Abstract
Objectives: Testicular cancer affects mainly men below the age of 50. An association with occupation and social status has been suggested but risk factors are not well understood. A registry-based case-control study focusing on occupation was performed in Germany.
Methods: All 348 testicular cancer cases with available gainful occupational information registered between 2000 and 2005; as well as 564 suitable controls (from a pool of other cancers) were drawn from the Cancer Registry of Rhineland-Palatinate. Unconditional logistic regression was used to compute odds ratios (OR) and associated 95% confidence intervals (CI).
Results: Slightly elevated OR were observed for technicians and related professionals (OR 1.62, 95% CI 1.00–2.63) and for clerical support workers (OR 1.71, 95% CI 1.14–2.56). This increase was highest in the age group 20–50 for technicians (OR 2.02, 95% CI 1.23–3.33) and clerks (OR 2.00, 95% CI 1.30–3.09), respectively. An association with testicular cancer was observed for no other occupation.
Conclusion: An increased risk of testicular cancer was observed for technicians and related professionals and clerical support workers. This could be related to socioeconomic status or sedentary life style, two factors that were identified in previous studies. While the feasibility of a purely registry-based study was shown, missing occupational data and the choice of cancer controls represent challenges to the validity of this approach.
Keywords: cancer, clerical support workers, men's health, occupational health, sedentary life style, technicians
Zusammenfassung
Ziele: Hodenkrebs betrifft vor allem junge Männer im Alter von unter 50 Jahren. Ein Zusammenhang zwischen erhöhtem Auftreten von Hodenkrebs und Beruf bzw. sozialem Status wurde untersucht (in Betracht gezogen), aber die Risikofaktoren sind bislang noch nicht umfassend erforscht. Eine Register-basierte Fall-Kontroll-Studie zur Untersuchung eines Zusammenhangs von beruflicher Erwerbstätigkeit und Hodenkrebs wurde in Deutschland durchgeführt.
Methoden: 348 Hodenkrebsfälle mit den verfügbaren Informationen zur Erwerbstätigkeit zwischen 2000 und 2005, sowie 564 geeignete Kontrollen (aus einem Pool anderer Krebsarten) wurden aus dem Krebsregister Rheinland-Pfalz gezogen. Mittels einer unkonditionalen logistischen Regression wurden Odds Ratios (OR) und deren 95%-Konfidenzintervall (CI) berechnet.
Ergebnisse: Eine leichte Erhöhung wurde für Techniker und verwandte Berufe (OR 1,62, 95% CI 1,00 bis 2,63) und für Bürokräfte (OR 1,71, 95% CI 1,14 bis 2,56) beobachtet. Dieser Anstieg war am höchsten in der Altersgruppe 20–50 für Techniker (OR 2,02, 95% CI 1,23 bis 3,33) sowie für Bürokräfte (OR 2,00, 95% CI 1,30 bis 3,09). Es wurde keine weitere Assoziation zwischen Hodenkrebs und anderen Berufen beobachtet.
Fazit: Ein erhöhtes Risiko für Hodenkrebs wurde für Techniker und verwandte Berufe sowie für Bürokräfte beobachtet. Dies könnte auf den sozioökonomischen Status bzw. die bewegungsarme Lebensweise zurückgeführt werden, was auch schon in früheren Studien gezeigt wurde. Während die Machbarkeit einer rein Register-basierten Studie gezeigt wurde, stellen die fehlenden beruflichen Daten sowie die Wahl der Krebskontrollen eine Herausforderung für die Richtigkeit dieses Ansatzes dar.
Introduction
Testicular cancer is a rare disease; it occurs most commonly in young men in their third to fifth decade of life and accounts for about 1–3% of all cancers in men in Western countries and about 17% of cancers in men below 45 [1], [2]. Germany is one of the countries with the highest incidence rates of testicular cancer, with an estimated age-standardized incidence rate (Europe standard) of 11.1/105 in 2004 [3].
The risk factors associated with testicular cancer are not very well known apart from the association with cryptorchidism (undescended testis) documented in multiple studies [4], [5], [6], [7], [8], [9], familial association [10] and exposure to high level of estrogen in utero [11].
Some occupational exposures were suggested to be associated with a higher risk for testicular cancer. These occupations include work in agriculture [12]. Rural residence during adulthood was associated with an increased risk of testicular cancer in Italy (Odds Ratio (OR) = 3.31; 95% confidence interval (CI) 1.36–8.01); use of pesticides in gardening was similarly associated with an elevated OR of 1.83 (95% CI 1.02–3.29) [13]. Further relevant occupations seem to include fire fighters and carpenters. In professional fire fighters in Florida the Standardized Incidence Ratio (SIR) was 1.60 (95% CI 1.20–2.09) [14], and similar results were obtained in New Zealand [15] and in Germany [16]. Studies concerning carpenters also showed an increased risk for testicular cancer; in New Jersey the SIR of testicular cancer for carpenters between 1979–2000 was 1.29 (95% CI 0.78–2.01). The incidence rate was increased after a 15-years lag from initial work date (SIR=2.40; 95% CI 1.29–4.32) [17], with similar results documented in Germany [18]. Results for selected other occupations have shown inconsistency associated with an increased risk of testicular cancer. A study on Vietnam war veterans showed a twofold elevated risk for testicular cancer with an OR of 2.5 (95% CI 1.1–5.7) [19]. No clear associations were seen for metal workers [20], but paper and pulp maintenance workers (and not process workers) in Sweden had higher risk of testicular cancer [21]. No clear risk was observed for professional and technical workers [22].
In order to shed more light on the occupational risk factors of testicular cancer and to assess the feasibility of a registry-based case-control study, data from the cancer registry of the German federal state of Rhineland-Palatinate were used to conduct a case-control study for testicular cancer, where both the cases and controls were cancer patients registered in the years 2000–2005. Because of the small number of cases, only broad occupational categories, with limited specificity regarding occupational exposures were used.
Material and methods
The study population includes cases and controls with registered malignancies in the Rhineland Palatinate cancer registry for the period 2000–2005. The registry has an overall completeness of over 90% for all cancers [3]. Cases of testicular cancer diagnosed between 2000 and 2005 in the cancer registry and having occupational information were compared to a set of cancer diagnoses which were chosen to represent the controls pool. These included primary cancer of the stomach, colon, pancreas, kidney, Hodgkin’s lymphoma, thyroid, and lip, oral cavity and pharynx. These cancer types were selected because there was no strong indication of their association with occupational risk factors [23], [24], [25], [26], [27], [28], [29], [30]. Additionally, these cancers affect a wide age group including young patients which made it possible to broadly match them to testicular cancer patients basing on age groups [3], [23].
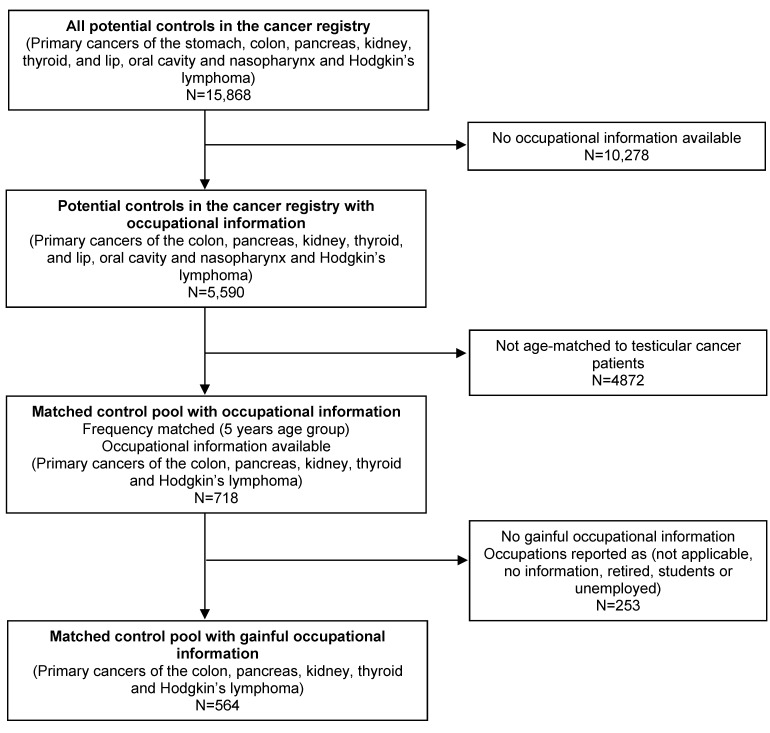
From the group of 15,868 potential controls, controls were matched by 5 years age groups (≤24, 25–29, 30–34, 35–39, 40–44, 45–49, ≥50), giving priority to controls with occupational information. The selection probabilities for the controls were 1 for the age groups ≤24, 25–29, 30–34, 35–39, 0.26 for the age groups 40–44, 45–49 and 0.02 for the age group ≥50. However, not all the cancer types included in the control pool eventually contributed controls to be matched to our cases, either due to absence of registered patients in specific age group (mostly people younger than 40 years) or because of missing occupational information. As a result of these restrictions, only a subset of cancers (colon, pancreas, kidney, thyroid cancers and Hodgkin’s lymphoma) eventually formed our control population from the potential control pool.
Frequency matching was implemented because of the relatively young age of testicular cancer cases which rendered the selection of individually matched controls rather difficult. The occupations were originally coded according to the German Federal Employment Office coding system. They were re-coded according to the International Standard Classification of Occupations version 2008 [31], for better comparability with international results.
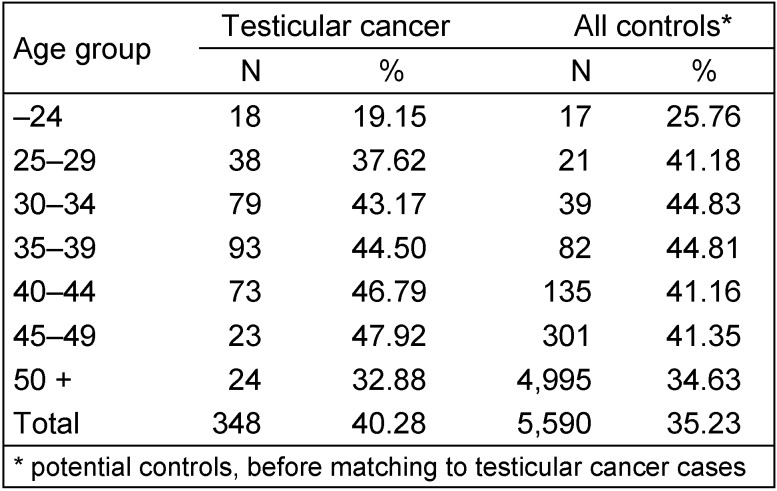
Due to the very large proportion of registrations with missing occupational information in the control population (about 70% of the potential controls in the cancer registry) a decision to include only cases and controls with job titles indicating gainful occupations in the analyses was made. The availability of job information for the potential controls in the age groups 25–49 was similar to that of testicular cancer patients as shown in Table 1 (Tab. 1). The stepwise process of controls selection is illustrated in more details in Figure 1 (Fig. 1).
Table 1. Availability of gainful occupational information for the testicular cancer cases and potential control population.
Figure 1. Stepwise selection of the controls population.
Because of the relatively small number of cases, the analysis included only the major occupational groups and the main subgroups rather than specific job titles to avoid diluting any possible effects.
The analysis of the case-control study included calculating the odds ratio for the different jobs via unconditional logistic regression in relation to the different job titles. The reference group for the analysis was all the other occupations combined against the occupational title under study. To investigate the effect of this approach, a sensitivity analysis was done with another reference group including a set of occupational titles with no proven associations with testicular cancer risk reported in the literature (armed forces, services and sales workers, skilled agriculture, and elementary occupations). Age-group specific odds ratios for the occupational distribution of the patients in the highest risk age group (20–50) were also calculated. No additional adjustment for confounders could be done as no relevant additional information on cases and controls is available in the registry.
Results
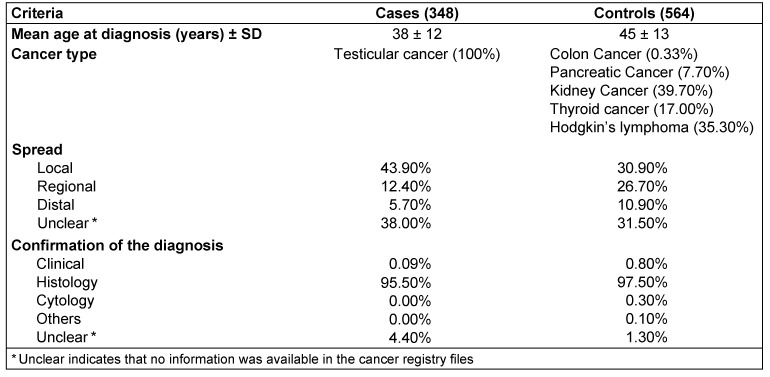
There were 864 primary testicular cancer cases and 718 age matched controls selected from the Rhineland-Palatinate cancer registry. For the analysis 348 cases and 564 cancer controls with gainful occupational information were available. The vast majority of the cases and controls were verified histologically (95.5% and 97.5% respectively) (Table 2 (Tab. 2)).
Table 2. Main characteristics of the testicular cancer cases and controls included.
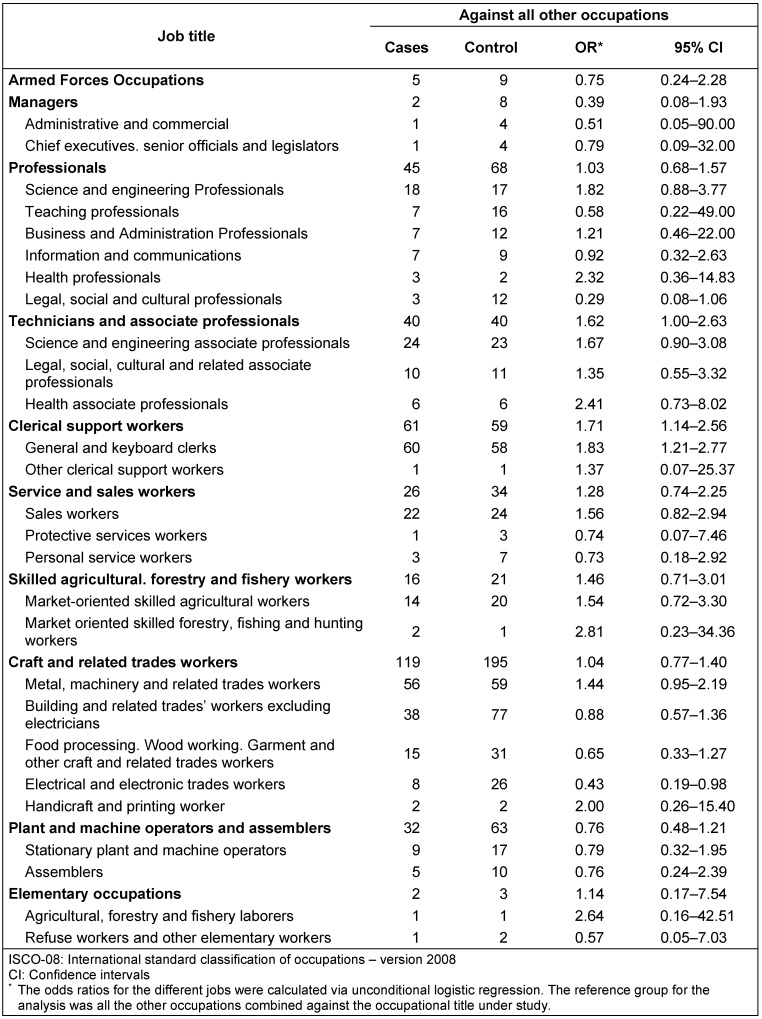
The odds ratios for testicular cancer risk are shown in Table 3 (Tab. 3). There was a significant risk elevation for technicians and associate professionals, OR=1.62 (95% CI 1.00–2.63) and clerical support workers, OR=1.71 (95% CI 1.14–2.56) mostly for the subgroup general and keyboard clerics with an OR=1.83 (95% CI 1.21–2.77).
Table 3. Age adjusted Odds ratio of testicular cancer risk in association with different occupational categories (ISCO-08). Gainful occupations only with all other occupations as reference group.
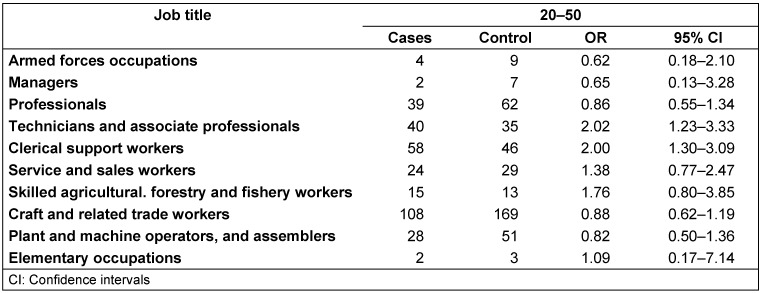
In analyses stratified by age group the OR for the technicians and associate professionals and the clerical support workers was also elevated for the age-group 20–50 years, OR=2.02 (95% CI 1.23–3.33) and 2.00 (95% CI 1.30–3.09) respectively (Table 4 (Tab. 4)).
Table 4. Odds ratios for different occupations in 20–50 years age category for testicular cancer patients gainful occupations only (main occupational categories).
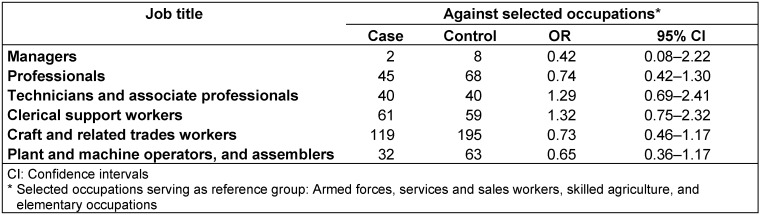
When the OR was calculated against a selected group of occupations as reference (see methods), no significant increase was noted for any of the occupations, but the directions of associations were unchanged (Table 5 (Tab. 5)).
Table 5. Age adjusted Odds ratio of testicular cancer risk in association with different occupational categories gainful occupations only with selected occupations as the reference group.
Discussion
This is the first registry-based case-control analysis to be conducted in the Rhineland Palatinate cancer registry, where both cases and controls were anonymously derived from the registry database. The registry has a good completeness of over 90% (and 95% for testicular cancer).
The study showed a slight increase in the OR for testicular cancer in association with occupational codes related to “technicians and associate professionals” and to “clerical support workers”. However, due to the large number of missing occupational data these results need to be viewed with great caution.
The feasibility of the registry-based case-control approach was tested with a view to better utilize the data stored in the cancer registry. However, this approach was associated with some difficulties. The use of cancer cases as controls instead of the general population might raise concerns regarding the findings of this study. However, the cancer types included in our control group are generally not known to be strongly associated with occupational exposures. Thyroid cancer and Hodgkin’s Lymphoma are considered to be associated with radiation exposure [23], [25], but this was not a limitation since testicular cancer does not seem to be associated with radiation [32]. Other difficulties encountered include the fact that the average age of male cancer patients is usually high while testicular cancer patients are mostly young or middle-aged men. This led to problems in finding appropriate age-matched controls for testicular cancer patients since there were very few cancers with relatively young age at occurrence. An additional limitation of this study was the high proportion of missing occupational information for both the cases and controls. Less than 50% of all cases and a little more than 30% of the overall potential controls had occupational information available. To overcome this limitation the analysis was restricted to cases and controls with gainful occupational information available in the registry. This may induce selection bias if availability of occupational information is linked to other differences relevant for the comparisons performed in this study, or if particular occupations had a higher probability to be noted in the registry. While this remains a possibility, we observed a wide range of occupational codes among both cases and controls. Additionally, the availability of occupational information in the high risk age groups was similar in testicular cancer patients and the selected controls.
We found an increased risk of testicular cancer in two groups, technicians and associate professionals; and clerical support workers. An increase in testicular cancer risk in these groups was also reported in some previous studies [22], [33]. However, in a large prospective study that included 7,519 incident cases of testicular cancer from Denmark, Finland, Iceland, Norway and Sweden (NOCCA study), the Standardized Incidence Ratios (SIR) for these occupations were only slightly elevated. The SIR for technician workers and clerical workers were 1.06 (95% CI 0.99–1.15) and 1.14 (95% CI 1.02–1.27) respectively. In the NOCCA study, physicians were found to have the highest risk for testicular cancer, with an SIR of 1.48 (95% CI 1.15–1.88) [34]. In our study the risk for health professionals and health associate professionals was non-significantly elevated, OR 2.32 (95% CI 0.36–14.83) and 2.41 (95% CI 0.73–8.02) respectively. Combining both groups into one “health related jobs” group resulted in an OR of 1.82 (95% CI 0.73–4.54). Obviously, the Nordic study included a much larger number of cases in comparison to our study, did not rely on cancer controls and was much less afflicted by missing data issues, which once again underlines the need for caution when interpreting our data. It is, however, interesting to note that both studies indicate risk elevations associated with medical occupations.
The two groups (technicians and associate professionals and clerical support workers) with elevated OR noted in our analysis share a similar job environment, including long hours of office work. The increase of testicular cancer risk in both technicians and clerical support workers could be expected to be related to their socioeconomic status which, although not available in the cancer registry data, may be higher than in comparison groups. Several studies have indicated that testicular cancer is associated with higher socioeconomic status [35], [36], [37], but more detailed mechanisms are not understood. A possible explanation of our findings is the sedentary life style characteristic of these two groups. In a review discussing the lifestyle factors associated with testicular dysfunction, sedentary work habits were suggested to increase testicular temperature [38]. An increase in testicular temperature has long been associated with the increase in testicular cancer incidence; however, in a study conducted in the United States, exposure to elevated temperatures (≥80ºF or 26.7ºC) was not significantly associated with testicular cancer risk (OR 1.20; 95% CI 0.80–1.80) [39]. Other studies investigating the effect of raised temperature on testicular cancer incidence have also failed to detect an association [8], [40], [41], [42]. The specific work environment may also lead to reduced physical activity. The UK testicular cancer study group reported a protective effect of exercise against testicular cancer, whereas a positive association with sedentary life style was reported [8]. A Canadian study also showed protective effects of moderate to high levels of recreational and – somewhat less clearly – for occupational activities [5]. An inverse association between physical activity during childhood and the risk of testicular cancer was also reported [43]. Contrary to the above findings, many studies reported no effect [44], [45] or even positive associations [46] between testicular cancer and physical activity.
In conclusion, we found a slightly increased risk of testicular cancer for both technicians and associate professionals and for clerical support workers. Whether this increase is related to specific occupational exposure in those people including the lifestyle factors associated with these occupations such as increased scrotal temperature or lack of physical activity due to prolonged periods of sitting, or exposure to electromagnetic fields from electrical equipments such as laptops [32], [47] is still an open question. These exposures (heat, physical activity and exposure to electromagnetic fields) were previously discussed as possible causes for testicular cancer among other possibilities in pulp and paper workers in Sweden, a relationship was not confirmed though [21]. Further studies are needed to investigate these associations in more detail. The feasibility of a registry-based case-control study in the cancer registry could be demonstrated, while limitations were highlighted. For the future, such studies are likely to become more informative if the amount of missing data can be reduced, as physicians provide more complete data to the registry wherever possible.
Notes
Competing interests
The authors declare that they have no competing interests.
Funding
L. Y.’s work on this review was supported by the DAAD (German Academic Exchange Service) as part of her doctoral study.
Authorship
All authors participated in planning the study and writing the manuscript.
References
- 1.Chia VM, Quraishi SM, Devesa SS, Purdue MP, Cook MB, McGlynn KA. International trends in the incidence of testicular cancer, 1973-2002. Cancer Epidemiol Biomarkers Prev. 2010 May;19(5):1151–1159. doi: 10.1158/1055-9965.EPI-10-0031. Available from: http://dx.doi.org/10.1158/1055-9965.EPI-10-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray F, Richiardi L, Ekbom A, Pukkala E, Cuninkova M, Moller H. Trends in testicular cancer incidence and mortality in 22 European countries: continuing increases in incidence and declines in mortality. Int J Cancer. 2006 Jun;118(12):3099–3111. doi: 10.1002/ijc.21747. Available from: http://dx.doi.org/10.1002/ijc.21747. [DOI] [PubMed] [Google Scholar]
- 3.Emrich K, Husmann G, Zeißig S, Seebauer G, Blettner M. Krebs in Rheinland-Pfalz. Inzidenz und Mortalität im Jahr 2006. Mainz: Krebsregister Rheinland-Pfalz; 2009. [Google Scholar]
- 4.Møller H, Prener A, Skakkebaek NE. Testicular cancer, cryptorchidism, inguinal hernia, testicular atrophy, and genital malformations: case-control studies in Denmark. Cancer Causes Control. 1996 Mar;7(2):264–274. doi: 10.1007/BF00051302. Available from: http://dx.doi.org/10.1007/BF00051302. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher RP, Huchcroft S, Phillips N, Hill GB, Coldman AJ, Coppin C, Lee T. Physical activity, medical history, and risk of testicular cancer (Alberta and British Columbia, Canada) Cancer Causes Control. 1995 Sep;6(5):398–406. doi: 10.1007/BF00052179. Available from: http://dx.doi.org/10.1007/BF00052179. [DOI] [PubMed] [Google Scholar]
- 6.Prener A, Engholm G, Jensen OM. Genital anomalies and risk for testicular cancer in Danish men. Epidemiology. 1996 Jan;7(1):14–19. doi: 10.1097/00001648-199601000-00004. Available from: http://dx.doi.org/10.1097/00001648-199601000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Kanto S, Hiramatsu M, Suzuki K, Ishidoya S, Saito H, Yamada S, Satoh M, Saito S, Fukuzaki A, Arai Y. Risk factors in past histories and familial episodes related to development of testicular germ cell tumor. Int J Urol. 2004 Aug;11(8):640–646. doi: 10.1111/j.1442-2042.2004.00853.x. Available from: http://dx.doi.org/10.1111/j.1442-2042.2004.00853.x. [DOI] [PubMed] [Google Scholar]
- 8.Forman D, Pike MC, Davey G, Dawson S, Baker K, Chilvers CED, Oliver RTD, Coupland CAC United Kingdom Testicular Cancer Study Group. Aetiology of testicular cancer: association with congenital abnormalities, age at puberty, infertility, and exercise. BMJ. 1994 May 28;308(6941):1393–1399. doi: 10.1136/bmj.308.6941.1393. Available from: http://dx.doi.org/10.1136/bmj.308.6941.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swerdlow AJ, Higgins CD, Pike MC. Risk of testicular cancer in cohort of boys with cryptorchidism. BMJ. 1997 May;314(7093):1507–1511. doi: 10.1136/bmj.314.7093.1507. Available from: http://dx.doi.org/10.1136/bmj.314.7093.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong C, Lönnstedt I, Hemminki K. Familial testicular cancer and second primary cancers in testicular cancer patients by histological type. Eur J Cancer. 2001 Oct;37(15):1878–1885. doi: 10.1016/S0959-8049(01)00172-1. Available from: http://dx.doi.org/10.1016/S0959-8049(01)00172-1. [DOI] [PubMed] [Google Scholar]
- 11.Sonke GS, Chang S, Strom SS, Sweeney AM, Annegers JF, Sigurdson AJ. Prenatal and perinatal risk factors and testicular cancer: a hospital-based case-control study. Oncol Res. 2007;16(8):383–387. doi: 10.3727/000000006783980928. [DOI] [PubMed] [Google Scholar]
- 12.Hofmann J, Guardado J, Keifer M, Wesseling C. Mortality among a cohort of banana plantation workers in Costa Rica. Int J Occup Environ Health. 2006 Oct-Dec;12(4):321–328. doi: 10.1179/oeh.2006.12.4.321. [DOI] [PubMed] [Google Scholar]
- 13.Nori F, Carbone P, Giordano F, Osborn J, Figa-Talamanca I. Endocrine-disrupting chemicals and testicular cancer: a case-control study. Archives of environmental & occupational health. 2006;61(2):87–95. doi: 10.3200/AEOH.61.2.87-95. Available from: http://dx.doi.org/10.3200/AEOH.61.2.87-95. [DOI] [PubMed] [Google Scholar]
- 14.Ma F, Fleming LE, Lee DJ, Trapido E, Gerace TA. Cancer incidence in Florida professional firefighters, 1981 to 1999. J Occup Environ Med. 2006 Sep;48(9):883–888. doi: 10.1097/01.jom.0000235862.12518.04. Available from: http://dx.doi.org/10.1097/01.jom.0000235862.12518.04. [DOI] [PubMed] [Google Scholar]
- 15.Bates MN, Fawcett J, Garrett N, Arnold R, Pearce N, Woodward A. Is testicular cancer an occupational disease of fire fighters? Am J Ind Med. 2001 Sep;40(3):263–270. doi: 10.1002/ajim.1097. Available from: http://dx.doi.org/10.1002/ajim.1097. [DOI] [PubMed] [Google Scholar]
- 16.Stang A, Jöckel KH, Baumgardt-Elms C, Ahrens W. Firefighting and risk of testicular cancer: results from a German population-based case-control study. Am J Ind Med. 2003 Mar;43(3):291–294. doi: 10.1002/ajim.10178. Available from: http://dx.doi.org/10.1002/ajim.10178. [DOI] [PubMed] [Google Scholar]
- 17.Dement J, Pompeii L, Lipkus IM, Samsa GP. Cancer incidence among union carpenters in New Jersey. J Occup Environ Med. 2003 Oct;45(10):1059–1067. doi: 10.1097/01.jom.0000085892.01486.6a. Available from: http://dx.doi.org/10.1097/01.jom.0000085892.01486.6a. [DOI] [PubMed] [Google Scholar]
- 18.Stang A, Ahrens W, Baumgardt-Elms C, Bromen K, Stegmaier C, Jöckel KH. Carpenters, cabinetmakers, and risk of testicular germ cell cancer. J Occup Environ Med. 2005 Mar;47(3):299–305. doi: 10.1097/01.jom.0000155716.63919.0a. Available from: http://dx.doi.org/10.1097/01.jom.0000155716.63919.0a. [DOI] [PubMed] [Google Scholar]
- 19.Tarone RE, Hayes HM, Hoover RN, Rosenthal JF, Brown LM, Pottern LM, Javadpour N, O'Connell KJ, Stutzman RE. Service in Vietnam and risk of testicular cancer. J Natl Cancer Inst. 1991 Oct;83(20):1497–1499. doi: 10.1093/jnci/83.20.1497. Available from: http://dx.doi.org/10.1093/jnci/83.20.1497. [DOI] [PubMed] [Google Scholar]
- 20.Rhomberg W, Schmoll HJ, Schneider B. High frequency of metalworkers among patients with seminomatous tumors of the testis: a case-control study. Am J Ind Med. 1995 Jul;28(1):79–87. doi: 10.1002/ajim.4700280107. Available from: http://dx.doi.org/10.1002/ajim.4700280107. [DOI] [PubMed] [Google Scholar]
- 21.Andersson E, Nilsson R, Torén K. Testicular cancer among Swedish pulp and paper workers. Am J Ind Med. 2003 Jun;43(6):642–646. doi: 10.1002/ajim.10223. Available from: http://dx.doi.org/10.1002/ajim.10223. [DOI] [PubMed] [Google Scholar]
- 22.Pollán M, Gustavsson P, Cano MI. Incidence of testicular cancer and occupation among Swedish men gainfully employed in 1970. Ann Epidemiol. 2001 Nov;11(8):554–562. doi: 10.1016/S1047-2797(01)00234-4. Available from: http://dx.doi.org/10.1016/S1047-2797(01)00234-4. [DOI] [PubMed] [Google Scholar]
- 23.Robert Koch-Institut, editor; Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V., editor Krebs in Deutschland 2005/2006. Häufigkeiten und Trends. 7th ed. Berlin: Robert Koch-Institut; 2010. (Beiträge zur Gesundheitsberichterstattung des Bundes). Available from: http://www.krebsdaten.de/Krebs/SharedDocs/Downloads/KiD_2010/KID2010.html. [Google Scholar]
- 24.Kaerlev L, Lynge E, Sabroe S, Olsen J. Colon cancer controls versus population controls in case-control studies of occupational risk factors. BMC Cancer. 2004 Apr;4:15. doi: 10.1186/1471-2407-4-15. Available from: http://dx.doi.org/10.1186/1471-2407-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karunanayake CP, Singh GV, Spinelli JJ, McLaughlin JR, Dosman JA, McDuffie HH, Pahwa P. Occupational exposures and Hodgkin Lymphoma: Canadian case-control study. J Occup Environ Med. 2009 Dec;51(12):1447–1454. doi: 10.1097/JOM.0b013e3181be6bfe. Available from: http://dx.doi.org/10.1097/JOM.0b013e3181be6bfe. [DOI] [PubMed] [Google Scholar]
- 26.Chow WH, Dong LM, Devesa SS. Epidemiology and risk factors for kidney cancer. Nat Rev Urol. 2010 May;7(5):245–257. doi: 10.1038/nrurol.2010.46. Available from: http://dx.doi.org/10.1038/nrurol.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lowenfels AB, Maisonneuve P. Epidemiology and prevention of pancreatic cancer. Jpn J Clin Oncol. 2004 May;34(5):238–244. doi: 10.1093/jjco/hyh045. Available from: http://dx.doi.org/10.1093/jjco/hyh045. [DOI] [PubMed] [Google Scholar]
- 28.Kernan GJ, Ji BT, Dosemeci M, Silverman DT, Balbus J, Zahm SH. Occupational risk factors for pancreatic cancer: a case-control study based on death certificates from 24 U.S. states. Am J Ind Med. 1999 Aug;36(2):260–270. doi: 10.1002/(SICI)1097-0274(199908)36:2<260::AID-AJIM5>3.0.CO;2-P. Available from: http://dx.doi.org/10.1002/(SICI)1097-0274(199908)36:2<260::AID-AJIM5>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 29.Leux C, Guénel P. Risk factors of thyroid tumors: role of environmental and occupational exposures to chemical pollutants. Rev Epidemiol Sante Publique. 2010 Oct;58(5):359–367. doi: 10.1016/j.respe.2010.05.005.. Available from: http://dx.doi.org/10.1016/j.respe.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 30.Lope V, Pérez-Gómez B, Aragonés N, López-Abente G, Gustavsson P, Plato N, Silva-Mato A, Pollán M. Occupational exposure to chemicals and risk of thyroid cancer in Sweden. Int Arch Occup Environ Health. 2009 Jan;82(2):267–274. doi: 10.1007/s00420-008-0314-4. Available from: http://dx.doi.org/10.1007/s00420-008-0314-4. [DOI] [PubMed] [Google Scholar]
- 31.International Standard Classifications of Occupations. Version 2008. 2008. [last accessed April 4 2011]. Available from: http://www.ilo.org/public/english/bureau/stat/isco/index.htm. [Google Scholar]
- 32.Yousif L, Blettner M, Hammer GP, Zeeb H. Testicular cancer risk associated with occupational radiation exposure: a systematic literature review. J Radiol Prot. 2010 Sep;30(3):389–406. doi: 10.1088/0952-4746/30/3/R01. Available from: http://dx.doi.org/10.1088/0952-4746/30/3/R01. [DOI] [PubMed] [Google Scholar]
- 33.Swerdlow AJ, Douglas AJ, Huttly SR, Smith PG. Cancer of the testis, socioeconomic status, and occupation. Br J Ind Med. 1991 Oct;48(10):670–674. doi: 10.1136/oem.48.10.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pukkala E, Martinsen JI, Lynge E, Gunnarsdottir HK, Sparén P, Tryggvadottir L, Weiderpass E, Kjaerheim K. Occupation and cancer - follow-up of 15 million people in five Nordic countries. Acta Oncol. 2009;48(5):646–790. doi: 10.1080/02841860902913546. Available from: http://dx.doi.org/10.1080/02841860902913546. [DOI] [PubMed] [Google Scholar]
- 35.Pukkala E, Weiderpass E. Socio-economic differences in incidence rates of cancers of the male genital organs in Finland, 1971-95. Int J Cancer. 2002 Dec 20;102(6):643–648. doi: 10.1002/ijc.10749. Available from: http://dx.doi.org/10.1002/ijc.10749. [DOI] [PubMed] [Google Scholar]
- 36.Møller H, Skakkebaek NE. Risks of testicular cancer and cryptorchidism in relation to socio-economic status and related factors: case-control studies in Denmark. Int J Cancer. 1996 May 3;66(3):287–293. doi: 10.1002/(SICI)1097-0215(19960503)66:3<287::AID-IJC2>3.0.CO;2-V. Available from: http://dx.doi.org/10.1002/(SICI)1097-0215(19960503)66:3<287::AID-IJC2>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 37.van den Eeden SK, Weiss NS, Strader CH, Daling JR. Occupation and the occurrence of testicular cancer. Am J Ind Med. 1991;19(3):327–337. doi: 10.1002/ajim.4700190307. Available from: http://dx.doi.org/10.1002/ajim.4700190307. [DOI] [PubMed] [Google Scholar]
- 38.Agarwal A, Desai NR, Ruffoli R, Carpi A. Lifestyle and testicular dysfunction: a brief update. Biomed Pharmacother. 2008 Oct;62(8):550–553. doi: 10.1016/j.biopha.2008.07.052.. Available from: http://dx.doi.org/10.1016/j.biopha.2008.07.052. [DOI] [PubMed] [Google Scholar]
- 39.Zhang ZF, Vena JE, Zielezny M, Graham S, Haughey BP, Brasure J, Marshall JR. Occupational exposure to extreme temperature and risk of testicular cancer. Arch Environ Health. 1995 Jan-Feb;50(1):13–18. doi: 10.1080/00039896.1995.9955007. Available from: http://dx.doi.org/10.1080/00039896.1995.9955007. [DOI] [PubMed] [Google Scholar]
- 40.UK Testicular Cancer Study Group. Social, behavioural and medical factors in the aetiology of testicular cancer: results from the UK study. Br J Cancer. 1994 Sep;70(3):513–520. doi: 10.1038/bjc.1994.337. Available from: http://dx.doi.org/10.1038/bjc.1994.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karagas MR, Weiss NS, Strader CH, Daling JR. Elevated intrascrotal temperature and the incidence of testicular cancer in noncryptorchid men. Am J Epidemiol. 1989 Jun;129(6):1104–1109. doi: 10.1093/oxfordjournals.aje.a115232. [DOI] [PubMed] [Google Scholar]
- 42.Brown LM, Pottern LM, Hoover RN. Testicular cancer in young men: the search for causes of the epidemic increase in the United States. J Epidemiol Community Health. 1987 Dec;41(4):349–354. doi: 10.1136/jech.41.4.349. Available from: http://dx.doi.org/10.1136/jech.41.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cook MB, Zhang Y, Graubard BI, Rubertone MV, Erickson RL, McGlynn KA. Risk of testicular germ-cell tumours in relation to childhood physical activity. Br J Cancer. 2008 Jan;98(1):174–178. doi: 10.1038/sj.bjc.6604109. Available from: http://dx.doi.org/10.1038/sj.bjc.6604109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thune I, Lund E. Physical activity and the risk of prostate and testicular cancer: a cohort study of 53,000 Norwegian men. Cancer Causes Control. 1994 Nov;5(6):549–556. doi: 10.1007/BF01831383. Available from: http://dx.doi.org/10.1007/BF01831383. [DOI] [PubMed] [Google Scholar]
- 45.Littman AJ, Doody DR, Biggs ML, Weiss NS, Starr JR, Schwartz SM. Physical activity in adolescence and testicular germ cell cancer risk. Cancer Causes Control. 2009 Oct;20(8):1281–1290. doi: 10.1007/s10552-009-9347-6. Available from: http://dx.doi.org/10.1007/s10552-009-9347-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Srivastava A, Kreiger N. Relation of physical activity to risk of testicular cancer. Am J Epidemiol. 2000 Jan;151(1):78–87. doi: 10.1093/oxfordjournals.aje.a010126. Available from: http://dx.doi.org/10.1093/oxfordjournals.aje.a010126. [DOI] [PubMed] [Google Scholar]
- 47.Baumgardt-Elms C, Schümann M, Ahrens W, Bromen K, Stang A, Jahn I, Stegmaier C, Jöckel KH. Residential exposure to overhead high-voltage lines and the risk of testicular cancer: results of a population-based case-control study in Hamburg (Germany) Int Arch Occup Environ Health. 2005 Feb;78(1):20–26. doi: 10.1007/s00420-004-0550-1. Available from: http://dx.doi.org/10.1007/s00420-004-0550-1. [DOI] [PubMed] [Google Scholar]