Abstract
OBJECTIVE
To examine 12-month effects of a booster-enhanced preconception counseling (PC) program (READY-Girls) on family planning for teen girls with type 1 and type 2 diabetes.
RESEARCH DESIGN AND METHODS
Participants 13–19 years of age (n = 109) were randomized to a standard care control group (CG) or intervention group (IG) that received PC over three consecutive clinic visits. Prepost data were collected at baseline, 3- and 6-month booster sessions, and a 12-month follow-up visit.
RESULTS
Mean age was 15.8 years; 9 (8%) subjects had type 2 diabetes; and 18 (17%) subjects were African American. At baseline, 20% (n = 22 of 109) had been sexually active, and of these, 50% (n = 11) had at least one episode of unprotected sex. Over time, IG participants retained greater PC knowledge (F[6, 541] = 4.05, P = 0.0005) and stronger intentions regarding PC (significant group-by-time effects) especially after boosters. IG participants had greater intentions to discuss PC (F[6, 82.4] = 2.56, P = 0.0254) and BC (F[6, 534] = 3.40, P = 0.0027) with health care providers (HCPs) and seek PC when planning a pregnancy (F[6, 534] = 2.58, P = 0.0180). Although not significant, IG participants, compared with CG, showed a consistent trend toward lower rates of overall sexual activity over time: less sexual debut (35 vs. 41%) and higher rates of abstinence (44 vs. 32%). No pregnancies were reported in either group throughout the study.
CONCLUSIONS
READY-Girls appeared to have long-term sustaining effects on PC knowledge, beliefs, and intentions to initiate discussion with HCPs that could improve reproductive health behaviors and outcomes. Strong boosters and providing PC at each clinic visit could play important roles in sustaining long-term effects.
Women with diabetes who receive preconception counseling (PC) have significantly lower rates of maternal and neonatal complications; yet, up to two-thirds of women with diabetes have unplanned pregnancies (1). Teens in particular are at high risk for an unplanned pregnancy. Sexual activity usually begins in adolescence (22% of teens have had sex by 15 years of age; 76% by 19 years of age) (2), and for teens with diabetes, it is often associated with unsafe sexual practices (3). Most teens with diabetes are unaware of diabetes-related reproductive complications related to unplanned pregnancies and have no knowledge of PC (3). Therefore, the American Diabetes Association (ADA) recommends that PC should be included in the routine clinical care of all women with diabetes of child-bearing potential beginning at puberty (4). READY-Girls (Reproductive-health Education and Awareness of Diabetes in Youth for Girls) is a self-administered PC program specifically tailored for adolescent girls with diabetes (5). Our previous READY-Girls (CD-ROM and book) intervention studies were for teens with type 1 diabetes and demonstrated cost-effectiveness and short-term (3 months) efficacy on reproductive health knowledge, intentions, beliefs, social support, and discussion with health care providers (HCPs) (3), with only some changes being sustained over 6 months (3,6). Boosters have been found to sustain the effectiveness of adolescent health behavior interventions (7). READY-Girls was modified as a booster-enhanced intervention with DVDs and a book for teens with both type 1 and type 2 diabetes validated by expert opinion using mental modeling (8). During the modification phase, this research used a formal model developed by a panel of experts, and confirmed by the literature, to identify the most critical relevant concepts. A panel of the target population (adolescents with both type 1 and type 2 diabetes) was interviewed. This approach systematically assesses understanding of a topic in relation to these identified concepts, to inform the need for PC among adolescents, the beliefs that they hold, and how their beliefs may either help them manage their sexuality or potentially undermine their ability to make good decisions about sex. Common misconceptions or gaps in understanding gleaned from these interviews help guide educational efforts for the patients.
This validated, developmentally appropriate, evidence-based educational intervention presents the effects of diabetes on reproductive health, puberty, sexuality, and pregnancy and the benefits of PC and includes skill-building exercises for healthy decision making and communications with HCPs (1,4,6). Given that the use of different instructional mediums enhances learning (9), the program is divided into three sessions with two different stand-alone formats for self-instruction: DVD-1 (health information), exercise booster DVD-2 (decision-making and skills-building exercises), and an information booster as a book to reinforce the content from DVD-1. In a previous three-group randomized, controlled trial that compared the READY-Girls’ computer-based program to the book format and a control group (CG) on psychosocial/cognitive outcomes, we found that subjects in both the CD and book groups were satisfied with their method and had significantly enhanced their knowledge and attitudes compared with the CG (3). Both methods appeared to be reliable formats (3). This current randomized, controlled trial reports on the long-term effects (12 months) of the booster-enhanced READY-Girls program that used both a computer-based program and a book format for adolescent females with type 1 and type 2 diabetes on intentions and behaviors regarding family planning and PC/preconception care.
RESEARCH DESIGN AND METHODS
Adolescent girls between 13 and <20 years of age with either type 1 or type 2 diabetes for >1 year were recruited from diabetes clinics at two university hospitals and randomized using a minimization algorithm considering diabetes type (type 1 or type 2 diabetes), sexual activity status (no or yes), and age (<17 or ≥17 years) to either a standard care CG that received general PC March of Dimes pamphlets or an intervention group (IG) that additionally received the READY-Girls program over three consecutive visits attached to their routine clinic visits. A trained research nurse/research associate prepared the computer in a private room for data collection and DVD program viewing. At baseline, IG participants were given DVD-1; they received boosters at 3 (DVD-2) and 6 months (book). The first DVD session, which provided evidenced-based information, had a mean viewing time of 36.3 min (±6.2) (6). The second DVD, which included exercises to apply information about PC from DVD-1, had a mean viewing time of 25.4 min (± 7.4) (6). The third session, in which IG teens read a book that reinforced the information in DVD-1, had a mean reading time of 20.4 min (± 4.0) (6). To ensure that the subjects read the book during their clinic visit, small detachable inserts instructing them to remove the tab and hand it to the research nurse were randomly placed inside the pages.
Data were collected by validated computer-based, self-administered questionnaires pre/post intervention (IG) (or pamphlet [CG]) at baseline, each booster session (3 and 6 months), and the 12-month follow-up. The protocol and READY-Girls materials were approved by the institutional review boards at both institutions, and teen assent and parental consent were obtained from all participants. Outcome measures included diabetes and reproductive health knowledge, attitudes/beliefs based on the Expanded Health Belief Model (intention, self-efficacy, benefits, and barriers to seeking PC and using effective family planning; perceived severity and risks of pregnancy-related complications) (10), behaviors related to family planning, initiation of PC, and discussions with HCP.
Reproductive health knowledge was evaluated by 80 items. The split-half method was used to measure instrument reliability and to statistically separate items to differentiate the pretest from the posttest. Questions were multiple choice problem-solving vignettes developed by the mental model technique with groups of expert health professionals and teens with diabetes (8). The total scale (80 items) measures knowledge of diabetes and pregnancy, puberty, contraception, and sexuality, and general family planning, general diabetes, and PC (14 items). Scores were summed and based on 100% correctness. Because PC was the major focus of this study, we reported on both the total reproductive health knowledge score and the PC subscale score (total scale: Cronbach α = 0.71; test-retest reliability r = 0.76). Other variables were assessed by summated Likert-type scales from the validated Reproductive Health Attitudes and Behavior (RHAB) questionnaire described elsewhere (10), where higher scores indicated greater levels of the construct. Psychometric properties of RHAB were reanalyzed for this sample. Results indicate robust measures, with all scale scores having Cronbach α ≥0.70 (Cronbach α: intention = 0.84; self-efficacy = 0.96; benefit = 0.88; barriers = 0.97; severity = 0.94; risk/susceptibility = 0.74). Data were analyzed using descriptive statistics and linear mixed and marginal modeling of the longitudinally assessed continuous and binary outcomes, respectively, to compare between- and within-group differences over time using SAS (version 9.3; SAS Institute, Inc., Cary, NC).
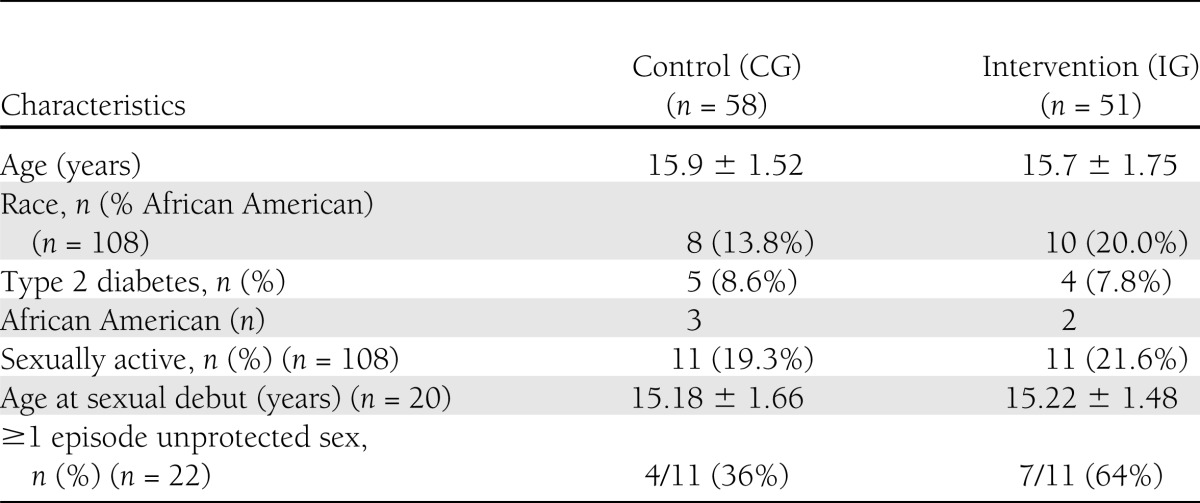
At the two study sites, 548 girls met the inclusion criteria for age. Reasons for not enrolling were as follows: ineligibility because they did not meet other inclusion criteria, loss of contact, clinic cancellations, and refusal. Moreover, most eligible patients with type 2 diabetes at these sites were already enrolled in the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study, which precluded them from participating in other studies (11). Potential subjects for our study were recruited in person at the clinics or by phone from a clinic list. Recruitment at both sites ended when the required sample size was reached. There were no significant differences between girls who were recruited for the study and those who were not for age; however, the girls recruited into the study had slightly higher mean HbA1c values at baseline (mean HbA1c = 8.9% [75 mmol/mol] vs. 8.2% [64 mmol/mol], P < 0.05). A sample of 113 subjects was recruited and randomized (109 had complete data) to either CG (n = 58) or IG (n = 51). For all participants (n = 109), the mean self-reported age was 15.8 years, range 13–19; 8.3% (n = 9) had type 2 diabetes; and 16.7% (n = 19) were African American. Attrition at 12 months was 16% (n = 18). At baseline, 20% (n = 22; CG = 11) had been sexually active, with a mean age at sexual debut of 15.4 years (range 12–18), and of these, 50% (11 of 22) had at least one episode of unprotected sex, 64% (n = 7) of IG teens vs. 36% (n = 4) of CG teens (P = 0.40). There were no significant demographic differences between groups at baseline (see Table 1).
Table 1.
Baseline characteristics of the study subjects (N = 109)
RESULTS
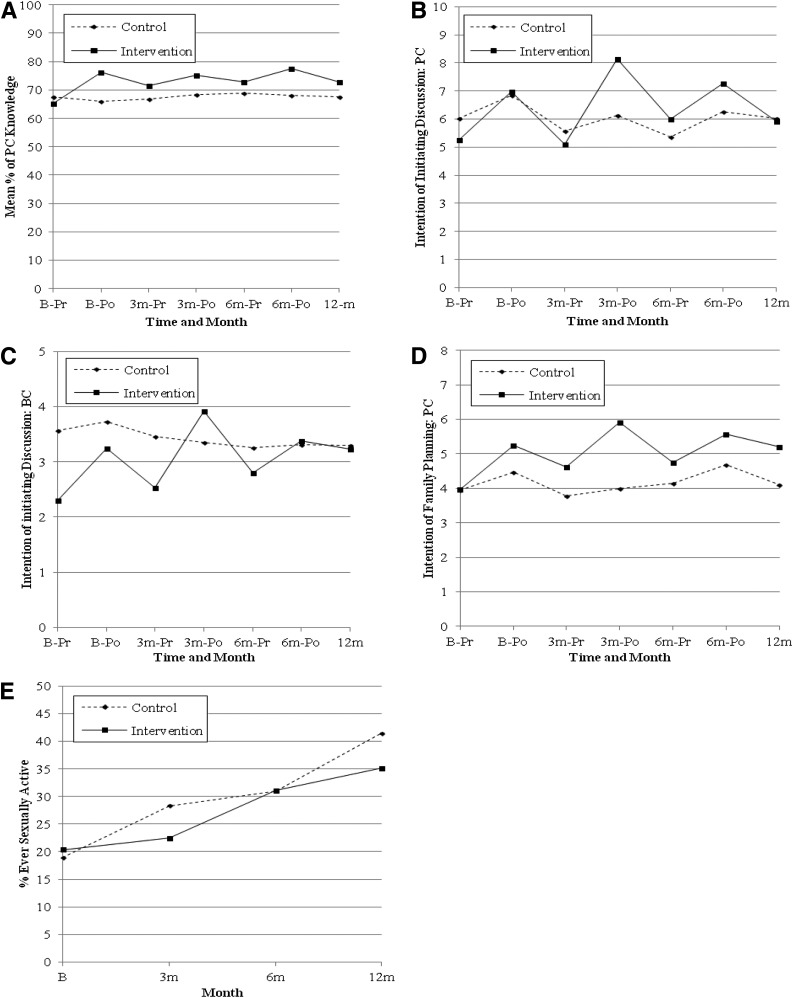
There were significant group-by-time interactions, showing improvement for IG teens in total and PC knowledge (F[6, 81.5] = 10.41, P < 0.0001; F[6, 541] = 4.05, P = 0.0005, respectively) (Fig. 1A for PC knowledge), intentions to initiate discussion with HCP regarding PC (F[6, 82.4] = 2.56, P = 0.0254) (Fig. 1B) and birth control (BC) (F[6, 534] = 3.40, P = 0.0027) (Fig. 1C), and intention to preplan pregnancies and seek PC (F[6, 534] = 2.58, P = 0.0180) (Fig. 1D). The jagged response pattern represents a booster effect, with each peak occurring immediately after a READY-Girls PC session (DVD or book). Although some significant positive changes in other attitudes/beliefs among IG teens appeared at given time points over 12 months, they did not have significant group-by-time interactions.
Figure 1.
Group-by-time effects of READY-Girls intervention over 12 months on PC knowledge (A), intentions to initiate discussion with HCPs regarding PC (B), intentions to initiate discussion with HCP regarding BC (C), intention to preplan pregnancies by family planning and seeking PC (D), and sexual debut (E). Time points are baseline (B), 3 months (3 m), 6 months (6 m), 12 months (12 m), and presession (Pr) and postsession (Po).
IG participants, compared with CG, showed a trend toward lower rates of overall sexual activity: less sexual debut (35 vs. 41%) (Fig. 1E) and increased abstinence (44 vs. 32%). Although not significant, these patterns were consistent over time. As expected over time, both groups showed an increase in becoming sexually active (χ2 [3] = 18.36, P = 0.0004). There were no significant group, time, or group-by-time effects for abstinence. With regard to risk-taking behaviors, there were no significant group-by-time effects or group or time differences at 12 months on the number of partners, unprotected sexual intercourse, or condom use, although fewer IG participants tended to engage in these risky behaviors at the 12-month follow-up visit (for example, 11% [n = 4] of CG vs. 0% of IG had multiple partners at 12 months).
To determine cost-effectiveness, we computed program delivery cost and compared the IG to CG on the probability of becoming pregnant. Self-reported outcome measures included a weighted probability of becoming pregnant calculated for each subject at each time point using an algorithm on the effectiveness and frequency of their BC methods used in the past 3 months. There appeared to be a trend in the direction of decreasing the probability of becoming pregnant for the IG teens and increasing for the CG teens (t = 1.715, P = 0.09).
Given the young age of this sample, none of the teens reported any actual PC-seeking behavior to plan a pregnancy. There were no pregnancies in either group during the course of the study.
CONCLUSIONS
We examined the long-term effects (12 months) of the booster-enhanced READY-Girls PC program for adolescent females with type 1 and type 2 diabetes on intentions and behaviors regarding family planning and seeking PC/preconception care. Booster-enhanced READY-Girls appeared to have long-term sustaining effects on intentions to initiate discussion with HCPs regarding diabetes, BC, and PC and trends on family planning behaviors that could improve reproductive health outcomes. According to cognitive behavioral theories, intention is among the strongest predictors of behavior (12).
Significant and sustained positive changes in intentions occurred after a booster. Jagged patterns were noted with the intention to initiate PC and BC discussions and to use family planning, indicating a booster effect; a spiked increase was observed after each booster. Boosters appeared to be an important component of the intervention. Interventions with boosters have been found to sustain the effectiveness of adolescent health behaviors, such as sexual risk reduction (7).
In a previous clinic-based study, the READY-Girls program added only 20 min to diabetes clinic time, at a resource utilization cost of $18, and was found to be cost-effective (6). Similar patterns were noted in this study. Trends were emerging whereby the probability of becoming pregnant decreased for the IG teens and increased for the CG teens.
Teens who received the READY-Girls intervention had greater knowledge of PC and reproductive health over time. Behavioral outcomes appeared to have positive trends with READY-Girls but did not remain significant over 12 months. READY-Girls had more significant effects on intentions and less effects on actual family planning or seeking PC care behavior. This could be due to the fact that most subjects were not yet sexually active, and it may have been too early to observe these behaviors and detect these effects. Also, this may have been affected by the small sample of teens who were sexually active.
In addition to the initial low number of teens reporting sexual activity in this study, there were some other limitations that could have explained some of the findings. The sample consisted of 109 adolescent girls with mostly type 1 diabetes. Although we recruited fewer teens with type 2 diabetes, their participation in this PC study for teens was unique and important. Because of the similarities in the risks to complications and disease management during a pregnancy for women with type 1 and type 2 diabetes, and because the questionnaires were the same for both, subjects with both type 1 and type 2 diabetes were included in the analyses. The majority of our sample was young (68% of teens were <17 years of age). These factors could limit the generalizability of our findings.
Future studies should explore a stronger, internal, more permanent booster. Providing knowledge and skills to the teen’s social network to boost support could have long-term behavioral effects. Follow-up studies of women receiving PC as teens on future preconception care behavior and pregnancy outcomes are warranted.
Strong boosters and providing PC at each clinic visit appear to play an important role in sustaining long-term effects. These findings suggest that READY-Girls intervention with boosters imparts knowledge and stimulates interest and discussion. It then becomes the responsibility of the HCP to seize these opportunities to build on this foundation and provide more individualized face-to-face counseling and care. Starting PC at puberty is imperative. The content and delivery of that message is the key to improving reproductive health outcomes in women with diabetes and their offspring.
Acknowledgments
This work was supported by Grant R01-HD-044097 from the National Institutes of Health (NIH)/Eunice Kennedy Shriver National Institute of Child Health and Human Development, the General Clinical Research Center of the Children’s Hospital of Pittsburgh (M01-RR-0084), the Pediatric Clinical and Translational Research Center (NIH/National Center for Research Resources/Clinical and Translational Science Award UL1-RR-024153), and the NIH/National Institute of Nursing Research/Center for Research in Chronic Disorders (P30-NR-03924).
No potential conflicts of interest relevant to this article were reported.
D.C.-P. was primarily responsible for the conception and design of the study in addition to data collection, integrity, and analysis and was the primary writer for this manuscript. S.M.S. and A.B.P. were responsible for data analysis and integrity. D.B., N.H.W., A.M.D., and J.J. participated in recruitment and conducting the study. P.S. was the project director for the grant. W.H.H., A.F.R.F., and L.M. were involved with the cost-analysis. M.D. and F.G. were involved with data management and subject correspondence. J.D. was primarily responsible for the conception and design of the study in addition to data collection, integrity, and analysis. D.C.-P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented at the 70th Scientific Sessions of the American Diabetes Association, Orlando, Florida, 25–29 June 2010, and the 71st Scientific Sessions of the American Diabetes Association, San Diego, California, 24–28 June 2011.
The authors give special thanks to the READY-Girls study participants. The authors also acknowledge the Center for Instructional Development and Distance Education at the University of Pittsburgh, Flipside Production Company, Amanda N. Botscheller (University of Pittsburgh), Wändi Bruine de Bruin (Carnegie Mellon University), Jessica Devido (University of Pittsburgh), Baruch Fischhoff (Carnegie Mellon University), Margaret Hannan (University of Pittsburgh), Mandy Holbrook and Mark Huneke (Carnegie Mellon University), and Margaret M. Maly, Kathleen Moltz, Angela Purleski, Rebecca Hunnicutt Farren, and Kerry Reynolds (Wayne State University).
References
- 1.Kitzmiller JL, Buchanan TA, Kjos S, Combs CA, Ratner RE. Pre-conception care of diabetes, congenital malformations, and spontaneous abortions. Diabetes Care 1996;19:514–541 [DOI] [PubMed] [Google Scholar]
- 2.Abma JC, Martinez GM, Mosher WD, et al. Teenagers in the United States: Sexual Activity, Contraceptive Use, and Childbearing, 2002 Atlanta, Georgia, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, December 2004 (Vital and Health Statistics, series 23, no. 24) [PubMed] [Google Scholar]
- 3.Charron-Prochownik D, Ferons-Hannan M, Sereika S, Becker D. Randomized efficacy trial of early preconception counseling for diabetic teens (READY-girls). Diabetes Care 2008;31:1327–1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association Standards of medical care in diabetes—2009. Diabetes Care 2009;32(Suppl. 1):S13–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charron-Prochownik D, Downs J. READY-Girls. Pittsburgh, PA, University of Pittsubrgh, 2009 [Google Scholar]
- 6.Fischl AF, Herman WH, Sereika SM, et al. Impact of a preconception counseling program for teens with type 1 diabetes (READY-Girls) on patient-provider interaction, resource utilization, and cost. Diabetes Care 2010;33:701–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaydos CA, Hsieh Y-H, Galbraith JS, Barnes M, Waterfield G, Stanton B. Focus-on-Teens, sexual risk-reduction intervention for high-school adolescents: impact on knowledge, change of risk-behaviours, and prevalence of sexually transmitted diseases. Int J STD AIDS 2008;19:704–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Downs JS, Arslanian S, de Bruin WB, et al. Implications of type 2 diabetes on adolescent reproductive health risk: an expert model. Diabetes Educ 2010;36:911–919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Najjar LJ. Multimedia information and learning. Journal of Educational Multimedia and Hypermedia 1996;5:129–150 [Google Scholar]
- 10.Charron-Prochownik D, Wang S-L, Sereika SM, Kim Y, Janz NK. A theory-based reproductive health and diabetes instrument. Am J Health Behav 2006;30:208–220 [DOI] [PubMed] [Google Scholar]
- 11.Copeland KC, Zeitler P, Geffner M, et al. TODAY Study Group Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. J Clin Endocrinol Metab 2011;96:159–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burns AC. The expanded health belief model as a basis for enlightened preventive health care practice and research. J Health Care Mark 1992;12:32–45 [PubMed] [Google Scholar]