Abstract
Sleep disturbances in the general population are associated with elevated blood pressure. This may be due to several mechanisms, including sympathetic activation and hypothalamic-pituitary-adrenal (HPA) axis disturbance. Elevated blood pressure in pregnancy can have devastating effects on both maternal and fetal health and is associated with increased risk for preeclampsia and poor delivery outcomes. Preliminary evidence suggests that mechanisms linking sleep and blood pressure in the general population may also hold in the pregnant population. However, the effects of disturbed sleep on physiologic mechanisms that may directly influence blood pressure in pregnancy have not been well studied. The role that sleep disturbance plays in gestational blood pressure elevation and its subsequent consequences warrant further investigation. This review evaluates the current literature on sleep disturbance and elevated blood pressure in pregnancy and proposes possible treatment interventions.
Citation:
Haney A; Buysse DJ; Okun M. Sleep and pregnancy-induced hypertension: a possible target for intervention? J Clin Sleep Med 2013;9(12):1349-1356.
Keywords: Sleep disturbance, blood pressure, pregnancy, hypertension, weight
The association between sleep disturbances and elevated blood pressure has been extensively studied in the general population. However, relatively few studies have investigated this relationship in the pregnant population. Pregnancy predisposes women to a variety of sleep disturbances.1,2 Similar to non-pregnant individuals, sleep disturbance in pregnancy may be a risk factor for elevated blood pressure, which can lead to maternal and fetal morbidity.3,4 Gestational hypertension, defined as a blood pressure higher than 140/90 diagnosed after 20 weeks of gestation, is associated with fetal growth restriction and abruptio placentae and can predispose to preeclampsia, as well as cardiovascular disease later in life.1,4–6 There are few studies evaluating the link between sleep and blood pressure during pregnancy. In this paper, we first review the relationship between sleep and blood pressure in non-pregnant adults. We then outline factors that predispose pregnant women to poor sleep. We conclude with a review of the emerging literature on the associations between sleep and blood pressure in pregnancy.
SLEEP AND BLOOD PRESSURE IN THE NON-PREGNANT POPULATION
In the U.S. the average sleep duration has decreased by 1.5-2 h/night, with > 30% of Americans sleeping < 6 h/night.7 This phenomenon and the concurrent increase in hypertension intimated a possible link between sleep duration and blood pressure. Recently, a series of epidemiological papers have noted an association between sleep duration (both short and long) and elevated blood press ure8–11; for example, the Sleep Heart Health Study reported that participants who slept < 5 or ≥ 9 h/night had a greater frequency of hypertension than individuals sleeping 7 to 8 h/ni ght.12 Buxton et al. analyzed the 2004-2005 US National Health Interview Survey data (n = 56,507 observations, adults 18-85 years) and found those with short (< 7 h) and long (> 8 h) sleep were more likely to have elevated blood pressure than those sleeping 7 to 8 h/n ight.13 These studies underscore the potential consequences of obtaining too little or too much sleep.
Similar to sleep duration, sleep quality is commonly evaluated. It can be ascertained directly with subjective methods or inferred from objective measures. Fiorentini et al., for instance, evaluated sleep quality in a cohort of hypertensive and type 2 diabetic participants. They found that poor sleep quality, defined by a Pittsburgh Sleep Quality Index score > 5, was more frequent among those with hyperte nsion.14 Knutson et al. examined the association between sleep quality, measured by actigraphy, and blood pressure in mid-life adults. They found that lower sleep quality, as indicated by sleep duration and sleep maintenance, was associated with higher systolic and diastolic blood pressure levels both cross-sectionally and longitudinally over 5 years.11
Hypertension is commonly thought to occur in mid-life or aging individuals. However, pre-hypertension and hypertension are rapidly rising in adolescents. It is possible that several health behaviors that originate in adolescence, including poor diet, smoking, and poor sleep, may increase the risk for prehypertension and an earlier development of hyper tension.15,16
This phenomenon could partly explain why adverse pregnancy outcomes, such as preeclampsia and gestational diabetes, are increasing despite advances in medical technology. Support for this hypothesis comes from Javaheri et al. who studied the sleep of 238 adolescents using actigraphy. They found that poor quality sleep, defined as sleep efficiency ≤ 85% or short sleep duration (≤ 6.5 h), was associated with elevated blood pressure. Specifically, they found that the odds of prehyper-tension increased 4.5-fold in adolescents who had low sleep efficiency and 2.8-fold for those with short sleep.17 Taken together, these studies support the hypothesis that poor sleep quality, beginning much earlier in life than previously recognized, is associated with increased risk of developing hyper-tension and associated morbidities. They also suggest that early intervention may prove beneficial in reducing adverse health outcomes.15–17
In addition to associations with quantitative aspects of blood pressure, sleep disturbance has been associated with impaired nocturnal blood pressure dipping.18–20 During normal sleep, blood pressure dips by 10% to 20%, in part due to a decrease in sympathetic output.21 A nocturnal blood pressure dip < 10% defines non-dipping. Several studies have shown that reduced blood pressure dipping during sleep is an indicator of cardiovascular disease.22–24 Ohkubo and colleagues, for instance, studied 24-h ambulatory blood pressure in 1,542 Japanese adults > 40 years of age, and followed them for an average 9.2 years. They found that for each 5% deficit in normal nocturnal dipping values, there was an associated 20% greater risk of developing cardiovascular disease.25 This study highlights emerging evidence which indicates that nocturnal blood pressure may be a better predictor for cardiovascular risk than daytime blood pressure readings.26–28 Reduced nocturnal blood pressure dipping can have significant immediate and future cardiovascular implications, including cognitive impairment and cerebrovascular disease.18–20,29,30 Furthermore, since sleep disturbances, such as poor sleep quality, have been associated with blunted nocturnal blood pressure dipping, the clinical importance of assessing sleep as a potential risk factor for cardiovascular disease is substantially strengthened.19,20
Sleep disordered breathing (SDB), also referred to as obstructive sleep apnea (OSA), has a prevalence of up to 15% in the general population, and is even greater in obese (40%) and morbidly obese (70% to 90%) patients.31 It is strongly associated with elevated blood pressure. In OSA, repeated episodes of partial or complete upper airway collapse lead to apneas (cessation of airflow for ≥ 10 sec, usually followed by an electroencephalographically measured arousal) or hypopneas (discernible reduction in airflow for 10 sec associated with an oxyhemoglobin desaturation of 4%). The apnea-hypopnea index (AHI), defined by the number of apneas or hypopneas per hour of sleep, describes disease severity. Mild OSA is defined as AHI of 5 to 15, moderate disease as AHI of 15 to 30, and severe disease as AHI > 30.31 Episodes of apnea or hypopnea can cause hypoxia and result in frequent arousals, and thus sleep fragmentation. Repeated episodes of hypoxia and reoxygenation have also been shown to be associated with endocrine and metabolic disturbance, as well as elevated risk for metabolic syndrome and cardiovascular disease in OSA patients.5,6,32,33 SDB has also been shown to be an independent risk factor for hypertension.34–36 Indeed, treatment of SDB using positive airway pressure is associated with a reduction in incident hypertension and a significant improvement in hypertensive patients.37,38 However, these relationships have not been observed universally.39
PSYCHOSOCIAL CORRELATES OF SLEEP AND ELEVATED BLOOD PRESSURE
In addition to sleep disturbance, several psychosocial factors are recognized correlates of increased blood pressure. These factors may also exacerbate the occurrence and the negative consequences of sleep disturbance in pregnancy, similar to what has been observed in non-pregnant individuals.40,41 Psychosocial stress, including occupational stress, social isolation, marital stress, and low socioeconomic status, have been associated with elevated blood pressure in the non-pregnant population.42–50 The most commonly evaluated, however, is acute psychological stress. It has been postulated that stress and sleep disturbance interact to compound cardiovascular vulnerability.51 A detailed examination of the role of psychosocial factors on sleep and blood pressure is beyond the scope of this review (see reviews20,52,53). Here, we merely highlight the importance of appreciating the complex relationships among these factors that may be particularly relevant during pregnancy.
The mechanisms that link sleep disturbances and elevated blood pressure are complex and involve several pathways. In OSA for example, nocturnal hypoxemia induces oxidative stress, inflammatory responses, and reduction in nitric oxide, which mediates vascular functions including dilatation and anticoagulation and has antioxidant properties.54 Sleep disturbances have also been shown to increase sympathetic tone and hypothalamic-pituitary-adrenal axis function in experimental studies. Spiegel at al. found that experimentally induced short sleep (4 h) is associated with alterations in sympathovagal balance and 24-h salivary cortisol levels when compared to normal sleep (7-8 h).55 Similar findings have been found in other experimental studies.56,57 Sleep quality measures, including sleep latency and non-restorative sleep, have also been linked to metabolic and autonomic changes which have been associated with cardiovascular disease and hypertension.17,58
The relationship among cardiovascular changes, neuroendocrine changes, and sleep disturbance is not as clear. Tochikubo et al. found that in overtime workers, blood pressure, urinary norepinephrine levels, and sympathovagal disturbance (measured by heart rate variability) were higher on days after sleep restriction. However, sympathovagal disturbance was measured the evening after sleep restriction. Hence, this finding could have been due to increased stress due to sleepiness after a work day.59 Additionally, Kato et al. described elevated blood pressure after sleep restriction, although they did not find significant changes in heart rate, forearm vascular resistance, or plasma catecholamines with sleep deprivation.60 These studies show that although blood pressure appears to be directly influenced by sleep restriction, the exact mechanisms remain unclear.
SLEEP DISTURBANCE IN PREGNANCY
Sleep disturbances are distinctly more common in pregnant than in non-pregnant women assessed from the general population. Okun and Coussons-Read examined sleep data collected at 12, 24, and 36 weeks' gestation from 35 pregnant and once from 43 comparable non-pregnant women. As early as 12 weeks, pregnant women reported an increased number of naps, nocturnal awakenings, time spent awake during the night, and poorer sleep quality than non-pregnant women.61 Sleep in the pregnant women progressively worsened, with over 50% of the women meeting sleep criteria for insomnia by the end of pregnancy. Suzuki et al. found that that among 192 pregnant women surveyed retrospectively, 88% had alterations in sleep compared with their usual experience.62 The reported changes included insomnia, parasomnias (nightmares and night terrors), restless leg syndrome (RLS), snoring, and sleep apnea. Among the most frequent self-reported causes of sleep disturbance during pregnancy were urinary frequency, back or hip ache, and heartburn. Facco et al. investigated sleep during pregnancy in a prospective cohort of 189 women assessed at 2 points during pregnancy, with a mean baseline assessment of 13.8 (± 3.8) weeks and a mean second assessment of 30.0 (± 2.2) weeks. At the second assessment, sleep duration significantly decreased compared to baseline (7.4 ± 1.2 h vs. 7.0 ± 1.3), the number of participants who reported snoring increased (11% vs. 16.4%), incidence of restless leg syndrome increased (17.5% vs. 31.2%), and there was an increase of poor sleep quality as measured by Pittsburgh Sleep Quality Index > 5 (39.0% vs. 53.5%).36
In pregnancy, hormonal changes occur to ensure the survival of the fetus. However, these hormonal changes may result in substantial sleep disturbances.1 By the last few weeks of pregnancy, daily estrogen production is one thousand times premenopausal ovulatory levels, and progesterone levels increase from 25 ng/mL at 6 weeks to 150 ng/mL at 37 weeks.64 Estrogen reduces rapid eye movement sleep (REM) and progesterone reduces NREM sleep.1,65,66 Estrogen can also cause physical changes that can affect sleep, including hyperemia, mucosal edema, hypersecretion, and increased friability in the upper airways. These changes result in reduction of nasopharyngeal airway patency, which can cause a sensation of nasal stuffiness and may exacerbate sleep disordered breathing in women with elevated body mass index.67 Progesterone is thought to act via peripheral chemoreceptors and centrally in the medulla to increase respiratory drive.68 This, in conjunction with greater metabolic carbon dioxide production and increased minute ventilation, can cause respiratory alkalosis, which can reduce respiratory drive and predispose to central sleep apnea.1 Furthermore, oxygen consumption is increased by approximately 20% to 33% by the third trimester due to fetal demands and changes in maternal metabolism. Increased oxygen consumption, along with a reduced functional residual capacity due to an enlarging uterus, results in a lowered oxygen reserve and can affect oxygen homeostasis more than in the non-pregnant state.1,69 Table 1 illustrates the major physical and hormonal changes in pregnancy that can affect sleep.
Table 1.
Physical and hormonal changes in pregnancy, subsequent symptoms, and effect on sleep
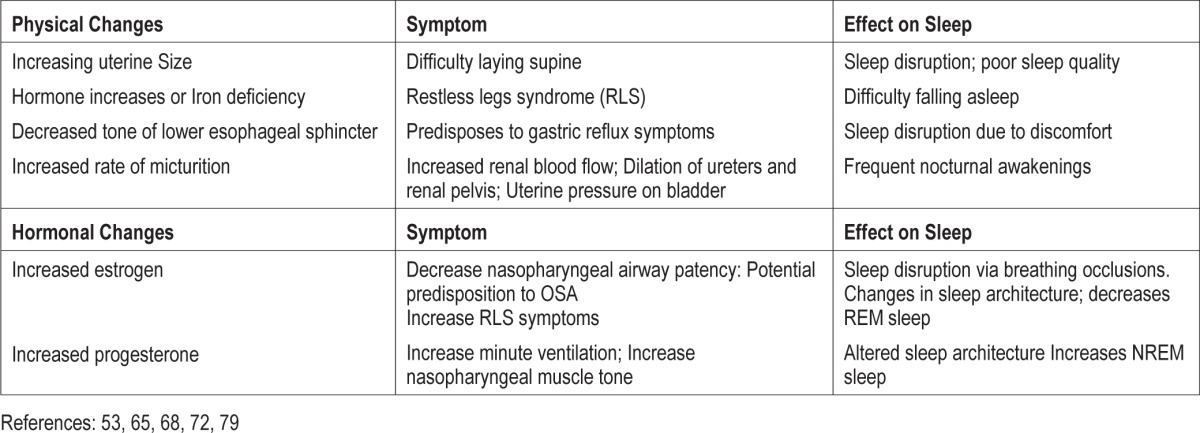
The dramatic physical changes unique to pregnancy can further affect sleep. The enlarging uterus can upwardly displace the diaphragm, further compromising functional residual capacity, which decreases by 10% to 25% at term. This, together with reduction in chest wall and total respiratory compliance, may lead many pregnant women to experience shortness of breath while lying supine. The inability to assume a comfortable sleeping position, especially during the third trimester of pregnancy, may have a significant impact on a pregnant woman's ability to initiate and maintain sleep.36 Discomfort from back and leg cramps may also disrupt sleep. Lower esophageal sphincter tone decreases throughout pregnancy, reaching its lowest point in late pregnancy. Resulting gastroesophageal reflux can cause discomfort and sleep disruptions.70 Additionally, renal blood flow increases in pregnancy throughout first and second trimester, along with dilation of the ureters and renal pelvises. These changes and the pressure of an enlarged uterus on the bladder cause pregnant women to wake several times per night to urinate.36
SLEEP AND HYPERTENSION IN PREGNANCY
Elevated maternal blood pressure during pregnancy poses great risk for both mother and fetus. Approximately 10% of pregnancies are affected by hypertension. Consequences of pregnancy-related hypertension include increased risk of abruptio placentae, disseminated intravascular coagulation, cerebral hemorrhage, hepatic failure, and acute renal failure.5 Furthermore, elevated blood pressure in pregnancy can be part of preeclampsia and eclampsia, which carry maternal mortality rates of 10% to 15%, and future risk for cardiovascular disease.4,71
Systolic and diastolic blood pressure normally fall in early pregnancy by 5-10 mm Hg, reaching a mean nadir of 105/60 mm Hg, and then gradually rise to pre-pregnancy values by term.72 However, emerging evidence indicates that sleep disturbance may disrupt the normal course of gestational blood pressure changes. Williams et al. found that self-reported short (≤ 6 h) and long (≥ 10 h) sleep durations in early pregnancy (mean 14 weeks) were associated with elevated blood pressure, particularly mean third trimester blood pressures, in 1,272 women. Mean third trimester systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial blood pressure (MAP) for women who reported short early pregnancy sleep durations (≤ 6 h) compared to normal sleep duration (9 h) were 3.72, 3.04, and 3.18 mm Hg higher, respectively, after adjustment for maternal age, race/ethnicity, parity, educational status, and pre-pregnancy body mass index. The differences in third trimester SBP, DBP, and MAP for women who reported long sleep durations (≥ 10 h), compared with those reporting sleeping 9 h nightly, were 4.21, 3.43, and 3.65 mm Hg higher, respectively.3 A similar conclusion was reached by Reid and colleagues who reported that women with gestational hypertension has less total sleep time, lower sleep efficiency, and a lower percentage of REM sleep than healthy pregnant women.73 Although the mechanisms behind these differences are not clear, they may be similar to those that link short and long sleep durations with increased BP in the non-pregnant population.
Furthermore, as in the non-pregnant population, psychological stress may play a role in both sleep disturbance and blood pressure elevation.74 Pregnancy can be a mentally taxing time for women, especially in those with concurrent stressful life events or psychosocial stress. Stress may further elevate blood pressure in pregnant women, similar to what has been observed in non-pregnant cohorts.40,41,74 We propose that the hormonal and physical changes, as well as stress of pregnancy, induce sleep disturbance and may result in blood pressure perturbations. Figure 1 illustrates this model.
Figure 1. Proposed model of how physical and hormonal changes in pregnancy coupled with stress result in disturbed sleep which can result in elevated blood pressure.
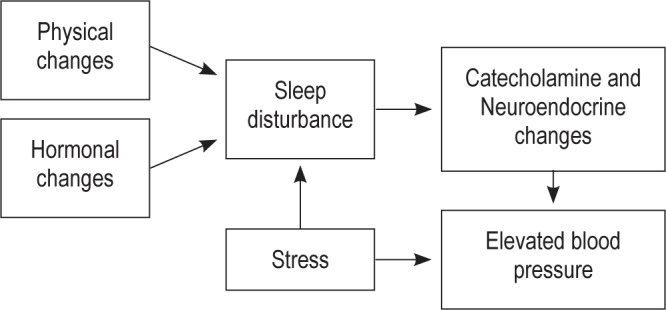
Normative physical changes, such as changes in body habitus, and hormonal changes, including dramatic increases in estrogen and progesterone, are recognized contributors to sleep disturbance in pregnancy. Subsequent to the sleep disturbance are various catecholamine and neuroendocrine changes which can negatively impact blood pressure. Concurrent stress, whether daily hassles or serious life events, is both an independent and dependent modifier of blood pressure. These associations are critical throughout pregnancy as elevated blood pressure is linked with increased risk of preeclampsia and preterm birth.
SLEEP RELATED BREATHING DISORDERS IN PREGNANCY
SDB is characterized by abnormal respiratory patterns (e.g., apneas, hypopneas) or abnormal gas exchange (e.g., hypoxia). Sleep related breathing disorders like snoring and obstructive sleep apnea occur in pregnancy; however, there is little data detailing their incidence or prevalence. Most investigators agree that sleep related breathing disorders are more prevalent in pregnant women than non-pregnant women. As previously noted, estimates in non-pregnant women range from 2% to 5%, whereas estimates in pregnancy range from ∼10% in early pregnancy to upwards of 30% in late pregnancy.67,75–78 There is currently a paucity of objective data on the incidence of sleep related breathing disorders in pregnancy. Our current knowledge relies primarily on self-reported symptoms, including excessive daytime sleepiness, snoring, or breathing cessations, which suggest but do not confirm the presence of OSA. The development of SDB in pregnancy is considered a consequence of necessary physiologic adaptations that occur in pregnancy,79 such as dramatic hormonal and subsequent physical changes. Estrogen, for instance, can cause upper airway narrowing and could predispose pregnant women to snore and develop SDB. Progesterone, on the other hand, increases minute ventilation, and the resulting respiratory alkalosis enhances sensitivity of the respiratory center to carbon dioxide in pregnancy, which may predispose to central sleep apnea.1
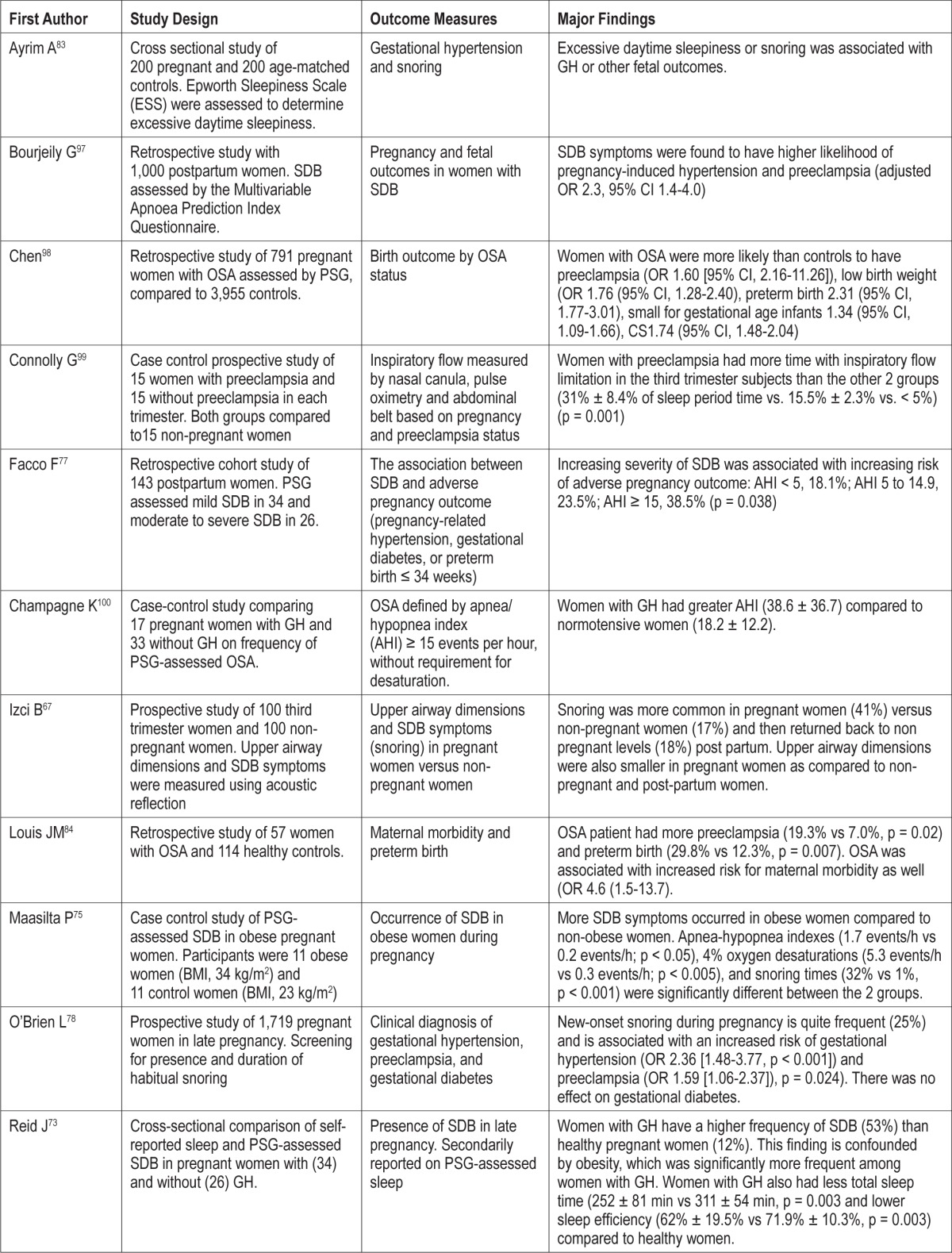
SDB, independent of maternal BMI, is associated with an increased risk of hypertension in pregnancy, as well as maternal morbidity.73,78,80–86 In one study, preeclampsia, a hypertensive syndrome in pregnancy, was significantly more common among snorers than non-snorers (10% versus 4%, p < 0.05), as was gestational hypertension (14% versus 6%, p < 0.01).87 This was recently corroborated in a report by O'Brien and colleagues, who found that pregnancy-onset snoring was independently associated with gestational hypertension (OR 2.36 [1.48-3.77], p < 0.001) and preeclampsia (OR 1.59 [1.06-2.37], p = 0.024) in 1,719 third-trimester pregnant women.78 Another study reported that snoring and “excessive daytime sleepiness,” which could indicate poor sleep, were reported more commonly in later pregnancy in women with preeclampsia than those without preeclampsia or non-pregnant controls.88 In a large cross-sectional study of immediately postpartum women, Perez-Chada et al. reported an increase in gestational hyper-tension and preeclampsia among those with symptoms of SDB even after adjusting for potential confounders such as BMI.89 In a similar study, Bourjeily et al. adjusted for comorbid conditions and reported an increase in preeclampsia and gestational hypertension in women with SDB.90 Table 2 summarizes a series of studies that have examined the frequency and consequences of SDB in pregnancy.
Table 2.
Selected listing of sleep disordered breathing (SDB) in pregnancy studies
SIGNIFICANCE
Hypertensive disorders in pregnancy are prevalent and pose risk to both mother and child. Additionally, they can carry risk for maternal morbidity later in life. Preeclampsia, especially if complicated by HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), predisposes to future cardiovascular disease.31 A meta-analysis by Bellamy et al. found that women who developed gestational hypertension or preeclampsia had an increased risk of developing hypertension later in life. The relative risk of ischemic heart disease, stroke, and venous thromboembolism were also increased later in life in women with prior diagnoses of preeclampsia. Furthermore, Bellamy et al. found that women who developed preeclampsia had greater all-cause mortality risk compared to women who had normal blood pressure during pregnancy. This risk was even greater for women who developed preeclampsia before 37 weeks.71 Kestenbaum et al. also found that gestational hypertension, mild and severe preeclampsia were associated with 2.8-fold higher risk of cardiovascular events, and that severe preeclampsia was associated with 2.3-fold higher risk of thromboembolic events.4 Furthermore, hypertensive disorders in pregnancy are associated with poor fetal outcomes including preterm birth, small for gestational age infants, and abruptio placentae.5 The delayed morbidity risk of hypertensive disorders, as well as the immediate risk to mother and fetus risk, only amplifies the need for better understanding and prevention.
CONCLUSION
Elevated blood pressure in pregnancy can have devastating effects on both maternal and fetal health during the perinatal period and beyond. The causes of hypertensive syndromes in pregnancy like preeclampsia and gestational hypertension appear to be multifactorial. However, numerous studies demonstrate a strong link between sleep duration, quality or sleep related breathing disorders and blood pressure in non-pregnant adults; emerging studies suggest a similar relationship in the pregnant population. This link represents a possible source of preventative measures for gestational hypertension and preeclampsia. However, more complete understanding of the association between sleep and blood pressure in pregnancy is needed. Well-controlled, longitudinal studies with large cohorts and both objective and subjective sleep measurements are needed to better assess sleep in pregnancy and how it relates to blood pressure. These studies should include blood pressure measurements throughout pregnancy, as well as pregnancy outcomes, to assess the effect of sleep on both maternal and fetal health. Currently, screening for sleep disruption in pregnant women is not common practice. More knowledge and widespread understanding of the effects that sleep has on pregnancy may improve upon the obstetrician's ability to screen for those with sleep disruption and who may be at risk for hyper-tensive disorders. Utilization of short questionnaires, such as the Insomnia Symptom Questionnaire (ISQ),91 could be incorporated into prenatal care to assist in the identification of those women at-risk for sleep problems. Emerging data suggests that a modest number of pregnant women have difficulty initiating sleep (DIS).92 Given the associations between DIS and adverse health outcomes,93–95 this may be an appropriate target for intervention. Early identification of at-risk women may allow for simple interventions, including counseling on the impacts of sleep on maternal and fetal health and prescribing behavioral sleep regimens to not only improve sleep but potentially blood pressure as well. While there is currently a paucity of studies that have examined the impact of interventions on sleep in pregnant women, there is some evidence from a study of post-partum mothers that a behavioral-education intervention could be applied in pregnancy.96 In this randomized controlled trial, women received intervention, which consisted of an in-person meeting with a nurse for sleep strategies, a booklet, and phone contacts, or usual care. Although there was no difference in the primary outcome of maternal nocturnal sleep, it is possible that the length of data collection or the measures used in the study were unable to capture the benefits of the intervention. It is probable, for instance, that improving sleep in the early postpartum is not feasible. Assessing the women further post-delivery may indicate otherwise.
DISCLOSURE STATEMENT
This was not an industry supported study. Funded by grants NIH ROO010813 (P.I. Okun) and the NIMH Medical Student Fellowship Program in Mental Health Research through the Department of Psychiatry of the University of Pittsburgh School of Medicine. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Joann Broadus for her assistance with manuscript preparation
REFERENCES
- 1.Sahota PK, Jain SS, Dhand R. Sleep disorders in pregnancy. Curr Opin Pulm Med. 2003;9:477–83. doi: 10.1097/00063198-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Balserak BI, Lee K. Sleep Disturbances and sleep-related disorders in pregnancy. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 5th ed. St. Louis: Elsevier; 2011. pp. 1572–86. [Google Scholar]
- 3.Williams MA, Miller RS, Qiu C, Cripe SM, Gelaye B, Enquobahrie D. Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. Sleep. 2010;33:1363–71. doi: 10.1093/sleep/33.10.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kestenbaum B, Seliger SL, Easterling TR, et al. Cardiovascular and thromboembolic events following hypertensive pregnancy. Am J Kidney Dis. 2003;42:982–9. doi: 10.1016/j.ajkd.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Liu CM, Cheng PJ, Chang SD. Maternal complications and perinatal outcomes associated with gestational hypertension and severe preeclampsia in Taiwanese women. J Formos Med Assoc. 2008;107:129–38. doi: 10.1016/S0929-6646(08)60126-6. [DOI] [PubMed] [Google Scholar]
- 6.Srinivas SK, Edlow AG, Neff PM, Sammel MD, Andrela CM, Elovitz MA. Rethinking IUGR in preeclampsia: dependent or independent of maternal hypertension? J Perinatol. 2009;29:680–4. doi: 10.1038/jp.2009.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luckhaupt SE. Short sleep duration among workers- United States, 2010. 2012 [PubMed] [Google Scholar]
- 8.Cappuccio FP, Stranges S, Kandala NB, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 10.Kim J, Jo I. Age-dependent association between sleep duration and hypertension in the adult Korean population. Am J Hypertens. 2010;23:1286–91. doi: 10.1038/ajh.2010.166. [DOI] [PubMed] [Google Scholar]
- 11.Knutson KL, Van CE, Rathouz PJ, et al. Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009;169:1055–61. doi: 10.1001/archinternmed.2009.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 13.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 14.Fiorentini A, Valente R, Perciaccante A, Tubani L. Sleep's quality disorders in patients with hypertension and type 2 diabetes mellitus. Int J Cardiol. 2007;114:E50–2. doi: 10.1016/j.ijcard.2006.07.213. [DOI] [PubMed] [Google Scholar]
- 15.Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla JR, Schneiderman N. Cardiometabolic risk in adolescents: associations with physical activity, fitness, and sleep. Ann Behav Med. 2013;45:121–31. doi: 10.1007/s12160-012-9428-8. [DOI] [PubMed] [Google Scholar]
- 16.Narang I, Manlhiot C, Davies-Shaw J, et al. Sleep disturbance and cardiovascular risk in adolescents. CMAJ. 2012;184:E913–20. doi: 10.1503/cmaj.111589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118:1034–40. doi: 10.1161/CIRCULATIONAHA.108.766410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sherwood A, Routledge FS, Wohlgemuth WK, Hinderliter AL, Kuhn CM, Blumenthal JA. Blood pressure dipping: ethnicity, sleep quality, and sympathetic nervous system activity. Am J Hypertens. 2011;24:982–8. doi: 10.1038/ajh.2011.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loredo JS, Nelesen R, Ancoli-Israel S, Dimsdale JE. Sleep quality and blood pressure dipping in normal adults. Sleep. 2004;27:1097–103. doi: 10.1093/sleep/27.6.1097. [DOI] [PubMed] [Google Scholar]
- 20.Matthews KA, Kamarck TW, Hall H, et al. Blood pressure dipping and sleep disturbance in African-American and Caucasian men and women. Am J Hypertens. 2008;21:826–31. doi: 10.1038/ajh.2008.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calhoun DA, Harding SM. Sleep and hypertension. Chest. 2010;138:434–43. doi: 10.1378/chest.09-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dolan E, Stanton AV, Thom S, et al. Ambulatory blood pressure monitoring predicts cardiovascular events in treated hypertensive patients--an Anglo-Scandinavian cardiac outcomes trial substudy. J Hypertens. 2009;27:876–85. doi: 10.1097/HJH.0b013e328322cd62. [DOI] [PubMed] [Google Scholar]
- 23.Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7. doi: 10.1161/hy1001.092640. [DOI] [PubMed] [Google Scholar]
- 24.Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–41. doi: 10.1161/HYPERTENSIONAHA.107.087262. [DOI] [PubMed] [Google Scholar]
- 25.Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens. 2000;18:847–54. doi: 10.1097/00004872-200018070-00005. [DOI] [PubMed] [Google Scholar]
- 26.Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61. doi: 10.1161/01.HYP.0000170138.56903.7a. [DOI] [PubMed] [Google Scholar]
- 27.Pedersen OL, Mancia G, Pickering T, et al. Ambulatory blood pressure monitoring after 1 year on valsartan or amlodipine-based treatment: a VALUE substudy. J Hypertens. 2007;25:707–12. doi: 10.1097/HJH.0b013e3280147119. [DOI] [PubMed] [Google Scholar]
- 28.Salles GF, Cardoso CR, Muxfeldt ES. Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med. 2008;168:2340–6. doi: 10.1001/archinte.168.21.2340. [DOI] [PubMed] [Google Scholar]
- 29.Barksdale DJ, Woods-Giscombe C, Logan JG. Stress, cortisol, and nighttime blood pressure dipping in nonhypertensive black American women. Biol Res Nurs. 2013;15:330–7. doi: 10.1177/1099800411433291. [DOI] [PubMed] [Google Scholar]
- 30.Yano Y, Kario K. Nocturnal blood pressure, morning blood pressure surge, and cerebrovascular events. Curr Hypertens Rep. 2012;14:219–27. doi: 10.1007/s11906-012-0261-z. [DOI] [PubMed] [Google Scholar]
- 31.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 32.Punjabi NM, Beamer BA. Alterations in glucose disposal in sleep-disordered breathing. Am J Respir Crit Care Med. 2009;179:235–40. doi: 10.1164/rccm.200809-1392OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu FB, Willett WC, Colditz GA, et al. Prospective study of snoring and risk of hypertension in women. Am J Epidemiol. 1999;150:806–16. doi: 10.1093/oxfordjournals.aje.a010085. [DOI] [PubMed] [Google Scholar]
- 34.Goncalves SC, Martinez D, Gus M, et al. Obstructive sleep apnea and resistant hypertension: a case-control study. Chest. 2007;132:1858–62. doi: 10.1378/chest.07-1170. [DOI] [PubMed] [Google Scholar]
- 35.Logan AG, Perlikowski SM, Mente A, et al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens. 2001;19:2271–7. doi: 10.1097/00004872-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 36.Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115:77–83. doi: 10.1097/AOG.0b013e3181c4f8ec. [DOI] [PubMed] [Google Scholar]
- 37.Bottini P, Taranto-Montemurro L, Novali M, et al. Effects of CPAP on systemic hypertension in OSAH: a monocentric, observational, cohort study. Respir Med. 2012;106:1329–34. doi: 10.1016/j.rmed.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 38.Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169–76. doi: 10.1001/jama.2012.3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kasiakogias A, Tsioufis C, Thomopoulos C, et al. Effects of continuous positive airway pressure on blood pressure in hypertensive patients with obstructive sleep apnea: a 3-year follow-up. J Hypertens. 2013;31:352–60. doi: 10.1097/HJH.0b013e32835bdcda. [DOI] [PubMed] [Google Scholar]
- 40.van Mill JG, Hoogendijk WJ, Vogelzangs N, van DR, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71:239–46. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- 41.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 42.Vrijkotte TG, van Doornen LJ, de Geus EJ. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension. 2000;35:880–6. doi: 10.1161/01.hyp.35.4.880. [DOI] [PubMed] [Google Scholar]
- 43.Steptoe A, Siegrist J, Kirschbaum C, Marmot M. Effort-reward imbalance, overcommitment, and measures of cortisol and blood pressure over the working day. Psychosom Med. 2004;66:323–9. doi: 10.1097/01.psy.0000126198.67070.72. [DOI] [PubMed] [Google Scholar]
- 44.Steptoe A, Marmot M. Psychosocial, hemostatic, and inflammatory correlates of delayed poststress blood pressure recovery. Psychosom Med. 2006;68:531–7. doi: 10.1097/01.psy.0000227751.82103.65. [DOI] [PubMed] [Google Scholar]
- 45.Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- 46.Nealey-Moore JB, Smith TW, Uchino BN, Hawkins MW, Olson-Cerny C. Cardiovascular reactivity during positive and negative marital interactions. J Behav Med. 2007;30:505–19. doi: 10.1007/s10865-007-9124-5. [DOI] [PubMed] [Google Scholar]
- 47.Smith TW, Uchino BN, Berg CA, et al. Conflict and collaboration in middle-aged and older couples: II. Cardiovascular reactivity during marital interaction. Psychol Aging. 2009;24:274–86. doi: 10.1037/a0016067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- 49.Albert MA, Glynn RJ, Buring J, Ridker PM. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation. 2006;114:2619–26. doi: 10.1161/CIRCULATIONAHA.106.660043. [DOI] [PubMed] [Google Scholar]
- 50.Conen D, Glynn RJ, Ridker PM, Buring JE, Albert MA. Socioeconomic status, blood pressure progression, and incident hypertension in a prospective cohort of female health professionals. Eur Heart J. 2009;30:1378–84. doi: 10.1093/eurheartj/ehp072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Franzen PL, Gianaros PJ, Marsland AL, et al. Cardiovascular reactivity to acute psychological stress following sleep deprivation. Psychosom Med. 2011;73:679–82. doi: 10.1097/PSY.0b013e31822ff440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chida Y, Hamer M. Chronic psychosocial factors and acute physiological responses to laboratory-induced stress in healthy populations: a quantitative review of 30 years of investigations. Psychol Bull. 2008;134:829–85. doi: 10.1037/a0013342. [DOI] [PubMed] [Google Scholar]
- 53.Jehn ML. Psychosocial factors and racial differences in blood pressure dipping. Am J Hypertens. 2009;22:584. doi: 10.1038/ajh.2009.73. [DOI] [PubMed] [Google Scholar]
- 54.Peker Y, Hedner J, Norum J, Kraiczi H, Carlson J. Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. Am J Respir Crit Care Med. 2002;166:159–65. doi: 10.1164/rccm.2105124. [DOI] [PubMed] [Google Scholar]
- 55.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 56.Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106:4453–8. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reynolds AC, Dorrian J, Liu PY, et al. Impact of five nights of sleep restriction on glucose metabolism, leptin and testosterone in young adult men. PLoS One. 2012;7:e41218. doi: 10.1371/journal.pone.0041218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep. 2007;30:1667–73. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tochikubo O, Ikeda A, Miyajima E, Ishii M. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension. 1996;27:1318–24. doi: 10.1161/01.hyp.27.6.1318. [DOI] [PubMed] [Google Scholar]
- 60.Kato M, Phillips BG, Sigurdsson G, Narkiewicz K, Pesek CA, Somers VK. Effects of sleep deprivation on neural circulatory control. Hypertension. 2000;35:1173–5. doi: 10.1161/01.hyp.35.5.1173. [DOI] [PubMed] [Google Scholar]
- 61.Okun ML, Coussons-Read ME. Sleep disruption during pregnancy: how does it influence serum cytokines? J Reprod Immunol. 2007;73:158–65. doi: 10.1016/j.jri.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 62.Suzuki S, Dennerstein L, Greenwood KM, Armstrong SM, Satohisa E. Sleeping patterns during pregnancy in Japanese women. J Psychosom Obstet Gynaecol. 1994;15:19–26. doi: 10.3109/01674829409025625. [DOI] [PubMed] [Google Scholar]
- 63.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 64.Challis JRG, Matthews SG, Gibb W, Lye SJ. Endocrine and paracrine regulation of birth at term and preterm. Endocr Rev. 2000;21:514–50. doi: 10.1210/edrv.21.5.0407. [DOI] [PubMed] [Google Scholar]
- 65.Baker FC, Mitchell D, Driver HS. Oral contraceptives alter sleep and raise body temperature in young women. Pflugers Arch. 2001;442:729–37. doi: 10.1007/s004240100582. [DOI] [PubMed] [Google Scholar]
- 66.Driver HS, Dijk DJ, Werth E, Biedermann K, Borbély AA. Sleep and the sleep electroencephalogram across the menstrual cycle in young healthy women. J Clin Endocrinol Metab. 1996;81:728–35. doi: 10.1210/jcem.81.2.8636295. [DOI] [PubMed] [Google Scholar]
- 67.Izci B, Vennelle M, Liston WA, Dundas KC, Calder AA, Douglas NJ. Sleep-disordered breathing and upper airway size in pregnancy and post-partum. Eur Respir J. 2006;27:321–7. doi: 10.1183/09031936.06.00148204. [DOI] [PubMed] [Google Scholar]
- 68.Saaresranta T, Polo O. Hormones and breathing. Chest. 2002;122:2165–82. doi: 10.1378/chest.122.6.2165. [DOI] [PubMed] [Google Scholar]
- 69.Kambam JR, Handte RE, Brown WU, Smith BE. Effect of normal and preeclamptic pregnancies on the oxyhemoglobin dissociation curve. Anesthesiology. 1986;65:426–7. doi: 10.1097/00000542-198610000-00014. [DOI] [PubMed] [Google Scholar]
- 70.Van Thiel DH, Gavaler JS, Joshi SN, Sara RK, Stremple J. Heartburn of pregnancy. Gastroenterology. 1977;72:666–8. [PubMed] [Google Scholar]
- 71.Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974. doi: 10.1136/bmj.39335.385301.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grindheim G, Estensen ME, Langesaeter E, Rosseland LA, Toska K. Changes in blood pressure during healthy pregnancy: a longitudinal cohort study. J Hypertens. 2012;30:342–50. doi: 10.1097/HJH.0b013e32834f0b1c. [DOI] [PubMed] [Google Scholar]
- 73.Reid J, Skomro R, Cotton D, et al. Pregnant women with gestational hypertension may have a high frequency of sleep disordered breathing. Sleep. 2011;34:1033–8. doi: 10.5665/SLEEP.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lynn FA, Alderdice FA, Crealey GE, McElnay JC. Associations between maternal characteristics and pregnancy-related stress among low-risk mothers: an observational cross-sectional study. Int J Nurs Stud. 2011;48:620–7. doi: 10.1016/j.ijnurstu.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 75.Maasilta P, Bachour A, Teramo K, Polo O, Laitinen LA. Sleep-related disordered breathing during pregnancy in obese women. Chest. 2001;120:1448–54. doi: 10.1378/chest.120.5.1448. [DOI] [PubMed] [Google Scholar]
- 76.Franklin KA, Holmgren PA, Jonsson F, Poromaa N, Stenlund H, Svanborg E. Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest. 2000;117:137–41. doi: 10.1378/chest.117.1.137. [DOI] [PubMed] [Google Scholar]
- 77.Facco FL, Liu CS, Cabello AA, Kick A, Grobman WA, Zee PC. Sleep-disordered breathing: a risk factor for adverse pregnancy outcomes? Am J Perinatol. 2012;29:277–82. doi: 10.1055/s-0031-1295658. [DOI] [PubMed] [Google Scholar]
- 78.O'Brien LM, Bullough AS, Owusu JT, et al. Pregnancy-onset habitual snoring, gestational hypertension, and preeclampsia: prospective cohort study. Am J Obstet Gynecol. 2012;207:487–9. doi: 10.1016/j.ajog.2012.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Feinsilver SH, Hertz G. Respiration during sleep in pregnancy. Clin Chest Med. 1992;13:637–44. [PubMed] [Google Scholar]
- 80.Guilleminault C, Kirisoglu C, Ohayon MM. C-reactive protein and sleep-disordered breathing. Sleep. 2004;27:1507–11. doi: 10.1093/sleep/27.8.1507. [DOI] [PubMed] [Google Scholar]
- 81.Guilleminault C, Kim YD, Palombini L, Li K, Powell N. Upper airway resistance syndrome and its treatment. Sleep. 2000;23(Suppl 4):S197–S200. [PubMed] [Google Scholar]
- 82.Blyton DM, Skilton MR, Edwards N, Hennessy A, Celermajer DS, Sullivan CE. Treatment of sleep disordered breathing reverses low fetal activity levels in preeclampsia. Sleep. 2013;36:15–21. doi: 10.5665/sleep.2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ayrim A, Keskin EA, Ozol D, Onaran Y, Yiidirim Z, Kafali H. Influence of self-reported snoring and witnessed sleep apnea on gestational hypertension and fetal outcome in pregnancy. Arch Gynecol Obstet. 2011;283:195–9. doi: 10.1007/s00404-009-1327-2. [DOI] [PubMed] [Google Scholar]
- 84.Louis JM, Auckley D, Sokol RJ, Mercer BM. Maternal and neonatal morbidities associated with obstructive sleep apnea complicating pregnancy. Am J Obstet Gynecol. 2010;202:261–5. doi: 10.1016/j.ajog.2009.10.867. [DOI] [PubMed] [Google Scholar]
- 85.Ursavas A, Karadag M, Nalci N, Ercan I, Gozu RO. Self-reported snoring, maternal obesity and neck circumference as risk factors for pregnancy-induced hypertension and preeclampsia. Respiration. 2008;76:33–9. doi: 10.1159/000107735. [DOI] [PubMed] [Google Scholar]
- 86.Yinon D, Lowenstein L, Suraya S, et al. Pre-eclampsia is associated with sleep-disordered breathing and endothelial dysfunction. Eur Respir J. 2006;27:328–33. doi: 10.1183/09031936.06.00010905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Edwards N, Blyton DM, Hennessy A, Sullivan CE. Severity of sleep-disordered breathing improves following parturition. Sleep. 2005;28:737–41. doi: 10.1093/sleep/28.6.737. [DOI] [PubMed] [Google Scholar]
- 88.Izci B, Martin SE, Dundas KC, Liston WA, Calder AA, Douglas NJ. Sleep complaints: Snoring and daytime sleepiness in pregnant and pre-eclamptic women. Sleep Med. 2005;6:163–9. doi: 10.1016/j.sleep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 89.Perez-Chada D, Videla AJ, O'Flaherty ME, et al. Snoring, witnessed sleep apnoeas and pregnancy-induced hypertension. Acta Obstet Gynecol Scand. 2007;86:788–92. doi: 10.1080/00016340701281919. [DOI] [PubMed] [Google Scholar]
- 90.Bourjeily G, Raker CA, Chalhoub M, Miller MA. Pregnancy and fetal outcomes of symptoms of sleep-disordered breathing. Eur Respir J. 2010;36:849–55. doi: 10.1183/09031936.00021810. [DOI] [PubMed] [Google Scholar]
- 91.Okun ML, Kravitz HM, Sowers MF, Moul DE, Buysse DJ, Hall M. Psychometric evaluation of the Insomnia Symptom Questionnaire: a self-report measure to identify chronic insomnia. J Clin Sleep Med. 2009;5:41–51. [PMC free article] [PubMed] [Google Scholar]
- 92.Okun ML, Luther JF, Wisniewski SR, Wisner KL. Disturbed sleep and inflammatory cytokine in depressed and nondepressed pregnant women: An exploratory analysis of pregnancy outcomes. Psychosom Med. 2013;75:670–81. doi: 10.1097/PSY.0b013e31829cc3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Torre-Bouscoulet L, Garcia SC, Vazquez Garcia JC, et al. Perceptions of short and long sleep duration and comorbid conditions: the PLATINO study. Sleep Med. 2013;14:850–7. doi: 10.1016/j.sleep.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 94.Troxel WM, Buysse DJ, Matthews KA, et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep. 2010;33:1633–40. doi: 10.1093/sleep/33.12.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Grandner MA, Perlis ML. Insomnia as a cardiometabolic risk factor. Sleep. 2013;36:11–2. doi: 10.5665/sleep.2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stremler R, Hodnett E, Kenton L, et al. Effect of behavioural-educational intervention on sleep for primiparous women and their infants in early postpartum: multisite randomised controlled trial. BMJ. 2013;346:f1164. doi: 10.1136/bmj.f1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bourjeily G, Ankner G, Mohsenin V. Sleep-disordered breathing in pregnancy. Clin Chest Med. 2011;32:175–89. doi: 10.1016/j.ccm.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 98.Chen YH, Kang JH, Lin CC, Wang IT, Keller JJ, Lin HC. Obstructive sleep apnea and the risk of adverse pregnancy outcomes. Am J Obstet Gynecol. 2012;206:136–5. doi: 10.1016/j.ajog.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 99.Connolly G, Razak AR, Hayanga A, Russell A, McKenna P, McNicholas WT. Inspiratory flow limitation during sleep in pre-eclampsia: comparison with normal pregnant and nonpregnant women. Eur Respir J. 2001;18:672–6. doi: 10.1183/09031936.01.00053501. [DOI] [PubMed] [Google Scholar]
- 100.Champagne K, Schwartzman K, Opatrny L, et al. Obstructive sleep apnoea and its association with gestational hypertension. Eur Respir J. 2009;33:559–65. doi: 10.1183/09031936.00122607. [DOI] [PubMed] [Google Scholar]


