated primary efficacy endpoints were body weight, fat mass and BES scores.36, 37
Aspects of hedonic responses and eating behaviour were examined during the inpatient visits on Days −1, 14 and 28 using three paradigms: (i) hedonic taste preference;31, 41 (ii) ad libitum snacking;31, 41 and (iii) ad libitum buffet dining. At approximately 1245 hours, subjects were asked to quantify on a nine-point scale (ranging from ‘dislike extremely' to ‘like extremely'), hedonic responses to dairy products of varying fat and sugar content. This was followed by an ad libitum snack eating challenge41 at approximately 1330 hours featuring a selection of participants' favourite snack foods, categorised into high and low levels of fat and sugar. Total calorific intake of each food type was recorded.41 These tasks were previously shown to be sensitive to GSK1521498.31 At pre-specified times during the day, subjects indicated their preferences for the foods to be served at the dinner buffet on a menu card. Familiar foods from local supermarkets, containing 20, 40 or 60% fat were used (no fat content information was provided) and equicaloric portions of all menu options were presented at the dinner buffet at approximately 1800 hours. Additionally, on admission to the unit on days −2, 13 and 27, participants selected a single main course and dessert from a similar menu for dinner (‘restaurant meal'). For each subject, all menus were unique and the total calories consumed and the ranked preference of each item were recorded.
Safety was assessed serially by means of the Power of Attention (POA) composite score of drug-induced sedation,32, 42 Visual Analogue Scales (yielding overall subjective scores for alertness, contentedness and calmness),43, 44, 45 clinical instruments (Profile of Mood States—Brief; Beck's Anxiety and Depression Inventory; Columbia Suicide Severity Rating Scale; Young Mania Rating Scale),39, 46, 47, 48, 49 cardiovascular parameters, adverse events and standard laboratory measures (urea, electrolytes, liver function tests, full blood count). Other aspects of hedonic function were assessed using self report (Temporal Experience of Pleasure; Changes in Sexual Functioning Questionnaire-1450, 51).
For the estimation of PK parameters, plasma concentrations of GSK1521498 were sampled serially on days 1 and 28. Pre-dose samples were collected on days 7, 14 and 21 for the estimation of steady state (trough) concentrations.
Some participants provided additional consent for pharmacogenetic analysis of a venous blood sample. Previous studies have implicated the A118G single nucleotide polymorphism of the OPRM1 gene in variability of therapeutic response to naltrexone and other MOR antagonists.52, 53 We therefore genotyped all consenting Caucasian participants at this allele (see Supplementary Material for details).
Statistical analyses
The primary analyses focused on change scores for each endpoint at each time point in the higher dosing cohort (GSK1521498 5 mg day−1) versus placebo. Change scores for each endpoint were calculated by subtracting the baseline values from the post-randomisation values for each subject at each time point; missing data were not replaced. Repeated measures of analysis of covariance models with PROC MIXED from SAS were used, fitting gender, treatment, day and study day-by-treatment interaction as fixed effects and baseline score as a covariate.
For inpatient food challenges, measures were analysed hierarchically: first, overall hedonic ratings during taste testing and total calorific intake during ad libitum snacking and ad libitum buffet dining were analysed. Where global measures were statistically significant for a given paradigm, supplementary analyses were conducted for the high-fat/high-sugar conditions; and where significant, for low-fat/low-sugar conditions to assess specificity of drug effects.
If significant treatment effects were identified in the GSK1521498 5 mg day−1 group versus placebo, possible dose dependency was evaluated in two ways: firstly, we conducted supplemental analyses in the GSK1521498 2 mg day−1 group; and secondly, we estimated correlations between trough GSK1521498 plasma concentrations and pharmacodynamic endpoints measured over all study participants. This approach minimised the number of statistical comparisons, as the most pronounced effects of treatment were expected a priori for the higher dose, but also permitted dose dependency to be evaluated comprehensively.
This being an exploratory study in which the interest lay equally in determining ‘an effect' versus ‘no effect' of active treatment compared with placebo, statistical significance was defined as two-tailed P<0.05 uncorrected, and the sample size was powered to justify this (vide supra).
Results
Demographic characteristics for all subjects are displayed in Table 1. There were no significant differences between the groups on baseline measures of age, gender balance, weight, body mass index or total BES score (all P>0.10).
Table 1. Baseline characteristics and demographics.
| Run-in only | Placebo | 498 2 mg | 498 5 mg | Total | |
|---|---|---|---|---|---|
| Number of subjects | |||||
| Planned, N | 0 | 20 | 20 | 20 | 60 |
| Dosed, N | 4 | 21 | 21 | 21 | 67 |
| Completed, n (%) | 0 | 21 (100) | 18 (86) | 21 (100) | 60 (90) |
| Total number of subjects withdrawn, n (%) | 4 (100) | 0 | 3 (14) | 0 | 7 (10) |
| Withdrawn due to adverse event, n (%) | 1 (25) | 0 | 2 (10)a | 0 | 3 (4)a |
| Withdrawn at investigator discretion, n (%) | 2 (50) | 0 | 1 (5) | 0 | 3 (4) |
| Subject withdrew consent, n (%) | 1 (25) | 0 | 0 | 0 | 1 (1) |
| Demographics | |||||
|---|---|---|---|---|---|
| N (all subjects) | 4 | 21 | 21 | 21 | 67 |
| Mean age in years (s.d.) | 44.8 (9.50) | 41.3 (9.22) | 44.9 (10.08) | 37.8 (10.06) | 41.5 (10.00) |
| Females: males | 2:2 | 11:10 | 12:9 | 12:9 | 37:30 |
| Mean Weight in kg (s.d.) | 109.7 (21.68) | 109.2 (18.17) | 110.9 (23.63) | 104.0 (9.82) | 108.1 (18.11) |
| Mean body mass index in kg m−2 (s.d.) | 36.2 (4.15) | 37.8 (4.87) | 37.1 (5.37) | 37.1 (4.38) | 37.3 (4.76) |
| White/Caucasian/European heritage, n (%) | 4 (100) | 17 (81) | 19 (90) | 17 (81) | 57 (85) |
| African American/African heritage, n (%) | 0 | 3 (14) | 2 (10) | 3 (14) | 8 (12) |
| White—Arabic/North African heritage, n (%) | 0 | 1 (5) | 0 | 1 (5) | 2 (3) |
Includes one subject withdrawn from the study due to a serious adverse event.
Pharmacokinetics
Both 2 mg and 5 mg doses were absorbed rapidly with a median time to maximal concentration (Tmax) of 2–3 h on Days 1 and 28. Consistent with the previously reported half-life of 20–24 h,31 approximate steady state levels were achieved by Day 7 (see Supplementary Figure S2 and Supplementary Table S4). Estimated mean MOR occupancy based on the steady state levels ranged between 64 and 80% for a 2-mg dose and 82–92% for a 5-mg dose.
Primary efficacy measures
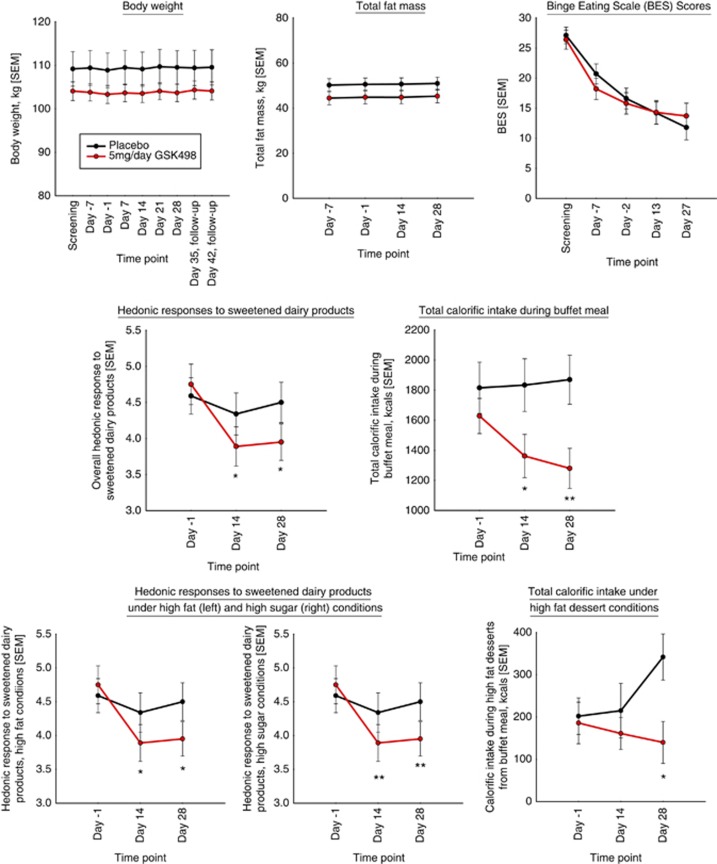
Figure 2, top panel indicates the mean body weight, fat mass and BES scores for the three treatment arms over time. Body weight and fat mass were relatively stable in all the groups, while BES scores reduced over time in all the groups both before and after randomisation. Analysis of covariance indicated no differential effects of 5 mg day−1 GSK1521498 on the primary efficacy measures compared with placebo (all P>0.10). However, a significant correlation was seen between the changes in the BES score and weight (in the 5 mg group, Pearson's r=0.719, P=0.0004; across all subjects r=0.4, P=0.0018), that is, greater reduction of binge eating was associated with greater weight loss. Moreover, the small sub-group of participants (N=3) with one or more copies of the 118G allele (‘G-carriers') demonstrated greater weight reduction (t(df)=−4.41(28), P=0.0001; see Figure 3, Supplementary Table S3) compared with A118 homozygotes (N=12).
Figure 2.
Primary and secondary endpoints: the top panel shows the measures on the primary end points of weight, fat mass and binge-eating scale scores. The change in overall hedonic response to sweetened dairy products and the buffet intake are depicted in the middle panel. The bottom panel shows hedonic responses to high-fat and high-sugar concentrations and intake of the high-fat desserts.
Figure 3.
Pharmacogenetic analyses: three subjects in the GSK1521498 5 mg day−1 group with one or more copies of the 118 G allele (AG) were compared with A118 homozygotes (AA, N=12). The left panel depicts the mean weight change over the treatment period and the right panel displays the individual weight plots for all 15 Caucasian subjects. It can be seen that greatest weight change is seen in two of the G-carriers (AG). ***P<0.001.
Hedonic responses and eating behaviour
Hedonic responses
Treatment with GSK1521498 5 mg day−1 significantly reduced hedonic ratings for sweetened dairy products overall, on Day 14 (t(df)=2.36(59), P=0.0215) and Day 28 (t(df)=2.61(57), P=0.0115), compared with placebo (Figure 2, middle panel). Follow-up analyses indicated that this was due to significant effects on pleasurable response to high-sugar (Day 14: t(df)=3.14(141), P=0.0021; Day 28: t(df)=3.09(141), P=0.0024) and high-fat food samples (Day 14: t(df)=2.01(132), P=0.0464; Day 28: t(df)=2.45(132), P=0.0157), with no effects on responses to low-fat and low-sugar samples (all P>0.10; Figure 2, bottom panel). No significant effect of GSK1521498 2 mg day−1 on overall hedonic preference was detected for Day 14 or 28 (both P>0.10). No gender effects were seen. The changes in overall, high-fat and high-sugar hedonic responses were negatively correlated with the maximal plasma drug concentration (Cmax) (r=−0.33, P=0.01; r=−0.353, P=0.0055; r=−0.34, P=0.007) and 24-h drug exposure (AUC24) (r=−0.31, P=0.017; r=−0.34, P=0.0094; r=−0.33, P=0.011). (see Supplementary Figure S4).
Ad libitum snacking
There was a non-significant trend towards reduction in overall calorific intake in the GSK1521498 5 mg day−1 group compared with placebo on Day 14 (t(df)=1.73(58), P=0.0883) but not on Day 28 (P>0.10).
Ad libitum buffet dining
There was a significant reduction in total calorific intake in the GSK1521498 5 mg day−1 group versus placebo, on Day 14 (t(df)=2.10(52), P=0.0405) and Day 28 (t(df)=−2.74(45), P=0.0087; Figure 2, middle panel). Follow-up analyses for Day 28 indicated that this finding was largely attributable to a significant reduction in calorific intake for the main courses (21.4%, t(df)=−2.4(45), P=0.0207) and the 60% fat dessert (24.75%, t(df)=2.35(48), P=0.023; Figure 2, bottom panel). Men consumed more calories than women; but there was no drug-by-gender interaction. There was no significant effect in the 2 mg day−1 GSK1521498 group versus placebo (P>0.10). Variation in the main course calorie intake was negatively correlated with Cmax (Pearson's r=−0.29, P=0.036). The changes in hedonic responses did not correlate with changes in calorie intake (Supplementary Table S11).
There was no significant change in intake at the restaurant meals in the GSK1521498 5 mg day−1 group (P>0.10) and no change in the ranked preferences on the menus on either the buffet or the restaurant meals (Supplementary Results).
Safety results
Power of attention
There was no significant effect of GSK1521498 5 mg day−1 on the POA composite score of drug-related sedation on Days −1 and 28 (all P>0.10; Supplementary Table S15).
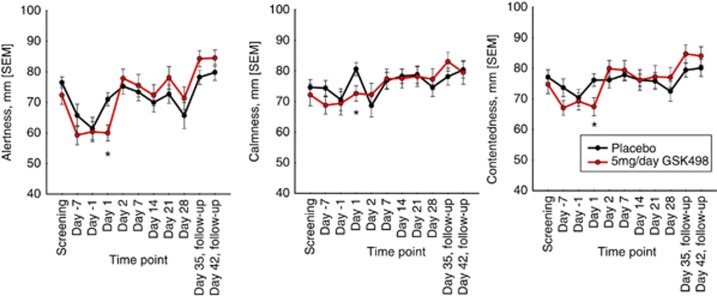
Visual analogue scales
There were statistically significant impairments in alertness, contentedness and calmness scores in the GSK1521498 5 mg day−1 group compared with placebo on Day 1 only (t(df)=2.89(57), P=0.005; t(df)=2.77(57), P=0.008; and t(df)=2.30(57), P=0.0253, respectively; Figure 4, Supplementary Table S15). These three measures increased from baseline by 19–34% in the placebo group between Day −1 and Day 1 as compared with relatively static levels (changes of −1% to +6%) seen in the active treatment group.
Figure 4.
Changes in Visual Analogue Scale measures of alertness, calmness and contentedness in the placebo and GSK1521498 groups over the study duration. *P<0.05.
Exploration of dose dependency revealed a trend towards a reduction on calmness alone (t(df)=1.74(58), P=0.087; other P>0.10) with GSK1521498 2 mg day−1 compared with placebo. No significant gender differences or correlations with PK parameters were seen.
Clinical safety instruments
There were no significant or trend significant effects of GSK1521498 (2 mg or 5 mg) compared with placebo on the Profile of Mood States—Brief, Beck's Anxiety and Depression Inventory (all P>0.10; Supplementary Table S15). No subjects endorsed suicidality on the Columbia Suicide Severity Rating Scale and only one subject reported a non-zero Young Mania Rating Scale score (not clinically significant). No significant treatment differences were observed for GSK1521498 versus placebo for change from baseline in Temporal Experience of Pleasure or Changes in Sexual Functioning Questionnaire-14 scores (Supplementary Tables S20 and S21).
Cardiovascular parameters
There was no significant effect of GSK1521498 at either dose on pulse or blood pressure versus placebo (all P>0.05, Supplementary Figure S5). No abnormal or clinically significant electrocardiogram findings were detected.
Adverse events
The proportion of subjects reporting any adverse event was similar in all the three treatment groups: 86, 81 and 76% for GSK1521498 2 mg day−1, GSK1521498 5 mg day−1 and placebo, respectively (chi-square, P>0.10), and the majority were of mild-to-moderate severity (Supplementary Table S17). The incidence of commonly reported adverse events was similar across the treatment groups; some gastrointestinal effects (for example, diarrhoea, abdominal discomfort) tended to be more commonly reported in the GSK1521498 groups. Three subjects were withdrawn from the GSK1521498 2 mg day−1 cohort for reasons deemed by the investigator to be unrelated to the study drug: one due to arthralgia; one became pregnant; and one subject reported persecutory delusions following randomisation. Clinical interview by a consultant psychiatrist (EB), who also obtained collateral history from this subject's parents, suggested long-standing delusions, the nature and intensity of which were unrelated to study participation or receiving active treatment. This subject was referred for urgent local mental health follow-up.
Safety laboratory measures
There were no significant effects of treatment with GSK1521498 on any of the primary safety laboratory parameters (see Supplementary Figure S6).
Discussion
This study assessed the effects of 4-weeks of treatment with the MOR antagonist GSK1521498 on hedonic evaluation and consumption of food, binge-eating severity and body weight in obese people with binge-eating symptoms. There were two key effects: GSK1521498 was associated with significant reductions in hedonic preference, specifically for higher concentrations of sugar and fat. GSK1521498 also markedly reduced calorie intake in an ad libitum buffet and particularly for more palatable foods (high-fat desserts). These effects were dose dependent, occurring only in the 5 mg group, and were, to an extent, correlated with variability in plasma concentrations of GSK1521498. These observations are in keeping with predictions and offer proof of the drug's mechanistic on-target effects.
The effects of GSK1521498 were not entirely consistent across all measures of eating behaviour. Changes in hedonic ratings did not correlate with the effects on calorie intake, perhaps because the latter involved multiple foods of varying compositions, whereas the former used relatively homogeneous food samples. No significant effects on consumption were found for the ad libitum snacking or the restaurant meal. The snacking paradigm may quantify a type of eating that is relatively difficult to modify: consumption of favourite foodstuffs following prolonged fasting (>12 h). The restaurant meal captures consumption in a context with limited food availability. It appears that the effects of mu-opioid antagonism become apparent only in settings that permit overconsumption. This distinction might be considered akin to eating what is in the fridge rather than eating what is on the plate.
Moreover, these effects on eating behaviour measured by in-unit assessments did not translate into reductions in weight or fat mass. There are several possible reasons for this. First, acute changes in hedonic and consummatory aspects of eating may take longer than 28 days to translate to changes in habitual decision making about food consumption, sufficient to cause significant weight loss. The duration of this study was limited by the toxicological data currently available for GSK1521498. Second, participants were treated as outpatients without dietary restriction or other active lifestyle management interventions. It is a limitation of the design that we do not have data on calorie consumption outside the controlled setting of in-unit assessments. Third, there may be significant heterogeneity between obese patients in their responsiveness to GSK1521498 or other MOR antagonists. For example, post-hoc pharmacogenetic analysis showed that a small sub-group of Caucasian participants carrying one or more copies of the 118G allele of the OPRM1 gene in the 5 mg treatment group showed a greater weight reduction compared with A118 homozygotes: indeed two of the three subjects who showed the greatest weight loss were G-carriers. These data must be treated with caution given the post-hoc, exploratory nature of the analysis and the very small sample size. Nonetheless, they suggest that allelic variation in the MOR gene may contribute to variable therapeutic response to MOR antagonists in the treatment of obesity. Finally, we note that the highest dose of GSK1521498 administered was not sufficient to cause sustained receptor occupancy >90% and high levels of MOR blockade have been considered necessary for optimal therapeutic effect of naltrexone and other MOR antagonists.54 The encouraging safety profile of GSK1521498 suggests that repeated dosing up to 10 mg day−1 may be tolerable in outpatients and higher doses might be expected to demonstrate stronger therapeutic effects in future studies of obesity.
Certain other limitations should be considered. BES scores diminished considerably across all groups even before randomisation, limiting the ability to discriminate any benefits of active treatment on this endpoint. The use of the self-reported BES is a limitation as high placebo response rates have been reported with subjective measures in clinical trials in binge-eating individuals.27 The findings are preliminary as the study was not powered to correct for multiple comparisons; however, we did deploy strategies designed to minimise these.
Multiple anti-obesity agents have been withdrawn due to central/psychiatric/cardiovascular safety concerns.26, 55, 56 GSK1521498 was generally well tolerated compared with placebo, with no deleterious effects detected on anxiety, mood or other aspects of hedonic function or on liver or other blood safety parameters. Akin to previous studies,31, 32 transient impairments on subjective ratings of alertness, contentedness and calmness, were seen with GSK1521498 on the first day of active treatment, largely driven by relative increases in the placebo group. Therefore, the only central effects of GSK1521498 identified were mild and not clinically significant.
Although the lack of effect on weight does not support immediate progression for obesity therapeutics, the effects on eating behaviour and the early pharmacogenetic data warrant further evaluation of GSK1521498 as a more genetically targeted treatment in obesity and binge eating. The similarities between the MOR dysregulation in binge eating and substance addiction motivate exploration of GSK1521498 as a treatment for drug addictions. This study highlights the value of using experimental medicine models to demonstrate clinical proof-of-mechanism for a novel compound targeting abnormal reward-driven eating behaviour.
Acknowledgments
The authors wish to thank Barry O'Neill for work on the protocol and all the participants and GSK support staff. This study was funded and conducted by GSK.
HZ is a Clinical PhD Fellow on the Wellcome Trust and GSK funded Translational Medicine and Therapeutics (TMAT) programme. SRC is a Psychiatric Academic Clinical Fellow, funded by NIHR in CPFT; he received no financial or other remuneration from GSK for this project. SRC consults for Cambridge Cognition, Shire, Lilly, and P1Vital. The following authors are employed by and hold shares in GSK: AK, WT, KM, AN, AS, AB, DR, MB, EB, PN.
Footnotes
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
Supplementary Material
References
- Le Merrer J, Becker JA, Befort K, Kieffer BL. Reward processing by the opioid system in the brain. Physiol Rev. 2009;89:1379–1412. doi: 10.1152/physrev.00005.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanger DJ, McCarthy PS. Increased food and water intake produced in rats by opiate receptor agonists. Psychopharmacology (Berl) 1981;74:217–220. doi: 10.1007/BF00427097. [DOI] [PubMed] [Google Scholar]
- Will MJ, Franzblau EB, Kelley AE. Nucleus accumbens mu-opioids regulate intake of a high-fat diet via activation of a distributed brain network. J Neurosci. 2003;23:2882–2888. doi: 10.1523/JNEUROSCI.23-07-02882.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecina S, Berridge KC. Hedonic hot spot in nucleus accumbens shell: where do mu-opioids cause increased hedonic impact of sweetness. J Neurosci. 2005;25:11777–11786. doi: 10.1523/JNEUROSCI.2329-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KS, Berridge KC.The ventral pallidum and hedonic reward: neurochemical maps of sucrose "liking" and food intake J Neurosci 200525p8637–8649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apfelbaum M, Mandenoff A. Naltrexone suppresses hyperphagia induced in the rat by a highly palatable diet. Pharmacol Biochem Behav. 1981;15:89–91. doi: 10.1016/0091-3057(81)90344-0. [DOI] [PubMed] [Google Scholar]
- Marks-Kaufman R, Kanarek RB. Modifications of nutrient selection induced by naloxone in rats. Psychopharmacology (Berl) 1981;74:321–324. doi: 10.1007/BF00432739. [DOI] [PubMed] [Google Scholar]
- Leventhal L, Kirkham TC, Cole JL, Bodnar RJ. Selective actions of central mu and kappa opioid antagonists upon sucrose intake in sham-fed rats. Brain Res. 1995;685:205–210. doi: 10.1016/0006-8993(95)00385-4. [DOI] [PubMed] [Google Scholar]
- Smith KS, Berridge KC. Opioid limbic circuit for reward: interaction between hedonic hotspots of nucleus accumbens and ventral pallidum. J Neurosci. 2007;27:1594–1605. doi: 10.1523/JNEUROSCI.4205-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans MR, Gray RW. Opioid peptides and the control of human ingestive behaviour. Neurosci Biobehav Rev. 2002;26:713–728. doi: 10.1016/s0149-7634(02)00041-6. [DOI] [PubMed] [Google Scholar]
- Nathan PJ, Bullmore ET. From taste hedonics to motivational drive: central mu-opioid receptors and binge-eating behaviour. Int J Neuropsychopharmacol. 2009;12:995–1008. doi: 10.1017/S146114570900039X. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders(4th edn, text rev.). Washington, DC2000
- Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite. 2009;53:1–8. doi: 10.1016/j.appet.2009.05.018. [DOI] [PubMed] [Google Scholar]
- de Zwaan M, Mitchell JE. Opiate antagonists and eating behavior in humans: a review. J Clin Pharmacol. 1992;32:1060–1072. [PubMed] [Google Scholar]
- Striegel-Moore RH, Cachelin FM, Dohm FA, Pike KM, Wilfley DE, Fairburn CG, et al. Comparison of binge eating disorder and bulimia nervosa in a community sample. Int J Eat Disord. 2001;29:157–165. doi: 10.1002/1098-108x(200103)29:2<157::aid-eat1005>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Wadden TA. Psychological aspects of severe obesity. Am J Clin Nutr. 1992;55 (2 Suppl:524S–532S. doi: 10.1093/ajcn/55.2.524s. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aigner M, Treasure J, Kaye W, Kasper S. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of eating disorders. World J Biol Psychiatry. 2011;12:400–443. doi: 10.3109/15622975.2011.602720. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Arnold LM, Shapira NA, Keck PE, Rosenthal NR, Karim MR, et al. Topiramate in the treatment of binge eating disorder associated with obesity: a randomized, placebo-controlled trial. Am J Psychiatry. 2003;160:255–261. doi: 10.1176/appi.ajp.160.2.255. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Arnold LM, Shapira NA, Keck PE, Rosenthal NR, Karim MR, et al. Atomoxetine in the treatment of binge-eating disorder: a randomized placebo-controlled trial. J Clin Psychiatry. 2007;68:390–398. doi: 10.4088/jcp.v68n0306. [DOI] [PubMed] [Google Scholar]
- Appolinario JC, Bacaltchuk J, Sichieri R, Claudino AM, Godoy-Matos A, Morgan C, et al. A randomized, double-blind, placebo-controlled study of sibutramine in the treatment of binge-eating disorder. Arch Gen Psychiatry. 2003;60:1109–1116. doi: 10.1001/archpsyc.60.11.1109. [DOI] [PubMed] [Google Scholar]
- Kang JG, Park CY, Kang JH, Park YW, Park SW. Randomized controlled trial to investigate the effects of a newly developed formulation of phentermine diffuse-controlled release for obesity. Diabetes Obes Metab. 2011;12:876–882. doi: 10.1111/j.1463-1326.2010.01242.x. [DOI] [PubMed] [Google Scholar]
- Van Gaal LF, Rissanen AM, Scheen AJ, Ziegler O, Rössner S. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet. 2005;365:1389–1397. doi: 10.1016/S0140-6736(05)66374-X. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Hudson JI, Malhotra S, Welge JA, Nelson EB, Keck PE, et al. Citalopram in the treatment of binge-eating disorder: a placebo-controlled trial. J Clin Psychiatry. 2003;64:807–813. doi: 10.4088/jcp.v64n0711. [DOI] [PubMed] [Google Scholar]
- Guerdjikova AI, McElroy SL, Kotwal R, Welge JA, Nelson E, Lake K, et al. High-dose escitalopram in the treatment of binge-eating disorder with obesity: a placebo-controlled monotherapy trial. Hum Psychopharmacol. 2008;23:1–11. doi: 10.1002/hup.899. [DOI] [PubMed] [Google Scholar]
- Nathan PJ, O'Neill BV, Napolitano A, Bullmore ET. Neuropsychiatric adverse effects of centrally acting antiobesity drugs. CNS Neurosci Ther. 2011. [DOI] [PMC free article] [PubMed]
- Jacobs-Pilipski MJ, Wilfley DE, Crow SJ, Walsh BT, Lilenfeld LR, West DS, et al. Placebo response in binge eating disorder. Int J Eat Disord. 2007;40:204–211. doi: 10.1002/eat.20287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR, et al. Prevalence and correlates of eating disorders in adolescents: results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yager J.Binge eating disorder: the search for better treatments Am J Psychiatry 2008165p4–6. [DOI] [PubMed] [Google Scholar]
- Rosner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M, et al. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2010. p. CD001867. [DOI] [PubMed]
- Nathan PJ, O'Neill BV, Bush MA, Koch A, Tao WX, Maltby K, et al. Opioid receptor modulation of hedonic taste preference and food intake: a single-dose safety, pharmacokinetic, and pharmacodynamic investigation with GSK1521498, a novel mu-opioid receptor inverse agonist. J Clin Pharmacol. 2011;52:464–474. doi: 10.1177/0091270011399577. [DOI] [PubMed] [Google Scholar]
- Nathan PJ, Bush MA, Tao WX, Koch A, Davies KM, Maltby K, et al. Multiple-dose safety, pharmacokinetics, and pharmacodynamics of the mu-opioid receptor inverse agonist GSK1521498. J Clin Pharmacol. 2011;52:1456–1467. doi: 10.1177/0091270011421785. [DOI] [PubMed] [Google Scholar]
- Rabiner EA, Beaver J, Makwana A, Searle G, Long C, Nathan PJ, et al. Pharmacological differentiation of opioid receptor antagonists by molecular and functional imaging of target occupancy and food reward-related brain activation in humans. Mol Psychiatry. 2011;16:826–835. doi: 10.1038/mp.2011.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignar DM, Goetz AS, Noble KN, Carballo LH, Stroup AE, Fisher JC, et al. Regulation of ingestive behaviors in the rat by GSK1521498, a novel mu-opioid receptor-selective inverse agonist. J Pharmacol Exp Ther. 2011;339:24–34. doi: 10.1124/jpet.111.180943. [DOI] [PubMed] [Google Scholar]
- Giuliano C, Robbins TW, Nathan PJ, Bullmore ET, Everitt BJ.Inhibition of opioid transmission at the mu-opioid receptor prevents both food seeking and binge-like eating Neuropsychopharmacology 2012. e-pub ahead of print 18 July 2012; doi: 10.1038/npp.2012.128 [DOI] [PMC free article] [PubMed]
- Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- Gladis MM, Wadden TA, Foster GD, Vogt RA, Wingate BJ. A comparison of two approaches to the assessment of binge eating in obesity. Int J Eat Disord. 1998;23:17–26. doi: 10.1002/(sici)1098-108x(199801)23:1<17::aid-eat3>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beamesderfer A. Assessment of depression: the depression inventory. Mod Probl Pharmacopsychiatry. 1974;7:151–169. doi: 10.1159/000395074. [DOI] [PubMed] [Google Scholar]
- Napolitano A, Miller SR, Murgatroyd PR, Delafont B, Brooke A, Elkhawad M, et al. Prediction of weight loss and regain following dietary, lifestyle, and pharmacologic intervention. Clin Pharmacol Ther. 2012;91:1027–1034. doi: 10.1038/clpt.2011.333. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Krahn DD, Demitrack MA, Nairn K, Gosnell BA. Naloxone, an opiate blocker, reduces the consumption of sweet high-fat foods in obese and lean female binge eaters. Am J Clin Nutr. 1995;61:1206–1212. doi: 10.1093/ajcn/61.6.1206. [DOI] [PubMed] [Google Scholar]
- Kennedy DO, Scholey AB, Wesnes KA. The dose-dependent cognitive effects of acute administration of Ginkgo biloba to healthy young volunteers. Psychopharmacology (Berl) 2000;151:416–423. doi: 10.1007/s002130000501. [DOI] [PubMed] [Google Scholar]
- Bond A, Lader M. The use of analogue scales in rating subjective feelings. Br J Med Psychol. 1974;47:211–218. [Google Scholar]
- Bond A, Lader M, Shrotriya R. Comparative effects of a repeated dose regime of diazepam and buspirone on subjective ratings, psychological tests and the EEG. Eur J Clin Pharmacol. 1983;24:463–467. doi: 10.1007/BF00609887. [DOI] [PubMed] [Google Scholar]
- Chamberlain SR, Müller U, Deakin JB, Corlett PR, Dowson J, Cardinal RN, et al. Lack of deleterious effects of buspirone on cognition in healthy male volunteers. J Psychopharmacol. 2006;21:210–215. doi: 10.1177/0269881107068066. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- McNair DM, Heuchert JP. Multi-Health Systems: New York; 2005. Profile of Mood States – Technical update. [Google Scholar]
- Steer RA, Rissmiller DJ, Ranieri WF, Beck AT. Structure of the computer-assisted Beck Anxiety Inventory with psychiatric inpatients. J Pers Assess. 1993;60:532–542. doi: 10.1207/s15327752jpa6003_10. [DOI] [PubMed] [Google Scholar]
- Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164:1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller A, McGarvey EL, Clayton AH. Reliability and construct validity of the Changes in Sexual Functioning Questionnaire short-form (CSFQ-14) J Sex Marital Ther. 2006;32:43–52. doi: 10.1080/00926230500232909. [DOI] [PubMed] [Google Scholar]
- Gard DE, Gard MG, Kring AM, John OP. Anticipatory and consummatory components of the experience of pleasure: a scale development study. J Res Personality. 2006;40:1086–1102. [Google Scholar]
- Anton RF, Oroszi G, O'Malley S, Couper D, Swift R, Pettinati H, et al. An evaluation of mu-opioid receptor (OPRM1) as a predictor of naltrexone response in the treatment of alcohol dependence: results from the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) study. Arch Gen Psychiatry. 2008;65:135–144. doi: 10.1001/archpsyc.65.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamorro AJ, Marcos M, Mirón-Canelo JA, Pastor I, González-Sarmiento R, Laso FJ, et al. Association of micro-opioid receptor (OPRM1) gene polymorphism with response to naltrexone in alcohol dependence: a systematic review and meta-analysis. Addict Biol. 2012;17:505–512. doi: 10.1111/j.1369-1600.2012.00442.x. [DOI] [PubMed] [Google Scholar]
- Weerts EM, Kim YK, Wand GS, Dannals RF, Lee JS, Frost JJ, et al. Differences in delta- and mu-opioid receptor blockade measured by positron emission tomography in naltrexone-treated recently abstinent alcohol-dependent subjects. Neuropsychopharmacology. 2008;33:653–665. doi: 10.1038/sj.npp.1301440. [DOI] [PubMed] [Google Scholar]
- Elangbam CS. Review paper: Current strategies in the development of anti-obesity drugs and their safety concerns. Vet Pathol. 2009;46:10–24. doi: 10.1354/vp.46-1-10. [DOI] [PubMed] [Google Scholar]
- Bariohay B, Roux JA, Bonnet MS, Dallaporta M, Troadec JD. An update in the management of obesity: the weight of CNS targets. Recent Pat CNS Drug Discov. 2011;6:164–180. doi: 10.2174/157488911796958048. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.