Abstract
Study Objectives:
Obstructive sleep apnea syndrome (OSAS) is associated with impairment of cognitive function, and improvement is often noted with treatment. Golf is a sport that requires a range of cognitive skills. We evaluated the impact of nasal positive airway pressure (PAP) therapy on the handicap index (HI) of golfers with OSAS.
Methods:
Golfers underwent a nocturnal polysomnogram (NPSG) to determine whether they had significant OSAS (respiratory disturbance index > 15). Twelve subjects with a positive NPSG were treated with PAP. HI, an Epworth Sleepiness Scale (ESS), and sleep questionnaire (SQ) were submitted upon study entry. After 20 rounds of golf on PAP treatment, the HI was recalculated, and the questionnaires were repeated. A matched control group composed of non-OSAS subjects was studied to assess the impact of the study construct on HI, ESS, and SQ. Statistical comparisons between pre- and post-PAP treatment were calculated.
Results:
The control subjects demonstrated no significant change in HI, ESS, or SQ during this study, while the OSAS group demonstrated a significant drop in average HI (11.3%, p = 0.01), ESS, (p = 0.01), and SQ (p = 0.003). Among the more skilled golfers (defined as HI ≤ 12), the average HI dropped by an even greater degree (31.5%). Average utilization of PAP was 91.4% based on data card reporting.
Conclusions:
Treatment of OSAS with PAP enhanced performance in golfers with this condition. Treatment adherence was unusually high in this study. Non-medical performance improvement may be a strong motivator for selected subjects with OSAS to seek treatment and maximize adherence.
Commentary:
A commentary on this article appears in this issue on page 1243.
Citation:
Benton ML; Friedman NS. Treatment of obstructive sleep apnea syndrome with nasal positive airway pressure improves golf performance. J Clin Sleep Med 2013;9(12):1237-1242.
Keywords: Golf, golf handicap, obstructive sleep apnea, nasal positive airway pressure
Obstructive sleep apnea syndrome (OSAS) is characterized by repeated episodes of airway obstruction during sleep, often leading to symptoms such as daytime sleepiness. The severity of this condition is typically determined by factors that include the frequency of the respiratory disturbances (respiratory disturbance index, or RDI, which is comprised of the average number of apneas, hypopneas, and respiratory event-related arousals per hour of sleep), often associated oxygen desaturation, and overall negative impact on restorative sleep and sleep continuity. Optimum treatment of moderate to severe OSAS (RDI > 15) usually incorporates nasal positive airway pressure (PAP).1
OSAS is a risk factor for hypertension, cardiac disease, stroke, and death.1–3 It also has negative effects on neurocognitive performance, including memory, concentration, and executive function.1,4–8 Regular use of PAP reduces the frequency of respiratory disturbances and hypoxemia, and improves overall sleep quality.9 PAP compliance is typically defined as a minimum of 4 hours of use per night for at least 70% of the nights,9–11 although some studies indicate that the use of PAP for 6 or more hours per night may be more clearly associated with improvement in sleepiness, daily functioning, and memory.12 PAP devices commonly incorporate software that measures and records adherence data such as the number of days and duration that the PAP device is used as well as its efficacy, allowing for more accurate assessment of success with treatment. The impact of treatment on daytime sleepiness can be assessed with the Epworth Sleepiness Scale (ESS), a validated questionnaire that can be administered before and after starting PAP therapy to measure changes in daytime sleepiness.13
BRIEF SUMMARY
Current Knowledge/Study Rationale: OSAS is an extraordinarily prevalent medical condition, and there is strong evidence that successful treatment with CPAP positively impacts quality-of-life and many associated morbidities. Achieving high rates of treatment adherence remains challenging, and we felt that investigating the impact that CPAP had on a real-life outcome that has not previously been assessed, golf performance, could offer a unique insight into the potential benefits of therapy.
Study Impact: Demonstrating that CPAP treatment improves golf performance may serve as a motivator for selected patients to seek and accept therapy for OSAS when they might otherwise remain untreated. Future studies investigating the beneficial impact that treatment of OSAS and other medical conditions has on day-to-day acitivites may help us in our efforts to reach more patients successfully.
There is conflicting evidence regarding the effect of PAP treatment on the neurocognitive deficits associated with OSAS, ranging from significant benefits to no improvement.14–16 In these studies the severity of OSAS, the degree of cognitive impairment, the optimal length of PAP treatment, and the specific areas of cognitive improvement vary, making meaningful interpretation of the data difficult. The impact of OSAS and its treatment has been extensively investigated with regard to motor vehicle accidents, medical risks, and academic performance in children.2,3,9,17 Surprisingly, a relative paucity of data has been published regarding the impact of this condition on athletic and recreational performance.
Golf is an internationally popular sport in which performance is largely dependent on physical and cognitive factors, including concentration, endurance, decision-making and mood control, along with hand-eye coordination and the athleticism of the participant.18 In this study we used the individual subjects' handicap index (HI) to measure changes in their golf performance. The HI can be used to measure an individual golfer's skill, and it can be used to allow golfers of differing skill levels to compete with each other adjusting for differing skill levels.
In the United States, most avid golfers are adult males, 40-70 years old, which coincides with the population most likely to have OSAS.1,19 The United States Golf Association (USGA) defines an avid golfer as someone who plays 25 or more rounds of golf per year, and most surveys indicate that approximately 80% of avid golfers are male. The aim of this study was to assess the impact of PAP treatment on the neuro-cognitive and motor functions, stratified by their playing ability, of avid amateur golfers with moderate-to-severe OSAS. Given the known benefits of PAP therapy to OSAS patients, we expected all golfers to experience an improvement in their HI over the course of this study.
METHODS
Patient Selection
Patients were considered for candidacy for the treatment group of this study if they played ≥ 20 rounds of golf per year, had undergone an NPSG that demonstrated an RDI > 15, and had never been successfully treated for OSAS. Between April 2007 and August 2008, a total of 24 participants were enrolled for and completed this study: 12 participants were identified with moderately severe or worse OSAS (RDI > 15; Table 1). Twelve subjects who were matched for age and HI (Table 2) were selected as non-OSAS control subjects. All of the control subjects had either undergone an NPSG demonstrating a RDI < 15 or were felt to be at very low risk for OSAS based on a detailed evaluation by a board-certified sleep physician prior to their enrollment in the study. The original study design called for 2 control groups, with one group assessed to be at low risk for OSAS, and another group documented to have OSAS but refusing therapy or non-adherent with PAP treatment. The second control group never materialized, as all OSAS patients enrolled in this study were very compliant with their PAP therapy for the duration of the study. Most participants for this study were recruited directly from a busy sleep practice in a non-randomized fashion, with some individuals responding to flyers sent to local golf clubs and/or a newspaper article that was published during the enrollment period. All services were provided using standard outpatient treatment protocols. Billing for all services and equipment was done through healthcare insurance, and no stipends or other inducements were provided for study participation. The Atlantic Health Institutional Review Board approved this study, and all subjects signed an informed consent form at the time of their entry into this study.
Table 1.
Descriptive statistics for clinical variables among OSAS group (n = 12)
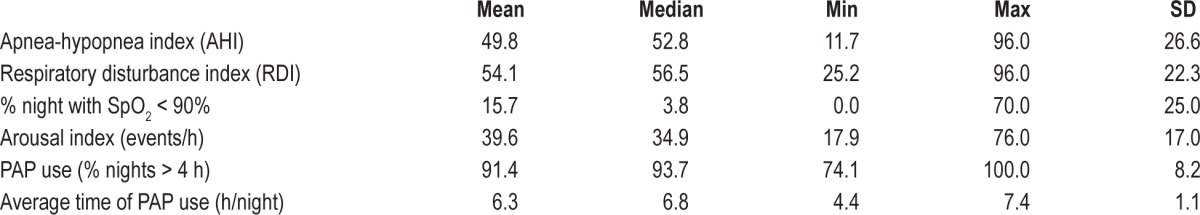
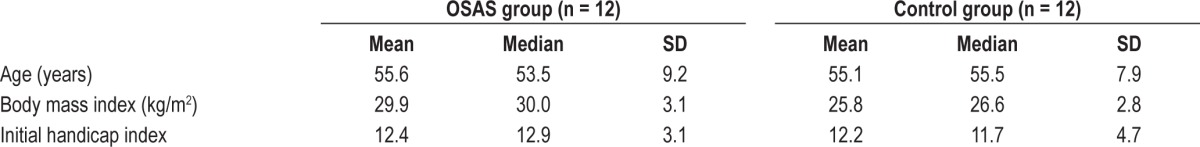
Table 2.
Descriptive statistics for variables in OSAS and control groups
NPSG
Each study consisted of a complete NPSG with a digital sleep system using the international 10-20 electrode placement for recording EEG, EOG, EMG from the chin, ECG, respiratory effort, oximetry, body position, airflow, snoring, and limb movement. During PAP titration studies standard algorithms were utilized to guide changes made in pressure level and modality. Studies were manually scored by a registered sleep technologist and then interpreted by a board-certified sleep physician.
Study Design
After the subjects signed informed consent, all participants were emailed the initial set of questionnaires. These questionnaires contained queries regarding medical and golf demographics, the ESS, a sleep questionnaire (SQ) developed by the authors to assess sleep-related quality-of-life in an online format, a golf questionnaire (GQ) developed by the authors to assess subjective assessment of golf performance, and a golf score template to allow score and other relevant data entry of the first 20 rounds played after treatment initiation. Participants from the OSAS group were titrated onto PAP per Sleep Lab protocol, and received all sleep care under the direct supervision of a board-certified sleep physician. They were seen by the sleep specialist at the time of treatment initiation, 4-6 weeks into treatment, and again 3-6 months afterwards. During each visit subsequent to the initiation of PAP, data card download was acquired when available, and treatment adherence was monitored throughout the duration of their participation in the study. After a total of 20 golf scores were submitted, subjects again completed the ESS, SQ, and GQ.
In order to participate in this study, each individual was required to maintain a handicap with the Golf Handicap and Information Network (GHIN), which is a service of the USGA that calculates and maintains golfer handicaps. The HI is a very complex and specific arithmetic formula that estimates how many strokes above or below par a golfer is likely to score based upon their 10 best scores out of the last 20 rounds that they have played. A number of factors are incorporated into the calculation: the actual number of strokes the golfer reports for each hole of each round that they play, the course rating, the slope rating, and other structured adjustments that are made to player scores that assure that the handicap index reflects playing skill regardless of the actual courses played during each round of golf. The course rating of each course played is a measure of golf course difficulty for scratch golfers, who are skilled golfers likely to score par on each hole played. The slope rating of each course that is played is a measure of difficulty for each golf course for bogey golfers (one more stroke than par per hole) relative to the course rating. Each participant's HI was submitted by them at the time of entry into the study, and it was confirmed at the GHIN website. We utilized templates during the study to collect relevant information from the golfers about each of the 20 rounds that they played, including the dates they played and their scores, along with the slope rating and course rating of each round they played. We used an on-line handicap calculator to determine their HI at the end of their participation in the study, and we then confirmed that the HI was correct by rechecking their HI on the GHIN website after 20 scores had been submitted.
Statistical Analyses
Comparisons between pre- (initial) and post-PAP (final) in terms of total score from SQ, ESS, and HI were made using the paired t-test for normally distributed differences and the nonparametric Wilcoxon signed-rank test for non-normally distributed differences. The same statistical comparisons were analyzed in a subset sample including subjects with HI ≤ 12. A p-value < 0.05 was considered significant.
RESULTS
Subjects
A total of 41 participants, all male, completed consent forms. Of that total, 24 participants met the criteria for participation in the OSAS group, and 12 of them completed both sets of questionnaires and submitted 20 consecutive golf scores. There were 17 subjects who met the criteria for participation in the control group, which included undergoing either an NPSG that did not demonstrate OSAS or a formal assessment by a board-certified sleep physician identifying him as being at very low risk for having OSAS. Twelve of those participants completed both sets of questionnaires and submitted 20 consecutive golf scores. All subjects who dropped out of this study cited the inconvenience of filling out the questionnaires or submitting the scores, or that they were not playing golf frequently enough to meet the 20-score criterion. All subjects completed this study within 6 months or less of enrollment without seasonal breaks. Three of the 12 golfers in the control group and 2 of the 12 golfers in the OSAS group received golf lessons during their participation in this study.
Treatment Outcomes
The 12 control subjects demonstrated no change in HI, ESS, or SQ throughout their participation in this study (Table 3B, 4B, Figure 1). The active treatment group demonstrated a significant drop in average HI (12.4 ± 3.5 to 11.0 ± 4.7; p = 0.01), average ESS (11.8 ± 6.6 to 5.5 ± 3.6; p = 0.01), and average SQ (14.3 ± 7.5 to 3.1 ± 3.1; p = 0.003) (Table 3A, Figure 1). Among the better golfers (HI ≤ 12), the average HI dropped from 9.2 ± 2.9 to 6.3 ± 3.0 (p < 0.001) and the average SQ from 10.8 ± 1.9 to 2.8 ± 2.6 (p = 0.004). The average ESS among these golfers did not drop significantly (Table 4A, Figure 2).
Table 3.
Paired comparison between initial and final total scores from two questionnaires and handicap index in OSAS group (A) and control group (B)
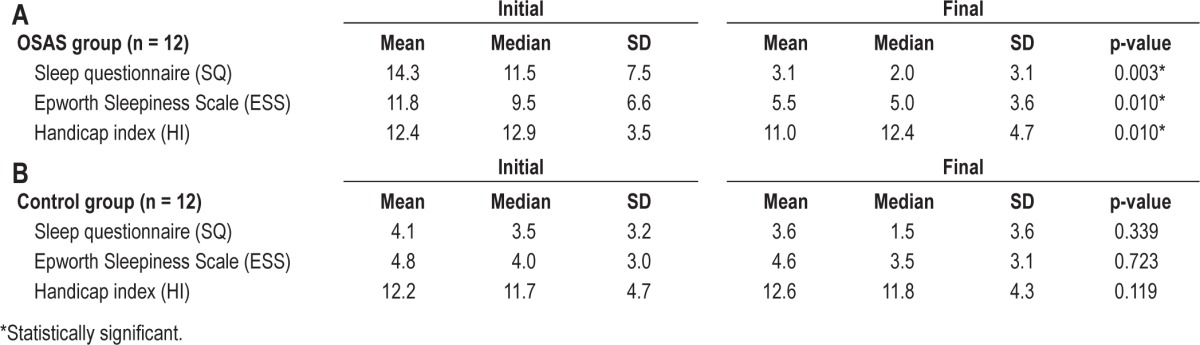
Table 4.
Subjects with handicap index < 12: paired comparison between initial and final total scores from two questionnaires and handicap index in OSAS group (A) and control group (B)
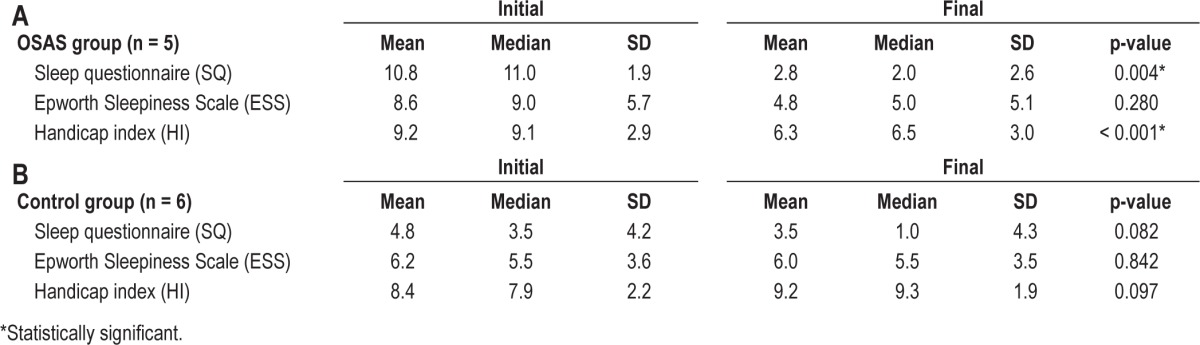
Figure 1. Comparison of initial and final handicap indexes across all subjects.
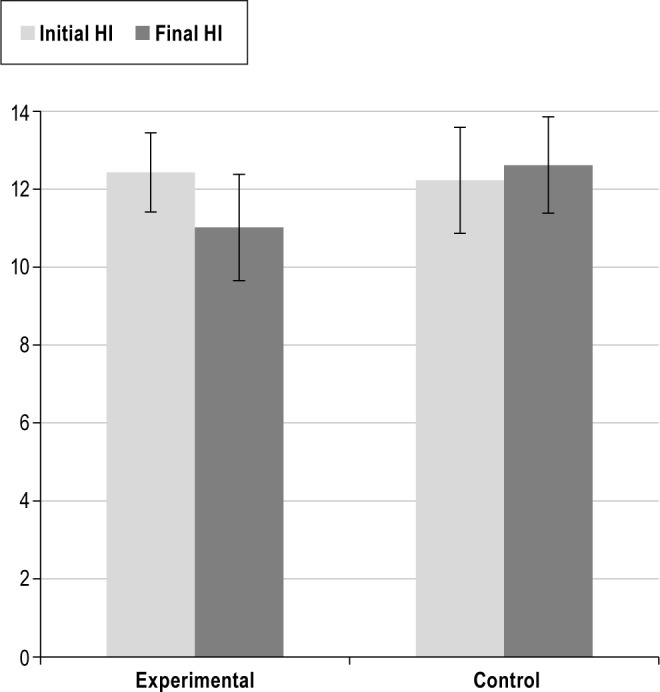
Bars represent handicap indexes as reported by each of the OSAS subjects (n = 12) and control subjects (n = 12). Averages ± standard error are shown.
Figure 2. Comparison of initial and final handicap indexes among skilled golfers.
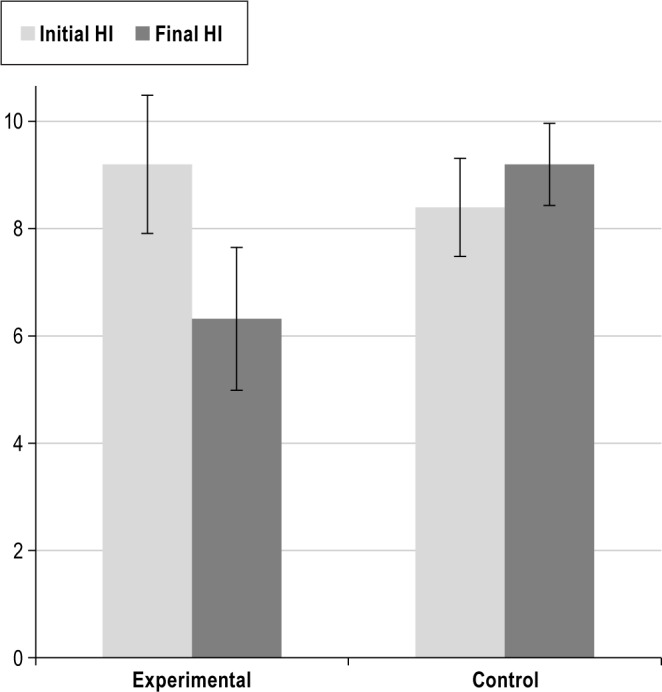
Bars represent handicap indexes as reported by all golfers with an initial handicap index of 12 or less, both in the OSAS group (n = 5) and in the control group (n = 6). Averages ± standard error are shown.
Treatment Adherence
Of the 12 subjects with OSAS, digital compliance reporting was obtained from 9 subjects. The remaining 3 participants had PAP devices that did not include digital compliance software, and they all reported 100% compliance with treatment. However, this data was not included in compliance calculations. Throughout the duration of their participation in the study, the average utilization of PAP was 91.4% of the nights, for an average of 6.3 h per night, as measured by digital compliance reporting (Table 1).
DISCUSSION
Improvements in the ESS and SQ in the OSAS group reconfirm that with successful treatment, patients enjoy substantial reductions in daytime somnolence. The post-treatment questionnaire scores of our subjects with OSAS were similar to those without OSAS (Table 3).
The HI dropped significantly following successful treatment of OSAS (Table 3, Figure 1). The majority of improvement was seen in the better golfers (HI < 12; Table 4, Figure 2), with the average HI dropping 32% during the first 20 rounds played after the initiation of PAP therapy. Many of these golfers were in their late 50s and early 60s, at an age when they would be more likely to experience an increasing HI due to the age-related deterioration of their physical skills. Our findings suggest that better golfers have maximized their golf skills, and that the drop in their HI concurrent with treatment of their OSAS was due to enhanced cognitive functioning. Successful treatment of OSAS, therefore, could lead to improved concentration and endurance, along with better decision making, all of which are likely to improve golf performance and lower the HI. These factors were clearly cited by golfers who participated in this study.
It is estimated that over 80% of Americans with OSAS have not been diagnosed or effectively treated.20 For most patients with significant OSAS, PAP is the most effective modality of treatment.12 Treatment adherence rates with PAP in clinical practice have been measured to range between 40% and 70%.10,11 Clinicians who treat OSAS devote substantial resources to improving patient adherence, often with poor results. These measures include the addition of heated tubing and humidification, flex technology to reduce peak airway pressures, auto-titrating PAP devices, and aggressive management of nasal congestion. The effectiveness of these and other interventions are widely debated throughout the recent sleep literature.21–25 Most of the newer PAP devices incorporate sophisticated compliance and efficacy-reporting software, with detailed reports routinely available at the time of office visits as well as via real-time wireless transmission. Some practitioners have developed and implemented comprehensive compliance-enhancement programs with encouraging results. Unfortunately, these efforts are time-consuming, expensive, and not reimbursed by payers, all of which serves as a disincentive to institute programs of this sort.
Avid golfers often go to great lengths to lower their golf scores, often channeling vast amounts of time, money, and effort into those endeavors.18 Over the last ten years there has been a proliferation of programs available to enhance physical and/or psychological fitness as a means to improve golf performance. Less commonly are those efforts directed in ways that could improve their neurocognitive and motor skills. Identifying and treating OSAS in avid golfers allowed us to measure the impact of treatment on golf performance, which is a real-life outcome that certain patients can relate to.
Treatment adherence was unusually high in our subjects with OSAS despite the absence of specific adherence-enhancement techniques during this study (Table 2). It is possible that the potential for improved golf performance may have served a motivational role in increasing treatment compliance. In a number of cases, the participants in this study had previously refused or failed earlier attempts at treatment with PAP, citing a variety of reasons for their unsuccessful experiences.
Major limitations of this study include the small sample size and the fact that patients were not enrolled in a randomized and blinded fashion. However, the 24 subjects who completed this study comprise a representative sampling of avid golfers (most commonly defined as middle-aged, male, playing 25 or more rounds of golf annually, with handicap indexes ranging between 4.9 and 21.4) in the United States. The Epworth Sleepiness Scale, a validated questionnaire that is commonly used to measure reductions in sleepiness, was used in this study. It has been the experience of the authors that when used to track treatment response to PAP use in OSAS patients, the ESS frequently does not correlate with the clinical assessment of the patient's status. Because of this, we developed a simple 16-question survey (SQ) that can easily be filled out without assistance in an online format, and it contained many of the questions that we routinely ask when assessing response to PAP treatment in our patients. The answers to the SQ correlated with PAP response to a higher degree of statistical significance than the ESS did in this study, particularly in the low HI subjects. We developed a golf questionnaire in an effort to determine if there were specific aspects of playing golf that improved in the OSAS subjects with treatment. No statistically significant findings were observed, but it is possible that a modified version of that questionnaire might yield valuable insight in a larger study. To our knowledge, there are currently no validated questionnaires that investigate the details of playing golf.
The original study design included a second control group which was to consist of subjects with OSAS who either declined treatment with PAP or were found to be non-adherent with therapy during the study period. Due to the small study size and the fact that all of the OSAS subjects exceeded compliance benchmarks, we were unable to include this control group in our data, and this represents another major factor that impacts the interpretation of the data derived from this study. In future studies, it would also make sense to wait one month after PAP therapy has been initiated before assessing the impact of treatment, as many patients need to undergo a period of acclimation and adjustments before the treatment is optimized. Despite these limits, we believe our findings are relevant in the context of OSAS treatment and have strong clinical implications.
Clinical Implications
This pilot study demonstrated a novel positive treatment outcome that some patients may identify as relevant and important as it pertains to the decisions that they make related to their healthcare. The possibility of improving golf performance may have contributed to high rates of adherence with PAP therapy in this study. Non-traditional methods of motivation could prove successful in convincing patients to seek evaluation for and accept treatment of certain medical conditions, in addition to improving treatment adherence. Enhanced performance in sports, hobbies, social, and professional endeavors should be investigated as possible motivators to improve receptiveness to and adherence with treatment.26,27 Golf performance, as defined by the HI, appears to improve in a number of subjects related to treatment of their OSAS. It is possible that other discrete aspects of performance enhancement, particularly in work and social environments, may be realized when OSA is successfully treated. Developing tools to assist in the measurement of performance in these areas may facilitate the efforts of providers to more actively engage some of their patients in the evaluation and treatment process.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. There was no off-label or investigational use. Work Performed at the Morristown Medical Center and Atlantic Sleep & Pulmonary Associates, Madison, NJ.
ACKNOWLEDGMENTS
Author Contributions: Dr. Benton had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Benton contributed to the original idea for the study, subject recruitment, data collection and analysis, manuscript draft and editing. Mr. Friedman contributed to the original idea for the study, data collection and analysis, manuscript draft and editing.
The authors are indebted to Laura Benton and Alison Kole for their help in editing the manuscript, along with Sherin Ibrahim for her contributions to study design. We also thank Rami Bustami for his assistance in statistical analysis, along with Mark Rosen and Christopher Ritchlin for their critical review of the manuscript.
REFERENCES
- 1.Qureshi A, Ballard RD, Nelson HS. Obstructive sleep apnea. J Allergy Clin Immunol. 2003;112:643–51. doi: 10.1016/j.jaci.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 2.Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea. Sleep. 2010;33:1373–80. doi: 10.1093/sleep/33.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 4.Knoepke C, Aloia M. Proposed mechanisms of cognitive dysfunction in obstructive sleep apnea. Prim Psychiatry. 2009;16:51–6. [Google Scholar]
- 5.Lau EYY, Eskes GA, Morrison DL, et al. Executive function in patients with obstructive sleep apnea treated with continuous positive airway pressure. J Int Neuropsychol Soc. 2010;16:1077–88. doi: 10.1017/S1355617710000901. [DOI] [PubMed] [Google Scholar]
- 6.Saunamäki T, Jehkonen M, Huupponen E, Polo O, Himanen S. Visual dysfunction and computational sleep depth changes in obstructive sleep apnea syndrome. Clin EEG Neurosci. 2009;40:162–7. doi: 10.1177/155005940904000308. [DOI] [PubMed] [Google Scholar]
- 7.Saunamäki T, Himanen SL, Polo O, et al. Executive dysfunction in patients with obstructive sleep apnea syndrome. Eur Neurol. 2009;62:237–42. doi: 10.1159/000232156. [DOI] [PubMed] [Google Scholar]
- 8.Twigg GL, Papaioannou I, Jackson M, et al. Obstructive sleep apnea syndrome is associated with deficits in verbal but not visual memory. Am J Respir Crit Care Med. 2010;182:98–103. doi: 10.1164/rccm.200901-0065OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avlonitou E, Kapsimalis F, Varouchakis G, et al. Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients. Sleep Breath. 2011:1–7. doi: 10.1007/s11325-011-0543-8. [DOI] [PubMed] [Google Scholar]
- 10.Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30:635–40. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]
- 11.Weaver T, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711–9. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weaver T, Grunstein R. Adherence to continuous positive airway pressure therapy. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johns M. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Sleep. 1993;103:30–6. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 14.Antic N, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34:111–9. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quan S, Chan CS, Dement WC, et al. The association between obstructive sleep apnea and neurocognitive performance—the Apnea Positive Pressure Long-term Efficacy Study (APPLES) Sleep. 2011;34:303–14. doi: 10.1093/sleep/34.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quan SF, Wright R, Baldwin CM, et al. Obstructive sleep apnea-hypopnea and neurocognitive functioning in the Sleep Heart Health Study. Sleep Med. 2006;7:498–507. doi: 10.1016/j.sleep.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Vertes R, Siegel JM. Time for the sleep community to take a critical look at the purported role of sleep in memory processing. Sleep. 2005;28:1228–9. doi: 10.1093/sleep/28.10.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hellström J. Psychological hallmarks of skilled golfers. Sports Med. 2009;39:845–55. doi: 10.2165/11317760-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Heerwagen P. Golfer demographics show lots of green. Quad - State Business Journal. 1997;8:9. [Google Scholar]
- 20.Lee W, Nagubadi S, Kryger MH, et al. Epidemiology of obstructive sleep apnea: a population-based perspective. Expert Rev Respir Med. 2008;2:349–64. doi: 10.1586/17476348.2.3.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryan S, Doherty LS, Nolan GM, McNicholas WT. Effects of heated humidification and topical steroids on compliance, nasal symptoms, and quality of life in patients with obstructive sleep apnea syndrome using nasal continuous positive airway pressure. J Clin Sleep Med. 2009;5:422–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Worsnop CJ, Miseski S, Rochford PD. Routine use of humidification with nasal continuous positive airway pressure. Intern Med J. 2010;40:650–6. doi: 10.1111/j.1445-5994.2009.01969.x. [DOI] [PubMed] [Google Scholar]
- 23.Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2009:CD007736. doi: 10.1002/14651858.CD007736. [DOI] [PubMed] [Google Scholar]
- 24.Sparrow D, Aloia M, DeMolles DA, et al. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax. 2010;65:1061–6. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]
- 25.Vennelle M, White S, Riha RL, et al. Randomized controlled trial of variable-pressure versus fixed-pressure continuous positive airway pressure (CPAP) treatment for patients with obstructive sleep apnea/hypopnea syndrome (OSAHS) Sleep. 2010;33:267–71. doi: 10.1093/sleep/33.2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taskin U, Yigit O, Acioglu E, et al. Erectile dysfunction in severe sleep apnea patients and response to CPAP. Int J Impot Res. 2010;22:134–9. doi: 10.1038/ijir.2009.54. [DOI] [PubMed] [Google Scholar]
- 27.Emsellem HA, Murtagh KE. Sleep apnea and sports performance. Clinics Sports Med. 2005;24:329–41. doi: 10.1016/j.csm.2005.01.002. [DOI] [PubMed] [Google Scholar]


