Introduction
Prostate cancer disparities have been well documented for African American men, including a 60% higher incidence rate, later stage at diagnosis, and a mortality rate that is more than twice that of Caucasian men (American Cancer Society, 2011). To address these disparities, medical research has focused increasingly on early diagnosis and treatment of prostate cancer among African American men, resulting in increased survival rates (American Cancer Society, 2011). However, little attention has been paid to post-treatment survivorship issues where disparities have been documented. African American men report slower recovery from prostate cancer treatment, more dissatisfaction and regret following prostatectomy (Schrock, Krupski, et al., 2008), more persistent problems with sexual, urinary, and bowel symptoms (Lubeck, Kim, et al., 2001; National Cancer Institute, 2004) and greater emotional distress in response to having cancer compared to Caucasian men (Rodrigue, 1997; Campbell, Keefe, et al., 2004). In spite of the evidence that African American men experience worse long-term physical and emotional outcomes from prostate cancer, research examining psychosocial functioning in African American prostate cancer survivors has been limited (Weber & Sherwill-Navarro, 2005).
One variable that is potentially quite important, but that has not been addressed in prior work with African-American prostate cancer survivors is conformity to majority culture norms on masculinity (often termed “traditional masculinity”). Such norms include emotional control, self-reliance, and social dominance (Mahalik, Locke, et al., 2003; Mahalik, 1999; Richard & Richard, 1995). Men who have been treated for prostate cancer often experience physical symptoms (e.g., sexual or urinary dysfunction; [ Litwin, Hays, et al., 1995; Potosky, Legler, et. al, 2000 ]), and can experience related emotional difficulties (e.g., depression, heightened emotionality; [ Weber & Sherwill-Navarro, 2005 ]) and social changes (e.g., social isolation, concerns about losing intimate relationships) that conflict with these common beliefs about masculinity. As a result, survivors may perceive a diminished sense of manhood which could have a negative impact on their psychosocial functioning.
Previous research suggests that men who conform to more traditional views of masculinity report increased emotional distress, including higher depression and anxiety (Good, Robertson, et. al, 1995). African American prostate cancer survivors may be particularly vulnerable in the face of a threatened sense of manhood since they are caught in a bind between maintaining a strong masculine image consistent with the majority culture as a buffer against racism, powerlessness and socioeconomic disadvantage on the one hand (Mahalik, Pierre, et. al, 2007), and accommodating the realities of their illness on the other. However, researchers are only just beginning to explore how masculinity beliefs impact prostate cancer survivorship.
An earlier study by Burns and Mahalik (2006) reported that, in a sample of 230 men treated for prostate cancer, men with poor physical health who held more strongly to traditional masculinity views about self-reliance and emotional control reported much worse mental health (Burns & Mahalik, 2006). In contrast, men with poor physical health who believed less strongly in traditional masculine norms related to self-reliance and emotional control, reported much better mental health. However, in this study there were only 6 African American men in the sample (3%) which limits the extent to which these findings can be generalized to African American prostate cancer survivors.
Another study of masculine conformity and psychological functioning by Mahalik and colleagues (2007) employed a larger sample of African American men (aged 18-25). The results of this study indicated that greater conformity to traditional masculine norms was associated with lower self-esteem and higher psychological distress (Mahalik, Pierre, et. al, 2007). However, because the participants in this study were young men who were not prostate cancer survivors, the findings may have limited generalizability to middle-aged and older men coping with the physical, emotional and social challenges of prostate cancer survivorship.
This study addresses the gaps in the research literature noted above by examining conformity to traditional masculinity norms related to self-reliance, emotional control and social dominance in a sample of middle-aged and older African-American prostate cancer survivors. Specifically this study examines how variations in masculinity beliefs are related to important indices of psychosocial functioning (symptom distress, self-efficacy for symptom control, negative mood, functional wellbeing and social wellbeing).
Methods
The study was approved by the Institutional Review Board of Duke University Medical Center. All participants underwent the informed consent process and gave written consent prior to participating in this study.
Participants and Eligibility
Participants were African-American prostate cancer survivors who received active treatment (i.e., surgery, radiation, hormone therapy) for localized prostate cancer within the previous 2 years. Eligibility was confirmed by each participants' physician.
Recruitment
An important recruitment aim of this study was to reach an economically diverse population of African American men, including the economically disadvantaged and the medically underserved. To achieve this aim, recruitment was carried out in both clinical settings and through community outreach. Clinic-based recruitment was coordinated through the Duke University Medical Center Prostate Center. Community recruitment involved comprehensive outreach utilizing newspaper and web-based advertising, and community-based prostate cancer advocates serving African American communities. As a result of these outreach efforts 37% of participants were self-referred in response to our outreach efforts. Sixty-three percent of participants were clinic-referred.
Measures
Demographic Information
Demographic data collected included participant age, education, income, prostate cancer treatment modality (e.g., surgery or radiation), and comorbid medical or psychiatric conditions.
Masculine Conformity
Masculine Conformity was assessed using 3 subscales (21 items) of the Conformity to Masculine Norms Inventory (CMNI [Mahalik, Locke, et. al, 2003]) that assess the extent to which an individual desires to conform to masculinity norms related to emotional control, self-reliance, and pursuit of power/dominance. The CMNI has demonstrated validity and reliability (Mahalik, Locke, et. al, 2003). Reliability coefficients (Cronbach's alphas) for CMNI subscales for the current study were .82 for emotional control subscale, .72 for self-reliance subscale, and .56 for dominance subscale. Alpha coefficients are reported similarly for all other study measures described below.
Measusures of Psychosocial Functioning
Symptom Distress was assessed using the Expanded Prostate Cancer Index Composite (EPIC; Wei, Dunn, et al., 2000). The EPIC is a 50-item scale that assesses symptom severity and symptom distress in sexual, urinary, and bowel symptom domains related to prostate cancer treatment. Sexual Bother, Urinary Bother, and Bowel Bother subscales of the EPIC were used to assess Symptom Distress. Higher scores on these scales reflect less symptom distress. Each of these subscales has demonstrated good internal consistency in African American prostate cancer survivors (Campbell, Keefe, et. al, 2004). In the current study, Cronbach alpha coefficients were .78 for the urinary bother subscale, .75 for bowel bother subscale and .72 for sexual bother subscale.
Self-Efficacy for Symptom Control was assessed using a modified version of a standard self-efficacy scale (Lorig, Chastain, et. al, 1989). This 22-item self-efficacy scale has shown good reliability in previous research with African American prostate cancer survivors (Campbell, Keefe, et al, 2004) and includes 3 subscales: symptom management self-efficacy (i.e., confidence in managing cancer-related symptoms), coping-self-efficacy (i.e., confidence in coping with emotional aspects of cancer), and functional self-efficacy (i.e., confidence in one's ability to function in spite of symptoms). In the current study, all three self-efficacy subscales demonstrated excellent reliability. The coefficient alphas were .92 for symptom management self-efficacy, .96 for coping self-efficacy, and .95 for functional self-efficacy.
Negative Mood was assessed using the depression and tension (i.e., anxiety) subscales of the Profile of Mood States-SF (POMS; Lorig, Chastain, et. al, 1989). Higher scores on these POMS-SF subscales indicate more distress. The POMS has been used previously in prostate cancer research (Clarke & Talcott, 2001; Ulrich, Carson, et. al, 2003) and demonstrated good reliability in the current study sample, with alpha coefficients of .82 (Depression subscale) and .74 (Tension subscale).
Functional Wellbeing was measured using the Functional Well-being subscale of the Functional Assessment of Cancer Therapy-General (Fact-G;Cella, Tulsky, et. al, 1993). This subscale includes 7 items that assess survivors' ability to carry out life activities that can be negatively affected by cancer treatment (e.g., work, leisure activities). Evidence supports the reliability of this subscale (Cella, Tulsky, et. al, 1993). In the current study, the functional wellbeing subscale demonstrated good internal consistency with a coefficient alpha of .86.
Social Wellbeing was measured using the 7-item Social/Family Wellbeing subscale of the Functional Assessment of Cancer Therapy-General (Fact-G; Cella, Tulsky, et. al, 1993). This subscale assesses survivors' perceived support from family and friends. In the current study, the alpha coefficient for the social wellbeing subscale was .71.
Statistical Analyses
Descriptive statistics were calculated including means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Correlational analyses were conducted to identify associations between demographic variables and key study variables and among key study variables. Hierarchical multiple regression analyses were then conducted to evaluate how well masculine conformity predicted symptom distress, self-efficacy for symptom control, negative mood, and physical and social functioning, over and above demographic factors. For each regression model, demographic variables found to be significantly correlated with measures of masculine conformity and psychosocial functioning were entered into the model first, followed by masculine conformity indices.
Results
Descriptive Statistics
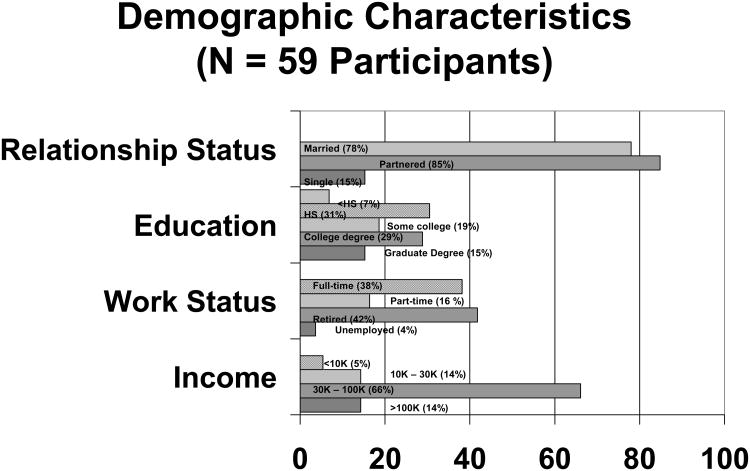
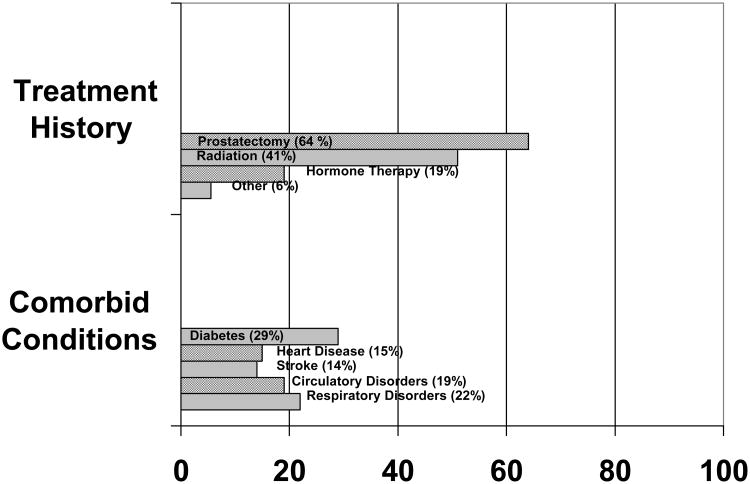
A total of 59 participants completed a baseline questionnaire battery as part of a pilot randomized controlled trial comparing 2 supportive care interventions. The mean age of participants was 61.2 years (SD 8.3). Most participants were married or partnered (85%) and received prostate surgery as their primary form of treatment (64%). Forty-three percent of participants were college graduates, 44% were working full or part-time, and 80% of participants reported middle-income levels or higher. Descriptive statistics for demographic variables are summarized in Table 1. Means, ranges, and standard deviations for masculinity subscales and other psychosocial measures are provided in Table 2.
Table 1. Demographic Characteristics (n = 59 participants).
| M (SD) | |
|---|---|
| Age | 61.2 (8.3) |
| Marital Status | n (%) |
| Partnered | 50 (84.8) |
| Married | 46 (78) |
| Not partnered | 9 (15.3) |
| Education | n (%) |
| < HS | 4 (7) |
| Completed HS | 18 (31) |
| Some college | 11 (19) |
| College degree | 17 (29) |
| Graduate degree | 9 (15) |
| Work Status | n (%) |
| Full time | 21 (38) |
| Part time | 9 (16) |
| Retired | 23 (42) |
| Unemployed | 2 (3.6) |
| Income level | n (%) |
| <10,000 | 3 (5) |
| 10,000 – 30,000 | 8 (14) |
| 30,000 – 100,000 | 37 (66) |
| > 100,000 | 8 (14) |
|
| |
| Treatment History | n(%) |
| Prostatectomy | 38 (64) |
| Ext. Beam Radiation | 23 (39) |
| Brachytherapy | 7 (12) |
| Hormone therapy | 11 (19) |
| Other (e.g., cryotherapy | 3 (6) |
|
| |
| Medical Comorbidities | n(%) |
| Diabetes | 17 (29.) |
| Heart Disease | 9 (15) |
| Stroke | 8 (14.) |
| Circulation | 11(19) |
| Respiratory | 13 (22) |
| Gastrointestinal | 6 (10) |
| Kidney | 4 (7) |
| Seizures | 4 (7) |
| Alcohol Problems | 3 (5) |
| Drug Problems | 1 (2) |
| Major Depression | 4 (7) |
Table 2. Means and Standard Deviations for Self-Efficacy, Masculine Conformity, and QOL Variables.
| Mean (SD) | |
|---|---|
|
| |
| Masculine Conformity | |
| Self-Reliance | 6.84 (2.1) |
| Emotional Control | 15.15 (3.8) |
| Power/Dominance | 4.64 (1.4) |
|
| |
| EPIC Subscales | |
| Sexual Bother | 35.2 (31.4) |
| Urinary Bother | 71.4 (18.6) |
| Bowel Bother | 90.8 (12.5) |
|
| |
| Self-Efficacy Inventory | |
| Symptom Management | 70.4 (23.6) |
| Physical Function | 85.8 (20.6) |
| Coping | 74.2 (20.9) |
| Total | 229.3 (58.4) |
|
| |
| POMS-SF Subscales | |
| Depression | 2.8 (3.1) |
| Tension | 3.5 (2.8) |
|
| |
| FACT-G Subscales | |
| Functional Wellbeing | 20.0 (6.2) |
| Social Wellbeing | 23.0 (4.7) |
Correlational Analyses
Demographic Variables and Key Study Variables
Several significant correlations were observed between demographic and key study variables, however none of the correlations should be interpreted as implying causality. First, older participants reported stronger masculinity beliefs about emotional control, and less urinary symptom distress. Second, participants reporting a higher income level also reported higher functional self-efficacy (r = .52, p < .001) and functional wellbeing (r=.42, p< .01), and lower levels of depression (r = −.36, p < .01). Third, patients with a greater number of medical comorbidities also reported lower symptom management self-efficacy, coping self-efficacy, and functional self-efficacy (r = − .36, −34, and −.43, respectively; all p values < .01), functional wellbeing (r = − .294, p< .001), and more depressed mood (r = .29, p< .05). In sum, of the demographic variables examined, age, income, and medical comorbidities were each related to one or more measures of masculine conformity and psychosocial functioning.
Correlations between Masculine Conformity and Psychosocial Variables
Unadjusted correlations between masculine conformity subscales and psychosocial variables indicated that self-reliance was significantly positively correlated with tension/anxiety scores (r(58) = .32, p < .05), and significantly negatively correlated with social wellbeing (r (59) = −.37, p < .01. Analyses also indicated that dominance was significantly positively correlated with depression scores (r (59) = .39, p < .01) and significantly negatively correlated with coping self-efficacy(r (59) = −.33, p < .05), functional self-efficacy(r (59) = −.30, p < .05), functional wellbeing (r (59) = −.43, p < .01) and social wellbeing (59) = −.49, p < .001). These correlations are presented in Table 3.
Table 3. Masculine Conformity Subscale Correlations with Symptom Distress, Self-Efficacy, Negative Mood, Physical Functioning, and Social Functioning Subscales.
| Self-Reliance | Emotional Control | Dominance | |
|---|---|---|---|
| EPIC Subscales | |||
| Sexual Bother | .15 | .14 | .09 |
| Urinary Bother | -.08 | -.08 | -.22 |
| Bowel Bother | -.08 | -.04 | -.14 |
| Self-Efficacy Subscales | |||
| Management Self-Efficacy | -.09 | -.08 | -.19 |
| Coping Self-Efficacy | -.15 | .01 | -.33* |
| Functional Self-Efficacy | -.08 | .08 | -.30* |
| POMS Subscales | |||
| Tension | .32* | .03 | .19 |
| Depression | .21 | -.05 | .39** |
| Fact-G Subscales | |||
| Functional Wellbeing | -.23 | .01 | -.43** |
| Social Wellbeing | -.37** | -.24 | -.49*** |
p < .05,
p < .01,
p < .001
The low alpha coefficient for the Dominance subscale (.56) identified in this study suggests that, in this sample, this subscale may not be reliably capturing the traditional masculinity norm related to dominance. To explore this further, each of the four items in this subscale was correlated with the psychosocial variables. An adjusted alpha of .005 was used to test for significance (.05/10 subscales). The item “In general, I must get my way” was significantly negatively correlated with physical functioning (r (58) = −.37, p < .005). The item “I should be in charge” was significantly negatively correlated with physical functioning (r (58) = −.41, p < .005, and social wellbeing (r (58) = −.41, p < .005). The item “I make sure people do as I say” was significantly negatively correlated with the functional self-efficacy (r(58) = −.38, p < .005), physical functioning (r (58) = −.37, p < .005, and social wellbeing (r (58) = −.41, p < .005). The item “I'm comfortable trying to get my own way” did not correlate with psychosocial variables when using the adjusted alpha level. To promote comparability across other studies using this subscale, we did retain the full Dominance subscale in the analyses but associations between this scale and other study variables are interpreted with caution.
Regression Analyses
Hierarchical multiple regression analyses were conducted to examine the unique contribution of masculine conformity beliefs to symptom distress, self-efficacy for symptom control, negative mood, functional wellbeing and social wellbeing, controlling for age, income and medical comorbidities (See Table 4).
Table 4.
Regression Results Predicting Negative Mood, Functional Wellbeing and Social Wellbeing
| B | ß | F | |
|---|---|---|---|
| Tension | 3.56* | ||
| Masculine Conformity | |||
| Self-Reliance | .697 | .514** | |
| Emotional Control | |||
| Dominance | |||
| Depression | |||
| Masculine Conformity | 5.11** | ||
| Self-Reliance | .534 | .213* | |
| Emotional Control | -.341 | -.402* | |
| Dominance | .668 | .265* | |
| Functional Wellbeing | |||
| Masculine Conformity | 4.43** | ||
| Self-Reliance | -1.01 | -.326* | |
| Emotional Control | .578 | .351* | |
| Dominance | -1.26 | -.280* | |
| Social Wellbeing | |||
| Masculine Conformity | 5.25** | ||
| Self-Reliance | |||
| Emotional Control | |||
| Dominance | -1.22 | -.371** |
p < .05,
p < .01
Symptom Distress and Self-Efficacy for Symptom Control
The results of the regression analyses indicated that, after controlling for age, masculine conformity was not a significant predictor of symptom distress. Similarly, after controlling for age, income and number of comorbid medical conditions, masculine conformity also did not account for a significant proportion of the variance in self-efficacy for symptom control.
Negative Mood
Masculine conformity accounted for 18% of the variance in POMS depression scores R2 change = .18, F (3,48) = 5.1, p <.01, controlling for age, income and medical comorbidities. Self-reliance and dominance were significant positive predictors of depressed mood, indicating that men who more strongly endorsed traditional masculinity beliefs related to self-reliance and dominance also reported more depressed mood. In contrast, emotional control was a significant negative predictor of depressed mood, indicating that men who more strongly endorsed traditional masculinity beliefs related to emotional control also reported less depressed mood.
Masculine conformity also accounted for 17% of the variance in POMS tension scores R2 change = .17, F (3,54) = 3.70, p <.05, after controlling for age. Of the masculine conformity indices, self-reliance was a significant positive predictor of tension, such that men reporting a greater need for self-reliance also reported higher levels of tension.
Functional Wellbeing
Masculine conformity accounted for 16% of the variance in functional wellbeing after controlling for age, income and medical comorbidities, R2 change = .16, F (3,48) = 4.43, p <.01. In this model, self-reliance and dominance were significant negative predictors of functional wellbeing, indicating that men who more strongly endorsed traditional masculinity beliefs related to self-reliance and dominance also reported lower functional well being. In contrast, emotional control was a significant positive predictor of functional wellbeing, indicating that men who more strongly endorsed traditional masculinity beliefs related to emotional control also reported better functional wellbeing.
Social Wellbeing
Masculinity beliefs also accounted for 27% of the variance in social functioning, R2 change = .27, F (3,53) = 5.25, p <.01, after controlling for age. Of the masculine conformity indices, dominance was a statistically significant negative predictor of social wellbeing, indicating that men endorsing more traditional views of dominance also reported lower quality of life related to social relationships.
Discussion
This study is among the first to examine masculine conformity variables as predictors of psychosocial functioning in a sample of African American prostate cancer survivors. When findings of the current study are compared with the previous examination of masculine conformity in a predominantly Caucasian sample of prostate cancer survivors (Burns & Mahalik, 2006) both similarities and differences are observed. Like the previous study, the current study found that men who believed more strongly in traditional masculine views about self-reliance reported less favorable mental health (i.e., depressed mood and tension). However, unlike the previous study, stronger traditional views about emotional control, were associated with less depressed mood and better functional wellbeing. One explanation for these seemingly different findings could be related to cultural and generational differences in how emotional control is expressed. For example, in middle-aged and older African American men, desire for emotional control could lead to denial of sad feelings when asked about such feelings on a self-report measure. Another explanation might be that desire for emotional control stimulates active coping in African American men, leading them to “do” more to distract or distance themselves from the emotional impact of their disease. Staying active may ultimately convey benefits in the form of maintaining functional wellbeing. However, the extent to which the current study findings reflect cultural differences in enactment of traditional masculinity remains to be examined in future research. Both qualitative and quantitative research with sufficient representation of both African American and Caucasian men are needed to increase our understanding of how socialization and culture influence emotional adjustment and other aspects of quality of life in prostate cancer survivors.
There are study limitations that should be noted. While the sample size of 59 African American prostate cancer survivors outnumbers African American representation in most prostate cancer research, the sample is still relatively small. While care was taken to maximize the diversity of the sample with regard to demographic characteristics, a sample of this size may not be representative of the larger population of African American men. Indeed it should be noted that the educational attainment of the sample (43% college graduates) is greater than the 2010 estimates of educational attainment among African American men aged 25 or older (17.9% college graduates; Current Population Survey [U.S. Department of Commerce, 2010]). Also, the sample size may not have been sufficient to achieve sufficient power for all analyses. Another limitation was the low internal reliability of the dominance subscale. While this variable was found to predict psychosocial functioning and 3 of 4 items in the subscale were correlated with psychosocial variables in exploratory analyses, the relatively weaker internal reliability of the dominance subscale suggests the need to interpret findings related to this predictor variable with caution.
Despite the limitations noted above, the findings reported here could have important implications for development of effective supportive care interventions for African American prostate cancer survivors. Importantly, only a subset of interventions to improve quality of life in prostate cancer survivors have demonstrated substantial benefit (Chambers, Pinnock, et. al, 2011). Furthermore, intervention studies have not included significant numbers of African American men or focused on masculinity issues beyond sexual functioning (Chambers, Pinnock, et. al, 2011; Penedo, Traeger, et. al, 2007; Molton, Siegal, et. al, 2008). Therefore, there is little in the psychosocial intervention literature that addresses cultural factors that may shape how masculinity beliefs are enacted by African American prostate cancer survivors and what therapeutic strategies could be effective for promoting adjustment.
The findings reported here, while preliminary, suggest that masculinity beliefs related to self-reliance could be an important therapeutic target for cognitive-behavioral interventions. To the extent that perceived dependence on others is interpreted as diminished masculinity, survivors may avoid asking for needed help and be left alone to deal with the gap between life demands and current capacity to meet those demands. Such men could be at increased risk for anxiety as our findings linking self-reliance and tension/anxiety suggest. Similarly, when dominance or power figure heavily into one's concept of masculinity, the prostate cancer experience can present challenges (e.g., cutting back or early retirement from a job that allows demonstration of mastery). Perceived loss of power in public arenas could lead to efforts to preserve ones sense of masculinity by exerting more control within the private arena of the home or within close social networks (Charmaz, 1995). Based on clinical observations, the result of such efforts at exerting control is often diminished social relationships and greater psychological distress, which is also consistent with our study findings linking dominance beliefs to social functioning and depressed mood.
Masculinity theorists are calling increasingly for psychosocial interventions that address masculinity issues (Mahalik, Talmadge, et. al, 2005; Good, Thomson, et. al, 2005) not with the goal of pathologizing manhood, but to help men improve their lives in those areas that they value most (Fischer & Good, 1997). In future studies, cognitive-behavioral techniques may be useful for helping African American prostate cancer survivors and men from other cultural groups to identify important masculinity beliefs and enact these beliefs in ways that are culturally congruent and promote psychosocial adjustment to cancer survivorship.
Figure 1. Demographic Characteristics.
Figure 2. Treatment History and Medical Comorbidities.
References
- American Cancer Society. Cancer facts and figures for African Americans 2011-2012. Atlanta: American Cancer Society; 2011. [Google Scholar]
- Burns SM, Mahalik JR. Physical health, self-reliance, and emotional control as moderators of the relationship between locus of control and mental health among men treatment for prostate cancer. Journal of Behavioral Medicine. 2006;29:561–572. doi: 10.1007/s10865-006-9076-1. [DOI] [PubMed] [Google Scholar]
- Campbell LC, Keefe FJ, McKee DC, Edwards CL, Herman SH, Johnson LE, et al. Prostate cancer in African Americans: Relationship of patient and partner self-efficacy to quality of life. Journal of Pain and Symptom Management. 2004;28:433–444. doi: 10.1016/j.jpainsymman.2004.02.020. [DOI] [PubMed] [Google Scholar]
- Cella D, Tulsky D, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: Development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Chambers SK, Pinnock C, Lepore SJ, Hughes S, O'Connell DL. A systematic review of psychosocial interventions for men with prostate cancer and their partners. Patient Education and Counseling. 2011;85:e75–e88. doi: 10.1016/j.pec.2011.01.027. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Identity dilemmas in chronically ill men. In: Sabo D, Gordon DF, editors. Men's health and illness: Gender, power and the body (266-291) Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- Clarke JA, Talcott JA. Symptom indexes to assess outcomes of treatment for early prostate cancer. Medical Care. 2001;39:1118–1130. doi: 10.1097/00005650-200110000-00009. [DOI] [PubMed] [Google Scholar]
- Courneyer RJ, Mahalik JR. Cross-sectional study of gender role conflict examining college-age and middle-aged men. Journal of Counseling Psychology. 1995;42:11–19. [Google Scholar]
- Fischer AR, Good GE. Men and psychotherapy: An investigation of alexithymia, intimacy, and masculine gender roles. Psychotherapy: Theory, Research, Practice, Training. 1997;34:160–170. [Google Scholar]
- Good GE, Robertson JM, O'Neil JM, Fitzgerald LF, Stevens M, DeBord KA, et al. Male gender role conflict: Psychometric issues and relations to psychological distress. Counseling Psychology. 1995;42:3–10. [Google Scholar]
- Good GE, Thomson DA, Braithwaite AD. Men and therapy: Critical concepts, theoretical frameworks, and research recommendations. Journal of Clinical Psychology. 2005;61:699–711. doi: 10.1002/jclp.20104. [DOI] [PubMed] [Google Scholar]
- Lazur RF, Majors R. A new psychology of men. New York City: Basic Books Inc; 1995. Men of Color: Ethnocultural Variations of Male Gender Role Strain. [Google Scholar]
- Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Leach GE, et al. Quality of life outcomes in men treated for localized prostate cancer. JAMA. 1995;273:129–135. doi: 10.1001/jama.273.2.129. [DOI] [PubMed] [Google Scholar]
- Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis and Rheumatism. 1989;32:37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- Lorr M, McNair D. Profile of Mood States. San Diego: Educational and Industrial Testing Service; 1982. [Google Scholar]
- Lubeck DP, Kim H, Grossfeld G, Ray P, Penson DF, Flanders SC, et al. Health related quality of life differences between black and white men with prostate cancer: Data from the cancer of the prostate strategic urology research endeavor. Journal of Urology. 2001;166:2281–2285. [PubMed] [Google Scholar]
- Mahalik JR. Incorporating a gender role strain perspective in assessing and treating men's cognitive distortions. Professional Psychology Research and Practice. 1999;30:333–340. [Google Scholar]
- Mahalik JR, Talmadge WT, Locke BD, Scott RPJ. Using the conformity to masculine norms inventory to work with men in a clinical setting. Journal of Clinical Psychology. 2005;61:661–674. doi: 10.1002/jclp.20101. [DOI] [PubMed] [Google Scholar]
- Mahalik JR, Locke BD, Ludlow LH, Diemer MA, Scott RPJ, Gottfried M, et al. Development of the conformity to masculine norms inventory. Psychology of Men & Masculinity. 2003;4:3–25. [Google Scholar]
- Mahalik JR, Pierre MR, Wan SC. Examining racial identity and masculinity as correlates of self-esteem and psychological distress in Black men. Journal of Multicultural Counseling and Development. 2007;34:94–104. [Google Scholar]
- Molton IR, Siegel D, Penedo FJ, Dahn JR, Kinsinger D, Traeger LN, et al. Promoting recovery of sexual functioning after radical prostatectomy with group-based stress management: The role of interpersonal sensitivity. Journal of Psychosomatic Research. 2008;64:527–536. doi: 10.1016/j.jpsychores.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prostate Cancer Progress Report: Addressing the recommendations of the Prostate Cancer Progress Review Group. National Cancer Institute; Washington DC: Department of Health and Human Services, National Institutes of Health; 2004. [Google Scholar]
- Penedo FJ, Traeger L, Dahn J, Molton I, Gonzalez JS, Schneiderman N, et al. Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual Hispanic men treated for localized prostate cancer: Results of a randomized controlled trial. International Journal of Behavioral Medicine. 2007;14:164–172. doi: 10.1007/BF03000188. [DOI] [PubMed] [Google Scholar]
- Potosky AL, Legler J, Albertsen PC, Stanford JL, Gilliland FD, Hamilton AS, et al. Health outcomes after prostatectomy or radiotherapy for prostate cancer: Results from the Prostate Cancer Outcomes Study. Journal of the National Cancer Institute. 2000;93:401–402. doi: 10.1093/jnci/92.19.1582. [DOI] [PubMed] [Google Scholar]
- Rodrigue JR. An examination of race differences in patients' psychological adjustment to cancer. Journal of Clinical Psychology in Medical Settings. 1997;4:271–280. [Google Scholar]
- Schroek F, Krupski TL, Sun L, Albala DM, Price MM, Polascik TJ, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. European Journal of Urology. 2008;54:785–93. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- Ulrich PM, Carson MR, Lutgendorf SK, Williams RD. Cancer fear and mood disturbance after radical prostatectomy: Consequences of biochemical evidence of recurrence. Journal of Urology. 2003;169:1449–1452. doi: 10.1097/01.ju.0000053243.87457.60. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Commerce Census Bureau. Current Population Survey (CPS), March 1970 through March 2010. Washington DC: 2010. [Google Scholar]
- Weber BA, Sherwill-Navarro P. Psychosocial consequences of prostate cancer: 30 years of research. Geriatric Nursing. 2005;26:166–175. doi: 10.1016/j.gerinurse.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]