Abstract
OBJECTIVE
To determine whether older adults with diabetes are at increased risk of an injurious fall requiring hospitalization.
RESEARCH DESIGN AND METHODS
The longitudinal Health, Aging, and Body Composition Study included 3,075 adults aged 70–79 years at baseline. Hospitalizations that included ICD-9-Clinical Modification codes for a fall and an injury were identified. The effect of diabetes with and without insulin use on the rate of first fall-related injury hospitalization was assessed using proportional hazards models.
RESULTS
At baseline, 719 participants had diabetes, and 117 of them were using insulin. Of the 293 participants who were hospitalized for a fall-related injury, 71 had diabetes, and 16 were using insulin. Diabetes was associated with a higher rate of injurious fall requiring hospitalization (hazard ratio [HR] 1.48 [95% CI 1.12–1.95]) in models adjusted for age, race, sex, BMI, and education. In those participants using insulin, compared with participants without diabetes, the HR was 3.00 (1.78–5.07). Additional adjustment for potential intermediaries, such as fainting in the past year, standing balance score, cystatin C level, and number of prescription medications, accounted for some of the increased risk associated with diabetes (1.41 [1.05–1.88]) and insulin-treated diabetes (2.24 [1.24–4.03]). Among participants with diabetes, a history of falling, poor standing balance score, and A1C level ≥8% were risk factors for an injurious fall requiring hospitalization.
CONCLUSIONS
Older adults with diabetes, in particular those using insulin, are at greater risk of an injurious fall requiring hospitalization than those without diabetes. Among those with diabetes, poor glycemic control may increase the risk of an injurious fall.
Unintentional falls are the leading cause of injury-related hospitalization and death among older adults aged 70–79 years in the United States and resulted in $2.5 billion in medical care expenditures in 2005 (1). The risk of falling is higher in older adults with diabetes, particularly in those using insulin (2,3). Several established risk factors for falls are more common in people with diabetes, including peripheral neuropathy, decreased physical performance, decreased cognitive performance, poor vision, and increased use of antidepressant medication (4–7). Additionally, hypoglycemic episodes may contribute to fall risk. Furthermore, falls are the leading cause of fractures (8), and fractures are more common in those with diabetes (9–13). Taken together, this evidence suggests that people with diabetes, especially those using insulin, may be more likely to sustain a serious injury in a fall. However, previous studies have yielded conflicting findings regarding the association between diabetes and the risk of serious fall-related injuries (14–16). Moreover, there is a knowledge gap regarding the risk factors for injurious falls specific to the population with diabetes, because no such studies exist. Understanding and acting on these risk factors could help to reduce the burden of falls in the population with diabetes. We used longitudinal data from the Health, Aging, and Body Composition (Health ABC) Study to determine whether older adults with diabetes, with or without insulin therapy, are more likely than those without diabetes to have an injurious fall requiring hospitalization. We also assessed risk factors for an injurious fall hospitalization within the subset of participants with diabetes.
RESEARCH DESIGN AND METHODS
The Health ABC Study, a prospective longitudinal study that investigates changes in body composition and functional decline among older adults, has been previously described (17). In summary, participants were recruited from a sample of Medicare-eligible adults living near Pittsburgh, Pennsylvania, or Memphis, Tennessee. Participants were excluded if they reported difficulty getting around without assistive devices, reported difficulty performing basic activities of daily living, reported difficulty walking one-quarter mile or climbing 10 steps without resting, reported life-threatening illnesses, were not planning to stay in the study area for ≥3 years, or were participating in any research involving medications or modification of eating habits. There were 3,075 black and white adults (52% female, 58% white) aged 70–79 years who enrolled in the study from April 1997 to June 1998 and completed a baseline evaluation. Participants were observed for an average of 10 years. Study procedures were approved by the institutional review boards at all participating institutions. Participants provided written informed consent.
Diabetes
Baseline diabetes was ascertained by self-report of a physician’s diagnosis, self-report of antidiabetes medication use, elevated fasting glucose level (≥126 mg/dL), or elevated levels on a 2-h oral glucose tolerance test (≥200 mg/dL) (18).
Injurious fall requiring hospitalization
A hospitalization was defined as an event where the attending physician admitted a Health ABC Study participant to an acute care, inpatient hospital and the participant stayed overnight at the hospital for at least one night. Participants reported hospitalizations biannually, and these hospitalizations were confirmed by medical record review. A hospitalization due to an injurious fall was defined as any hospitalization with an ICD-9-Clinical Modification (ICD-9-CM) external cause of injury code (E-code) for accidental fall (E880–E888), as well as an ICD-9-CM injury code (800–999). Only the first hospitalization of a participant with ICD-9-CM codes for both an injury and a fall were included. For this study, 293 participants were identified with at least one hospitalization with ICD-9-CM codes for both an injury and a fall.
Other covariates
Sociodemographic covariates, assessed by questionnaire at baseline, included age, race, sex, and education. Participants were asked to identify the highest level of school completed. Responses were then categorized as follows: less than high school, high school graduate, or any postsecondary education. The duration of diabetes was determined through self-reported age at the diagnosis of diabetes. Participants were asked to recall their history of falling and fainting in the past year, and to rate their vision with glasses or contact lenses. Medication use was determined by asking participants to list both prescription and nonprescription medications used in the preceding 2 weeks. Weight was measured using a standard balance beam scale. Standing height was measured using a wall-mounted Harpenden stadiometer (Holtain Ltd., Crymych, UK). BMI was calculated as weight (in kilograms) divided by standing height (in meters squared). Measurements of physical performance included the ability to do five chair stands, standing balance score, and usual walking speed (19,20). The ability to do five chair stands was measured by having participants begin in a seated position and stand up five times as quickly as possible while keeping arms folded across the chest. Standing balance score (0–4) was based on the ability to perform semitandem and tandem static balance tests, with a higher score indicating better performance. Usual walking speed was determined by asking a participant to walk for 6 m at a usual pace. Cognitive function was measured using the 100-point Modified Mini-Mental State examination (3MS) (21). Serum cystatin C level, a measure of kidney function, was measured using a BN II nephelometer (Dade Behring, Inc., Deerfield, IL) utilizing a particle-enhanced immunonephelometric assay (N Latex Cystatin C) (22). Hemoglobin A1c was measured in baseline blood specimens with Bio-Rad VARIANT high-performance liquid chromatography assay. Hypoglycemic episodes associated with the hospitalizations due to an injurious fall were determined by the presence of ICD-9-CM codes 250.3, 250.8, and 251.0–251.2 (23).
Statistical analyses
Baseline characteristics were compared across categories of diabetes status (i.e., without diabetes; with diabetes, no insulin; with diabetes, insulin), using ANOVAs for continuous measures and χ2 tests for categorical measures. The rate of first hospitalization with an injurious fall was calculated as the number of events per thousand person-years of follow-up. Additionally, within the subpopulation of Health ABC Study participants with diabetes, baseline characteristics were compared between those with and without a hospitalized fall injury using two-sample t tests for continuous measures and χ2 tests for categorical measures.
Rates of first hospitalization with injurious fall were compared using Cox proportional hazards models with time to first fall injury requiring hospitalization as the dependent variable. Minimally adjusted models included age, sex, race, study site, education, and BMI; these potential confounders were retained in the full models. To identify potential intermediary variables in the relationship between insulin-treated diabetes and injurious fall requiring hospitalization, the following variables were assessed: fainting in the past year, falling in the past year, self-rated eyesight, ability to do five chair stands, usual walking speed, standing balance score, 3MS score, cystatin C level, number of prescription medications, benzodiazepine use, selective serotonin reuptake inhibitor use, and antihypertensive medication use. Models assessing potential intermediaries were limited to participants with baseline data on all of these variables (N = 2,949). Usual walking speed, standing balance score, 3MS score, cystatin C level, and number of prescription medications were included in models as categorical variables. The potential intermediary variables were entered individually into the minimally adjusted model and retained if the effect estimate for insulin-treated diabetes compared with no diabetes was attenuated by ≥10%. None of the variables met this criterion. Potential intermediary variables were then entered in groups of two or three and retained based on the same criterion.
To identify the risk factors for an injurious fall requiring hospitalization within the subpopulation of people with diabetes in this study, all variables that were assessed for inclusion in the model for risk associated with diabetes (see above), plus A1C level, sulfonylurea use, insulin use, and duration of diabetes, were assessed in unadjusted models. Variables that differed between those with and without an injurious fall (P < 0.20) were included in the initial model. Variables were removed using backward selection until only variables that were significant at P < 0.05 remained in the model. Based on previous literature showing an increased risk of falls among people using insulin, insulin use remained in the model, regardless of statistical significance.
All results were considered statistically significant at P < 0.05. Data analyses were performed using SAS (version 9.2; SAS Institute, Cary, NC).
RESULTS
Diabetes and risk of injurious fall
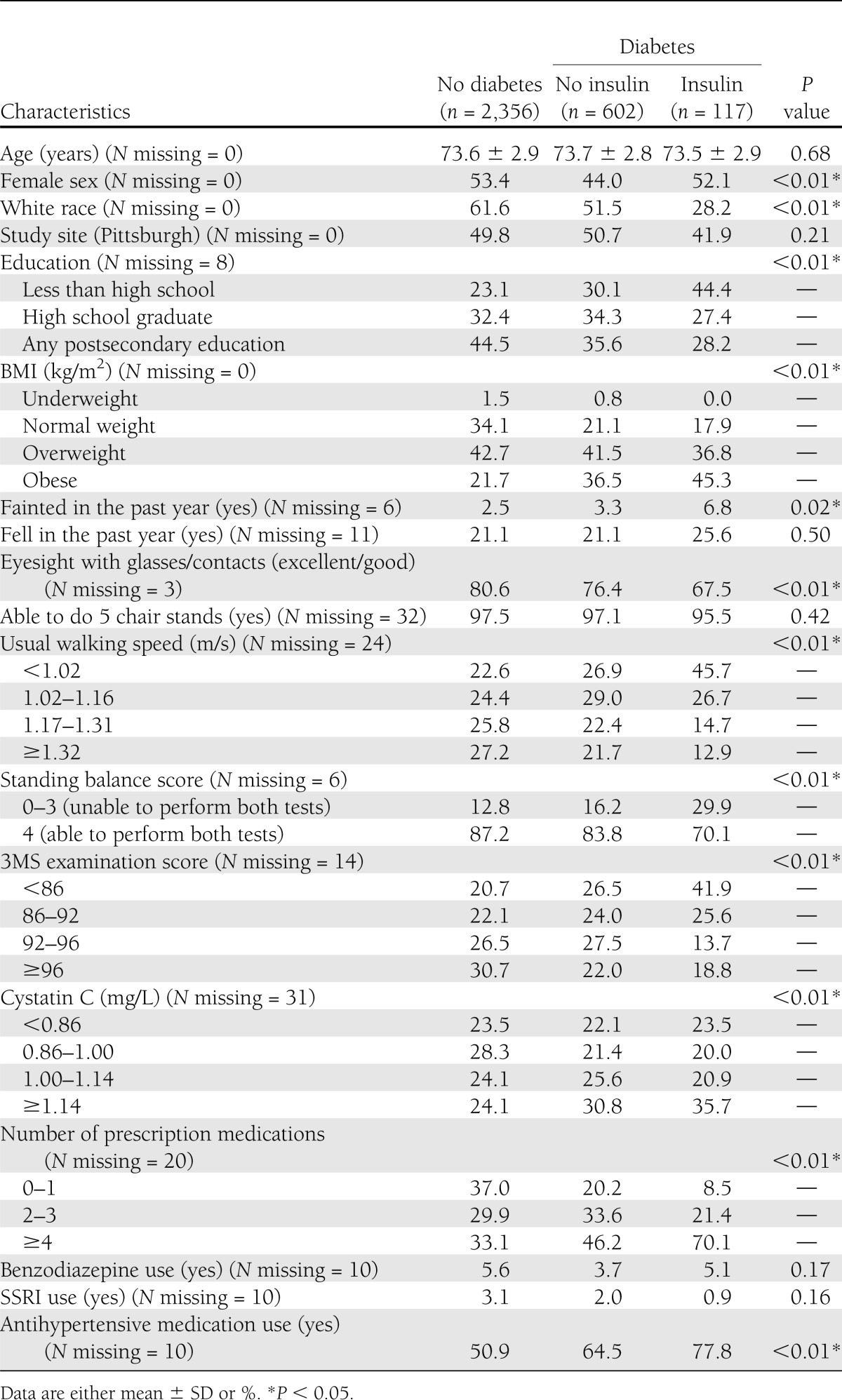
At baseline, 602 participants (19.6%) had diabetes and were not using insulin, and 117 participants (3.8%) had diabetes and were using insulin. Baseline characteristics by diabetes and insulin use status are presented in Table 1. Those with diabetes did not report more falls in the year before baseline, but were more likely to have poor performance on the walking speed and balance tests.
Table 1.
Baseline characteristics by diabetes and insulin status in the Health ABC Study
During the mean follow-up period of 10.1 years (SD 3.5 years), 293 participants experienced at least one injurious fall requiring hospitalization, including 223 participants without diabetes, 55 with diabetes who were not using insulin, and 16 with diabetes who were using insulin. The rate of injurious fall requiring hospitalizations was 9.4 per 1,000 person-years among participants without diabetes. Among participants with diabetes, the rate was 10.0 per 1,000 person-years (P = 0.70 compared with participants without diabetes) in those who were not using insulin and 16.4 per 1,000 person-years (P = 0.03 compared with participants without diabetes) in those using insulin. Of 293 participants who experienced a first hospitalization for an injurious fall, 63.5% (n = 186) had a fracture. The rate of hospitalization for an injurious fall when excluding fractures was 3.6 per 1,000 person-years. Among participants with diabetes who were not using insulin, 2 of 55 hospitalizations for an injurious fall (3.6%) were associated with a hypoglycemic episode. Among participants with diabetes who were using insulin, 1 of 16 hospitalizations for an injurious fall (6.2%) was associated with a hypoglycemic episode.
Relative to participants without diabetes, those with any diabetes had an elevated risk of hospitalization for an injurious fall (hazard ratio [HR] 1.48 [95% CI 1.12–1.95]) (Table 2), even after adjustment for potential intermediaries (history of fainting, standing balance score, cystatin C level for renal function, and number of prescription medications) (1.41 [1.05–1.88]). In models stratified by insulin use, those who had diabetes but were not using insulin had an elevated risk of hospitalization for an injurious fall relative to participants without diabetes, but the difference was not statistically significant (1.30 [0.96–1.76]). Participants who used insulin had a significantly higher risk of hospitalization for an injurious fall than those without diabetes (3.00 [1.78–5.07]) and those with diabetes not using insulin (2.18 [1.22–3.93]). For analyses of potential intermediaries, models were restricted to the 2,949 participants with complete data on the covariates considered. Adjusting for a combination of fainting in the past 12 months, standing balance score, cystatin C level, and number of prescription medications explained 13% of the association comparing participants using insulin to those without diabetes (2.24 [1.24–4.03]), and 40% of the association comparing participants using insulin to those with diabetes not using insulin (1.44 [0.74–2.77]) (Table 2). Adjustment for additional covariates did not further attenuate the estimate of the association between insulin-treated diabetes and hospitalization for an injurious fall.
Table 2.
Association between diabetes and having an injurious fall requiring hospitalization in the Health ABC Study
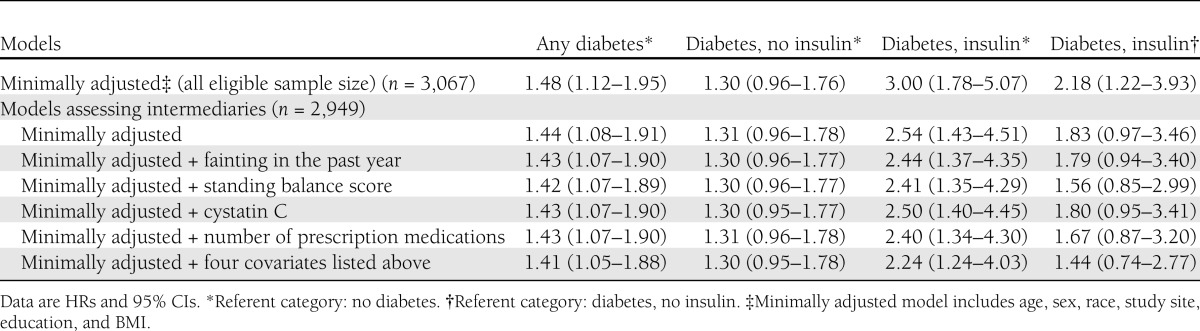
In secondary models excluding hospitalizations with a fracture injury, the effect estimates in minimally adjusted models for diabetes without insulin use (HR 1.35 [95% CI 0.83–2.19]) and diabetes with insulin use (2.80 [1.11–7.07]) remained similar to the results for all hospitalizations due to an injurious fall.
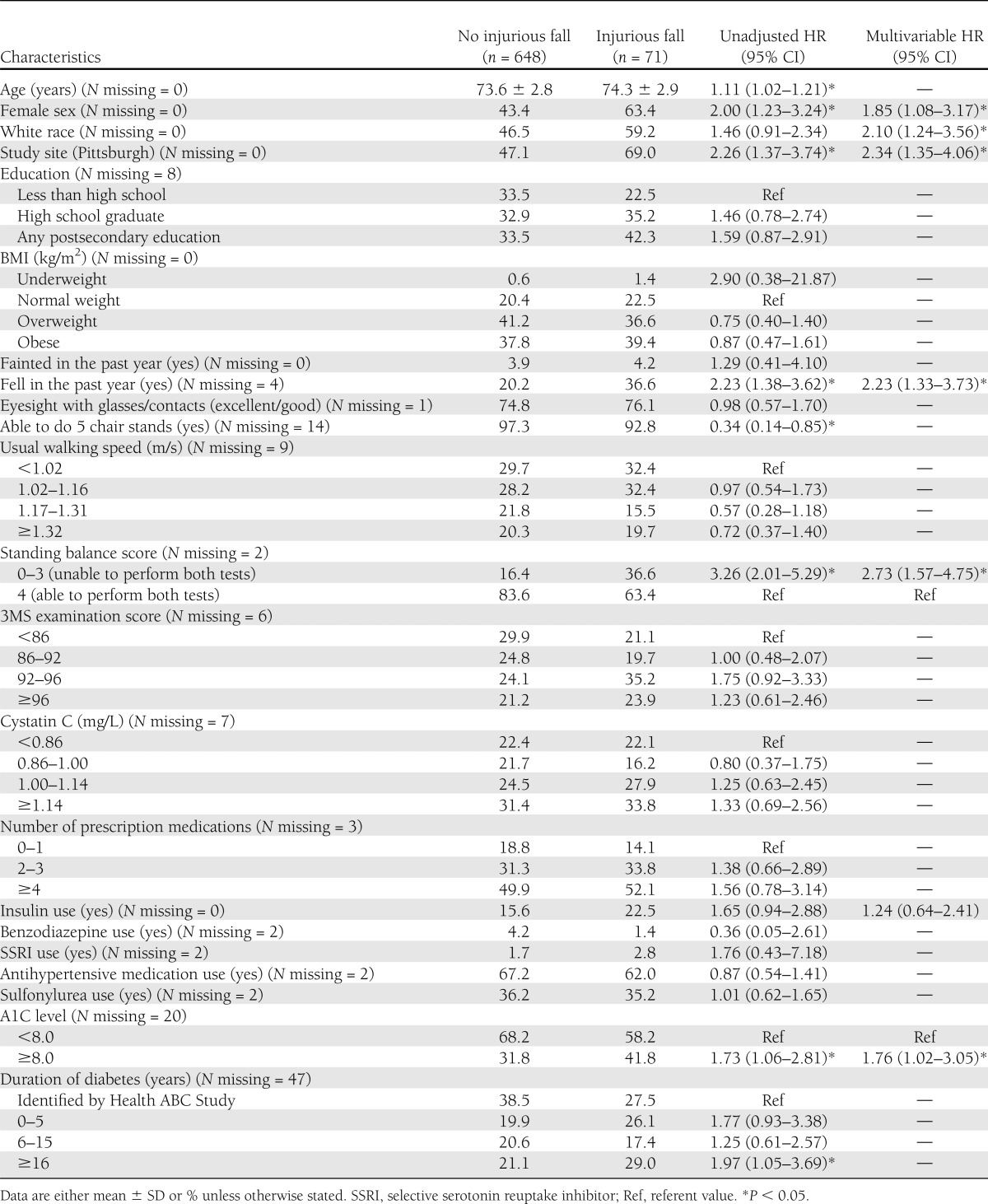
Risk factors for injurious falls among those with diabetes
Among 719 participants with diabetes at baseline, 71 (9.9%) were hospitalized with an injurious fall. In unadjusted models, factors associated with increased risk of hospitalization for an injurious fall included older age and female sex (Table 3). Falling in the past 12 months, but not a history of fainting, was associated with an increased risk of hospitalization for an injurious fall. The ability to do five chair stands and standing balance performance, but not walking speed, were also associated with hospitalization for an injurious fall. Poor glycemic control (A1C ≥8%) was associated with hospitalization for an injurious fall in unadjusted models. Participants with a longer duration of diabetes (≥16 years) had an increased risk of injurious fall hospitalization, compared with participants identified as having diabetes by baseline glucose tests administered during the Health ABC Study. Factors independently associated with hospitalization for an injurious fall in multivariable models included falling in the past 12 months, lower standing balance score, and poor glycemic control. Insulin use was not independently associated with hospitalization for an injurious fall in multivariable models (Table 3).
Table 3.
Risk factors for injurious fall requiring hospitalization among participants with diabetes in the Health ABC Study
CONCLUSIONS
Older adults with diabetes had a higher risk of sustaining a fall-related injury requiring hospitalization than those without diabetes. In particular, those using insulin had three times the risk. In those with diabetes who were not using insulin, our results are consistent with a modest (30%) increase in risk, but we could not rule out a lack of effect. A small portion (13%) of the increased risk in those with insulin-treated diabetes was accounted for by more frequent fainting, poorer balance, reduced renal function, and use of more prescription medications. However, factors that accounted for a greater portion of the increased risk could not be identified in this study.
Within the subpopulation of participants with diabetes, participants using insulin had two times the risk of sustaining a fall-related injury requiring hospitalization than those not using insulin. Falling in the past year, poor standing balance, and A1C levels ≥8.0% were independently associated with this increased risk, but insulin use was not an independent risk factor in the multivariable models.
Diabetes is associated with an increased risk of falling (14–16), particularly in people using insulin (5). However, there is little information available on whether diabetes is associated with serious injury due to a fall. A few previous studies have investigated this association but have produced conflicting results. In a case-control study investigating the effect of chronic medical conditions and the risk of fall injuries, diabetes did not have an effect on fall injuries after adjusting for age and sex (14). However, a longitudinal study of adults aged ≥20 years found that individuals with a history of diabetes had an increased risk for injurious falls (16). And, a study in Scotland using a national trauma registry found that the rate of serious injury due to a low trauma fall was greater in those with insulin-treated diabetes compared with the general population (15).
Previous studies, including a report from this cohort, have shown that fracture risk is elevated in older adults with diabetes, and insulin use appears to further increase this risk (5,11,12,24). Falls are the leading cause of fractures among older adults (8). Consistent with these previous findings, the results of our study reflect in part an increased risk of fall-related fractures with diabetes. However, the increase in serious fall-related injuries associated with insulin-treated diabetes in our study was not limited to fractures. This increased risk of fall-related injuries among patients with diabetes using insulin may reflect the fact that, compared with diabetes patients not using insulin, diabetes patients using insulin have more severe comorbidities, such as peripheral vascular disease (25) and peripheral neuropathy (6), that affect proprioception and function in the legs (26).
The factors that we identified as intermediaries in the association between insulin-treated diabetes and increased risk of injurious falls, including more frequent fainting (27), poorer balance (28), reduced renal function (29), and polypharmacy (30), have been identified as risk factors for falls or fall injuries in previous studies in broader populations of older adults. Hypoglycemic episodes are thought to contribute to fall risk in patients with diabetes using insulin. However, in our data, very few fall injuries were associated with hypoglycemia. Only 1 of 16 hospitalizations for an injurious fall (6.2%) among participants with diabetes who were using insulin was related to a potential hypoglycemic episode. Hospital records were used to identify episodes that may have underestimated the occurrence of hypoglycemia. With increasing use of glucose monitoring, studies show that hypoglycemia is more common than thought, and usually remains unrecognized in patients (31–33). Therefore, hypoglycemia possibly contributes to falls more often than was found in this study.
Among participants with diabetes in this study, poor balance and inadequate glycemic control were associated with an increased risk of injurious falls. To our knowledge, there have been no previous studies examining risk factors for injurious falls in older adults with diabetes. However, other studies have considered risk factors for any fall in people with diabetes (7,29,34,35). In a previous report based on the Health ABC Study population, we found that poor balance, but not high A1C level, was a risk factor for any fall in older adults with diabetes (29). The Women’s Health and Aging Study found that poor lower extremity function, including a test of balance, was a risk factor for recurrent falls in participants with diabetes (7). Results from other studies for the effect of glycemic control on fall risk have been mixed with reports of increased risk (35) with poorer control and reports of no association (36). While previous research has demonstrated that balance training among adults 50–75 years old with diabetes reduces the risk of all falls (37), further research, including intervention studies, would be warranted to determine whether improvements in balance and glycemic control could reduce the number of injurious falls in older adults with diabetes.
Our study had several strengths. The Health ABC Study was a prospective longitudinal study, with an average follow-up time of 10 years. Furthermore, diabetes status was determined through glucose measurements as well as self-report, decreasing the likelihood of misclassification of diabetes status. Additionally, all hospitalization records were validated and reviewed by trained study staff. Despite these strengths, our study also contained limitations. Falls were identified from hospital record E-codes that are potentially underused (38) and misused (39). It seems likely that misclassification of falls would be nondifferential with respect to diabetes status and would therefore tend to bias results toward the null. Furthermore, it is possible that participants with diabetes were more likely to be hospitalized for treatment for any condition, including falls, which would tend to overestimate the association between diabetes and hospitalization due to an injurious fall. Finally, this study did not capture nonhospitalized fall injuries, and therefore these results may not apply to less severe falls.
In summary, we found that older adults with diabetes have an increased rate of fall-related injury requiring hospitalization. In particular, those with insulin-treated diabetes were almost three times more likely than their counterparts without diabetes to experience such a fall-related injury. Improving balance and maintaining adequate glycemic control in older adults with diabetes, especially those with a history of falls, may reduce the risk of a serious fall injury.
Acknowledgments
This research was supported by National Institute on Aging contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106; National Institute on Aging grant R01-AG028050; and National Institute of Nursing Research grant R01-NR012459. This research was also supported by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists and funded by Centers for Disease Control and Prevention Cooperative Agreement number 5U38HM000414. This research was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute on Aging.
No potential conflicts of interest relevant to this article were reported.
R.K.Y. designed the analysis, conducted the analysis and wrote the manuscript. E.S.S., H.E.R., D.E.S., K.R.F., J.A.C., and T.B.H. reviewed and edited the manuscript. E.V. contributed to statistical analysis and reviewed the manuscript. N.D.R., M.C.N., S.R.C., and R.I.S. reviewed the manuscript. A.V.S. contributed to data acquisition, conceptualized the study, designed the analysis, and reviewed and edited the manuscript. R.K.Y. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Lisa Palmero, Department of Epidemiology and Biostatistics, University of California, San Francisco, for help with data management.
References
- 1.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control: data & statistics (WISQARS) [article online], 2013. Available from http://www.cdc.gov/injury/wisqars/index.html Accessed 7 July 2013
- 2.Hanlon JT, Landerman LR, Fillenbaum GG, Studenski S. Falls in African American and white community-dwelling elderly residents. J Gerontol A Biol Sci Med Sci 2002;57:M473–M478 [DOI] [PubMed] [Google Scholar]
- 3.Maurer MS, Burcham J, Cheng H. Diabetes mellitus is associated with an increased risk of falls in elderly residents of a long-term care facility. J Gerontol A Biol Sci Med Sci 2005;60:1157–1162 [DOI] [PubMed] [Google Scholar]
- 4.Park SW, Goodpaster BH, Strotmeyer ES, et al. Decreased muscle strength and quality in older adults with type 2 diabetes: the Health, Aging, and Body Composition Study. Diabetes 2006;55:1813–1818 [DOI] [PubMed] [Google Scholar]
- 5.Schwartz AV, Hillier TA, Sellmeyer DE, et al. Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care 2002;25:1749–1754 [DOI] [PubMed] [Google Scholar]
- 6.Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med 1993;328:1676–1685 [DOI] [PubMed] [Google Scholar]
- 7.Volpato S, Leveille SG, Blaum C, Fried LP, Guralnik JM. Risk factors for falls in older disabled women with diabetes: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci 2005;60:1539–1545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bell AJ, Talbot-Stern JK, Hennessy A. Characteristics and outcomes of older patients presenting to the emergency department after a fall: a retrospective analysis. Med J Aust 2000;173:179–182 [DOI] [PubMed] [Google Scholar]
- 9.Nicodemus KK, Folsom AR, Iowa Women’s Health Study Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care 2001;24:1192–1197 [DOI] [PubMed] [Google Scholar]
- 10.Schwartz AV, Sellmeyer DE, Ensrud KE, et al. Study of Osteoporotic Features Research Group Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab 2001;86:32–38 [DOI] [PubMed] [Google Scholar]
- 11.Strotmeyer ES, Cauley JA, Schwartz AV, et al. Nontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the Health, Aging, and Body Composition Study. Arch Intern Med 2005;165:1612–1617 [DOI] [PubMed] [Google Scholar]
- 12.Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes: a meta-analysis. Osteoporos Int 2007;18:427–444 [DOI] [PubMed] [Google Scholar]
- 13.Wolinsky FD, Bentler SE, Liu L, et al. Recent hospitalization and the risk of hip fracture among older Americans. J Gerontol A Biol Sci Med Sci 2009;64:249–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herndon JG, Helmick CG, Sattin RW, Stevens JA, DeVito C, Wingo PA. Chronic medical conditions and risk of fall injury events at home in older adults. J Am Geriatr Soc 1997;45:739–743 [DOI] [PubMed] [Google Scholar]
- 15.Kennedy RL, Henry J, Chapman AJ, Nayar R, Grant P, Morris AD. Accidents in patients with insulin-treated diabetes: increased risk of low-impact falls but not motor vehicle crashes: a prospective register-based study. J Trauma 2002;52:660–666 [DOI] [PubMed] [Google Scholar]
- 16.Malmivaara A, Heliövaara M, Knekt P, Reunanen A, Aromaa A. Risk factors for injurious falls leading to hospitalization or death in a cohort of 19,500 adults. Am J Epidemiol 1993;138:384–394 [DOI] [PubMed] [Google Scholar]
- 17.Strotmeyer ES, Cauley JA, Schwartz AV, et al. Health ABC Study Diabetes is associated independently of body composition with BMD and bone volume in older white and black men and women: the Health, Aging, and Body Composition Study. J Bone Miner Res 2004;19:1084–1091 [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization, International Diabetes Federation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. Geneva, Switzerland, World Health Organization, 2006 [Google Scholar]
- 19.Cesari M, Kritchevsky SB, Newman AB, et al. Health, Aging and Body Composition Study Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging And Body Composition Study. J Am Geriatr Soc 2009;57:251–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simonsick EM, Newman AB, Nevitt MC, et al. Health ABC Study Group Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci 2001;56:M644–M649 [DOI] [PubMed] [Google Scholar]
- 21.Yaffe K, Fiocco AJ, Lindquist K, et al. Health ABC Study Predictors of maintaining cognitive function in older adults: the Health ABC study. Neurology 2009;72:2029–2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shlipak MG, Wassel Fyr CL, Chertow GM, et al. Cystatin C and mortality risk in the elderly: the Health, Aging, and Body Composition Study. J Am Soc Nephrol 2006;17:254–261 [DOI] [PubMed] [Google Scholar]
- 23.Ginde AA, Blanc PG, Lieberman RM, Camargo CA., Jr Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord 2008;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 2007;166:495–505 [DOI] [PubMed] [Google Scholar]
- 25.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation 2004;110:738–743 [DOI] [PubMed] [Google Scholar]
- 26.Mold JW, Vesely SK, Keyl BA, Schenk JB, Roberts M. The prevalence, predictors, and consequences of peripheral sensory neuropathy in older patients. J Am Board Fam Pract 2004;17:309–318 [DOI] [PubMed] [Google Scholar]
- 27.Shaw FE, Kenny RA. The overlap between syncope and falls in the elderly. Postgrad Med J 1997;73:635–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35(Suppl. 2):ii37–ii41 [DOI] [PubMed] [Google Scholar]
- 29.Schwartz AV, Vittinghoff E, Sellmeyer DE, et al. Health, Aging, and Body Composition Study Diabetes-related complications, glycemic control, and falls in older adults. Diabetes Care 2008;31:391–396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robbins AS, Rubenstein LZ, Josephson KR, Schulman BL, Osterweil D, Fine G. Predictors of falls among elderly people. Results of two population-based studies. Arch Intern Med 1989;149:1628–1633 [PubMed] [Google Scholar]
- 31.Hay LC, Wilmshurst EG, Fulcher G. Unrecognized hypo- and hyperglycemia in well-controlled patients with type 2 diabetes mellitus: the results of continuous glucose monitoring. Diabetes Technol Ther 2003;5:19–26 [DOI] [PubMed] [Google Scholar]
- 32.Munshi MN, Segal AR, Suhl E, et al. Frequent hypoglycemia among elderly patients with poor glycemic control. Arch Intern Med 2011;171:362–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weber KK, Lohmann T, Busch K, Donati-Hirsch I, Riel R. High frequency of unrecognized hypoglycaemias in patients with type 2 diabetes is discovered by continuous glucose monitoring. Exp Clin Endocrinol Diabetes 2007;115:491–494 [DOI] [PubMed] [Google Scholar]
- 34.Quandt SA, Stafford JM, Bell RA, Smith SL, Snively BM, Arcury TA. Predictors of falls in a multiethnic population of older rural adults with diabetes. J Gerontol A Biol Sci Med Sci 2006;61:394–398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tilling LM, Darawil K, Britton M. Falls as a complication of diabetes mellitus in older people. J Diabetes Complications 2006;20:158–162 [DOI] [PubMed] [Google Scholar]
- 36.Miller DK, Lui LY, Perry HM, 3rd, Kaiser FE, Morley JE. Reported and measured physical functioning in older inner-city diabetic African Americans. J Gerontol A Biol Sci Med Sci 1999;54:M230–M236 [DOI] [PubMed] [Google Scholar]
- 37.Morrison S, Colberg SR, Mariano M, Parson HK, Vinik AI. Balance training reduces falls risk in older individuals with type 2 diabetes. Diabetes Care 2010;33:748–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Langlois JA, Buechner JS, O’Connor EA, Nacar EQ, Smith GS. Improving the E coding of hospitalizations for injury: do hospital records contain adequate documentation? Am J Public Health 1995;85:1261–1265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lawrence BA, Miller TR, Weiss HB, Spicer RS. Issues in using state hospital discharge data in injury control research and surveillance. Accid Anal Prev 2007;39:319–325 [DOI] [PubMed] [Google Scholar]


