Abstract
A 77-year-old female, who suffered from rheumatoid arthritis and hypothyroidism, developed severe muscle weakness. Clinical features, blood results and muscle biopsy suggested a possible diagnosis of dermatomyositis. A computed tomography of the chest, abdomen and pelvis showed a solid mass in the left kidney. She underwent a left laparoscopic nephrectomy and histology confirmed conventional (clear cell) renal cell carcinoma. She recovered slowly and almost back to normal life after 6 months. Early appreciation of the typical skin rash may provide a clue to the diagnosis and screening for neoplasm may improve prognosis.
Keywords: Dermatomyositis, laparoscopic, nephrectomy, renal cancer
INTRODUCTION
Dermatomyositis (DM) is an autoimmune disorder associated with idiopathic inflammatory myopathy and a characteristic rash with an overall incidence of 9.63 per 1,000,000.[1] DM is associated with neoplasm in 15-60% of cases which may pre-date, peri-date or post date the onset of myositis.[2,3] In 1916, first two cases of malignancy-associated DM were reported by Stertz,[4] who described a patient with gastric carcinoma, and Kankeleit,[5] who reported on a female with DM associated with breast carcinoma. The most commonly observed cancers in female patients with DM are breast and gynecologic cancers, whereas the most commonly observed cancer in male patients with DM is lung cancer. The most common cancer types noted were adenocarcinomas.[2] Interestingly, nasopharyngeal carcinoma is most common in South-East Asia.[6,7] Cancer screening is usually recommended in these patients.[2,6,7] Treatment usually includes systemic corticosteroids, alone or in combination, with immunosuppressive agents. There is a paucity of published data on the association of renal cell carcinoma with DM and the effect of immunosuppressive therapy in treatment.
CASE REPORT
A 77-years-old Caucasian lady, with known rheumatoid arthritis and hypothyroidism, presented with a 4 months history of facial rash and progressive muscle weakness affecting the legs more than the arms. Examination revealed Gottron papules (erythematous papules on the dorsal surface of the phalangeal joints), heliotrope rash (oedematous erythema of the eyelids) and proximal muscle weakness [Figure 1]. Blood biochemistry revealed a creatine kinase (CK) level of >6000 U/L (normal 0-70 U/L) and positive ANA (Antinuclear Antibody). The electromyography (EMG) studies and a muscle biopsy were subsequently performed. The EMG showed signs of severe myopathic features. The needle EMG examination showed profuse spontaneous activities affecting the upper and lower limb muscles indicating an active stage of myositis. The muscle biopsy showed infiltration of the muscle fibres by lymphocytes and macrophages associated with muscles fibres necrosis. In view of these findings, a diagnosis of dermatomyositis was made. The patient was admitted due to the severe muscle weakness and was commenced on high dose steroids and intravenous immunoglobulins (IV-IG) without any significant benefit. Cancer screening was undertaken and a staging computed tomography (CT) of the chest, abdomen and pelvis revealed a 4 cm upper pole solid mass on the left kidney, suggestive of renal cell carcinoma. She was referred to urology and underwent a laparoscopic nephrectomy four weeks after presentation. Histopathology confirmed conventional (clear cell) renal cell carcinoma with focal nuclear changes accounting to Fulham grade 2. The carcinoma was confined to the kidney with no evidence of lympho-vascular invasion (stage pT1 a). Following the nephrectomy the patient was continued on steroids and had further monthly IV IG. Within four weeks of the nephrectomy her CK had improved to less than 200 U/L and there was a significant improvement in muscle strength [Figure 2]. She remained in hospital for 3 months during which she made a remarkable recovery with the disappearance of the rash, normalisation of CK levels and consistently improving muscle power. She was discharged on a reducing dose of prednisolone and within 6 months was back to normal life.
Figure 1.

Patient at presentation. (a) heliotrope rash and malar erythema, (b) Shawl sign, (c) poikiloderma vasculare atrophicans, (d) Gottrons papules, (e) paronychial erythema
Figure 2.
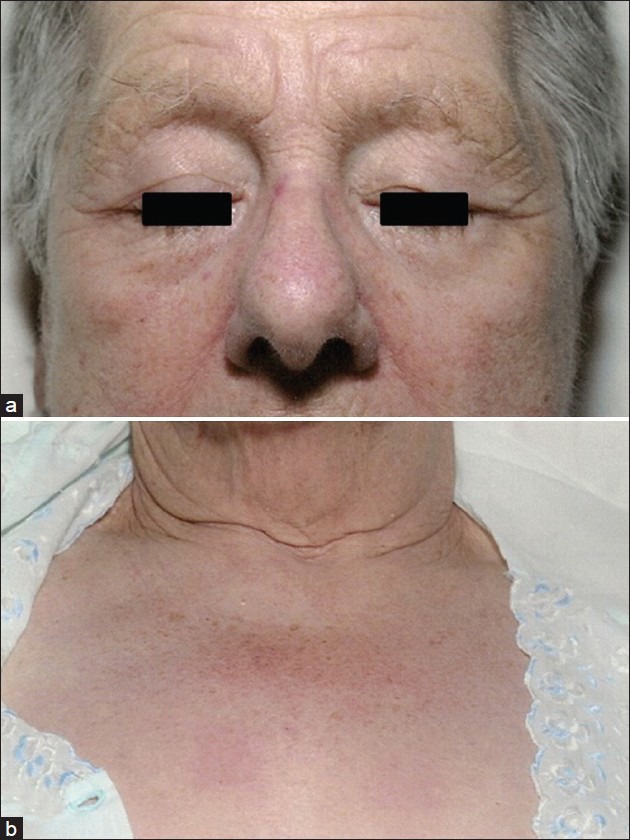
patient 4 weeks after nephrectomy with disappearance of the heliotrope rash (a) and upper chest erythema (b)
DISCUSSION
Dematomyositis has been reported to be associated with malignancies. An underlying mechanism of the association between DM and malignancies remains unclear. A model of crossover immunity for the development of cancer-associated myositis has been proposed recently. Common antigenic myositis-specific autoantigens were expressed in both tumour cells and undifferentiated myoblasts. Myositis-specific autoantigen expression in a nascent tumour leads to the generation of both specific T cells and B cells against those antigens, and then to successful anti-tumour immunity.[8,9]
It is rare for dermatomyositis to be associated with renal cancers. Our case illustrates the potential role of nephrectomy in cases of DM induced renal cell carcinoma (RCC) as there was no improvement with medical therapy prior to surgery. There was a previous case report of RCC–associated dermatomyositis treated successfully with renal arterial embolisation and percutaneous radiofrequency heat ablation (RFA).[10] A case of DM associated with RCC carcinoma was also reported by a Spanish group.[11] There have been two reports of polymyositis associated with RCC. One of them had slight improvement in the myopathic symptoms after having nephrectomy.[12] While with the other a distinct regression of the myopathic symptoms noted after the nephrectomy, but with the development of metastases the symptoms increased again.[13]
Various authors have suggested predictive factors that may indicate underlying malignancy in patients with DM; (a) Age > 40 years (b) pruritus (c) necrotic ulcerative skin lesions (d) perionycial erythema (e) blisters on extremities (f) dysphagia (h) elevated ESR (i) high C-reactive protein (j) low serum albumin (k) elevated CA [cancer antigen] 125 (l) poor response to corticosteroid therapy.[2,6,7,14] Of these, the patient we are reporting had 6 factors with the poor response to corticosteroid therapy probably being the most significant. There is no consensus regarding what cancer screening, when and how frequently tests should be performed. As a result, recommendations vary widely, and range from advising careful clinical examination and routine laboratory screening, to extensive invasive investigations. In view of the increased risk of cancer in addition to routine examination, gynaecological examination, laboratory screening (CA 125, CEA [carcinoembryonic antigen], AFP [alpha-fetoprotein], CA [cancer antigen] 19-9), faecal blood testing, mammography, CT chest, abdomen and pelvis are justified in those with dermatomyositis. Examination of nasopharynx should be done in Asian patients with DM. Recently a study reported using combined fluorodeoxyglucose (FDG)-Positron emission tomography (PET)/computed tomography (FDG-PET/CT), is one of the most sensitive single imaging techniques to detect occult malignancy. Authors observed positive and negative predictive values for the diagnosis of cancer were 85.7% and 93.8%, respectively.[15] Since the risk of malignant disease remains high for many years after diagnosis, vigilance needs to be maintained.[2,6,7]
ACKNOWLEDGMENT
The Author would like to thank the patient for providing consent to use her photograph in this article.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Bendewald MJ, Wetter DA, Li X, Davis MD. Incidence of dermatomyositis and clinically amyopathic dermatomyositis: a population-based study in Olmsted County, Minnesota. Arch Dermatol. 2010;146:26–30. doi: 10.1001/archdermatol.2009.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill CL, Zhang Y, Sigurgeirsson B, Pukkala E, Mellemkjaer L, Airio A, et al. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001;357:96–100. doi: 10.1016/S0140-6736(00)03540-6. [DOI] [PubMed] [Google Scholar]
- 3.Goh CL, Rajan VS. Dermatomyositis in a skin clinic. Ann Acad Med Singapore. 1983;12:6–12. [PubMed] [Google Scholar]
- 4.Stertz G. Polymyositis. Berl Klin Wochenschr. 1916;53:489. [Google Scholar]
- 5.Kankeleit H. Über primaire nichteitrige polymyositis. Dtsch Arch Klin Med. 1916;120:335–9. [Google Scholar]
- 6.Liu WC, Ho M, Koh WP, Tan AW, Ng PP, Chua SH, et al. An 11-year review of dermatomyositis in Asian patients. Ann Acad Med Singapore. 2010;39:843–7. [PubMed] [Google Scholar]
- 7.Chen YJ, Wu CY, Huang YL, Wang CB, Shen JL, Chang YT. Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan. Arthritis Res Ther. 2010;12:R70. doi: 10.1186/ar2987. Epub 2010 Apr 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dankó K, Ponyi A, Molnar AP, András C, Constantin T. Paraneoplastic myopathy. Curr Opin Rheumatol. 2009;21:594–8. doi: 10.1097/BOR.0b013e3283317fa5. [DOI] [PubMed] [Google Scholar]
- 9.Levine SM. Cancer and myositis: new insights into an old association. Curr Opin Rheumatol. 2006;18:620–4. doi: 10.1097/01.bor.0000245721.02512.77. [DOI] [PubMed] [Google Scholar]
- 10.Schaefer O, Lohrmann C, Harder J, Veelken H, Langer M. Treatment of renal cell carcinoma-associated dermatomyositis with renal arterial embolization and percutaneous radiofrequency heat ablation. J Vasc Interv Radiol. 2004;15:97–9. doi: 10.1097/01.rvi.0000114833.75873.25. [DOI] [PubMed] [Google Scholar]
- 11.Benages Pamies J, Cecchini Rosell L, Sanfeliu Cortés F, Comet Batlle J, Saladie Roig JM. Dermatomyositis and small cell tumor of the kidney. Actas Urol Esp. 1997;21:67–70. [PubMed] [Google Scholar]
- 12.Kumasaka K, Nomura K, Satoh S, Fujioka T, Kubo T, Sasou S. A case of renal cell carcinoma with polymyositis. Hinyokika Kiyo. 1990;36:1317–20. [PubMed] [Google Scholar]
- 13.Wurzer H, Brandstätter G, Harnoncourt K, Kullnig P, Kleinert R. Paraneoplastic polymyositis associated with a renal carcinoma. J Intern Med. 1993;234:521–4. doi: 10.1111/j.1365-2796.1993.tb00787.x. [DOI] [PubMed] [Google Scholar]
- 14.Marie I, Hatron PY, Levesque H, Hachulla E, Hellot MF, Michon-Pasturel U, et al. Influence of age on characteristics of polymyositis and dermatomyositis in adults. Medicine (Baltimore) 1999;78:139–47. doi: 10.1097/00005792-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Selva-O’Callaghan A, Grau JM, Gámez-Cenzano C, Vidaller-Palacín A, Martínez-Gómez X, Trallero-Araguás E, et al. Conventional cancer screening versus PET/CT in dermatomyositis/polymyositis. Am J Med. 2010;123:558–62. doi: 10.1016/j.amjmed.2009.11.012. [DOI] [PubMed] [Google Scholar]


