Abstract
Self-mutilations of the external genitals in psychiatric patients also known as Klingsor syndrome is a rare urologic trauma. Men with religious conflicts, low self-esteem, unresolved transsexual issues and feelings of guilt are the most vulnerable. This condition requires immediate surgical intervention. Currently replantation involves meticulous microsurgery and has become the primary method for managing these patients. In this paper, we report a case of self amputation of penis in a patient with a psychiatric history significant for schizopfrenia. Because of the unavailability of a microscope in our department, a non-microsurgical replantation without microscopic magnification was attempted. After surgery, normal appearance and function including a good normal voiding, sensation, and erections were observed.
Keywords: Amputation, penis, replantation methods
INTRODUCTION
Penile amputation is a rare injury, frequently due to self-mutilation in patients suffering from psychotic troubles, especially schyzophrenia. Three particular groups with risk of genital self-mutilation were initially identified by Blacker and Wong:[1] schizophrenics, transvestites, and men with religious or cultural conflicts. All races, religions and cultures were concerned.
The first report of genital self mutilation (GSM) was in 1901 by Strock.[2]
The current standard of treatment for this infrequent injury is replantation with approximation of the urethra, cavernosal bodies, and microsurgical dorsal vein, artery and nerve anastomosis. This technique is considered to reduce the immediate and long-term post-operative complications.
We report a case of self-amputation of the penis with successful surgical repair and complete functional recovery without the use of operating microscope.
CASE REPORT
A 29-year-old man, unmarried, with a history of schizoaffective personality disorder, but non-compliant with the antidepressant and antipsychotic medication, was admitted for self-cutting of penis 2 cm distal from the mons of the pubis.
At the admission, mental examination revealed apathetic and conscious patient but uncooperative. Eye contact was poor, speech was inaudible. There was no suicidal intent.
At the urological examination, we found a subtotal cut of the penis, interesting the anterior and lateral parts of the penile skin, and a clear cut trough cavernosal bodies, and urethra. The penis remained suspended only by a thin posterior part of the skin [Figures 1 and 2]. The patient received two intravenous antibiotics.
Figure 1.

Mutilation of the penis: The penis remained suspended only by a thin posterior part of the skin
Figure 2.
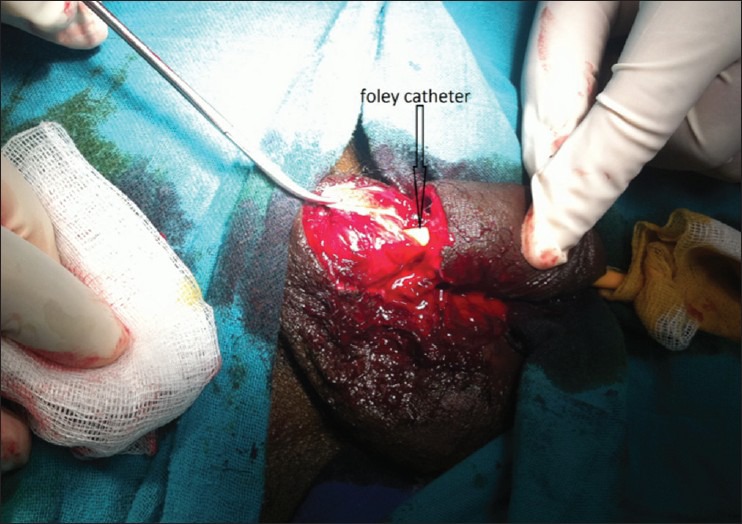
Foley catheter showing the complete urethral section
Immediately the patient was addressed in the operating room. The microsurgery was not available and the only chance to attempt to save the functionality of the organ was a non-microsurgical replantation of the amputated penis. A suprapubic cystostomy was first performed. The operation started about 5 hours after the trauma.
A 16-Fr silicon catheter was inserted through the urethra of the amputated part and the proximal urethral stump and passed on into the bladder. End-to-end urethral anostomosis was made with a two-layer closure over a using 5-0 polyglycolic acid [Figure 3].
Figure 3.

A 16-Fr silicon catheter was inserted through the urethra of the amputated part and the proximal urethral stump and passed on into the bladder
Afterwards the cavernous bodies of the penis were connected with 3-0 polyglycolic acid continuous suture.
We did not perform anastomosis of the dorsal vein, artery or the nerve. Buck's and dartos fascia were reapproximated, and the skin was closed.
The patient was transferred to the inpatient psychiatric unit for further management.
Twenty-four hours after the surgery, we did not observe any skin necrosis and the urethral mucosa showed a reassuring pink colour.
One week after the surgery, the patient in an agitation crisis pulled up his foley catheter.
We removed the cystostomy catheter 2 weeks later, after that the normal micturation was acquired.
The clinical exam 1 month after surgery showed a viable penis [Figures 4 and 5], with a pink urethral mucosa, and a normal sensation. The patient reported normal micturition and spontaneous morning erections 3 months after surgery. Those results were maintained 1 year after surgery.
Figure 4.

Pink urethral mucosa 1 month after surgery
Figure 5.

The penis 1 month after surgery showing no skin necrosis
During the psychiatric interview patient reported that the act was preceded by religious delusions and hallucinations: He was hearing voices and feeling guilty, and thought that God would punish him.
The psychiatrist ordered lithium 900 mg/day, sertraline 50 mg/day and risperidone 3 mg/day. The patient was fully remitted at the first month.
DISCUSSION
Jezior et al. Classified penile amputation into three groups: Self-mutilation, criminal amputation, and a traumatic accident.[3]
The eponym Klingsor syndrome has been used to describe the act of genital self-mutilation associated with religious delusions.
The name ‘Klingsor’ was based on a fictitious character in Wagner's opera where Klingsor was a magician who castrated himself because of his inability to remain chaste in order to be accepted from the Knights of the Grail.
Schweitzer[4] has suggested expanding the definition of this syndrome to include genital self mutilation (GSM) resulting from all delusional syndromes.
Blacker and Wong[1] identified six risk factors for male GSM: (1) Absence of a competent male figure for identification during the early developmental period, (2) over-controlling mothers who encouraged their sons’ masochistic behaviors, (3) pathological feminine behaviors of the male child, (4) repudiation of body image (especially the penis), (5) unresolved sexual conflicts and (6) anxiety and feelings of guilt often relieved by GSM. Recently Atonement is proposed as a new concept in formulating religiously themed psychotic male genital self mutilation.[5]
These patients show a high tendency to repeating self-aggressive actions, especially when their pharmacotherapy is discontinued.[6,7]
Since 1970, 23 cases of penile self-mutilations were described with successful microsurgical repair.[8]
Two different clinical cases can be seen in the emergency department: The amputated penis is brought, or has not been found by the witness. These situations suggest different treatment: Replanting the amputated organ, plastic surgery of the remaining stump, or a total replacement.[9]
Some conditions are required for replanting the amputated penis and forecast the success of surgery: Viability state of the organ, condition of the graft bed, or penile stump at the time of injury. The amputated part is to be wrapped in saline-soaked gauze and placed in a sterile bag.[10]
Currently replantation involves meticulous microsurgery to reduce skin, urethra and graft loss, and enables to repair vessels and neurologic injuries and permit better results on preserving the sensation of the organ, micturition and erectile function but complications may still occur.[11]
Indeed, a recent review has found that the value of microsurgical techniques to be uncertain.[12] It seems that a repair of a single dorsal penile artery is more important than a single or multiple profundi arteries and hence microscopic and non-microscopic repairs may permit the same results.[13]
Naraynsingh describes penile replantation in a 24-year-old mentally challenged patient using 4.59 loupe-magnification to restore a functional, fully erectile penis without tissue loss and a 20-year problem free follow-up.[14]
Non-microsurgical techniques have been employed with good postoperative outcomes. Ehrich reported the first case of replantation of an amputated penis in 1929.[15] An initial complication of penile replantation was excessive skin loss. McRoberts et al. in 1968[16] described a technique to improve the skin complications by débriding the native penile skin at the time of replantation and burying the denuded penis into the scrotum. After this technique improvement partial glans loss was seen in only one of four patients while complete skin loss occurred in 8 of 14 cases in the Thai series and 4 of 14 had partial skin loss, and 6 of 14 partial glans loss.[17] In theses series, the number of urethral strictures was also high, occurring in four of seven complete amputations and five of eight partial amputations.
In our situation no vessels or nerves anastomosis were done in consequence of other reason than medical (microsurgery was not available). Despite this, non-microsurgical replantation was effective with good functional results after 1 year of follow-up. This result is supported by the series of Carrol et al.[18] including 38 penile replantation after partial and complete amputation that found preservation of erectile function and the ability for intromission in all cases.
CONCLUSION
The klingsor syndrom is rare. The replantation of the penis is always recommended. Replantation of penis with application of microsurgery techniques of vessels and nerves connecting is the gold standard. Although if microsurgery is not available, non-microsurgical treatment has to be attempted.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Blacker KH, Wong N. Four cases of autocastration. Arch Gen Psychiatry. 1963;8:169–76. doi: 10.1001/archpsyc.1963.01720080059009. [DOI] [PubMed] [Google Scholar]
- 2.Eke N. Genital self-mutilation: There is no method in this madness. BJU Int. 2000;85:295–8. doi: 10.1046/j.1464-410x.2000.00438.x. [DOI] [PubMed] [Google Scholar]
- 3.Jezior JR, Brady JD, Schlossberg SM. Management of penile amputation injuries. World J Surg. 2001;25:1602–9. doi: 10.1007/s00268-001-0157-6. [DOI] [PubMed] [Google Scholar]
- 4.Schweitzer I. Genital self-mutilation and Klingsor syndrome. Aust N Z J Psychiatry. 1990;24:6–9. doi: 10.3109/00048679009062914. http://www.ncbi.nlm.nih.gov/pubmed/2073234 . [DOI] [PubMed] [Google Scholar]
- 5.Ozan E, Deveci E, Oral M, Yazici E, Kirpinar I. Male genital self-mutilation as a psychotic solution. Isr J Psychiatry Relat Sci. 2010;47:297–303. [PubMed] [Google Scholar]
- 6.Greilsheimer H, Groves JE. Male genital self-mutilation. Arch Gen Psychiatry. 1979;36:441–6. doi: 10.1001/archpsyc.1979.01780040083009. [DOI] [PubMed] [Google Scholar]
- 7.Bhargava SC, Sethi S, Vohra AK. Klingsor syndrome: A case report. Indian J Psychiatry. 2001;43:349–50. [PMC free article] [PubMed] [Google Scholar]
- 8.Szasz G, McLoughlin MG, Warren RJ. Return of sexual functioning following penile replant surgery. Arch Sex Behav. 1990;19:343–8. doi: 10.1007/BF01541929. [DOI] [PubMed] [Google Scholar]
- 9.Ozturk A, Kilinc M, Guven S, Gormus N, Belviranli M, Kaynar M, et al. Penis replantation after self-mutilation. Int Urol Nephrol. 2009;41:109–11. doi: 10.1007/s11255-008-9374-3. Epub 2008 Jun 24. [DOI] [PubMed] [Google Scholar]
- 10.Hayhurst JW, O›Brien BM, Ishida H, Baxter TJ. Experimental digital replantation after prolonged cooling. Hand. 1974;6:134–41. doi: 10.1016/0072-968x(74)90077-1. [DOI] [PubMed] [Google Scholar]
- 11.Darewicz B, Galek L, Darewicz J, Kudelski J, Malczyk E. Successful microsurgical replantation of an amputated penis. Int Urol Nephrol. 2001;33:385–6. doi: 10.1023/a:1015226115774. [DOI] [PubMed] [Google Scholar]
- 12.Volkmer BG, Maier S. Successful penile replantation following autoamputation: Twice! Int J Impot Res. 2002;14:197–8. doi: 10.1038/sj.ijir.3900842. [DOI] [PubMed] [Google Scholar]
- 13.Lowe MA, Chapman W, Berger RE. Repair of a traumatically amputated penis with return of erectile function. Urol J. 1991;145:1267–70. doi: 10.1016/s0022-5347(17)38597-x. [DOI] [PubMed] [Google Scholar]
- 14.Naraynsingh V, Harnarayan P, Hariharan S. Successful penile replantation using loupe magnification. Int Urol Nephrol. 2011;43:437–9. doi: 10.1007/s11255-010-9761-4. [DOI] [PubMed] [Google Scholar]
- 15.Ehrich WS. Two unusual penile injuries. J Urol. 1929;21:239. [Google Scholar]
- 16.McRoberts JW, Chapman WC, Ansell JS. Primary anastomosis of the traumatically amputated penis: Case report and summary of the literature. J Urol. 1968;100:751–4. doi: 10.1016/s0022-5347(17)62617-x. [DOI] [PubMed] [Google Scholar]
- 17.Bhanganada K, Chayavatana T, Pongnumkul C, Tonmukayakul A, Sakolsatayadorn P, Komaratat K, et al. Surgical management of an epidemic of penile amputations in Siam. Am J Surg. 1983;146:376–82. doi: 10.1016/0002-9610(83)90420-8. [DOI] [PubMed] [Google Scholar]
- 18.Carroll PR, Lue TF, Schmidt RA, Trengrove-Jones G, McAninch JW. Penile replantation: Current concepts. J Urol. 1985;133:281–5. doi: 10.1016/s0022-5347(17)48918-x. [DOI] [PubMed] [Google Scholar]


