Abstract
OBJECTIVE
The study objective was to evaluate the cost-effectiveness of alternative fasting plasma glucose (FPG) thresholds to identify adults at high risk for type 2 diabetes for diabetes preventive intervention.
RESEARCH DESIGN AND METHODS
We used a validated simulation model to examine the change in lifetime quality-adjusted life years (QALYs) and medical costs when the FPG threshold was progressively lowered in 5-mg/dL decrements from 120 to 90 mg/dL. The study sample includes nondiabetic adults aged ≥45 years in the United States using 2006–2010 data from the National Health and Nutrition Examination Survey. High-risk individuals were assumed to receive a lifestyle intervention, as that used in the Diabetes Prevention Program. We calculated cost per QALY by dividing the incremental cost by incremental QALY when lowering the threshold to the next consecutive level. Medical costs were assessed from a health care system perspective. We conducted univariate and probabilistic sensitivity analyses to assess the robustness of the results using different simulation scenarios and parameters.
RESULTS
Progressively lowering the FPG threshold would monotonically increase QALYs, cost, and cost per QALY. Reducing (in 5-mg/dL decrements) the threshold from 120 to 90 mg/dL cost $30,100, $32,900, $42,300, $60,700, $81,800, and $115,800 per QALY gained, respectively. The costs per QALY gained were lower for all thresholds under a lower-cost and less-effective intervention scenario.
CONCLUSIONS
Lowering the FPG threshold leads to a greater health benefit of diabetes prevention but reduces the cost-effectiveness. Using the conventional benchmark of $50,000 per QALY, a threshold of 105 mg/dL or higher would be cost effective. A lower threshold could be selected if the intervention cost could be lowered.
Impaired fasting glucose (IFG) is an intermediate state of hyperglycemia in which fasting plasma glucose (FPG) levels do not meet the criteria for diabetes but are consistently elevated above what is considered normal (1). The concept of IFG has been endorsed by leading professional organizations (2,3) and adopted as one measure for identifying the high-risk population for type 2 diabetes preventive interventions in clinical settings and large-scale, community-based prevention programs (4,5).
Despite the increasing use of FPG testing to identify the high-risk state, the appropriate threshold for the lower limit of IFG remains unclear. The American Diabetes Association (ADA) currently uses 100 mg/dL (5.6 mmol/L) as the threshold to define IFG (6), while the World Health Organization and the European Diabetes Epidemiology Group recommends using 110 mg/dL (6.1 mmol/L) (7). Varying standards exist in large part because there is no clear threshold at which an FPG value can be associated with a sharp increase in the risk of future diabetes and its complications (7–10). Recent ADA guidelines also recommend glycated hemoglobin (A1C) as a blood test to identify people at high risk for type 2 diabetes and such a continuous relationship with the incidence of diabetes and its complications also has been observed for A1C (6).
When FPG is used to identify the target population for type 2 diabetes prevention, the choice of the IFG-defining FPG threshold ultimately affects the intervention’s cost-effectiveness. A lower FPG threshold would result in more people being eligible for intervention, which would likely lead to more cases of diabetes being prevented or delayed. However, a lower threshold might be less cost-effective because it incurs costs for intervening in a population with a lower risk of developing type 2 diabetes. To better understand the potential cost implications, major clinical and public health organizations called for systematic economic analyses of the FPG thresholds (3). Our study sought to estimate and compare the long-term cost-effectiveness of alternative FPG thresholds for identifying high-risk adults for inclusion in type 2 diabetes prevention programs.
RESEARCH DESIGN AND METHODS
Using the model described below, we simulated average lifetime costs and quality-adjusted life years (QALYs) for U.S. adults aged ≥45 years who had no diabetes at baseline under scenarios using alternative FPG thresholds. For each scenario, the FPG threshold was lowered by 5 mg/dL from that in the previous scenario. We calculated results for seven scenarios with FPG thresholds ranging from 120 to 90 mg/dL. Thresholds <90 mg/dL were not considered because such a standard would identify a vast majority of the U.S. population as high risk. Lifetime cost and QALY estimates from each scenario were used to estimate the cost-effectiveness associated with each threshold.
Simulation model
Our model is a validated Markov-based model in which the progression of type 2 diabetes was simulated based on annual transition probabilities from a person’s diagnosis to death. In the model, separate modules simulated incidence of and progression through each of five types of diabetes complication (nephropathy, neuropathy, retinopathy, stroke, and coronary heart diseases) that people with diabetes could possibly develop. Details of the model appear in the Supplementary Data. The model has been validated (11) and used for assessing the long-term cost-effectiveness of various interventions for preventing type 2 diabetes and its complications (12–15).
A nationally representative sample of nondiabetic U.S. adults aged ≥45 years, based on the 2006–2010 data from the National Health and Nutrition Examination Survey, was used for the simulations. We did not include people younger than 45 years because data concerning diabetes incidence by FPG level in this population are limited and relatively few people are diagnosed with type 2 diabetes before age 45 (16). We identified people with diabetes by self-report or by test results: FPG ≥126 mg/dL, 2-h glucose value ≥200 mg/dL, or A1C ≥6.5% (6).
For each decremental 5 mg/dL FPG value (threshold i, e.g., threshold115) evaluated in our simulations, the nondiabetic sample was divided into two groups: those at high risk for type 2 diabetes (threshold i < FPG < 126 mg/dL) and those with “normal” FPG (FPG < thresholdi). The population size, baseline characteristics, and diabetes incidence rate in the two groups were all dependent on the FPG threshold selected (i.e., the value of i.)
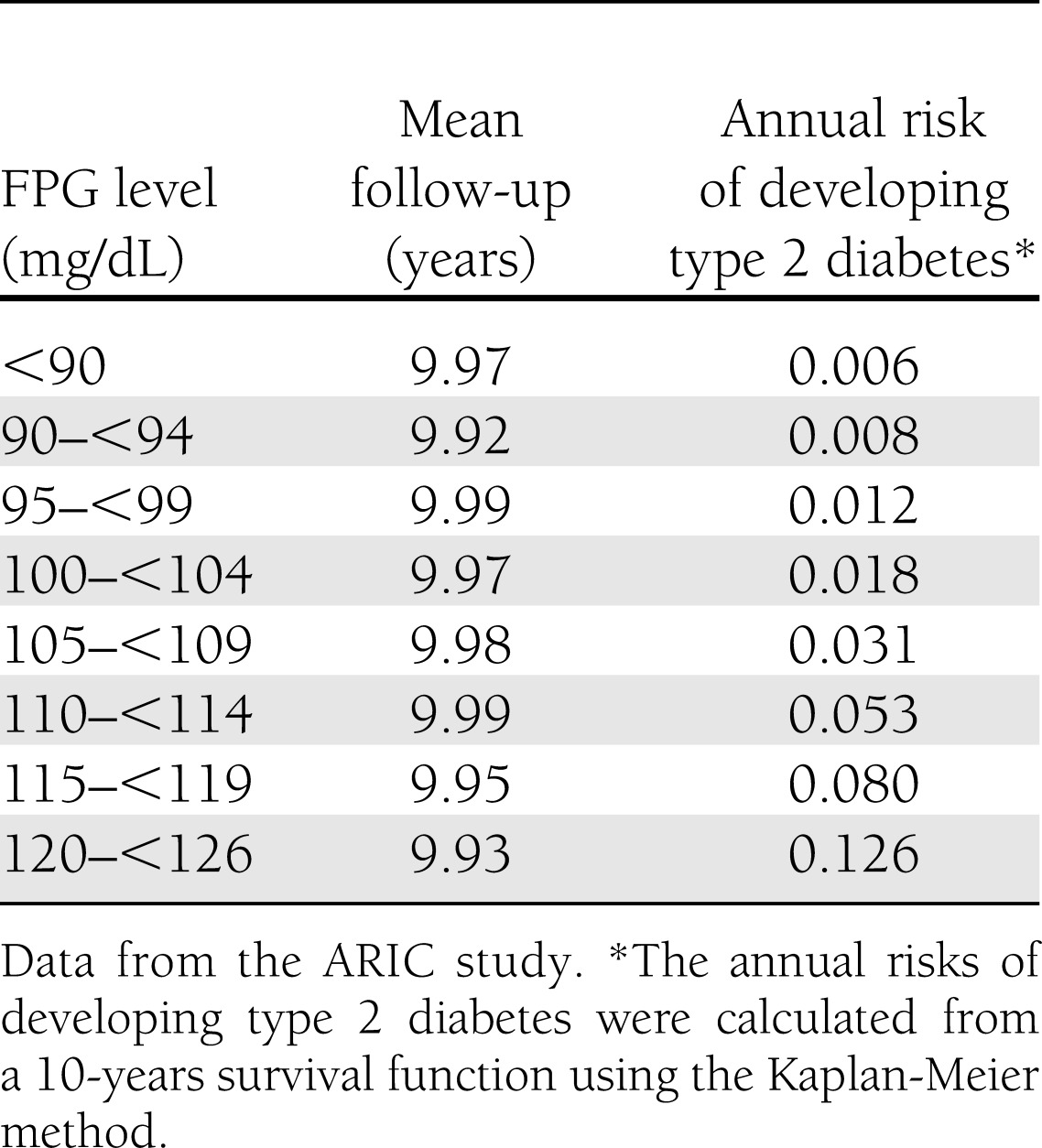
Rates of diabetes incidence in both the high-risk group and the normal FPG group were estimated using data from the Atherosclerosis Risk in Communities (ARIC) study, a prospective study including 15,792 adults aged 45 years or older at baseline in 1987 to 1989 (17). In the study, diabetes incidence was defined by subsequent plasma measurements (fasting glucose ≥126 mg/dL or nonfasting glucose ≥200 mg/dL), a self-reported diagnosis of diabetes, or use of antidiabetic medications during 6 years of follow-up (18). The estimates of annual risk for developing type 2 diabetes used in the simulation are presented in Table 1. We found that increments in the level of FPG were associated with a continuum of increasing risk for diabetes, which is consistent with previous studies (18–22).
Table 1.
Annual risk of developing type 2 diabetes by FPG level
In the model, disease progression subsequent to a diagnosis of diabetes was simulated based on data primarily obtained from the UK Prospective Diabetes Study (UKPDS) (23). Risk of developing hypertension, hyperlipidemia, coronary heart disease, or stroke, all of which are associated with diabetes, before the clinical diagnosis of diabetes also was incorporated in the model (9,24–26). Technical details are provided in the Supplementary Data.
Diabetes prevention interventions
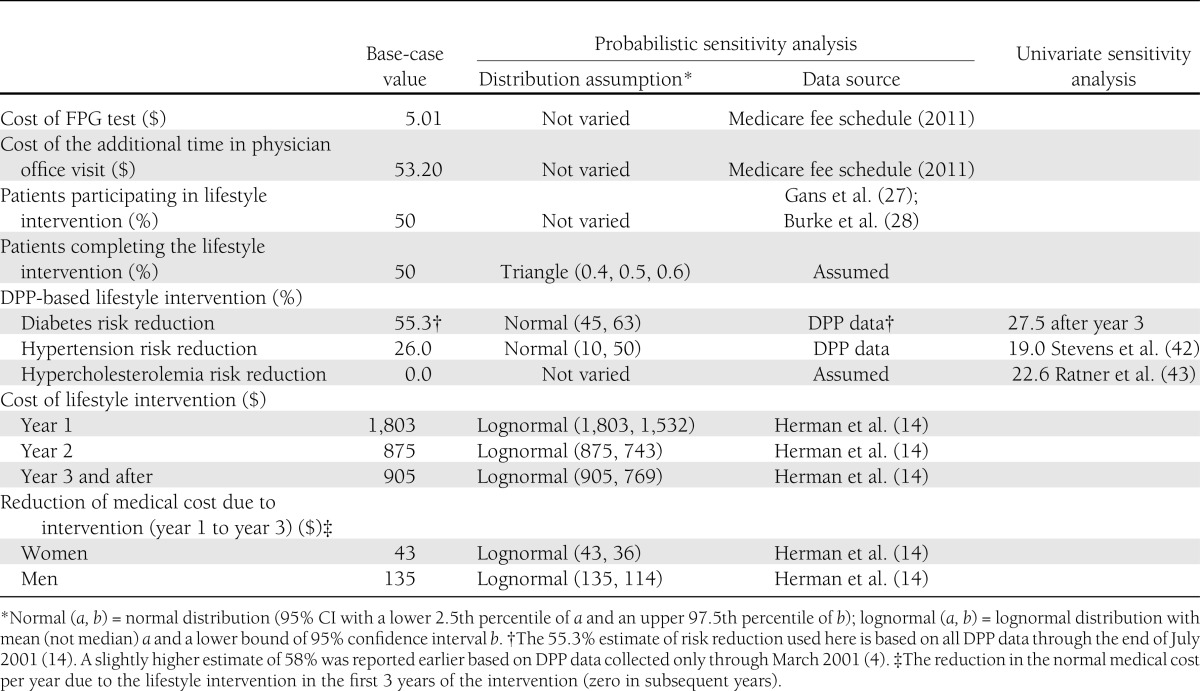
In the simulation, we assumed that 50% of individuals identified as high risk started the lifestyle intervention and 50% of those completed the program (27,28). Attrition was assumed to occur evenly through the years of participation. After 1 year of the lifestyle intervention, participants received a test for diabetes. The intervention and testing continued annually until an individual was diagnosed with diabetes (by the definition of diabetes used in the ARIC study), died, or dropped out. The intervention was modeled based on the intensive lifestyle intervention program implemented in the Diabetes Prevention Program (DPP) study (4). The DPP study was a 3-year randomized trial with a 16-lesson core curriculum covering diet, exercise, and behavior modification that was taught by case managers. Lessons were delivered one-on-one for the first 6 months, followed by individual and group sessions over the subsequent 6 months (4). The costs and effectiveness measures associated with the intervention are summarized in Table 2.
Table 2.
Cost of FPG testing and costs and effectiveness of a hypothetical lifestyle intervention program based on the DPP
Among people who developed diabetes while receiving intervention, we assumed diabetes was diagnosed during the year of onset. After diagnosis, these individuals would continue to receive the lifestyle intervention and additionally receive a metformin therapy (850 mg twice per day) (29). This treatment would last until the person’s A1C level reached 7.0%, at which point the person would receive intensive treatment for glycemic control, as implemented in the UKPDS (15). Patients in the UKPDS were treated intensively, with a goal of maintaining an A1C level below 7.0% using metformin, sulfonylureas, and dietary advice from a dietitian.
The group with an FPG value below a threshold (i.e., the low-risk group) was assumed to receive no lifestyle intervention. People in this group, as well as those who were identified as high-risk individuals but did not participate in the lifestyle intervention, were assumed to develop type 2 diabetes based on the incidence rates observed in the ARIC study. When their diabetes was clinically diagnosed, the mean A1C level was assumed to be 7.1%, the level observed among UKPDS subjects after the dietary run-in period (23). After diagnosis, they were assumed to receive the same intensive treatment for glycemic control as those in the UKPDS.
Cost and health utility
The study was conducted from a health care system perspective, and thus only the following costs were considered: 1) the cost of a one-time fasting glucose screening test for all participants; 2) the annual cost for the lifestyle program and the screening test for high-risk adults who took up the intervention; and 3) treatment costs for diabetes and diabetes-related complications (details appear in Supplementary Table 18). All costs are expressed in 2012 U.S. dollars. Future costs were discounted at 3% annually. Calculations were performed in full precision and costs were rounded to the nearest $100.
The health utility values of individuals with elevated FPG and type 2 diabetes were based on data from the DPP study (30) and a health utility model developed by Coffey et al. (31), who estimated health utility values associated with diabetes treatment mode and diabetes-related complications and adjusting for socioeconomic and demographic variables. Their estimated baseline utility score of 0.69 represents the utility value for a nonobese man with type 2 diabetes who is treated with diet and exercise, has no cardiovascular risk factors, and has no microvascular, neuropathic, or cardiovascular complications. Additional treatments, cardiovascular risk factors, or complications would lead to reductions from the baseline utility score. Detailed specifications on the health utilities appear in the Supplementary Data (Supplementary Table 19). QALYs were discounted at 3% annually.
Incremental cost-effectiveness ratio
The cost-effectiveness associated with a threshold was measured by the incremental cost-effectiveness ratio (ICER), which was calculated by dividing the incremental cost by the incremental effectiveness between that threshold (e.g.,115 mg/dL) and its next higher threshold (e.g.,120 mg/dL) (32). This differs from conventional cost-effectiveness analyses, in which ICERs are calculated by comparing cost and effectiveness of new interventions with those of existing interventions or with doing nothing. The objectives of conventional analyses are to compare cost-effectiveness of different intervention options in a fixed intervention population. Conversely, the objective here was to assess how the cost-effectiveness of a fixed intervention would change when the intervention population (people with IFG) is progressively expanded by lowering the FPG value used to define IFG.
Sensitivity analyses
We conducted both univariate and probabilistic sensitivity analyses. First we tested whether using a different preventive intervention might change the ICERs of the FPG thresholds. We considered a program implemented in the Promoting a Lifestyle of Activity and Nutrition for Working to Alter the Risk of Diabetes (PLAN4WARD) study. PLAN4WARD is a community-based program designed to deliver at a lower cost the key elements of the lifestyle intervention used in the DPP study (33). Compared with the DPP intervention, PLAN4WARD costs about 75% less and was 60% as effective in reducing risk of diabetes (34). Details of the cost and effectiveness of the intervention appear in the Supplementary Data.
Second, data from the DPP study suggest a greater reduction in diabetes incidence in adults aged ≥60 years than in those aged <60 years (71% vs. 59%) (4). To test the difference of the ICERs among different age groups, we ran the simulation for individuals aged 45–59 years and those aged ≥60 years, using DPP estimates of effectiveness for the two groups. In addition, we ran a separate analysis for persons aged 18 to 44, assuming that, given the same FPG value, they had the same level of risk of developing diabetes as persons aged 45 or older.
We performed four additional univariate sensitivity analyses to address uncertainty associated with the magnitude of the intervention effects. For the first, we replaced our base-case estimate for diabetes risk reduction (55.3%) with the estimate of 38.0% from the 10-year DPP follow-up (35). The lower risk reduction figure may be considered conservative because the intensive lifestyle intervention was discontinued at the end of the 3-year trial period and all participants, including those in the control group, received a group-based lifestyle intervention afterward. For the second analysis, to account for participants’ possibly diminished adherence to the practices of the lifestyle change intervention over time, we assumed that the effectiveness of the intervention declined by 50% after the third year of the intervention. For the third analysis, we varied the effectiveness of the intervention on reducing the risk of hypertension. For the fourth analysis, we varied the effectiveness of the intervention on reducing the risk of hypercholesterolemia (Table 2).
In addition, we conducted a probabilistic sensitivity analysis in which a set of 85 model parameters were simultaneously varied based on the associated probability in 500 iterations of the simulation. The probabilities of each FPG threshold being cost-effective, given a range of the monetary value of QALYs gained, were plotted to form cost-effectiveness acceptability curves (36). Details appear in the Supplementary Data. In addition, we tested the statistical difference of the ICER associated with one threshold versus the next level using the random sample (N = 500 × 7 = 3,500) generated from the probabilistic sensitivity analysis.
RESULTS
Base-case analysis
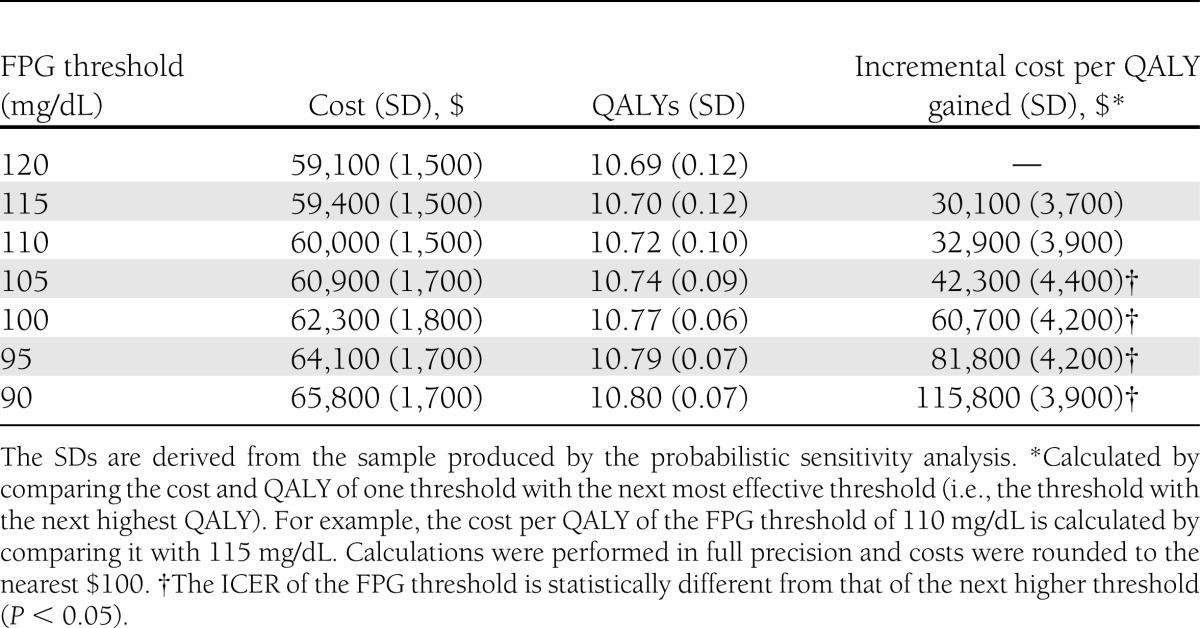
Table 3 shows the average lifetime cost and QALY estimates when using different FPG thresholds to define IFG. When 120 mg/dL was used as the initial threshold for intervention, the lifetime cost was $59,100 and achieved 10.69 QALYs. Progressively lowering the FPG threshold led to a monotonic increase in both QALYs and costs. Lowering the threshold from 120 to 90 mg/dL increased QALYs from 10.69 to 10.80 and increased lifetime costs from $59,100 to $65,800. Decreasing the FPG threshold—and thereby increasing the number of people eligible for the intervention and the health benefit—also increased the cost per QALY gained. Because of the monotonic relationship between the FPG threshold and QALYs, the next higher threshold always yielded a larger QALY than the current one. Lowering the threshold from 120 to 115 mg/dL cost $30,100 per additional QALY gained. The cost per QALY gained of moving the threshold from 115 to 110 mg/dL was $32,900; from 110 to 105 mg/dL was $42,300; from 105 to 100 mg/dL was $60,700; from 100 to 95 mg/dL was $81,800; and from 95 to 90 mg/dL was $115,800.
Table 3.
Lifetime cost and QALY per person and incremental cost per QALY gain under seven FPG threshold scenarios
Univariate sensitivity analyses
Table 4 shows that, regardless of model parameters or assumptions, the ICER consistently increased as the FPG threshold was lowered. However, referring individuals to a less costly and less effective intervention, such as PLAN4WARD, in the first sensitivity analysis (SA1 in Table 4) considerably reduced ICERs at all threshold levels; these reductions were greater at lower thresholds. The cost per QALY gained associated with 115 mg/dL was $21,500, compared with $30,100 in the base-case. The cost per QALY gained was $22,600 when lowering the threshold from 115 to 110 mg/dL; $27,900 from 110 to 105 mg/dL; $40,800 from 105 to 100 mg/dL; was $71,500 from 100 to 95 mg/dL; and $96,000 from 95 to 90 mg/dL.
Table 4.
Incremental cost per QALY ($) of FPG threshold in the univariate sensitivity analyses
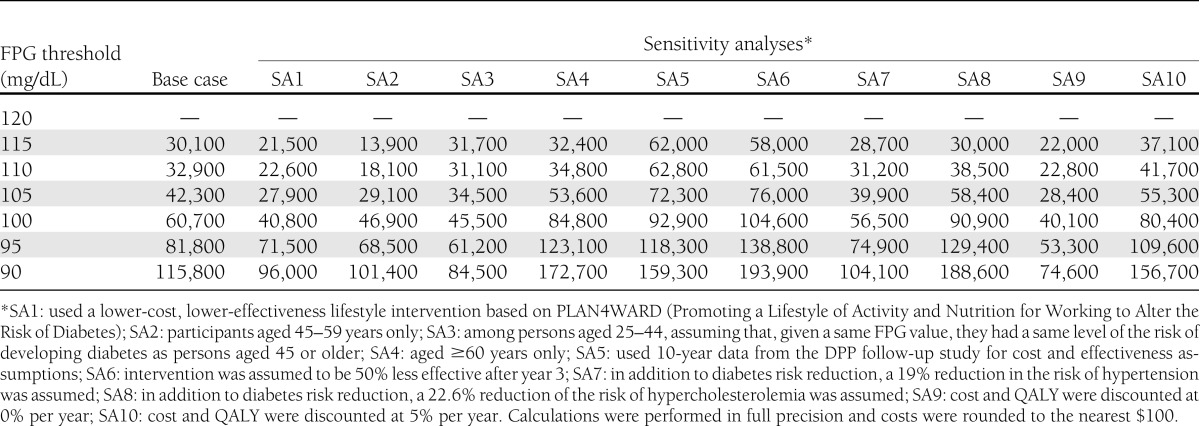
When the analysis was restricted to persons aged 45–59 years (SA2), the ICERs were lower at all FPG thresholds, ranging from $13,900 to $101,400 per QALY gained. For persons aged 25–44 (SA3), the ICERs for most of the thresholds evaluated were also lower than those in persons aged 45 or older. In comparison, the ICER for individuals aged ≥60 years were higher, ranging from $32,400 to $172,700 per QALY gained (SA4). Using data from the 10-year DPP risk reduction estimate (SA5) resulted in higher ICERs, as did assuming a long-term diminishing effect of the intervention (SA6). However, assuming that lifestyle intervention also reduced the risk of developing hypertension (SA7) or hypercholesterolemia (SA8) resulted in lower ICERs.
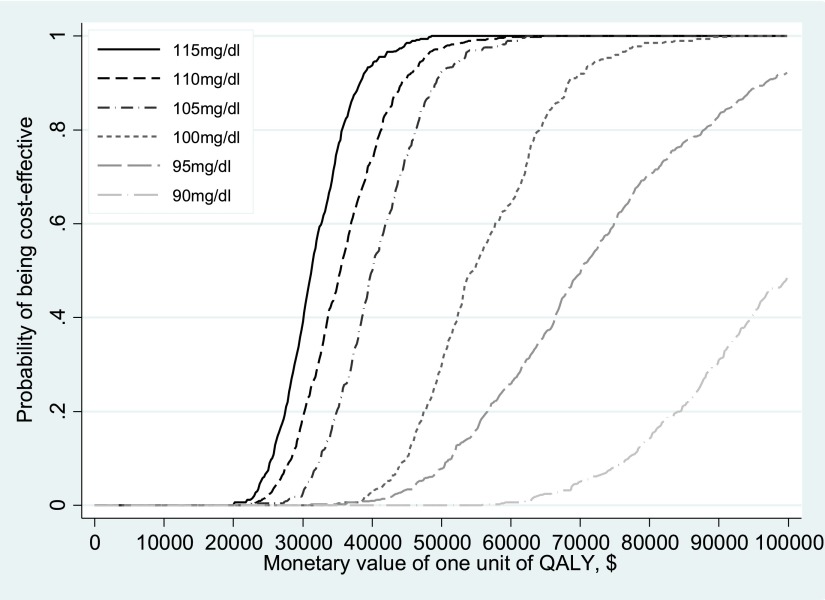
Probabilistic sensitivity analysis
Figure 1 shows the cost effectiveness acceptability curves of seven FPG thresholds. Each curve represents the probability that the given threshold is cost-effective by the monetary value of a QALY, or willingness to pay. One FPG threshold would be more likely to be cost-effective if the willingness to pay for QALY gain is higher. For instance, in a scenario in which the monetary value of $50,000 per QALY (a conventional benchmark figure for a society’s willingness to pay [37]) is assigned, the probability of the 105-mg/dL IFG threshold will be cost-effective was 0.92. The probability would increase to 0.99 if the value of a QALY was increased to $60,000. However, the probability that an IFG threshold of 100 mg/dL is cost effective is 0.29 and 0.65 at the willingness-to-pay benchmarks of the $50,000 and $60,000 per QALY, respectively. Each FPG threshold was statistically significantly different from its next higher threshold, except the level of 110 mg/dL. Details about the results of the probabilistic sensitivity analysis appear in section VII of the Supplementary Data.
Figure 1.
Cost-effectiveness acceptability curves associated with alternative FPG thresholds. Note that the FPG threshold of 120 mg/dL served as the reference threshold for 115 mg/dL. For each of the other FPG thresholds, the next higher threshold served as the reference threshold. For instance, the comparison threshold for FPG 110 mg/dL was 115 mg/dL. See Table 3 for more details.
CONCLUSIONS
FPG tests have been increasingly used to identify individuals at high risk of developing type 2 diabetes and refer them for diabetes prevention interventions (38). The selection of the threshold of the FPG test determines the target population for preventive intervention and thus ultimately affects the efficiency of the interventions. The economic implications need to be well understood so scarce health care resources can be used in an efficient manner. In this study we examined the cost-effectiveness of seven possible FPG test thresholds when they were used for referral to a diabetes prevention intervention. We found that as the FPG threshold was lowered the population-level health benefit increased but cost-effectiveness was reduced.
Our study results suggest that the selection of the FPG threshold may ultimately depend on the health care resources that are available for diabetes prevention or the willingness to pay to prevent diabetes. A lower IFG threshold might be preferred if more resources are available or the willingness to pay for preventing diabetes is higher. Using $50,000 per QALY as a benchmark for acceptability (37), we are quite certain (with more that 90% certainty) that diabetes prevention would be cost-effective if we used an FPG level of 105 mg/dL as the threshold to identify a high-risk state. However, if a higher willingness to pay per QALY were acceptable, a threshold that is lower than 105 mg/dL is preferred.
Furthermore, our findings suggest that a lower threshold might be preferred if the cost of the diabetes prevention intervention could be reduced. In our sensitivity analysis, under a scenario in which a less costly but less effective intervention was used, cost-effectiveness was improved at all threshold levels. For instance, the ICER associated with the threshold of 100 mg/dL decreased from $60,700 per QALY in the base-case to $40,800 per QALY when the less costly and less effective intervention was used. This indicates that by using the less expensive intervention the FPG threshold could be lowered from 105 to 100 mg/dL, even when the willingness to pay benchmark remained at the same level of $50,000 per QALY. Because the cost of the intervention affects the cost-effectiveness of the FPG threshold, it ultimately affects the selection of an economically preferred threshold of the FPG test for diabetes prevention.
Our study demonstrates a deteriorating cost-effectiveness associated with the decreasing FPG threshold and provides a valuable health economics perspective into the debate over the selection of the optimal FPG threshold. However, our study did not aim to determine the definitive value of a universally optimal threshold because selecting such a threshold may depend on many factors. In particular, the cost-effectiveness of a specified FPG threshold is likely to change by age: the risk of type 2 diabetes indicated by the value may vary depending on age (39,40). To understand how such differences in the population might affect the choice of a threshold, we estimated the ICERs at each FPG threshold by age group. We found lower cost-effectiveness ratios associated with all FPG thresholds in those aged 45–64 years and younger than 45 than in those aged ≥65 years. This is primarily because of the longer life expectancy of the younger populations. Preventing more cases of type 2 diabetes and possibly other risk factors over that time creates a higher likelihood of recouping the cost of the intervention via reduced treatment and complication costs, even though the intervention is more effective in the older group.
Limitations
Our study has several limitations. First, our analysis is based on a single measure of FPG. Since FPG can vary from day to day, multiple measures might give a better definition of IFG. Second, FPG is one of several markers that can be used to identify people at high risk for developing type 2 diabetes. Recent ADA guidelines also recommended A1C as a test to identify people at high risk (6). Other variables such as sex, race/ethnicity, family history, and body weight may affect an individual’s future risk of type 2 diabetes (39–41). Future studies should examine the cost-effectiveness of alternative thresholds of FPG testing, stratified by other risk factors, when data on diabetes incidences are available for those stratified subpopulations. Third, our simulation model was developed based on data collected from multiple sources and thus was inevitably subject to the accuracy of the data sources and the assumptions used by the researchers in the source studies.
Conclusion
When FPG testing is used to identify a target population for type 2 diabetes prevention, selecting a lower FPG threshold leads to a greater gain in overall health benefit but also to a deteriorated cost-effectiveness. The selection of an appropriate FPG threshold for any given population ultimately depends on the resources available or the willingness to pay for diabetes prevention. Using the conventional benchmark of $50,000 per QALY, a threshold of 105 mg/dL or higher is highly likely to be cost effective. Furthermore, a lower FPG threshold is preferred if the cost of the intervention can be lowered without compromising too much effectiveness.
Acknowledgments
This research uses data from the Atherosclerosis Risk in Communities (ARIC) study and the National Health and Nutrition Examination Survey (NHANES). The ARIC study is carried out as a collaboration supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022.
No potential conflicts of interest relevant to this article were reported.
X.Z., P.Z., H.S.K., and E.W.G. conceptualized and designed the study, interpreted the data, and edited the manuscript. X.Z. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The preliminary results of the analysis were presented at the 71st Scientific Sessions of the American Diabetes Association, San Diego, California, 24–28 June 2011.
The authors thank Tony Pearson-Clarke of the Division of Diabetes Translation (DDT) at the Centers for Disease Control and Prevention (CDC) for his excellent editorial assistance with this article. The authors also thank Lawrence Barker of the DDT at the CDC for his thoughtful comments and the staff and participants of the ARIC study and NHANES for their important contributions.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-0497/-/DC1.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Heianza Y, Hara S, Arase Y, et al. HbA1c 5·7-6·4% and impaired fasting plasma glucose for diagnosis of prediabetes and risk of progression to diabetes in Japan (TOPICS 3): a longitudinal cohort study. Lancet 2011;378:147–155 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2013;36(Suppl 1):S67–S74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation [report online], 2006. Geneva, Switzerland, World Health Organization. Available from http://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf Accessed 8 August 2013 [Google Scholar]
- 4.Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Diabetes Prevention Program [Internet], 2012. Atlanta, Georgia, Centers for Disease Control and Prevention. Available from http://www.cdc.gov/diabetes/prevention/index.htm Accessed June 2012
- 6.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl 1):S62–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forouhi NG, Balkau B, Borch-Johnsen K, et al. EDEG The threshold for diagnosing impaired fasting glucose: a position statement by the European Diabetes Epidemiology Group. Diabetologia 2006;49:822–827 [DOI] [PubMed] [Google Scholar]
- 8.Lawes CM, Parag V, Bennett DA, et al. Asia Pacific Cohort Studies Collaboration Blood glucose and risk of cardiovascular disease in the Asia Pacific region. Diabetes Care 2004;27:2836–2842 [DOI] [PubMed] [Google Scholar]
- 9.Levitan EB, Song Y, Ford ES, Liu S. Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med 2004;164:2147–2155 [DOI] [PubMed] [Google Scholar]
- 10.Sorkin JD, Muller DC, Fleg JL, Andres R. The relation of fasting and 2-h postchallenge plasma glucose concentrations to mortality: data from the Baltimore Longitudinal Study of Aging with a critical review of the literature. Diabetes Care 2005;28:2626–2632 [DOI] [PubMed] [Google Scholar]
- 11.Hoerger TJ, Segel JE, Zhang P, Sorensen SW. Validation of the CDC-RTI diabetes cost-effectiveness model [report online], 2009.. Research Triangle Park, North Carolina, RTI International. Available from https://www.rti.org/pubs/mr-0013-0909-hoerger.pdf Accessed 8 August 2013 [Google Scholar]
- 12.Hoerger TJ, Harris R, Hicks KA, Donahue K, Sorensen S, Engelgau M. Screening for type 2 diabetes mellitus: a cost-effectiveness analysis. Ann Intern Med 2004;140:689–699 [DOI] [PubMed] [Google Scholar]
- 13.Hoerger TJ, Hicks KA, Sorensen SW, et al. Cost-effectiveness of screening for pre-diabetes among overweight and obese U.S. adults. Diabetes Care 2007;30:2874–2879 [DOI] [PubMed] [Google Scholar]
- 14.Herman WH, Hoerger TJ, Brandle M, et al. Diabetes Prevention Program Research Group The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med 2005;142:323–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC Diabetes Cost-effectiveness Group Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA 2002;287:2542–2551 [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. N.C.f.H.S., Division of Health Interview Statistics. Distribution of age at diagnosis of diabetes among adult incident cases aged 18–79 years, United States, 2011. Available from http://www.cdc.gov/diabetes/statistics/age/fig1.htm Accessed 23 September 2013 [Google Scholar]
- 17.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Vegt F, Dekker JM, Jager A, et al. Relation of impaired fasting and postload glucose with incident type 2 diabetes in a Dutch population: The Hoorn Study. JAMA 2001;285:2109–2113 [DOI] [PubMed] [Google Scholar]
- 19.Balkau B, Hillier T, Vierron E, et al. Comment to: Borch-Johnsen K, Colagiuri S, Balkau B et al. (2004) Creating a pandemic of prediabetes: the proposed new diagnostic criteria for impaired fasting glycaemia. Diabetologia 47:1396-1402. Diabetologia 2005;48:801–802 [DOI] [PubMed] [Google Scholar]
- 20.Tirosh A, Shai I, Tekes-Manova D, et al. Israeli Diabetes Research Group Normal fasting plasma glucose levels and type 2 diabetes in young men. N Engl J Med 2005;353:1454–1462 [DOI] [PubMed] [Google Scholar]
- 21.Qiao Q, Lindström J, Valle TT, Tuomilehto J. Progression to clinically diagnosed and treated diabetes from impaired glucose tolerance and impaired fasting glycaemia. Diabet Med 2003;20:1027–1033 [DOI] [PubMed] [Google Scholar]
- 22.Wareham NJ, Byrne CD, Williams R, Day NE, Hales CN. Fasting proinsulin concentrations predict the development of type 2 diabetes. Diabetes Care 1999;22:262–270 [DOI] [PubMed] [Google Scholar]
- 23.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 24.Levitzky YS, Pencina MJ, D’Agostino RB, et al. Impact of impaired fasting glucose on cardiovascular disease: the Framingham Heart Study. J Am Coll Cardiol 2008;51:264–270 [DOI] [PubMed] [Google Scholar]
- 25.Diabetes Prevention Program Research Group Hypertension, insulin, and proinsulin in participants with impaired glucose tolerance. Hypertension 2002;40:679–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee M, Saver JL, Hong KS, Song S, Chang KH, Ovbiagele B. Effect of pre-diabetes on future risk of stroke: meta-analysis. BMJ 2012;344:e3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gans KM, Lapane KL, Lasater TM, Carleton RA. Effects of intervention on compliance to referral and lifestyle recommendations given at cholesterol screening programs. Am J Prev Med 1994;10:275–282 [PubMed] [Google Scholar]
- 28.Burke LE, Dunbar-Jacob JM, Hill MN. Compliance with cardiovascular disease prevention strategies: a review of the research. Ann Behav Med 1997;19:239–263 [DOI] [PubMed] [Google Scholar]
- 29.Eddy DM, Schlessinger L, Kahn R. Clinical outcomes and cost-effectiveness of strategies for managing people at high risk for diabetes. Ann Intern Med 2005;143:251–264 [DOI] [PubMed] [Google Scholar]
- 30.Diabetes Prevention Program Research Group Within-trial cost-effectiveness of lifestyle intervention or metformin for the primary prevention of type 2 diabetes. Diabetes Care 2003;26:2518–2523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coffey JT, Brandle M, Zhou H, et al. Valuing health-related quality of life in diabetes. Diabetes Care 2002;25:2238–2243 [DOI] [PubMed] [Google Scholar]
- 32.Gold M, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York, Oxford University Press, 1996 [Google Scholar]
- 33.Ackermann RT, Marrero DG. Adapting the Diabetes Prevention Program lifestyle intervention for delivery in the community: the YMCA model. Diabetes Educ 2007;33:69–, 74–75, 77–78. [DOI] [PubMed] [Google Scholar]
- 34.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY Pilot Study. Am J Prev Med 2008;35:357–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diabetes Prevention Program Research Group. Knowler WC, Fowler SE, Hamman RF, et al. 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779–787 [DOI] [PubMed] [Google Scholar]
- 37.Grosse SD. Assessing cost-effectiveness in healthcare: history of the $50,000 per QALY threshold. Expert Rev Pharmacoecon Outcomes Res 2008;8:165–178 [DOI] [PubMed] [Google Scholar]
- 38.Cheng C, Kushner H, Falkner BE. The utility of fasting glucose for detection of prediabetes. Metabolism 2006;55:434–438 [DOI] [PubMed] [Google Scholar]
- 39.Kahn HS, Cheng YJ, Thompson TJ, Imperatore G, Gregg EW. Two risk-scoring systems for predicting incident diabetes mellitus in U.S. adults age 45 to 64 years. Ann Intern Med 2009;150:741–751 [DOI] [PubMed] [Google Scholar]
- 40.Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D’Agostino RB., Sr Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch Intern Med 2007;167:1068–1074 [DOI] [PubMed] [Google Scholar]
- 41.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 2002;25:1862–1868 [DOI] [PubMed] [Google Scholar]
- 42.Stevens VJ, Obarzanek E, Cook NRet al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med 2001;134:1–11 [DOI] [PubMed] [Google Scholar]
- 43.Ratner R, Goldberg R, Haffner Set al. Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes Care 2005;28:888–894 [DOI] [PMC free article] [PubMed] [Google Scholar]