Sir,
Urinary tract infection (UTI) continues to be the commonest nosocomial infection according for approximately 40% of all hospital acquired infections and it is one of the most important causes of morbidity and mortality.[1,2] The genus Citrobacter is distinct group of aerobic, gram negative bacilli from the Enterobacteriaceae family, widely distributed in water, soil, food and intestinal tract of man and animals. UTIs caused by Citrobacter species have been described in 5 to 12% of bacterial urine isolates in adults.[3,4,5] We report here the emergence of Citrobacter as an increasingly common urinary pathogen in hospitalized patients.
A retrospective analysis was carried out in patients with urine culture positive for Citrobacter species from January, 2009 to December, 2010. Patients were identified and studied with respect to age, gender, underlying medical conditions, method of urine collection, and clinical presentations. Identification of isolates was done using standard microbiological techniques.[6] All isolates were tested for susceptibility to antimicrobial agents on Mueller Hinton agar by the standard disc diffusion method, recommended by the Clinical and Laboratory Standards Institute (CLSI).[7]
Of the 4,126 urine samples received for culture during the study period, significant bacteriuria was found in 747 (18.1%) samples. Among the 747 culture positive samples, the number of bacterial isolates obtained were 809 (716 had a single pathogen and 31 has two types of bacteria grown on culture). Citrobacter isolates were found to be third most common organism causing UTI in hospitalized patients after Escherichia coli and Klebsiella species accounting to 9.4% of all isolates. C. koseri (72.4%) was the predomint organism among the two Citrobacter species. Similar to the results of the other researchers, Citrobacter accounted for 9.4% of all UTIs in hospitalized patients in the current study.[3,4,5]
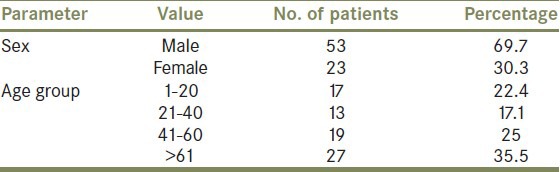
Most of the patients (55%) in whom Citrobacter was isolated had been subjected to in dwelling urethral catheterization or genitourinary instrumentation or had an obstructive uropathy. The highest incidence among various age groups was found in elderly hospitalized patients [Table 1] specially males. The possible reasons for high frequency in elderly male include obstructive uropathy due to prostrate enlargement, loss of bactericidal activity of prostatic secretions, frequent genitourinary instrumentation and catheterization.
Table 1.
Characteristics of patients
The antibiotic susceptibility showed discouraging pattern with multidrug resistance as a common problem. Amoxycillin and ampicillin are often used as oral therapy for gram-negative UTIs, but the high rate of in vitro resistance demonstrated in this study and others suggests that they should not be used. Trimethoprim and amoxiclav are also often prescribed; of concern is the increasing rate of resistance to trimethoprim over the last 10 years and the more recent increase in resistance to amoxyclav, presumably as a result of mechanisms other than production of beta-lactamase.[8] Majority of the urinary tract isolates were found to be resistant to cefotaxime, cephalaxin, norfloxacin, ciprofloxacin, and the aminoglycosides [Figure 1]. This has important implications as patients in a tertiary care hospital like ours receive cephalosoprins, aminoglycosides, fluoroquinolone, or a combination of these drugs as empirical therapy or as definitive treatment. Since good in vitro activity was shown by nitrofurantoin it may be considered as first line oral therapy for ambulatory patients. The high rates of antibiotic resistance observed in the present study may be due to the fact that ours is a tertiary care hospital with widespread usage of broad spectrum antibiotics leading to selective survival advantage of pathogens.
Figure 1.
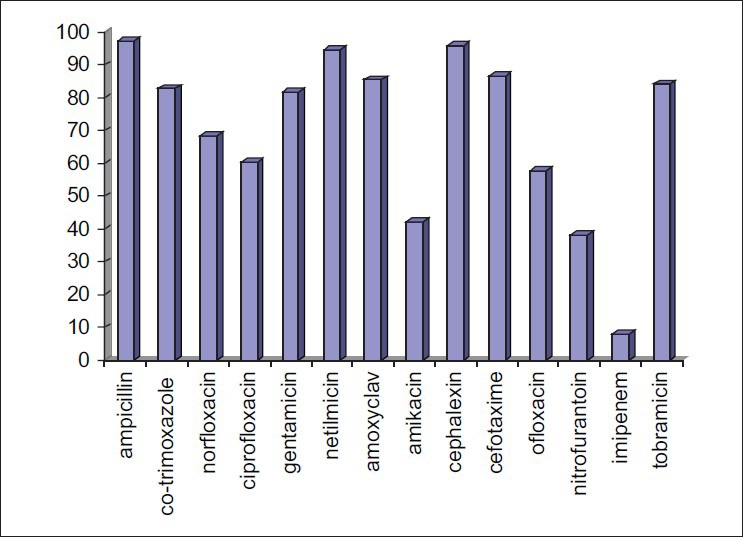
Antimicrobial resistance (%) of the Citrobacter isolates
The emergence of this usually rare organism as the third most common urinary pathogen, which is resistant to commonly available antibiotics is alarming. The indiscriminate use of antimicrobial agents and frequent genitourinary instrumentation are possibly responsible for this situation. Many such infections could be prevented by selective judicious use of urinary catheters as well as careful attention to underlying abnormalities in the urinary tract and by continuously evaluating susceptibility pattern of uropathogens to traditional as well as new antimicrobials in well-defined populations and limiting inappropriate and injudicious use of antibiotics so as to prevent further emergence of drug resistance.
REFERENCES
- 1.Cox CE. Nosocomial urinary tract infections. Urology. 1988;32:210–5. doi: 10.1016/0090-4295(88)90386-x. [DOI] [PubMed] [Google Scholar]
- 2.Steadman R, Topley N. The virulence of Escherichia coli in urinary tract. In: Brumfitt W, Jeremy MT, Hamilton Miller, editors. Urinary tract infections. 1st ed. London: Chapman and Hall; 1998. pp. 37–41. [Google Scholar]
- 3.Barton LL, Walentik CW. Citrobacter diversus urinary tract infection. Am J Dis Child. 1982;136:467–8. doi: 10.1001/archpedi.1982.03970410085023. [DOI] [PubMed] [Google Scholar]
- 4.Lipsky BA, Hook EW, 3rd, Smith AA, Plorde JJ. Citrobacter infections in humans: experience at Seattle Veterans Administration Medical Centre and review of literature. Rev Infect Dis. 1980;2:746–60. doi: 10.1093/clinids/2.5.746. [DOI] [PubMed] [Google Scholar]
- 5.Whitby JL, Muir GG. Bacteriological studies of urinary tract infection. Br J Urol. 1961;33:130–4. doi: 10.1111/j.1464-410x.1961.tb11595.x. [DOI] [PubMed] [Google Scholar]
- 6.Murray PR, Holmes B, Aucken HM. Citrobacter, Enterobacter, Klebsiella, Plesiomonas, Serratia, and other members of the Enterobacteriaceae. In: Borriello SP, Murray PR, Funke G, editors. Topley and Wilson's Microbiology and Microbial Infections. 10th ed. London: Hodder Arnold; 2005. pp. 1474–506. [Google Scholar]
- 7.Wayne, PA: CLSI document; 2005. Clinical and Laboratory Standards Institute performance standards for antimicrobial susceptibility testing. Fifteenth informational supplement; pp. M100–S15. [Google Scholar]
- 8.Gales AC, Jones RN, Gordon A, Sader HS, Wilke WW, Beach ML, et al. Activity and spectrum of 22 antimicrobial agents tested against urinary tract infection pathogens in hospitalized patients in Latin America: Report from the second year of the SENTRY Antimicrobial Surveillance Program (1998) J Antimicrob Chemother. 2000;45:295–303. doi: 10.1093/jac/45.3.295. [DOI] [PubMed] [Google Scholar]


