Abstract
Aims:
To analyze the results of balloon dilatation for short segment male urethral strictures.
Materials and Methods:
Retrospective analysis was done of 120 patients undergoing urethral balloon dilatation since January 2004 to January 2012. The inclusion criteria for analysis was a short segment (less than 1.5 cm) stricture, exclusion criteria were pediatric, long (more than 1.5 cm), traumatic, malignant strictures. The parameters analyzed included presentation of patients, ascending urethrogram (AUG) and descending urethrogram findings, pre- and postoperative International prostate symptoms score (IPSS), uroflowmetry (Qmax), and post-void residue (PVR). Need for self calibration/ancillary procedures were assessed. Failure was defined as requirement for a subsequent endoscopic or open surgery. A urethral balloon catheter (Cook Urological, Spencer, Indiana) is passed over a guide wire after on table AUG and inflated till 180 psi for 5 minutes under fluoroscopy till waist disappears. Dilatation is followed by insertion of a Foley catheter. Patients were followed up at 1, 3, and 6 months.
Results:
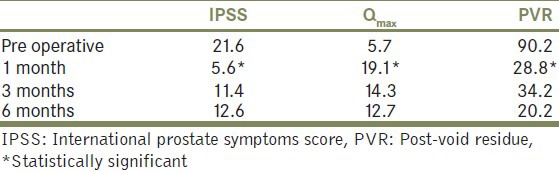
Mean age was 49.86 years. Mean follow-up was 6 (2–60) months. IPSS improved from 21.6 preoperative to 5.6 postoperatively. Qmax increased from 5.7 to 19.1 and PVR decreased from 90.2 to 28.8 (P < 0.0001*) postoperatively. At 1, 3, and at 6 monthly follow-up, 69.2% (n = 82) patients were asymptomatic.
Conclusions:
Balloon dilation is a safe, well-tolerated procedure with minimal complications. Further randomized studies comparing balloon dilatation with direct internal visual urethrotomy are warranted.
Keywords: Balloon dilatation, direct visual internal urethrotomy, urethral stricture
INTRODUCTION
Sequential dilation with metal sound and boogies has been practiced for urethral stricture disease since a long time. It is usually performed under local anesthesia and often is associated with significant discomfort, urethral bleeding, extravasations, and secondary spongiofibrosis due to shearing forces associated with serial dilation resulting in poor outcome.[1]
There are myriad treatment options to manage short segment urethral strictures which include endoscopic approaches and urethroplasties. Direct visual internal urethrotomy (DVIU) is an endoscopic treatment option for short segment anterior urethral strictures with success rates in the range of 46 to 76%.[1,2,3] Urethroplasty offers patients the greatest chance for cure; however, it requires surgical expertise.[4] Balloon dilation is a minimally invasive technique that has a potential to offer an alternative to DVIU.[5] It dilates by radial application of forces against the stricture, avoiding the potentially shearing forces associated with sequential rigid dilation. Theoretically, it reduces urethral trauma; thus, it reduces subsequent spongiofibrosis and potentially may translate into improved therapeutic outcomes. The potential complications with DVIU include bleeding and extravasation. In addition, it involves a certain amount of learning curve. Urethral balloon dilatation has the potential advantage of being less morbid and is technically simpler to perform. The majority of the studies done for balloon dilatation are anecdotal studies and lack follow up. In this analysis, we have “revisited” the technique of urethral balloon dilatation to assess its role in contemporary management of stricture urethra.
The aim of the study was to evaluate and revisit the technique in terms of the short-term efficacy short segment male urethral strictures.
MATERIALS AND METHODS
An institutional review board (IRB) approval was taken prior to initiating the analysis. Retrospective analysis of consecutive patients (n = 120) undergoing urethral balloon dilatation since January 2004 to January 2012 was done. Inclusion criteria were short segment (<1.5 cm) stricture on ascending urethrogram (AUG). Exclusion criteria were pediatric patients, long length strictures (longer than 1.5 cm), strictures after distraction injury, and malignant strictures. Parameters studied were – presentation of the patients, stricture site, location and length of stricture on AUG, International prostate symptoms score (IPSS), uroflowmetry (Qmax), post-void residual urinevolume (PVR). Need for post-procedural self calibration and ancillary procedures was analyzed. Requirement of the same or any other endoscopic or open surgery was considered as failure. Subsequent follow ups were at 1, 3, and 6 months.
The urethral balloon catheter set consists of (Cook Urological, Spencer, Indiana, USA) a 6F open-lumen, blunt-tip catheter and a 8-cm balloon that inflates fully to 24F at a maximum inflation pressure of 181 psi, using a pressure injector device [Figures 1 and 2]. The procedure starts with a “on table” urethrogram to assess the length and site of stricture. A 0.038 inch. hydrophilic guide wire is passed across the stricture. The hydrophilic property allows the wire to negotiate the narrow portion. Balloon dilatation of the stricture is done under fluoroscopic guidance. The disappearance of waisting indicated adequate dilatation [Figure 3]. Duration of the dilatation was 5 minutes. Cystoscopy with 19 Fr sheath was done to assess the urethra [Figure 4] and the dilated segment for any bleeding or mucosa tear. 16 Fr Foley's catheter was inserted.
Figure 1.
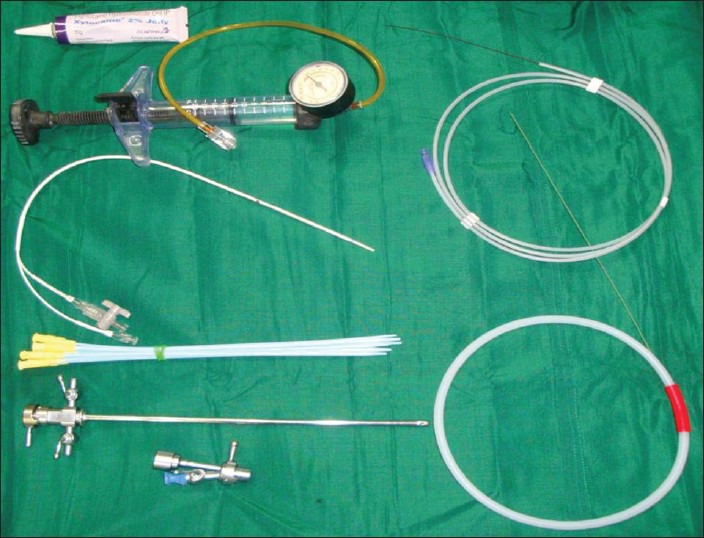
OR trolley set up
Figure 2.
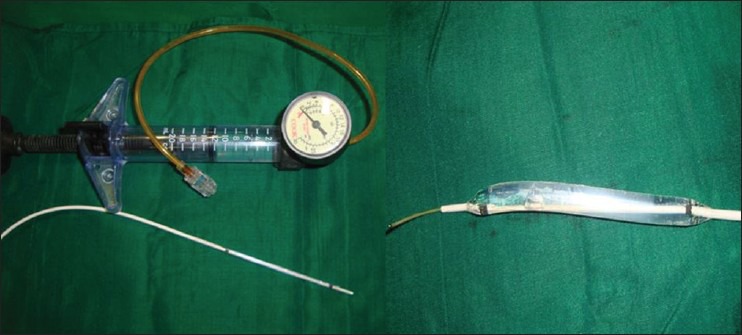
Urethral balloon dilator set (Urological Inc, spencer, Indiana, USA) contains7 Fr radioopague balloon catheter. Radioopague markers are placed at the proximal and distal ends of thecathter balloon. It is for one time use. 0.038 inch (0.97 mm) diameter TFE coated stainless steel wire 80 cm long with 3 cm flexible tip and a syringe are included
Figure 3.
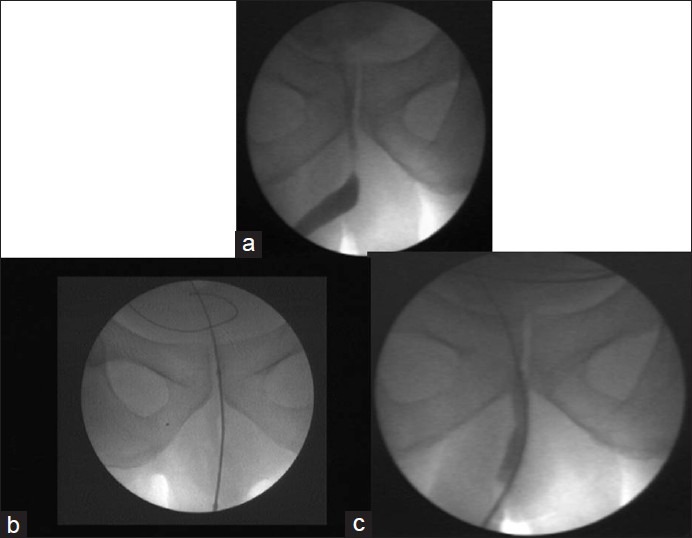
(a) A initial on table urethrogram is done to assess the length of the stricture (b) The urethral balloon catheter is positioned depending on the site of the stricture (c) The proper balloon dilatation is confirmed with appearance of waisting (the balloon is inflated till the waist disappears
Figure 4.
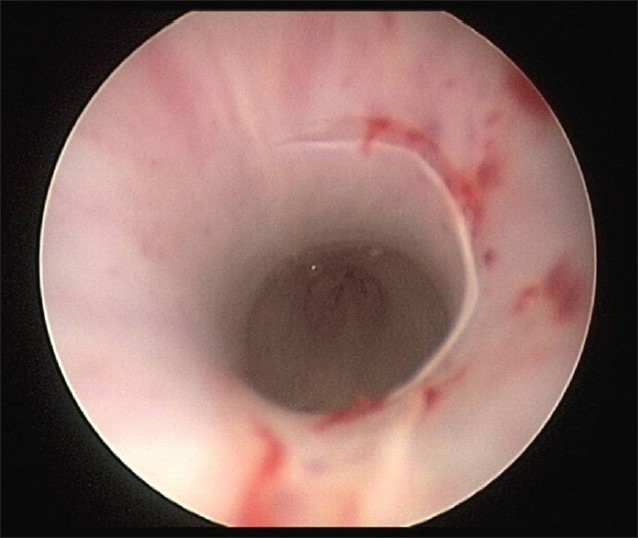
Endoscopic appearance of radial dilation with urethral balloon
RESULTS
A total of 120 patients were analyzed who had short segment urethral stricture. Patient's age ranged from 30 to 85 years (mean, 49.86 years). Follow up was 2 to 60 months (mean, 6 ± 8.1 months). Twelve patients (10%) were not fit for anesthesia, in these patients, the procedure was done under local anesthesia. 79.16% (n = 95) had bulbar, 15.83% (n = 19) had penile, and 5% (n = 6) had membranous strictures.
Average duration of symptoms was 23.6 + 4.1 months (3 months to 43 months). Most common presentation was poor stream of urine in 54.16% (n = 65). Patients presented with retention in 17.6% (n = 21) which required suprapubic catheter. On examination, Balanitis xerotica obliterans changes were seen in 26 patients (21.66%). Microscopic pyuria was detected in 65 patients (54.16%) and positive culture in 39 (32.5%) patients. Preoperative uroflow showed Qmax of 5.7 ± 2.8 ml/sec and PVR of 90.2 ± 103.9. Postoperatively, Qmax improved to 19.1 ± 9.3 ml/sec (0.001*) and PVR decreased to 28.8 ± 40 (0.001*) [Table 1]. Three patients had mild hematuria post procedure. All patients voided well immediately after treatment. Eighty-two patients (of 120) were asymptomatic and did not require auxillary procedures at 6 months.
Table 1.
Improvement in IPSS, Qmax, and PVR
DISCUSSION
Urethroplasty offers patients the greatest chance for cure, the procedure requires surgical expertise, as well as careful patient and procedure selection.[4] Minimally invasive therapies, such as internal urethrotomy, continue to be important first line treatment modalities.[6,7] Although the success rates of internal urethrotomy are inferior to urethroplasty (50% compared to 83%),[2] the ease and safety of urethrotomy make it the procedure of first choice for the treatment of male short segment urethral strictures.[1,2,3] Despite initial enthusiasm for the new technology, laser urethrotomy appears to offer no advantage over conventional internal urethrotomy.[8,9] Few studies have compared the efficacy of metal dilation and internal urethrotomy. In a retrospective study of 199 men with strictures treated at the Mayo Clinic between 1976 and 1990, 101 (67%) underwent dilation and 39 (26%) underwent direct vision internal urethrotomy.[10] At a median follow-up of 3.5 years, the probability of not requiring re-treatment within 3 years was 65% for dilation and 68% for urethrotomy, indicating that these procedures were equally efficacious as initial treatment of bulbar strictures.[10] Urethral metal or bougie dilation offers several advantages over internal urethrotomy. They avoid the need for general, spinal, or intravenous anesthesia. It is a simpler, less-invasive, a potentially office-based procedure that requires lesser degree of surgical expertise and equipment.[10,11] Balloon dilation offers several theoretical advantages over both above mentioned procedures. Balloon dilatation is less traumatic due to its effective radial force during stricture dilatation, thus reduces extravasations and thus subsequent spongiofibrosis.[12] Less urethral trauma may also make the procedure less painful, cause less bleeding, and be better tolerated under local anesthesia. Our results suggest that the recurrence rates in balloon dilatation are comparable to DVIU, suggesting a role of balloon dilatation as a first treatment modality in these short length strictures.[12] The statistically significant improvement in the mean symptom score and the mean maximum urinary flow at one month after balloon dilation is impressive. The short-term retreatment rate are acceptable and compares favorably with that of other published non-operative therapies such as DVIU.[12]
There have been anecdotal reports in the past regarding application of urethral balloon dilation in the management of urethral stricture.[13,14,15] The present series represents the largest series of management of urethral strictures with balloon dilatation. Our results suggest that urethral balloon dilatation is a potential alternative to DVIU.
CONCLUSIONS
Minimally invasive management of urethral stricture with balloon dilation is effective in the management of short segment non-traumatic urethral stricture. Balloon dilatation of the urethra is safe and effective option, short-term success rates are encouraging. Further randomized studies comparing balloon dilatation with DVIU are warranted.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.de Kock ML, Allen FJ. Guidelines for the treatment of urethral strictures. S Afr J Surg. 1989;27:182–4. [PubMed] [Google Scholar]
- 2.Sandozi S, Ghazali S. Sachse optical urethrotomy, a modified technique: 6 years of experience. J Urol. 1988;140:968–9. doi: 10.1016/s0022-5347(17)41900-8. [DOI] [PubMed] [Google Scholar]
- 3.Chilton CP, Shah PJ, Fowler CG, Tiptaft RC, Blandy JP. The impact of optical urethrotomy on the management of urethral strictures. Br J Urol. 1983;55:705–10. doi: 10.1111/j.1464-410x.1983.tb03410.x. [DOI] [PubMed] [Google Scholar]
- 4.Ruutu M, Alfthan O, Standertskjold-Nordenstam CG, Lehtonen T. Treatment of urethral stricture by urethroplasty or direct vision urethrotomy. A comparative retrospective study. Scand J Urol Nephrol. 1983;17:1–4. doi: 10.3109/00365598309179772. [DOI] [PubMed] [Google Scholar]
- 5.Levine LA, Engebrecht BP. Adjuvant home urethral balloon dilation for the recalcitrant urethral stricture. J Urol. 1997;158:818–21. doi: 10.1097/00005392-199709000-00034. [DOI] [PubMed] [Google Scholar]
- 6.Webster GD, Koefoot RB, Sihelnik SA. Urethroplasty management in 100 cases of urethral stricture: A rationale for procedure selection. J Urol. 1985;134:892–8. doi: 10.1016/s0022-5347(17)47512-4. [DOI] [PubMed] [Google Scholar]
- 7.Fourcade RO, Mathieu F, Chatelain C, Jardin A, Richard F, Kuss R. Endoscopic internal urethrotomy for treatment of urethral strictures. Urology. 1981;18:33–6. doi: 10.1016/0090-4295(81)90491-x. [DOI] [PubMed] [Google Scholar]
- 8.Devine CJ, Jr, Devine PC, Horton CE. Anterior urethral injury: Etiology, diagnosis, and initial management. Urol Clin North Am. 1977;4:125–31. [PubMed] [Google Scholar]
- 9.Becker HC, Miller J, Noske HD, Klask JP, Weidner W. Transurethral laser urethrotomy with argon laser: Experience with 900 urethrotomies in 450 patients from 1978 to 1993. Urol Int. 1995;55:150–3. doi: 10.1159/000282774. [DOI] [PubMed] [Google Scholar]
- 10.Vicente J, Salvador J, Caffaratti J. Endoscopic urethrotomy versus urethrotomy plus Nd-YAG laser in the treatment of urethral stricture. Eur Urol. 1990;18:166–8. doi: 10.1159/000463901. [DOI] [PubMed] [Google Scholar]
- 11.Stormont TJ, Suman VJ, Oesterling JE. Newly diagnosed bulbar urethral strictures: Etiology and outcome of various treatments. J Urol. 1993;150:1725–8. doi: 10.1016/s0022-5347(17)35879-2. [DOI] [PubMed] [Google Scholar]
- 12.Steenkamp JW, Heyns CF, de Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: A prospective, randomized comparison. J Urol. 1997;157:98–101. [PubMed] [Google Scholar]
- 13.MacDiarmid SA, Harrigan CT, Cottone JL, McIntyre WJ, Johnson DE. Assessment of a new transurethral balloon dilation catheter in the treatment of urethral stricture disease. Urology. 2000;55:408–13. doi: 10.1016/s0090-4295(99)00541-5. [DOI] [PubMed] [Google Scholar]
- 14.Giesy JD, Finn JC, Hermann GD, Kinney TB, Fogarty TJ. Coaxial balloon dilation and calibration of urethral strictures. Am J Surg. 1984;147:611–4. doi: 10.1016/0002-9610(84)90124-7. [DOI] [PubMed] [Google Scholar]
- 15.Daughtry JD, Rodan BA, Bean WJ. Balloon dilatation of urethral strictures. Urology. 1988;31:231–3. doi: 10.1016/0090-4295(88)90147-1. [DOI] [PubMed] [Google Scholar]


