Summary
Trachoma has been endemic in The Gambia for decades but national surveys indicate that the prevalence is falling. Risk factor data can help guide trachoma control efforts. This study investigated risk factors for active trachoma and ocular Chlamydia trachomatis infection in children aged below 10 years in two Gambian regions. The overall prevalence of C. trachomatis infection was only 0.3% (3/950) compared with 10.4% (311/2990) for active trachoma, therefore analyses were only performed for active trachoma. After adjustment, increased risk of trachoma was associated with being aged 1—2 years (odds ratio (OR) 2.20, 95% CI 1.07—4.52) and 3—5 years (OR 3.62, 95% CI 1.80—7.25) compared with <1 year, nasal discharge (OR 2.07, 95% CI 1.53—2.81), ocular discharge (OR 2.68, 95% CI 1.76—4.09) and there being at least one other child in the household with active trachoma (OR 11.28, 95% CI 8.31—15.31). Compared with other occupations, children of traders had reduced risk (OR 0.53, 95% CI 0.30—0.94). At the household level, only the presence of another child in the household with active trachoma was associated with increased risk of active trachoma, suggesting that current trachoma control interventions are effective at this level. In contrast, child-level factors were associated with increased risk after adjustment, indicating a need to increase control efforts at the child level.
Keywords: Trachoma, Chlamydia trachomatis, Prevalence, Risk factors, Control, The Gambia
1. Introduction
Trachoma, caused by the ocular serovars (A, B, Ba and C) of the bacterium Chlamydia trachomatis, is the leading infectious cause of blindness (Resnikoff et al., 2004). The presence of subepithelial follicles (trachomatous inflammation, follicular) and inflammation (trachomatous inflammation, intense) in the subtarsal conjunctiva are characteristic of active trachoma, which is usually found in children. Years of re-infection may result in conjunctival scarring, causing the eyelashes to turn inwards and scratch the cornea (trichiasis), eventually leading to corneal opacity and blindness. Trachoma is typically found in dry, dusty and poor communities. It is a focal disease, clustering in communities as well as in households. Transmission is thought to occur via flies, fingers and fomites, as well as coughing and sneezing, but the relative importance of these routes has not been ascertained (Mabey et al., 2003).
The Gambia provides the typical environment for trachoma endemicity, being one of the poorest countries in the world and located in the dry, arid Sahel belt of West Africa. Although trachoma has been endemic in The Gambia for decades, two national surveys showed that the prevalence of active trachoma in 0—14 year olds fell from 10.4% in 1986 to 4.9% in 1996 (Dolin et al., 1998). With this decline in trachoma prevalence, control efforts now need to focus on those at greatest risk of trachoma.
The WHO aims to achieve global elimination of trachoma as a cause of blindness by the year 2020 (GET2020) through employment of the SAFE strategy (Surgery for trichiasis, Antibiotics for active disease, Facial cleanliness, and Environmental improvement) (WHO, 1997). In accordance with the WHO strategy, The Gambia’s National Eye Care Programme (NECP) has implemented a number of trachoma control activities. These include training village health workers in primary eye care, covering health promotion activities, identification and referral of trichiasis cases, and recognition and treatment of conjunctivitis. School children are screened for trachoma, encouraged to wash their faces and provided with tetracycline eye ointment when they present with active inflammation (Faal et al., 2000). However, at the time of the survey The Gambia had not yet received a donation of the antibiotic azithromycin for mass treatment from Pfizer via the International Trachoma Initiative (ITI).
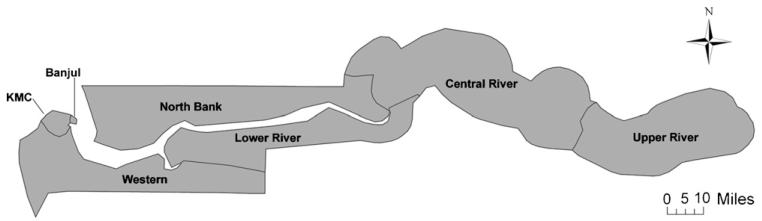
Since knowledge of risk factors associated with trachoma in particular settings can help guide focused interventions, risk factor data are of importance to The Gambia’s NECP. Such knowledge could also help to elucidate the transmission routes of trachoma, which are as yet incompletely understood. Previous risk factor studies looking at active trachoma and ocular C. trachomatis infection in The Gambia have been conducted in a limited geographical area (Bailey et al., 1989, 1991; Burton et al., 2003; Emerson et al., 2000a; Mabey et al., 1992). This study reports the results of a risk factor study conducted as part of a cross-sectional survey covering The Gambia’s Lower River Region (LRR) and North Bank Region (NBR) (Figure 1).
Figure 1.
Map of The Gambia, separated by region.
2. Methods
2.1. Sampling selection
A two-stage cluster random sampling strategy, with probability of selection proportional to size, was employed. In the first stage, 61 enumeration areas (EA) (settlements of approximately the same population size) were randomly selected (42 in NBR and 19 in LRR). The number of households per EA, with the name of each household head, was recorded. In the second stage, households were randomly selected from each EA. For each EA, a list of random numbers between 0 and 1 was generated using the ‘=RAND()’ command in Microsoft Excel v. 2002 (Microsoft Corp., Redmond, WA, USA). The number was then divided by the reciprocal of the number of households per EA. Households were selected sequentially from the top of this list, with duplicates excluded. An enumeration team went to the households in the order they had been selected and listed all household members who had slept in the village the night before (the de facto population) until more than 50 children per EA were enumerated. Infant welfare cards, given to mothers to record their child’s immunisations, were used where possible to confirm children’s dates of birth. A risk factor questionnaire, including questions on household head basic demographics, income, education, latrine availability and access to water, was administered to heads of all households with children.
2.2. Clinical examination
Children were examined in the same order as they had been selected until a total of 50 children per EA was obtained. In both LRR and NBR, children aged 0—9 years were examined for clinical signs of trachoma using a 2.5× magnifying loupe and classified according to the WHO simplified grading system: TF (trachomatous inflammation, follicular); TI (trachomatous inflammation, intense); TS (trachomatous conjunctival scarring); TT (trachomatous trichiasis); and CO (corneal opacity) (Thylefors et al., 1987).
Trachoma was graded by two experienced examiners whose observations are regularly validated by testing with the WHO trachoma grading slides, with an in-house slide and photograph collection and in the course of numerous field studies. In validation sessions the examiners were required to achieve a chance corrected agreement (Cohen’s κ statistic) with the standard over the scoring of active disease (TF and/or TI) of ≥0.8.
In LRR only, two ocular swabs were taken from the everted tarsal conjunctiva of the child’s right eye using a highly standardised technique (Solomon et al., 2003). A dry Dacron polyester-tipped swab (Hardwood Products Company, Gilford, ME, USA) was used. Labels with unique identification numbers linked the children’s swab samples and data collection forms. To avoid cross-contamination, the examiner wore a new pair of gloves for each participant. Another fieldworker passed the swab to the examiner, so the examiner only ever touched the stem of the swab. The presence of ocular and nasal discharge, dirt on the face and flies on the face at the time of examination were recorded for each child. Written (signature or thumbprint) informed consent was obtained from the guardians of all participants.
2.3. Laboratory methods
The first swab was processed in the field using a point-of-care test (data not presented). The second swab was kept cool in the field, frozen within 10 h and processed by the highly sensitive qualitative Amplicor PCR assay (Roche Molecular Systems, Branchburg, NJ, USA) at MRC Laboratories, The Gambia. A blind panel of samples provided by the WHO was successfully completed by the laboratory technicians. The manufacturer’s instructions were followed except for sample preparation, where a previously used procedure for ocular swabs was employed (Solomon et al., 2003). Both C. trachomatis DNA and the master mix internal control sequence were tested to identify inhibited samples. Inhibited samples were re-tested with a 1:10 dilution of 50/50 lysis buffer/specimen diluent and, if still inhibited, with a 1:100 dilution.
2.4. Statistical analysis
Results were double-entered by different entry clerks and verified in Microsoft Access (version 2000/2003XP). Data cleaning and analyses were performed in Stata version 9.2 (Stata Corp., College Station, TX, USA). Any discrepancies after verification and cleaning were checked against the original paper forms. Analyses were performed both at the child and household levels. No village-level covariates were measured. Univariate and multivariate analyses were performed using random-effects logistic GLLAMM (generalised linear latent and mixed models) modelling to account for between-household and between-EA variation (Rabe-Hesketh et al., 2002). Statistical significance of between-household and between-EA variation in the null model was estimated from Wald test statistics of the variation estimates. The design effect was calculated using the Stata ‘svy’ command for complex survey data using household as the sampling unit. Two univariate analyses were run to compare the effect estimates when including all children examined with children for whom there were no missing values for the potential risk factors investigated. Multivariate analyses were conducted on children with no missing data points. A forward stepwise model-building approach was used, including risk factors at the 5% significance level in the univariate analyses, and models were compared using the likelihood ratio test (LRT).
3. Results
A total sample of 2990 children aged 0—9 years was examined. Overall, 311 children (10.4%, 95% CI 9.3—11.6%) had active trachoma (11.9% (113/950) in LRR and 9.7% (198/2040) in NBR), of which only 1 child in NBR had TI only. Using the WHO indicator for treatment decisions, 298/2777 children (10.7%, 95% CI 8.7—13.1%) aged 1—9 years had TF overall (12.3% (108/876) in LRR and 10.0% (190/1901) in NBR). Of the 950 children in LRR from whom ocular swabs were taken, only 3 (0.3%, 95% CI 0.07—0.9%) were positive by PCR (all three confirmed positive by a real-time PCR targeting the omp1 gene, using a previously described methodology (Solomon et al., 2003)). Therefore, risk factor analyses were only performed for active trachoma.
The GLLAMM null model indicated strong evidence of variation both between households (Wald P < 0.001) and between EAs (Wald P = 0.004). The overall household design effect was 1.922. Univariate associations suggested increased risk of active trachoma (P < 0.01) for the following child-level factors: being aged 1—2 years or 3—5 years compared with <1 year, having dirt on the face, nasal discharge, ocular discharge or unclean face (nasal discharge or ocular discharge or flies on the face or dirt on the face) (Table 1). The sex of the child and flies on the face at the time of examination were not associated with risk of trachoma (P > 0.1). At the household level, increased risk of active trachoma was associated with another child in the household having active trachoma (P < 0.001), and there was reduced risk for children of traders compared with all other occupations (P = 0.019).
Table 1.
Random effects logistic regression modelling of child- and household-level risk factors for active trachoma (TF and/or TI in either eye) in children aged 0—9 years
| Characteristic | No. of children <10 yearsa |
No. with active trachoma (%) |
Univariate analysisa |
Multivariate analysisb |
||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | Wald test P-value |
OR | 95% CI | Wald test P-value |
|||
| Child-level variables | ||||||||
| Age (years)c | ||||||||
| ≤1 | 213 | 12 (5.6) | 1.00 | 1.00 | ||||
| 1—2 | 542 | 71 (13.1) | 2.56 | 1.28—5.12 | 0.008 | 2.20 | 1.07—4.52 | 0.033 |
| 3—5 | 798 | 136 (17.0) | 3.94 | 2.02—7.67 | <0.001 | 3.62 | 1.80—7.25 | <0.001 |
| 6—9 | 1437 | 92 (6.4) | 1.03 | 0.53—2.02 | 0.927 | 1.20 | 0.59—2.41 | 0.618 |
| Sex | ||||||||
| Male | 1482 | 152 (10.3) | 1.00 | — | — | — | ||
| Female | 1508 | 159 (10.5) | 1.06 | 0.81—1.38 | 0.693 | — | — | — |
| Dirty face | ||||||||
| No | 2178 | 166 (7.6) | 1.00 | — | ||||
| Yes | 727 | 126 (17.3) | 3.39 | 2.44—4.70 | <0.001 | — | — | — |
| Ocular discharge | ||||||||
| No | 2686 | 231 (8.6) | 1.00 | 1.00 | ||||
| Yes | 219 | 62 (28.3) | 5.37 | 3.52—8.19 | <0.001 | 2.68 | 1.76—4.09 | <0.001 |
| Nasal discharge | ||||||||
| No | 1789 | 116 (6.5) | 1.00 | 1.00 | ||||
| Yes | 1119 | 177 (15.8) | 3.40 | 2.52—4.59 | <0.001 | 2.07 | 1.53—2.81 | <0.001 |
| Flies on face | ||||||||
| No | 2867 | 287 (10.0) | 1.00 | — | — | — | ||
| Yes | 33 | 5 (15.2) | 2.44 | 0.79—7.50 | 0.121 | — | — | — |
| Unclean faced | ||||||||
| No | 1667 | 91 (5.5) | 1.00 | 1.00e | ||||
| Yes | 1243 | 203 (16.3) | 4.45 | 3.25—6.09 | <0.001 | 3.17 | 2.33—4.30 | <0.001 |
| Household head variables | ||||||||
| Age of household head (years) | ||||||||
| <30 | 84 | 4 (4.8) | 1.00 | — | — | — | ||
| 30—49 | 1094 | 108 (9.9) | 2.78 | 0.67—11.63 | 0.160 | — | — | — |
| 50—69 | 1360 | 145 (10.7) | 2.99 | 0.72—12.47 | 0.132 | — | — | — |
| >69 | 452 | 54 (11.9) | 3.72 | 0.85—16.22 | 0.081 | — | — | — |
| Sex of household head | ||||||||
| Male | 2720 | 280 (10.3) | 1.00 | — | — | — | ||
| Female | 270 | 31 (11.5) | 1.26 | 0.72—2.21 | 0.419 | — | — | — |
| Country of birth of household head | ||||||||
| The Gambia | 2781 | 295 (10.6) | 1.00 | — | — | — | ||
| Elsewhere | 209 | 16 (7.7) | 0.84 | 0.40—1.76 | 0.644 | — | — | — |
| Ethnic group of household head | ||||||||
| Mandinka | 1486 | 158 (10.6) | 1.00 | — | — | — | ||
| Other | 1504 | 153 (10.2) | 1.01 | 0.65—1.55 | 0.978 | — | — | — |
| Education of household head | ||||||||
| Yes | 1374 | 139 (10.1) | 1.00 | — | — | — | ||
| No | 1616 | 172 (10.6) | 1.16 | 0.80—1.68 | 0.447 | — | — | — |
| Type of education | ||||||||
| Arabic | 944 | 97 (10.3) | 1.00 | — | — | — | ||
| Western | 417 | 42 (10.1) | 0.98 | 0.52—1.84 | 0.958 | — | — | — |
| Education level | ||||||||
| Basic primary | 247 | 27 (10.9) | 1.00 | — | — | — | ||
| Middle | 177 | 22 (12.4) | 1.51 | 0.61—3.78 | 0.376 | — | — | — |
| Senior secondary | 88 | 8 (9.1) | 0.51 | 0.12—2.26 | 0.375 | — | — | — |
| College | 31 | 2 (6.5) | 0.72 | 0.09—5.87 | 0.756 | — | — | — |
| Occupation | ||||||||
| Other occupation | 2678 | 292 (10.9) | 1.00 | 1.00 | ||||
| Trader | 312 | 19 (6.1) | 0.45 | 0.23—0.88 | 0.019 | 0.53 | 0.30—0.94 | 0.03 |
| Monthly income | ||||||||
| <US$1/day | 2516 | 264 (10.5) | 1.00 | — | — | — | ||
| >US$1/day | 459 | 46 (10.0) | 1.04 | 0.64—1.70 | 0.873 | — | — | — |
| Household variables | ||||||||
| Other child with active trachoma in household | ||||||||
| No | 2448 | 121 (4.9) | 1.00 | 1.00 | ||||
| Yes | 542 | 190 (35.1) | 10.56 | 8.01—13.92 | <0.001 | 11.28 | 8.31—15.31 | <0.001 |
| No. of people in household | 2990 | 311 (10.4) | 1.02 | 1.00—1.04 | 0.097 | — | — | — |
| No. of adults in household | 2990 | 311 (10.4) | 1.02 | 0.99—1.06 | 0.213 | — | — | — |
| No. of children in household | 2990 | 311 (10.4) | 1.04 | 1.00—1.09 | 0.061 | — | — | — |
| Latrine presence | ||||||||
| Yes | 2602 | 273 (10.5) | 1.00 | — | — | — | ||
| No | 388 | 38 (9.8) | 1.01 | 0.59—1.73 | 0.963 | — | — | — |
| Latrine shared or private | ||||||||
| Shared | 2469 | 256 (10.4) | 1.00 | — | — | — | ||
| Private | 130 | 17 (13.1) | 1.57 | 0.60—4.12 | 0.358 | — | — | — |
| Water source | ||||||||
| Tap | 1548 | 176 (11.4) | 1.00 | — | — | — | ||
| Covered well with hand | 971 | 100 (10.3) | 1.08 | 0.65—1.81 | 0.754 | — | — | — |
| pump | ||||||||
| Uncovered well | 451 | 34 (7.5) | 0.90 | 0.46—1.76 | 0.750 | — | — | — |
| Borehole | 20 | 1 (5.0) | 0.51 | 0.04—6.14 | 0.598 | — | — | — |
| Distance to water source | ||||||||
| <1 km | 2911 | 302 (10.4) | 1.00 | — | — | — | ||
| >1 km | 79 | 9 (11.4) | 1.22 | 0.41—3.61 | 0.726 | — | — | — |
| Time to water source | ||||||||
| <30min | 2845 | 297 (10.4) | 1.00 | — | — | — | ||
| >30min | 145 | 14 (9.7) | 1.03 | 0.45—2.33 | 0.949 | — | — | — |
TF, trachomatous inflammation, follicular; TI, trachomatous inflammation, intense; OR, odds ratio.
Based on all children for whom data were available of the 2990 examined children.
Adjusted for child age, ocular and nasal discharge, another child in the household with active trachoma and occupation.
Age <1 year represents children aged ≤12 months, 1—2 years is children aged 13—36 months, 3—5 years is 37—72 months and 6—9 years is 73—120 months.
Unclean face comprised dirty face, ocular discharge, nasal discharge or flies on the face combined.
Adjusted for child age, another child in the household with active trachoma, occupation and unclean face.
Ninety-five children (22 in LRR and 73 in NBR) had missing values for potential risk factors. There were negligible differences in the univariate analyses for all children examined (2990 children) compared with those with no missing values (2895 children) in effect estimates and corresponding 95% CIs. Therefore, these 95 children were excluded from the multivariate analyses. Of the 2895 children included in the multivariate analyses, 290 had active trachoma (10.0%, 95% CI 8.9—11.2%).
In the multivariate analysis adjusting for young age, another child in the household with active trachoma, occupation and unclean face all remained significantly associated with active trachoma. When unclean face was separated into its four component parts, being aged 1—5 years, having ocular discharge, having nasal discharge, another child in the household with active trachoma or household head occupation being a trader were significantly associated with active trachoma. After adjustment for these risk factors, there was no evidence to suggest having dirt on the face further increased the risk of active trachoma (LRT, P = 0.161), indicating that the univariate effect of dirty face is absorbed by ocular and nasal discharge.
In both the univariate and multivariate analyses, accounting for another child in the household with active trachoma meant that the between-household variation disappeared and the estimated between-EA variation reduced by approximately 75%.
4. Discussion
National trachoma control efforts, including distribution of tetracycline eye ointment, have been in place in The Gambia since the mid-1980s (Faal et al., 2000) but there has not yet been a mass antibiotic treatment campaign. This risk factor study has shown that child-level factors still pose strong risks of active disease and potential transmission. Being of young age is a recognised risk factor for active trachoma in The Gambia (Bailey et al., 1991; Emerson et al., 2004) and elsewhere. The risk of active trachoma increased with age up to 5 years, but thereafter fell with increasing age. The association between young age and trachoma is probably because children are in close contact with each other thus facilitating transmission as well as the fact that the duration of disease episodes declines with age, most likely due to acquired immunity (Bailey et al., 1999).
In our study, faces with dirt on them, ocular discharge and nasal discharge were prevalent (25.0% (727/2905), 7.5% (219/2905) and 38.5% (1119/2908), respectively), but flies were present on only 1.1% (33/2900) of children’s faces at the time of examination. Our definition of ‘dirty face’ was the presence of dirt on the face. In other studies, dirty face has been characterised by the presence of ocular and/or nasal discharge (Abdou et al., 2007; Gower et al., 2006; Ngondi et al., 2007; Schemann et al., 2002; West et al., 1995, 1996). Although multivariate analyses combining all four unclean face components demonstrated a strong overall association with increased risk of trachoma, in analyses separating the components, dirt on the face was no longer associated with active trachoma. Discharge (ocular or nasal), but not the other factors, was associated with active trachoma in The Gambia. Similarly, a study aimed at developing a standard definition of a clean face has suggested that ocular discharge was the only component related to active trachoma after accounting for other potential confounders, and that flies, nasal discharge and ocular discharge provided the best interobserver agreement (Jonathan King, personal communication). The reliability of unclean faces as an indicator of trachoma merits attention, as national programmes supported by the ITI are encouraged to report this indicator and to use it as a measure of trachoma risk and success of face-washing campaigns. Since in our study the prevalence of flies was low but that of discharge was relatively high, and we only examined 50 randomly selected children per EA, we believe that the children’s faces were not additionally cleaned prior to examination. Thus, discharge appears to be the most reliable indicator of an unclean face associated with active trachoma.
Interestingly, ocular and nasal discharge explained the univariate association of dirt on the face with active trachoma. This may be because the discharge meant that dirt was more likely to stick to the face. However, the causal relationship between nasal and ocular discharge with active trachoma is unclear, as it is possible that discharge is both a cause and effect. Discharge could lead to transmission either directly, or indirectly through infected hands, clothing or the Musca sorbens fly species, which accounts for the vast majority of fly—eye contact. Indeed, Gambian children with ocular or nasal discharge have been noted to have twice as many fly—eye contacts as children with no discharge (Emerson et al., 2000a). Alternatively, discharge could be a consequence of having trachoma, as this in itself could result in the eye and nose producing discharge. Facewashing campaigns could therefore help curb the spread of trachoma, although the evidence base for this control strategy is limited and health education alone does not result in effective behaviour change (Edwards et al., 2006; West et al., 1995).
In our study, only 1.1% of children (33/2900) had flies on their face at the time of examination, and the presence of flies was not associated with active trachoma. This finding could be due to the study being conducted in the dry season, as flies are more prevalent in the wet season (Emerson et al., 2000a). It may also be a result of the high proportion of households with access to a latrine, as the presence of pit latrines has been associated with decreased density of M. sorbens (Emerson et al., 2000b, 2004).
The high prevalence of latrine access may also explain the lack of an association between latrines and active trachoma. When latrine access is low, an association with active trachoma has been found in The Gambia (Burton et al., 2003). Musca sorbens preferentially breeds in human faeces (Emerson et al., 2001), but is not found exiting latrines (Emerson et al., 2005). It is likely that latrines lead to reduced fly—eye contact, ultimately hindering transmission. With 84.8% of households (631/744) reporting access to a latrine, it is unsurprising that no association between latrine access and active trachoma was found in this study.
There was also no association between distance or time to a water source and active trachoma, supporting previous findings from The Gambia (Bailey et al., 1989). Water availability is good in The Gambia (Burton et al., 2005) and in our study 97.6% of households (726/744) reported being within 1 km of their primary water source and 94.2% (701/744) were less than 30 min away. This demonstrates the success of efforts to improve water supply to rural areas in The Gambia (Dolin et al., 1997). In other settings where water is scarcer, distance to a water source has been a risk factor for trachoma (Baggaley et al., 2006; Schemann et al., 2002). However, it appears from the relatively high prevalence of unclean faces that the relatively good access to water observed has not translated into good personal hygiene practices in this setting.
Clustering of active trachoma within households, measured as another child aged 0—9 years with TF and/or TI in the same household, was the only household-level factor associated with increased risk of active trachoma, after accounting for any possible underlying and unmeasured clustering at household and EA level in regression analyses. Studies previously conducted in The Gambia have demonstrated clustering at village, compound and bedroom levels (Bailey et al., 1989, 1994; Burton et al., 2003; Mabey et al., 1992). These findings support the idea of within-household transmission, indicating the importance of directing control efforts at individuals with trachoma as well as those with whom they have close contact. Interestingly, of the three PCR-positive cases in our study, two were from the same household.
Households where the heads were traders experienced less active trachoma than households where the heads had other occupations. This differs from previous findings in The Gambia where no association was found with fathers having a salary or income from trading (Bailey et al., 1991). Our finding may be indicative of traders having a socioeconomically higher status, despite the lack of association observed between monthly income and active trachoma. Perhaps a better measure of socioeconomic status would have been ownership of possessions, as Bailey et al. (1991) did note that families with no active trachoma owned more possessions than families in which at least one child had trachoma.
Our risk factor study was designed to be simple in order to increase participation and to make the study logistically manageable. We therefore asked a limited number of questions and did not support these with observational data, such as water-use behaviour or evidence of latrine use. This may have led to us missing more subtle or complex relationships between risk factors and active trachoma.
The current WHO definition of elimination of trachoma as a public health concern is <5% TF in children aged 1—9 years. The survey of active disease and ocular infection with C. trachomatis conducted alongside this risk factor study showed that both the NBR and LRR fulfilled the WHO criteria for mass antibiotic treatment (having a TF prevalence of ≥10% in children aged 1—9 years). However, only three ocular swabs from LRR yielded PCR-positive results, suggesting that elimination of infection may already be close. Control interventions would ideally be focused on the communities in which infection remains, but detecting such communities remains a problem. Identifying the remaining risk factors for active trachoma could help The Gambia reduce its prevalence of active trachoma and consequently achieve the WHO’s definition of trachoma elimination.
In conclusion, the effectiveness of the NECP’s efforts to control trachoma is evident from these risk factor results. Few household-level factors were associated with active trachoma, suggesting that the different interventions introduced over time have been effective at the household level. However, it would appear that the interventions have not translated down the hierarchy of risk factors to the child level. Similar results have been obtained in Ethiopia following mass delivery of azithromycin (Edwards et al., 2008), indicating that in low prevalence or mass-treated communities risk factors reside at the child level. It therefore seems that The Gambia could increase its focus on child-level risk factors, but should maintain household-level control interventions, especially for households containing at least one child with active trachoma.
Acknowledgements
The authors would like to thank the village leaders and villagers for participating in this study, as well as Bakary Ceesay, Jawo Colley, Bakary Gibba, Abdoulie Jallow, Hassan Joof, Mass Laye, Pateh Makalo and Binta Sonko for their work in the field. Thanks to Kaddy Conteh and Haddy Kanyi for help with data entry, and to Kebba Touray for the map of The Gambia. Thanks also to Aura Aguirre-Andreasen for laboratory support.
Funding: Wellcome Trust, London, UK (reference: 078460/Z/05/Z).
Footnotes
Conflicts of interest: None declared.
Ethical approval: Ethics Committee of the London School of Hygiene and Tropical Medicine (LSHTM), UK; and Joint Ethics Committee of The Gambian Government/UK Medical Research Council (MRC), The Gambia.
References
- Abdou A, Nassirou B, Kadri B, Moussa F, Munoz BE, Opong E, West SK. Prevalence and risk factors for trachoma and ocular Chlamydia trachomatis infection in Niger. Br. J. Ophthalmol. 2007;91:13–17. doi: 10.1136/bjo.2006.099507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggaley RF, Solomon AW, Kuper H, Polack S, Massae PA, Kelly J, Safari S, Alexander ND, Courtright P, Foster A, Mabey DC. Distance to water source and altitude in relation to active trachoma in Rombo district, Tanzania. Trop. Med. Int. Health. 2006;11:220–227. doi: 10.1111/j.1365-3156.2005.01553.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey R, Osmond C, Mabey DC, Whittle HC, Ward ME. Analysis of the household distribution of trachoma in a Gambian village using a Monte Carlo simulation procedure. Int. J. Epidemiol. 1989;18:944–951. doi: 10.1093/ije/18.4.944. [DOI] [PubMed] [Google Scholar]
- Bailey R, Downes B, Downes R, Mabey D. Trachoma and water use; a case control study in a Gambian village. Trans. R. Soc. Trop. Med. Hyg. 1991;85:824–828. doi: 10.1016/0035-9203(91)90470-j. [DOI] [PubMed] [Google Scholar]
- Bailey R, Hayes L, Pickett M, Whittle H, Ward M, Mabey D. Molecular epidemiology of trachoma in a Gambian village. Br. J. Ophthalmol. 1994;78:813–817. doi: 10.1136/bjo.78.11.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey R, Duong T, Carpenter R, Whittle H, Mabey D. The duration of human ocular Chlamydia trachomatis infection is age dependent. Epidemiol. Infect. 1999;123:479–486. doi: 10.1017/s0950268899003076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton MJ, Holland MJ, Faal N, Aryee EA, Alexander ND, Bah M, Faal H, West SK, Foster A, Johnson GJ, Mabey DC, Bailey RL. Which members of a community need antibiotics to control trachoma? Conjunctival Chlamydia trachomatis infection load in Gambian villages. Invest. Ophthalmol. Vis. Sci. 2003;44:4215–4222. doi: 10.1167/iovs.03-0107. [DOI] [PubMed] [Google Scholar]
- Burton MJ, Holland MJ, Makalo P, Aryee EA, Alexander ND, Sillah A, Faal H, West SK, Foster A, Johnson GJ, Mabey DC, Bailey RL. Re-emergence of Chlamydia trachomatis infection after mass antibiotic treatment of a trachoma-endemic Gambian community: a longitudinal study. Lancet. 2005;365:1321–1328. doi: 10.1016/S0140-6736(05)61029-X. [DOI] [PubMed] [Google Scholar]
- Dolin PJ, Faal H, Johnson GJ, Minassian D, Sowa S, Day S, Ajewole J, Mohamed AA, Foster A. Reduction of trachoma in a sub-Saharan village in absence of a disease control programme. Lancet. 1997;349:1511–1512. doi: 10.1016/s0140-6736(97)01355-x. [DOI] [PubMed] [Google Scholar]
- Dolin PJ, Faal H, Johnson GJ, Ajewole J, Mohamed AA, Lee PS. Trachoma in The Gambia. Br. J. Ophthalmol. 1998;82:930–933. doi: 10.1136/bjo.82.8.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards T, Cumberland P, Hailu G, Todd J. Impact of health education on active trachoma in hyperendemic rural communities in Ethiopia. Ophthalmology. 2006;113:548–555. doi: 10.1016/j.ophtha.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Edwards T, Harding-Esch EM, Hailu G, Andreason A, Mabey DC, Todd J, Cumberland P. Risk factors for active trachoma and Chlamydia trachomatis infection in rural Ethiopia after mass treatment with azithromycin. Trop. Med. Int. Health. 2008;13:556–565. doi: 10.1111/j.1365-3156.2008.02034.x. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Bailey RL, Mahdi OS, Walraven GE, Lindsay SW. Transmission ecology of the fly Musca sorbens, a putative vector of trachoma. Trans. R. Soc. Trop. Med. Hyg. 2000a;94:28–32. doi: 10.1016/s0035-9203(00)90427-9. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Cairncross S, Bailey RL, Mabey DC. Review of the evidence base for the ‘F’ and ‘E’ components of the SAFE strategy for trachoma control. Trop. Med. Int. Health. 2000b;5:515–527. doi: 10.1046/j.1365-3156.2000.00603.x. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Bailey RL, Walraven GE, Lindsay SW. Human and other faeces as breeding media of the trachoma vector Musca sorbens. Med. Vet. Entomol. 2001;15:314–320. doi: 10.1046/j.0269-283x.2001.00318.x. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Lindsay SW, Alexander N, Bah M, Dibba SM, Faal HB, Lowe KO, McAdam KP, Ratcliffe AA, Walraven GE, Bailey RL. Role of flies and provision of latrines in trachoma control: cluster-randomised controlled trial. Lancet. 2004;363:1093–1098. doi: 10.1016/S0140-6736(04)15891-1. [DOI] [PubMed] [Google Scholar]
- Emerson PM, Simms VM, Makalo P, Bailey RL. Household pit latrines as a potential source of the fly Musca sorbens—-a one year longitudinal study from The Gambia. Trop. Med. Int. Health. 2005;10:706–709. doi: 10.1111/j.1365-3156.2005.01432.x. [DOI] [PubMed] [Google Scholar]
- Faal H, Minassian DC, Dolin PJ, Mohamed AA, Ajewole J, Johnson GJ. Evaluation of a national eye care programme: re-survey after 10 years. Br. J. Ophthalmol. 2000;84:948–951. doi: 10.1136/bjo.84.9.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gower EW, Solomon AW, Burton MJ, Aguirre A, Munoz B, Bailey R, Holland M, Makalo P, Massae P, Mkocha H, Mabey DC, West SK. Chlamydial positivity of nasal discharge at baseline is associated with ocular chlamydial positivity 2 months following azithromycin treatment. Invest. Ophthalmol. Vis. Sci. 2006;47:4767–4771. doi: 10.1167/iovs.05-1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabey DC, Bailey RL, Ward ME, Whittle HC. A longitudinal study of trachoma in a Gambian village: implications concerning the pathogenesis of chlamydial infection. Epidemiol. Infect. 1992;108:343–351. doi: 10.1017/s0950268800049815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabey DC, Solomon AW, Foster A. Trachoma. Lancet. 2003;362:223–229. doi: 10.1016/S0140-6736(03)13914-1. [DOI] [PubMed] [Google Scholar]
- Ngondi J, Matthews F, Reacher M, Onsarigo A, Matende I, Baba S, Brayne C, Zingeser J, Emerson P. Prevalence of risk factors and severity of active trachoma in southern Sudan: an ordinal analysis. Am. J. Trop. Med. Hyg. 2007;77:126–132. [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A, Pickels A. Reliable estimation of generalized linear mixed models using adaptive quadrature. Stata J. 2002;2:1–21. [Google Scholar]
- Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP. Global data on visual impairment in the year 2002. Bull. World Health Organ. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- Schemann JF, Sacko D, Malvy D, Momo G, Traore L, Bore O, Coulibaly S, Banou A. Risk factors for trachoma in Mali. Int. J. Epidemiol. 2002;31:194–201. doi: 10.1093/ije/31.1.194. [DOI] [PubMed] [Google Scholar]
- Solomon AW, Holland MJ, Burton MJ, West SK, Alexander ND, Aguirre A, Massae PA, Mkocha H, Munoz B, Johnson GJ, Peeling RW, Bailey RL, Foster A, Mabey DC. Strategies for control of trachoma: observational study with quantitative PCR. Lancet. 2003;362:198–204. doi: 10.1016/S0140-6736(03)13909-8. [DOI] [PubMed] [Google Scholar]
- Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR. A simple system for the assessment of trachoma and its complications. Bull. World Health Organ. 1987;65:477–483. [PMC free article] [PubMed] [Google Scholar]
- West S, Munoz B, Lynch M, Kayongoya A, Chilangwa Z, Mmbaga BB, Taylor HR. Impact of face-washing on trachoma in Kongwa, Tanzania. Lancet. 1995;345:155–158. doi: 10.1016/s0140-6736(95)90167-1. [DOI] [PubMed] [Google Scholar]
- West SK, Munoz B, Lynch M, Kayongoya A, Mmbaga BB, Taylor HR. Risk factors for constant, severe trachoma among preschool children in Kongwa, Tanzania. Am. J. Epidemiol. 1996;143:73–78. doi: 10.1093/oxfordjournals.aje.a008659. [DOI] [PubMed] [Google Scholar]
- WHO . Planning Meeting for the Global Elimination of Trachoma, Geneva, 25—28 November 1996. World Health Organization; Geneva: 1997. WHO/PBL/97.60. [Google Scholar]