Abstract
OBJECTIVE
To evaluate whether socioeconomic environment affects the adoption of new laser technology for treatment of benign prostatic hyperplasia (BPH).
METHODS
Using all payer data, we identified all discharges for laser prostatectomy or transurethral resection of the prostate (TURP) performed in Florida (2001–2009). We determined whether or not each of 114 healthcare markets (Hospital Service Areas) offered laser prostatectomy or TURP and assessed the market-level socioeconomic environment using a previously described ZIP code based summary score. We used generalized estimating equations to examine the association of socioeconomic environment with offering laser prostatectomy or TURP, adjusting for additional market characteristics.
RESULTS
Better socioeconomic environment was associated with offering laser prostatectomy (odds ratio 1.21 for each 1 point increase in summary score, 95% confidence interval 1.08–1.35, P <.001). Adoption of laser prostatectomy over time was more rapid in markets with superior socioeconomic environment (P <.001 for interaction of socioeconomic summary score with year), such that by study midpoint, 82% of advantaged vs 54% of disadvantaged markets had adopted this new technology. In contrast, socioeconomic environment had only minimal effects on whether or not a market offered TURP.
CONCLUSION
We found delayed access to new laser technology in more disadvantaged socioeconomic environments, which may translate into disparities in certain outcomes after transurethral surgery for BPH.
Keywords: laser prostatectomy, benign prostatic hyperplasia, socioeconomic status, adoption of new technology
INTRODUCTION
Benign prostatic hyperplasia (BPH) is the most common benign neoplasm in men, with more than three out of four men over age 70 having significant lower urinary tract symptoms.1,2 However, men from different socioeconomic backgrounds differentially present with symptoms of BPH. For example, men with lower education, lower income, and Medicaid insurance are reporting more lower urinary tract symptoms (LUTS) than men of higher socioeconomic status (SES).3 Because symptom severity is associated with an increased need for BPH-related surgery,4 socioeconomically disadvantaged men are also at higher risk for ultimate surgical intervention.5
Surgical interventions for BPH have undergone significant changes over the last decade, due to the introduction of new surgical technology. Specifically, use of laser of laser prostatectomy has increased significantly, supplanting about half of all conventional transurethral resections of the prostate (TURP) by 2009.6 Although TURP was one of the first minimally invasive procedures in urology and provides excellent long-term outcomes, laser prostatectomy is thought to be less invasive. Advantages of laser prostatectomy include a lower risk of bleeding, no risk of transurethral resection (TUR) syndrome, shorter catheterization time, and hospital stay.7–9 However, adoption of this new technology requires upfront investments in physician training and surgical equipment. Physicians and hospitals in socioeconomically disadvantaged markets may not always have these resources, which may lead to differential adoption of laser prostatectomy. In fact, previous studies have found evidence that disparities in health care are often driven by where patients seek care. For example, hospitals with a large proportion of socioeconomically disadvantaged patients tend to deliver lower quality care and have higher mortality rates.10,11
For these reasons, we examined whether market-level socioeconomic environment was associated with the adoption of new laser technology for the treatment of BPH, which could have led to differences in access to this new technology. In order to assess whether differences in access to surgical care for BPH were technology specific, we also evaluated whether socioeconomic environment affected access to TURP.
METHODS
Study population
We used Florida’s State Ambulatory Surgery database (SASD) and State Inpatient database (SID) from the Healthcare Cost and Utilization Project to identify a cohort of patients who underwent TURP [Current Procedural Terminology (CPT) codes 52601, 52612, 52614, 52620, 52630, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 60.29] or laser prostatectomy (CPT codes 52647, 52648, 52649, ICD-9-CM code 60.21) between 2001 and 2009 (n=96,134). These databases capture 100% of the outpatient and inpatient discharges from Florida, respectively. We chose Florida because it is one of the larger and more socioeconomically diverse states participating in the Healthcare Cost and Utilization Project. In addition, the Florida data capture discharges from a variety of practice locations, including freestanding ambulatory surgery centers where many of these procedures are performed. We excluded patients with a diagnosis of prostate cancer (n=11,768), with a code for both TURP and laser prostatectomy (n=410), with a ZIP code for which the SES information was not available (n=2), as well as those under age 40 (n=100). We obtained patient insurance status directly from SASD and SID. In order to obtain market characteristics, we linked these surgical cases to ZIP code level 2000 census data (for median male population age; proportion of African Americans and Hispanics in the population; median household income; median value of housing units; proportion of households with interest, dividend, or rental income; proportion of adults completing high school; proportion of adults completing college; proportion of employed residents with management, professional, and related occupations; poverty rate; proportion of urban population) and to the Health Resources and Services Administration’s Area Resource File (county level data for number of urologists per 100,000 population, number of surgical procedures per 100,000 population). We then divided Florida into 114 healthcare markets based on Hospital Service Areas (HSA) as defined by the Dartmouth Atlas of Healthcare.12 Patients were assigned to their respective HSA according to their residence.
MEASURING SOCIOECONOMIC ENVIRONMENT
Each patient was assigned a ZIP code level socioeconomic summary score according to methods previously described by Diez-Roux et al.13 In brief, this score measured 3 components of SES based on data from the 2000 census: (1) wealth and income (median household income, median value of housing units, proportion of households with interest, dividend, or rental income), (2) education (proportion of adults completing high school and proportion of adults completing college), and (3) occupation (proportion of employed residents with management, professional, and related occupations). For each of these 6 variables, a ZIP code level z-score was calculated by subtracting the overall mean and dividing by the SD. These 6 z-scores were then summed for each ZIP code to derive a socioeconomic summary score.13 Finally, we computed an average summary score for each HSA. The resulting scores ranged from −7.8 to 13.8, with a higher score representing a more advantageous socioeconomic environment. We categorized HSAs according to their socioeconomic environment into equally sized groups based on whether they fell within the lowest, medium, or highest socioeconomic summary score tertile.
OUTCOMES
With the HSA serving as our unit of analysis, our primary outcome was whether or not an HSA offered laser prostatectomy in a given year. In order to compare whether these effects were specific to laser technology, we also examined whether or not a market offered TURP in a given year. To increase specificity, offering laser prostatectomy or TURP was defined as performing at least 5 laser prostatectomy or TURP procedures per year. To evaluate whether the choice of this cutoff value significantly affected our findings, we also performed sensitivity analyses categorizing markets as offering laser prostatectomy or TURP if they performed at least 2 TURP or laser prostatectomy procedures per year, respectively. This change did not materially affect the results, so only data from the main analyses are presented.
STATISTICAL ANALYSES
We compared patient insurance status and market characteristics (median male age, proportion of African Americans, proportion of Hispanics, median household income, value of housing units, households with interest, dividend, or rental income, education, occupation, number of urologists, poverty rate, urban population, and number of surgical procedures) across the 3 groups of HSAs using the Kruskal-Wallis test and analysis of variance (ANOVA) F-test. The proportion of markets offering or not offering laser prostatectomy and TURP was plotted across years to visualize time trends.
We used multivariable generalized estimating equations with a log it link, assuming a first-order autoregressive correlation structure to account for the longitudinal nature of our data.14 In these models, the dependent variable was whether or not an HSA offered laser prostatectomy. The main exposures were the market-level socioeconomic summary score and the calendar year. All models were adjusted for patient insurance status and for the market characteristics mentioned above. Similar models were constructed with the dependent variable being whether or not an HSA offered TURP. From these models, we calculated the adjusted probability of offering laser prostatectomy or TURP for markets within the lowest, medium, or highest socioeconomic summary score tertile.
We performed all analyses using Stata version 12SE. All tests were 2-tailed and we set the probability of a type 1 error at 0.05 or less. The University of Michigan Medical School Institutional Review Board exempted this study from review in accordance with the Code of Federal Regulations Title 45, subpart A, section 46.101, paragraph b, subparagraph 4.
RESULTS
Disadvantaged health care markets in the lowest socioeconomic summary score tertile had a younger population, higher proportion of minorities, higher poverty rates, less urban population, fewer urologists, and fewer surgical procedures performed than markets of better socioeconomic environment (Table 1). More socioeconomically disadvantaged markets also had slightly lower rates of transurethral procedures and a higher proportion of Medicaid insured patients, whereas the proportion of patients with Medicare or private insurance did not differ across markets (Table 1).
Table 1.
Summary statistics for the 114 Hospital Service Areas in Florida by socioeconomic environment
| Variables | Socioeconomic Summary Score Tertile
|
||
|---|---|---|---|
| Low (n = 38) | Medium (n = 38) | High (n = 38) | |
| Socioeconomic summary score, mean (range) | −2.7 (−7.8 to −0.4) | 0.9 (−0.4 to 2.1) | 4.5 (2.1 to 13.8) |
| Total number of TURP procedures performed 2001–2009 | 8283 | 29,331 | 16,783 |
| Total number of laser prostatectomy procedures performed 2001–2009 | 5295 | 14,987 | 9175 |
| Yearly number of transurethral procedures for BPH per 100,000 men age 40 and up, median (IQR)* | 209 (129–299) | 234 (164–345) | 236 (159–355) |
| Age, median (IQR), years* | 37.1 (34.3–40.9) | 41.1 (36.5–46.1) | 43.4 (37.5–48.5) |
| African American, %** | 16 | 10 | 5 |
| Hispanic, %** | 13 | 9 | 10 |
| Household income, median, $* | 31,036 | 38,160 | 46,928 |
| Value of housing units, median, $* | 75,700 | 101,883 | 139,104 |
| Households with interest, dividend, or rental income, %** | 28 | 37 | 47 |
| Adult residents who completed high school, %** | 70 | 82 | 88 |
| Adult residents who completed college, %** | 12 | 20 | 30 |
| Employed residents with executive, managerial, or professional occupations, %** | 24 | 30 | 37 |
| Poverty rate,%** | 17 | 11 | 8 |
| Urban population, %** | 58 | 87 | 92 |
| Number of urologists per 100,000 population** | 2.8 | 4.0 | 3.9 |
| Number of surgical procedures per 1000 population** | 73 | 87 | 86 |
| Proportion Medicare insured patients, % | 77 | 77 | 77 |
| Proportion Medicaid insured patients, %*** | 1.1 | 1.0 | 0.6 |
| Proportion privately insured patients, % | 19 | 20 | 20 |
BPH, benign prostatic hyperplasia; IQR, interquartile range; TURP, transurethral resection of the prostate.
P <.001 across socioeconomic summary score tertiles, Kruskat-Wallis test.
P <.001 across socioeconomic summary score tertiles, analysis of variance (ANOVA) F-test
P <.01 across socioeconomic summary score tertiles, ANOVA (F-test).
In bivariate analyses, disadvantaged markets were significantly less likely to offer laser prostatectomy (P <.001, Fig. 1). In 2001, 24% of these markets offered laser prostatectomy compared to 34% of the markets with a more socioeconomically privileged population (Fig. 1). In addition, adoption of laser prostatectomy was more tempered in markets with a worse socioeconomic environment. Only 53% offered laser prostatectomy by 2006, when adoption had plateaued, compared to almost all of the socioeconomically privileged markets (89%, Fig. 1). In contrast, more than 70% of the markets in the lowest socioeconomic tertile and almost all of the markets in the medium and high socioeconomic tertiles offered TURP throughout the study period (Fig. 1). Toward the end of the study period, several markets emerged within the highest socioeconomic tertile that offered only laser prostatectomy (Fig. 1). We performed multivariable analyses to calculate the proportion of markets offering laser prostatectomy or TURP while adjusting for insurance status and market characteristics. Socioeconomic environment was associated with offering laser prostatectomy. For each 1-point increase in the socioeconomic summary score, there were 1.21 times greater odds of offering laser prostatectomy (Table 2). Adoption of laser prostatectomy over time was more rapid among markets with better socioeconomic environment (P •••.001 for interaction of socioeconomic summary score with year), such that by 2005 only 54% of disadvantaged markets had adopted this new procedure, compared with 82% of markets with an advantageous socioeconomic environment (Fig. 2A).
Figure 1.
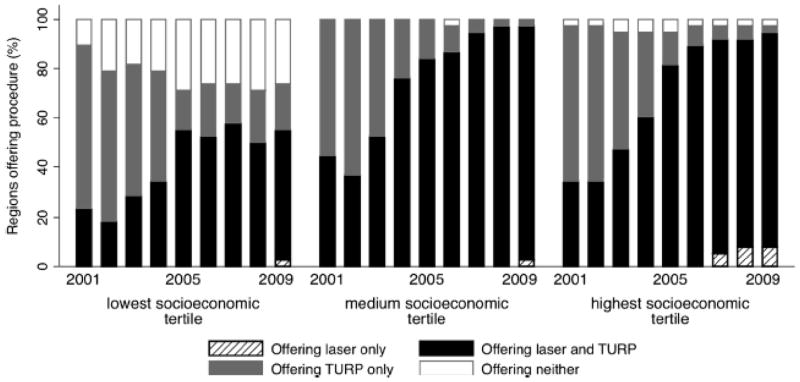
Unadjusted proportion of markets (n = 114) offering laser prostatectomy only, laser prostatectomy and transurethral resection of the prostate (TURP), TURP only, or neither from 2001 to 2009 by socioeconomic environment.
Table 2.
Multivariable regression models evaluating the association of market characteristics with offering laser prostatectomy or TURP, respectively
| Variables | Offering Laser
|
Offering TURP
|
||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Per year | 1.49 (1.35–1.64) | <.001 | 0.83 (0.75–0.93) | .001 |
| Per 1-point increase in socioeconomic summary score | 1.21 (1.08–1.35) | .001 | 0.89 (0.81–0.98) | .015 |
| Per 10 years of age | 2.01 (1.25–3.24) | .004 | 12.33 (4.75–32.01) | <.001 |
| African American* | 0.97 (0.94–1.01) | .153 | 0.93 (0.90–0.96) | <.001 |
| Hispanic* | 1.04 (1.01–1.07) | .009 | 1.02 (0.98–1.05) | .391 |
| Number of urologists per 100,000 population | 1.18 (0.96–1.45) | .111 | 1.85 (1.47–2.34) | <.001 |
| Number of surgical procedures per 100,000 population | 1.01 (1.00–1.02) | .034 | 1.01 (1.00–1.02) | .072 |
| Medicare* | 1.00 (0.99–1.01) | .502 | 1.00 (0.99–1.02) | .562 |
| Medicaid* | 1.02 (0.96–1.08) | .624 | 1.12 (0.97–1.29) | .119 |
CI, confidence interval; OR, odds ratio; other abbreviation as in Table 1.
Per each 1% increase in proportion.
Figure 2.
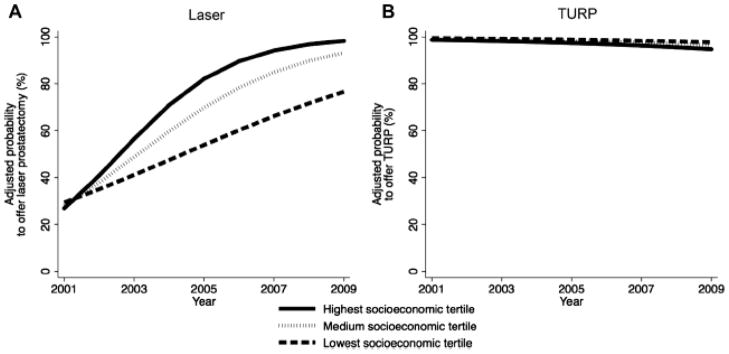
Adjusted proportion of markets offering laser prostatectomy (A) and transurethral resection of the prostate (TURP) (B) from 2001–2009. Models were adjusted for median male age. proportion of African Americans, proportion of Hispanics, number of urologists, number of surgical procedures, proportion of patients with Medicare insurance, and proportion of patients with Medicaid insurance.
In order to assess whether disparities in access to surgical care for BPH were technology specific, we performed similar multivariable analyses evaluating whether a market offered traditional TURP or not. Once we adjusted for covariates, markets with higher socioeconomic summary scores were statistically significantly less likely to offer this procedure (Table 2). There was a slight decline over time in the proportion of markets offering TURP, but socioeconomic environment did not affect this time-trend (P •••.985 for interaction of socioeconomic summary score with year, Fig. 2B). In addition, the absolute effect of socioeconomic environment on offering TURP was minimal after adjusting for all covariates (Fig. 2B).
COMMENT
We found that an increasing number of markets offered laser prostatectomy over time. However, adoption of this new technology was fastest in markets with advantageous socioeconomic environment, whereas socioeconomic environment had only minimal effects on whether or not a market offered TURP (Fig. 2). Toward the end of the study period, we noted the emergence of several markets within the highest socioeconomic tertile that offered exclusively laser prostatectomy (Fig. 1).
Access to surgical care and to surgical technology frequently differs by SES. For example, endovascular aortic aneurysm repair and laparoscopic surgery was less likely performed among socioeconomically disadvantaged patients.15–17 Regarding urologic procedures, patients of lower SES who underwent radical prostatectomy, radical cystectomy, or radical nephrectomy were significantly less likely to have their surgery at a high-volume hospital compared with patients of higher SES.18 Our study is the first to examine the extent to which socioeconomic environment is associated with access to new urologic technology. New technology plays an increasingly important role in urologic surgery19,20; and our findings reveal delayed access to one of these new technologies in socioeconomically disadvantaged markets.
There are several potential reasons for these findings. First, acquiring new surgical technology requires investments by the hospital. The hospital needs to acquire the appropriate laser system and cystoscopes, which have a cost of approximately $100,000, not including the disposable equipment.21 Hospitals in socioeconomic disadvantaged markets may already have significant strain on their budgets and may not be able to make these initial and ongoing investments.22 In contrast, TURP has been widely available and has low ongoing costs for disposables. However, as technology costs decrease over time, some hospitals in socioeconomically disadvantaged markets may be able to acquire the new technology with some delay. Second, surgeons need to invest time to acquire the necessary skills to perform a new procedure. For example, it is recommended that urologists take a formal training course, complete an online training module, watch several live procedures performed by an experienced surgeon, and be subsequently proctored for a minimum of 5 cases before performing laser prostatectomy independently.23 In addition, laser prostatectomy may initially take longer than TURP, especially while the surgeon is early in his learning curve.24 Thus, urologists need to invest a significant amount of time to learn this new procedure, which in turn carries an opportunity cost to the practice. Therefore, surgeons practicing in less favorable socioeconomic environments may be more inclined to use TURP rather than adopt new laser technology. Third, patients of low SES may be late adopters of new technology.25 This would then lead to decreased demand for the new procedure in more disadvantaged socioeconomic environments, lessening the incentive for hospitals and physicians to adopt this new surgical technology. Socioeconomic environment was not the only factor that limited access to newer technologies. Markets with a younger population and lower surgical volume tended to be less likely to offer laser prostatectomy (Table 2). The adoption of laser prostatectomy may also have been influenced by other factors that could not be assessed with our datasets, such as the nature of contractual relationships between physicians and hospitals or the availability of laser equipment for rent.
There are several limitations to our study. First, the use of SASD and SID data allowed us to examine 100% of the inpatient and outpatient discharges for laser prostatectomy and TURP in Florida during the study period, but office-based procedures could not be included. However, 85% or more of all laser procedures are performed in clinical settings that were included in our data (ie, inpatient, outpatient, or ambulatory surgery center).26,27 Thus, we were able to capture the vast majority of laser procedures done over the study period. Second, the lack of specificity of ICD-9-CM codes did not allow us to differentiate what kind of laser was used during the inpatient procedures. However, there was rapid diffusion of photovaporization of the prostate during the study period.27,28 In addition, 93% of the laser prostatectomies performed on an outpatient basis in 2009 (and therefore coded with explicit CPT codes within the SASD) were laser photovaporizations, whereas only 3% and 4% represented laser coagulations and laser enucleations. Therefore, our results very likely primarily reflect differential adoption of photovaporization of the prostate. Third, we assigned patients to HSAs based on their home ZIP code. Therefore, it is possible that some patients crossed borders into other markets to obtain their procedures. However, given that transurethral surgery for BPH is a low-risk procedure, which typically is performed by general urologists, it is very likely that the vast majority of patients received their care locally. Additionally, we decreased the risk of misclassification secondary to occasional border crossing by requiring that at least 5 procedures were performed in a year before we classified a market as offering a procedure. We also performed sensitivity analyses changing this threshold to 2 procedures per year, which confirmed our findings and adds additional validity to our results. Last, given that this is an observational study using secondary data, we were unable to account for unmeasured confounding. However, we linked the surgery data to the 2000 census and the Area Resource File and thus had many potentially confounding market characteristics available, which were included in our multivariable analyses.
CONCLUSIONS
In spite of these limitations, our findings have important implications. Our findings reveal that access to new laser technology for the treatment of BPH was delayed in socioeconomically disadvantaged markets. In contrast, socioeconomic environment was not important for whether or not a market offered TURP. Therefore, men from socioeconomically disadvantaged markets may face barriers in access to new technologies. To the extent that these new technologies offer significant advantages to patients, this may translate into disparities in outcomes, such as perioperative blood loss, incidence of TUR syndrome, length of hospital stay, or length of catheterization. Moving forward, ongoing efforts addressing and reducing social inequalities may ultimately help with providing more balanced access to surgical technology in the future.
Acknowledgments
Research support: FRS is supported by NIH/NIDDK grant T32 DK07782 and American Cancer Society Postdoctoral Fellowship award PF-12-118-01-CPPB
We thank Samuel R. Kaufman for statistical support.
Footnotes
Financial conflicts of interest: none
References
- 1.Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173:1256–1261. doi: 10.1097/01.ju.0000155709.37840.fe. [DOI] [PubMed] [Google Scholar]
- 2.Platz EA, Smit E, Curhan GC, et al. Prevalence of and racial/ethnic variation in lower urinary tract symptoms and noncancer prostate surgery in U.S. men. Urology. 2002;59:877–883. doi: 10.1016/s0090-4295(01)01673-9. [DOI] [PubMed] [Google Scholar]
- 3.Fowke JH, Munro H, Signorello LB, et al. Association between socioeconomic status (SES) and lower urinary tract symptom (LUTS) severity among black and white men. J Gen Intern Med. 2011;26:1305–1310. doi: 10.1007/s11606-011-1776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaplan S, Garvin D, Gilhooly P, et al. Impact of baseline symptom severity on future risk of benign prostatic hyperplasia-related outcomes and long-term response to finasteride. The Pless Study Group. Urology. 2000;56:610–616. doi: 10.1016/s0090-4295(00)00724-x. [DOI] [PubMed] [Google Scholar]
- 5.Fowke JH, Murff HJ, Signorello LB, et al. Race and socioeconomic status are independently associated with benign prostatic hyperplasia. J Urol. 2008;180:2091–2096. doi: 10.1016/j.juro.2008.07.059. discussion 2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schroeck FR, Hollingsworth JM, Kaufman SR, et al. Population based trends in the surgical treatment of benign prostatic hyperplasia. J Urol. 2012;188:1837–1841. doi: 10.1016/j.juro.2012.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strope SA, Yang L, Nepple KG, et al. Population based comparative effectiveness of transurethral resection of the prostate and laser therapy for benign prostatic hyperplasia. J Urol. 2012;187:1341–1345. doi: 10.1016/j.juro.2011.11.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burke N, Whelan JP, Goeree L, et al. Systematic review and metaanalysis of transurethral resection of the prostate versus minimally invasive procedures for the treatment of benign prostatic obstruction. Urology. 2010;75:1015–1022. doi: 10.1016/j.urology.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Lukacs B, Loeffler J, Bruyère F, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol. 2012;61:1165–1173. doi: 10.1016/j.eururo.2012.01.052. [DOI] [PubMed] [Google Scholar]
- 10.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. 2007;167:1233–1239. doi: 10.1001/archinte.167.12.1233. [DOI] [PubMed] [Google Scholar]
- 11.Birkmeyer NJ, Gu N, Baser O, et al. Socioeconomic status and surgical mortality in the elderly. Med Care. 2008;46:893–899. doi: 10.1097/MLR.0b013e31817925b0. [DOI] [PubMed] [Google Scholar]
- 12.The Dartmouth Institute for Health Policy & Clinical Practice. [Accessed September 1, 2011];Dartmouth Atlas of Health Care. 2011 Available at: http://www.dartmouthatlas.org/
- 13.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 14.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 2. College Station, TX: Stata Press; 2008. [Google Scholar]
- 15.Osborne NH, Mathur AK, Upchurch GR, Jr, Dimick JB. Understanding the racial disparity in the receipt of endovascular abdominal aortic aneurysm repair. Arch Surg. 2010;145:1105–1108. doi: 10.1001/archsurg.2010.213. [DOI] [PubMed] [Google Scholar]
- 16.Ricciardi R, Selker HP, Baxter NN, et al. Disparate use of minimally invasive surgery in benign surgical conditions. Surg Endosc. 2008;22:1977–1986. doi: 10.1007/s00464-008-0003-0. [DOI] [PubMed] [Google Scholar]
- 17.Abenhaim HA, Azziz R, Hu J, et al. Socioeconomic and racial predictors of undergoing laparoscopic hysterectomy for selected benign diseases: analysis of 341487 hysterectomies. J Minim Invasive Gynecol. 2008;15:11–15. doi: 10.1016/j.jmig.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 18.Trinh QD, Sun M, Sammon J, et al. Disparities in access to care at high-volume institutions for uro-oncologic procedures. Cancer. 2012;118:4421–4426. doi: 10.1002/cncr.27440. [DOI] [PubMed] [Google Scholar]
- 19.Atug F, Castle EP, Woods M, et al. Robotics in urologic surgery: an evolving new technology. Int J Urol. 2006;13:857–863. doi: 10.1111/j.1442-2042.2006.01428.x. [DOI] [PubMed] [Google Scholar]
- 20.Te AE. The development of laser prostatectomy. BJU Int. 2004;93:262–265. doi: 10.1111/j.1464-410x.2004.04598.x. [DOI] [PubMed] [Google Scholar]
- 21.El-Hakim A. TURP in the new century: an analytical reappraisal in light of lasers. Can Urol Assoc J. 2010;4:347–349. doi: 10.5489/cuaj.10149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bazzoli GJ, Clement JP, Lindrooth RC, et al. Hospital financial condition and operational decisions related to the quality of hospital care. Med Care Res Rev. 2007;64:148–168. doi: 10.1177/1077558706298289. [DOI] [PubMed] [Google Scholar]
- 23.Zorn KC, Liberman D. GreenLight 180W XPS photovaporization of the prostate: how I do it. Can J Urol. 2011;18:5918–5926. [PubMed] [Google Scholar]
- 24.Chung DE, Te AE. High-power 532 nm laser prostatectomy: an update. Curr Opin Urol. 2010;20:13–19. doi: 10.1097/MOU.0b013e3283336f58. [DOI] [PubMed] [Google Scholar]
- 25.Finney Rutten LJ, Nelson DE, Meissner HI. Examination of population-wide trends in barriers to cancer screening from a diffusion of innovation perspective (1987–2000) Prev Med. 2004;38:258–268. doi: 10.1016/j.ypmed.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 26.Malaeb BS, Yu X, McBean AM, Elliott SP. National trends in surgical therapy for benign prostatic hyperplasia in the United States (2000–2008) Urology. 2012;79:1111–1116. doi: 10.1016/j.urology.2011.11.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu X, Elliott SP, Wilt TJ, McBean AM. Practice patterns in benign prostatic hyperplasia surgical therapy: the dramatic increase in minimally invasive technologies. J Urol. 2008;180:241–245. doi: 10.1016/j.juro.2008.03.039. discussion 245. [DOI] [PubMed] [Google Scholar]
- 28.Malek RS. Photoselective KTP laser vaporization of obstructive BPH (PVP) In: Baba S, Ono Y, editors. Interventional Management of Urological Diseases. Vol. 8. Tokyo: Springer Japan; 2006. [Accessed October 10, 2011]. pp. 103–122. Available at: http://www.springerlink.com/content/t0624757428624x3/ [Google Scholar]


