Abstract
Purpose
Multikinase growth inhibitors inhibit their target kinases with varying potency. Patients often require lower doses or therapy breaks due to drug toxicities. To evaluate the effects of drug withdrawal on hepatocellular carcinoma cells after incubation with growth-inhibitory concentrations of regorafenib, cell growth, migration and invasion, and signaling were examined.
Methods
Cell proliferation, motility, and invasion were analyzed by MTT, wound healing, and invasion assays, respectively, and MAPK pathway protein markers were analyzed by Western blot.
Results
After regorafenib removal, cell growth, migration, and invasion recovered. Repeated drug exposure resulted in changes in cell growth patterns. Recovery could be blocked by sub-growth-inhibitory concentrations of either doxorubicin or vitamin K1. Recovery of growth was associated with increased phospho-JNK, phospho-p38, and phospho-STAT3 levels. The recovery of growth, migration, and signaling were blocked by a JNK inhibitor.
Conclusions
Removal of regorafenib from growth-inhibited cells resulted in a JNK-dependent recovery of growth and migration.
Keywords: Hepatocarcinoma; Regorafenib; Reversibility; Migration, invasion; Growth
Introduction
Sorafenib (Nexavar) is an oral multikinase inhibitor [1–3]. It has effects on many cell types, including hepatocellular carcinoma (HCC) cells [4], as well as tumor vascular endothelial cells. It causes HCC growth inhibition in vitro of experimental HCC in vivo and was FDA approved for treatment for human HCC after a phase III trial showed a 10-week survival benefit [5]. An Asian trial was similar [6], but with lower survival. It has dermal and systemic toxicities [7–9], which can result in lowering of drug dose, temporary or permanent therapy cessation.
The improved knowledge of molecular mechanisms in hepatocarcinogenesis today provides the opportunity for targeted therapy with new small molecule inhibitors, as regorafenib (BAY 73-4506, Stirvaga).
Regorafenib, a sorafenib analog [10], has a distinct biochemical kinase inhibition profile and pharmacologic characteristics, including potent inhibition of several angiogenic, stromal and oncogenic kinases, and broad spectrum activity against several experimental tumors [11]. It has shown clinical promise for GIST and colorectal cancer [12, 13] and is being tested in other tumors, including HCC. These drugs differ from cancer chemotherapies in mainly inhibiting cell growth, rather than being cytocidal. Although a reversal of kinase inhibitor effects has been previously noted, this has only recently been described for multikinase inhibitors [14–17].
While resistance to cancer drugs can result from rare, preexisting genetic mutations that emerge in response to drug treatment, accumulating evidence has pointed to additional non-genetic, potentially reversible mechanisms [18].
During acute response to various anticancer agents in several different drug sensitive human cancer cell lines, there is a small subpopulation of reversibly “drug-tolerant” cells that maintain viability under conditions where the vast majority of the cell population is rapidly killed.
We previously found that cells, treated with regorafenib and then replaced with drug-free medium, showed a recovery of normal cell growth [17]. In this report, we examine this phenomenon analyzing growth, migration, and invasion processes.
Materials and methods
Cells and drugs
Regorafenib was gifted from Bayer Corp (West Haven, CT USA); doxorubicin was purchased from Pfizer (Rome, Italy), vitamin K1 was purchased from International Medication Systems, Limited (So. El Monte, CA, USA), JNK inhibitor (SP600125) from Santa Cruz Biotechnology (Santa Cruz, CA, USA).
Hep3B, HepG2, and PLC/PRF/5 human HCC lines were purchased from the American Type Culture Collection (ATCC, Rockville, MD, USA). Culture medium was Dulbecco’s Modified Eagle’s Medium (DMEM). All culture materials were purchased from Sigma-Aldrich (Milan, Italy).
Cell culture
Cells were cultured in DMEM in monolayer culture, supplemented with 10 % fetal bovine serum (FBS), 100 U/ml penicillin, and 100 μg/ml streptomycin, and incubated at 37 °C in a humidified atmosphere containing 5 % CO2 in air. At confluence, cells were harvested by trypsinization and subcultured with a 1:4 split ratio.
Drug treatments
Cells were seeded at 0.6 × 105 cells/2 ml medium containing 10 % FBS in 35 mm tissue culture dishes (Corning Costar, Milan, Italy). They were incubated for 24 h for attachment; then, the medium was replaced by fresh culture medium containing regorafenib 5.0 μM, or other concentrations dissolved in dimethyl sulfoxide (DMSO) for 72 h. Doxorubicin was used at 0.012, 0.025, or 0.05 μM dissolved in 0.9 % NaCl solution. Vitamin K1 was used at 6.25, 12.5, or 25.0 μM in sterile water. JNK inhibitor was used at 20 μM dissolved in DMSO. Each experiment included an untreated and a solvent control. Triplicate cultures were used for each drug concentration and controls; each experiment was repeated three times.
Recovery/reversibility
Hep3B, HepG2, and PLC/PRF/5 cells were treated with regorafenib as previously described above; then, the medium was removed and replaced with fresh medium without drug (T0). The T0 represents the end of time of drug treatment (72 h). At this time, the cells were harvested and analyzed. The rate of cell recovery was then evaluated at different subsequent times: 24 h (T1), 48 h (T2), 72 h (T3), and 96 h (T4).
Assessment of cell proliferation
At the indicated times, the proliferative response was estimated by colorimetric 3-(4,5 dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) test and 5-bromo-2′-deoxy-uridine Labeling and Detection (BrdU) kit (Roche Diagnostics GmbH, Mannheim, Germany), as previously described [19]. Trypan blue exclusion was used to evaluate cell viability. Each experiment was performed in triplicate and repeated three times.
Migration assay
Cells grew for 48 h in medium containing regorafenib concentrations or solvent (control), until confluence. A scratch wound was generated with a pipette tip. After rinsing with medium to remove detached cells, low serum medium (1 % FBS) without drug was added. Photographs were taken of each well immediately (T0) and after various times T1, T2, T3, and T4 using a Leica DMRXA camera (Leica Microsystems, Milan, Italy). Images were analyzed using ImageJ Software (http://rsb.info.nih.gov/ij/). The distance that cells migrated through the area created by scratching was determined by measuring the wound width at T1, T2, T3, and T4 and subtracting it from the wound width at the start. The values were expressed as percentage of migration, with 100 % being when the wound was completely closed. The results were representative of three independent experiments.
Invasion assay
Cell invasion assays were performed using Matrigel (BD Transduction, San Jose, CA, USA)-coated Transwells (8 μm pore PET membrane, Millipore, Billerica, MA, USA) as previously described [19]. Briefly, treated or recovered cells were suspended in low serum medium. Complete medium was added to the bottom wells. After incubation, the invading cells were fixed and stained. The images were acquired and analyzed counting the cells with ImageJ Software. Values obtained were expressed as percentage of invasion, setting the cell counts of control cells as 100 %. Results were representative of three independent experiments.
Western blot (WB)
We analyzed the MAPK signaling, apoptosis, and autophagy pathways in Hep3B cells during cell proliferation from T0 to T4 by WB. WB method was previously described [17]. Briefly, cells were lysed in RIPA buffer (Sigma-Aldrich, Milan; Italy), and, after quantitation, equal amounts of protein (50 μg) were resolved on SDS/polyacrylamide gels and transferred to polyvinyldifluoride (PVDF) membrane (BioRad, Milan, Italy). The followed primary antibodies were used: MKK4 and phospho-MKK4 (Ser257) (pMKK4), JNK and phospho-JNK (Thr183, Tyr185) (pJNK), phospho-STAT3 (Tyr705, Ser727) (pSTAT3), STAT3, phospho-p38 MAPK (Thr180, Tyr182) (pp38) and p38 MAPK, phospho-Bcl-2 (Ser70) (pBcl-2), LC3 II, cleaved caspase-7 and caspase-8 and β-actin (Cell Signaling, Beverly, MA, USA), and Bax, Bcl-xL, and Beclin-1 (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Protein expression was determined with horseradish peroxidase-conjugated secondary antibody and enhanced chemiluminescence (ECL) (Cell Signaling).
The band intensity was measured by densitometry using the ChemiDoc XRS apparatus and specific software (Bio-Rad). The protein levels were normalized with respect to that of β-actin. At least three independent experiments have been carried out, and representative results are shown.
Transmission electron microscopy (TEM)
Transmission electron microscopy was performed on Hep3B cells at T0 and T3. After washing with PBS pH 7.4, the monolayer cells were immediately fixed with 2.5 % glutaraldehyde for 30 min at 4 °C and then postfixed in 1 % OsO4 for 20 min at 4 °C, progressively dehydrated by increasing concentrations of ethanol and finally treated with propylene oxide and included in epoxy resin. Sections (1.5 μm and 70–90 nm) prepared by ultramicrotome (PTXl-RMC, Tucson, AZ, USA) were examined by TEM Morgagni 268 (FEI Electron Optics, Eindhoven, the Netherlands) and its image analyzer iTEM (Soft Imaging System, Munster, Germany). Quantification of cells in apoptosis or autophagy: micrographs of 25 single cells in T0 or in T3 were analyzed. Cells were considered non-apoptotic and non-autophagic if the integrity of the nuclear and cytoplasmic structures was maintained. Differences between cells with and without morphological alterations in two groups of cells are expressed in percentage.
Statistical analysis
The differences between two unmatched groups were evaluated by Mann–Whitney nonparametric test.
For multiple comparisons was used one-way ANOVA test followed by Dunnett’s post test.
The computer software used was GraphPad Prism version 5.0.
P-values of < 0.05 were considered statistically significant.
All experiments were done in triplicate, and data are presented as mean ± standard deviation (SD).
Results
Growth recovery after regorafenib treatment
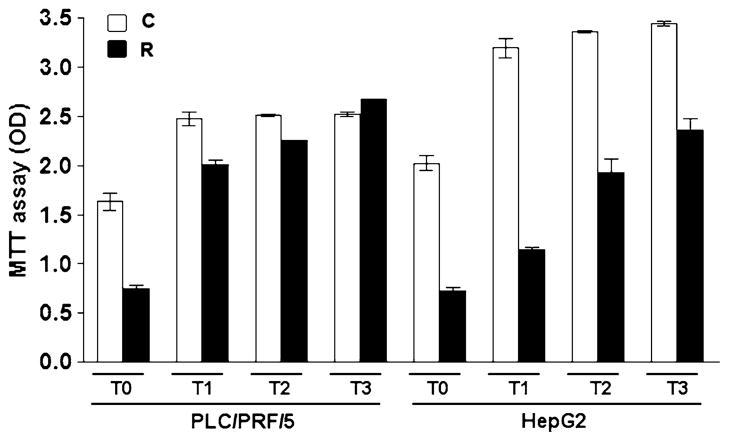
A preliminary report showed reversible growth inhibition of Hep 3B cells treated with regorafenib for 72 h [17]. In this report, we have extended this treatment to include both PLC/PRF/5 and HepG2 HCC cell lines (Fig. 1). The Hep3B cells were treated with regorafenib 5 μM for a longer period (5–7 days). If the cells reached confluence during this period, the treatment was prolonged after splitting and subcultures with 1:4 ratio.
Fig. 1.
Effects of regorafenib on cell growth recovery in PLC/PRF/5 and HepG2 cell lines. The PLC/PRF/5 and HepG2 cell lines were cultured in regorafenib 5 μM for 72 h. The medium was then removed (T0), and the cells were cultured for the indicated further days (T1–T3) in drug-free medium and analyzed using the MTT assay. The percentage of recovery of the treated cells respect control (vehicle) cells (100 % at T3) was 100 and 60 % for PLC/PRF/5 and HepG2, respectively
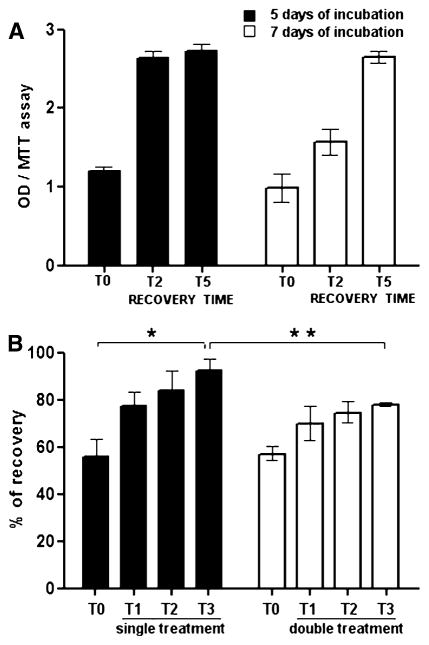
Trypan blue exclusion test was used to evaluate cell viability. After 5 or 7 days of treatment, the drug was removed, and growth recovery was examined for further 5 days (Fig. 2a).
Fig. 2.
Recovery of growth after regorafenib-mediated inhibition. a Hep3B cells were cultured in regorafenib 5 μM for 5 or 7 days to inhibit growth. The medium was then removed (T0), and the cells were cultured for the indicated further days in drug-free medium and analyzed using the MTT assay. b Hep3B cells were doubly treated with regorafenib or vehicle and followed after each treatment for growth recovery at different times (T1–T3), using the MTT assay. Values were expressed as percentage of recovery of the treated cells respect control (vehicle) cells (100 % at T3). *P < 0.05, **P < 0.001
This treatment period caused growth inhibition, with subsequent recovery. In separate experiments, recovered cells were subcultured to ensure normal growth and absence of residual toxicity and then treated a second time with regorafenib 1 μM for 72 h. Cell growth inhibition and recovery were examined. We found incomplete recovery in twice-treated cells in which the percentage of recovery after 72 h was 78 % against the 92 % in cells that received only one treatment (Fig. 2b).
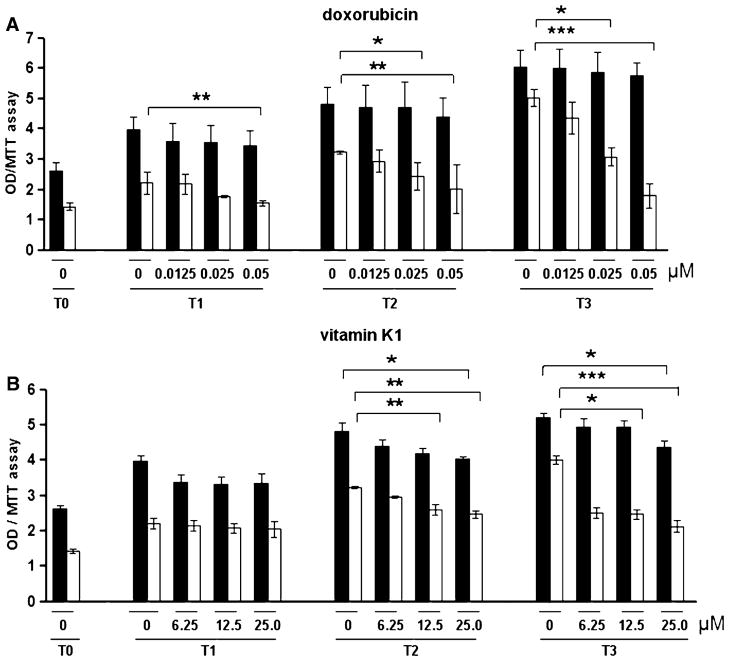
Both doxorubicin 0.1 μM and vitamin K1 50 μM inhibit HCC cell growth [17]. To investigate the possible modulation of growth recovery after regorafenib, regorafenib pre-treated cells were further treated after drug removal with low concentrations of either doxorubicin 0.0125–0.05 μM or vitamin K1 6.25–25.0 μM, concentrations that did not inhibit growth when the drugs were used alone. Growth recovery of the previously regorafenib-inhibited cells was then examined. Doxorubicin at non-growth-inhibitory concentrations when used alone partially inhibited the growth recovery (Fig. 3a), as did vitamin K1 (Fig. 3b).
Fig. 3.
Effects of doxorubicin and vitamin K1 on cell growth recovery. Hep3B cells were treated with regorafenib 5 μM (white columns) or vehicle (black columns). After medium renewal (T0), the cells cultured with the indicated concentrations of doxorubicin (a) or vitamin K1 (b) were followed for growth recovery at different times (T1–T3) using the MTT assay. *P < 0.05, **P < 0.001, ***P < 0.0001
Recovery from regorafenib-mediated inhibition of migration
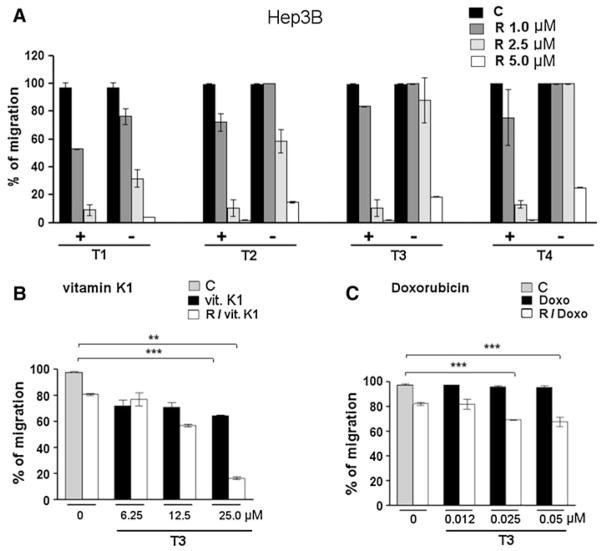
Regorafenib 1 μM can inhibit HCC cell migration, whereas 5.0 μM was needed for growth inhibition [19]. A migration assay was performed comparing the percentage of migration of cells treated with various regorafenib concentrations to that of cells after removal of the same drug concentrations (Fig. 4a). We found that migration recovered after removal of regorafenib 1.0 or 2.5 μM, but not after prior treatment with 5.0 μM. Recovery of migration was thus more sensitive than recovery of growth inhibition, as described above. Doxorubicin and vitamin K1 were then examined for their effects on recovery from regorafenib treatment on cell migration. As in the growth assays, low concentrations of doxorubicin (0.025–0.05 μM) were found to antagonize the recovery of cell migration (Fig. 4c). Vitamin K1 (12.5–25.0 μM) also significantly antagonized recovery of migration (Fig. 4b), as for cell growth recovery (Fig. 3b).
Fig. 4.
Effects of doxorubicin or vitamin K1 on recovery of cell migration. a Cells treated with different regorafenib concentrations (+) were compared with cells after removal of the same drug concentrations (−) and followed for recovery of migration at different times (T1–T4) after the scratch (T0). (b, c) Cells were treated with regorafenib or vehicle. Medium was then removed (T0) and cells cultured in medium containing the indicated concentrations of vitamin K1 (B) or doxorubicin (C) and followed for recovery of migration. Values were expressed as percentage of migration, 100 % representing the completely closed wound. The symbols minus and plus are two cell groups: cell treated with different concentrations of regorafenib (+) versus cells that, after regorafenib treatment, are cultured in fresh medium without drug (−). The gray bars represent non-drug-treated cells (c). C: vehicle, R: regorafenib. *P < 0.05, **P < 0.001, ***P < 0.0001
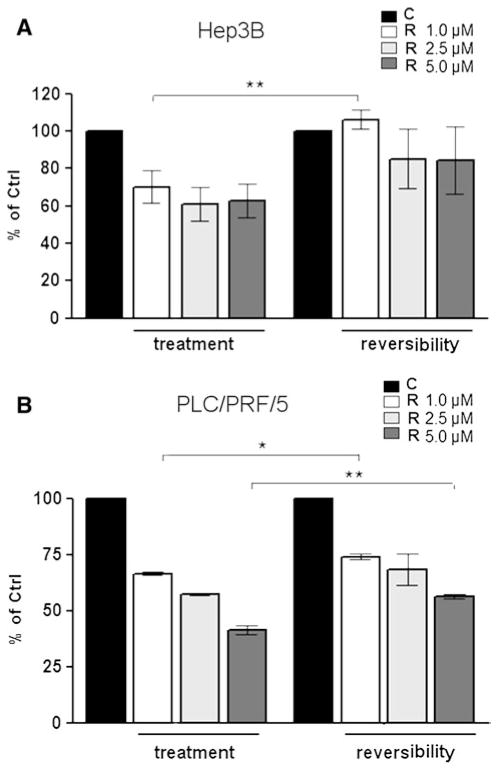
Recovery from regorafenib-mediated inhibition of cell invasion
An identical approach to recovery of cell invasion was taken, as for cell migration, but with slightly different results. After a 72 h exposure to different regorafenib concentrations, drug was removed from the growth medium and after 72 h of recovery, Hep3B and PLC/PRF/5 cells were then examined in invasiveness assay, using extra cellular matrix.
We found that Hep3B cells completely recovered their invasiveness properties after 1.0 μM treatment with drug, whereas the recovery was not complete (75 %) in PLC/PRF/5 cells. However, after a 5.0 μM drug treatment, complete recovery of invasiveness was not found in both cell lines (Fig. 5a, b).
Fig. 5.
Recovery of cell invasion after regorafenib treatment. Hep3B (a) and PLC/PRF/5 (b) cells were treated with different concentrations of regorafenib or vehicle. The first data set (called “treatment”) represents the percentage of the invading drug-treated cells compared to drug-untreated control cells, and the second one (called “reversibility”) represents the percentage of the invading recovered cells (after 72 h from drug removal) compared to drug-untreated control cells. C: vehicle, R: regorafenib. *P< 0.05, **P< 0.001
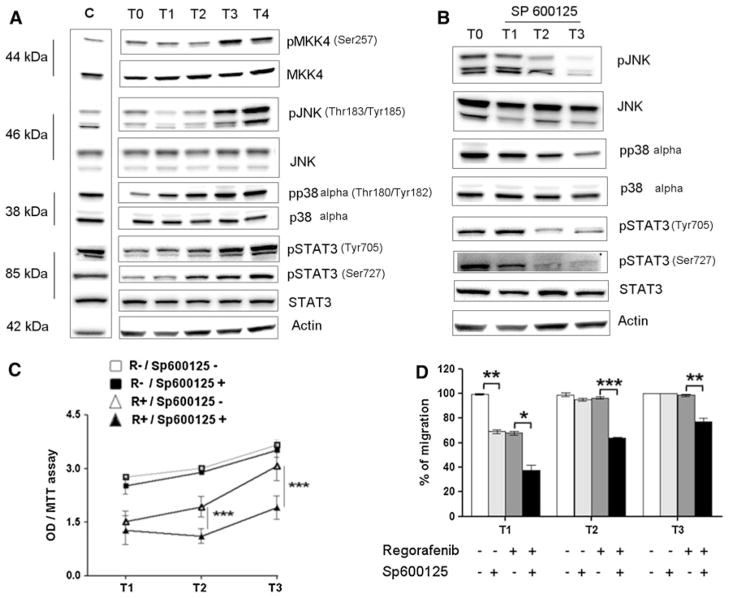
Mechanisms of growth recovery
Changes in MAPK pathway in Hep3B cells from T0 to T4 were analyzed by WB. Since pJNK levels are altered by regorafenib action [17], we examined its levels during growth recovery. We found that pJNK and pp38 levels were increased from T1 to T4. We then examined the common upstream and downstream kinases, and we found an increased levels of both pMKK4 (Ser257) and pSTAT3 (Tyr705, Ser727) from T1 to T4 (Fig. 6a). To test the significance of the pJNK (Thr183, Tyr185) changes, we used Sp600125 20 μM, a known JNK inhibitor, after exposure of Hep3B to regorafenib 5 μM for 72 h (T0). This treatment resulted in decreased pJNK (Thr183, Tyr185), pp38 (Thr180, Tyr182), and pSTAT3 (Ser727, Tyr705) levels at T1, T2, and T3 (Fig. 5b). Levels of p38, JNK, and STAT3 were not inhibited (Fig. 6b).
Fig. 6.
Mechanisms of cell growth and migration recovery in Hep3B cells. a Recovery of cells pre-treated with regorafenib 5 μM for 72 h. Phospho-JNK (pJNK) and pp38 levels were increased during reversibility (T1–T4), as were pMKK4 and pSTAT3 (Ser727 and Tyr705) levels, which are upstream and downstream of JNK, respectively. b To test the significance of pJNK changes, SP600125 (JNK inhibitor) 20 μM was used during reversibility. The inhibition of the induced increase in pJNK, pp38, and pSTAT3 (Ser727 and Tyr705) kinase levels (T1–T3) was observed. c, d Cell growth (C) and migration (D) during recovery (T1–T3). R− and R + represent the cells without and with regorafenib treatment (5 μM), respectively. Sp− and Sp + represent cells without or with JNK inhibitor treatment (20 μM), respectively. *P< 0.05, **P< 0.001, ***P< 0.0001
JNK inhibitor actions on recovery of cell growth and migration
Cells were then treated with regorafenib 5 μM for 72 h and, after growth inhibition, were allowed to recover for 3 days in the presence or absence of JNK inhibitor 20 μM. Recovery of growth was almost completely blocked by JNK inhibitor presence (Fig. 6c). Since the JNK inhibitor antagonized growth recovery after regorafenib release, we examined whether it would have similar effects on recovery of cell migration. The recovery of migration in regorafenib pre-treated cells was examined in the absence or presence of the JNK inhibitor, and the inhibitor was found to partially antagonize recovery of cell migration (Fig. 6d).
Apoptosis and autophagy processes in recovery
In a previous study [17], we have analyzed the autophagy and apoptosis in regorafenib-treated cell; here, we have evaluated some markers of these two processes. The results were then confirmed by TEM.
The recovery, after a treatment with regorafenib 5 μM for 72 h, showed an increase in anti-apoptotic markers (Bcl-xL and pBcl-2) and decrease in pro-apoptotic proteins (caspase-7, caspase-8) together with a decrease in pro-autophagy markers (Beclin-1 and LC3 II). Thus, reversibility was associated with anti-apoptotic and anti-autophagy effects (Fig. 1S). TEM showed that most cells in T0 (36.0 %) contained typical autophagic vacuoles in different stages of maturation and extensive mitochondrial swelling with disruption of cristae and large clumps of heterochromatin adjacent to the nuclear envelope, consistent with biochemical results.
During cell recovery, seemingly normal subcellular structures returned, and only 9.5 % of cells in T3 showed apoptotic and/or autophagy signs (Fig. 1S).
Discussion
Sorafenib clinical toxicities often result in dose reductions, dose delays, or even cessation of treatments [7–9, 20]. Regorafenib is a potent inhibitor of HCC growth, migration, and invasion, associated with early and transient suppression of pERK and delayed induction of pJNK levels, with biochemical evidence for induction of apoptosis and autophagy [18]. Even very low regorafenib concentrations for longer times could cause these events [19]. In the current study, we treated HCC cells in culture with growth-inhibitory concentrations of regorafenib and then observed the changes after drug removal. We found that growth recovered, as well as inhibition of migration and invasion. When the process was repeated by treating pre-treated and recovered cells with a second drug exposure, cells also recovered, but their growth was slower than non-pre-treated cells, suggesting residual drug effects.
We considered that the cells were possibly damaged by the first treatment. However, when we subcultured, pre-treated, and recovered cells several times, a second treatment followed by drug removal still resulted in a slower recovery. We interpreted this as signifying that there was some longer term cellular alteration from the initial drug exposure. We also noted a difference in cell sensitivity to inhibition of growth compared with inhibition of cell migration, as noted previously [19], since lower concentrations of regorafenib were needed for growth inhibition, compared with migration inhibition. At the concentrations of regorafenib needed to completely inhibit cell migration without subsequent recovery, inhibition of cell growth could still reverse.
These multikinase inhibitors are not considered to be cytocidal. We reasoned that drug removal from treated cells could result in recovery of cell growth and examined whether we could modulate or antagonize cell growth recovery, using agents previously shown to inhibit HCC cell growth, but at low concentrations.
Doxorubicin has a long use in HCC treatment [21]. We found concentrations that did not inhibit cell growth when used alone. We then exposed regorafenib pre-treated and recovering cells to these low doxorubicin concentrations and found that recovery of growth and migration could be substantially antagonized.
Since non-toxic vitamin K1 has been evaluated experimentally for its ability to inhibit HCC cell growth [23], we exposed regorafenib-recovering cells to a range of vitamin K1 concentrations and found that low concentrations of vitamin K1 that did not inhibit HCC cell growth when used alone could inhibit recovery of growth and migration. Sequential chemotherapies in HCC are previously reported [20].
Given the low response rates, but increased survival in sorafenib HCC clinical trials [5], several clinical studies of combinations, using sorafenib plus chemotherapy, are ongoing. Others have also noted reversibility of tumor cell growth after cessation of kinase inhibitor actions [15, 24].
We previously observed cell quiescence after regorafenib treatment in vitro [17]. The current study extends that to show that growth-inhibited cells can fully recover their growth after drug removal and suggests that long-term treatment might be needed for prolonged cancer control. These might involve use of chronic low regorafenib concentrations [19], or combinations of regorafenib, either with chemotherapies, or with agents targeting other pathways [25–27].
We evaluated possible mechanisms involved in growth reversibility and found increased levels of pJNK. We expected the opposite, because we previously found that regorafenib treatment caused a pJNK increase [17]. To confirm these new findings, we used a JNK inhibitor (SP600125) and found that it antagonized both growth recovery and associated increased pJNK. JNK has a dual function in the cell, in growth arrest/apoptosis, and in recovery from cell stress [28, 29].
Our experiments showed that JNK plays an important role in recovery of both growth and migration. Recent studies of cell migration showed that serine phosphorylation of paxillin was mediated by JNK and that p38 MAPK was crucial for this cellular process [30, 31].
MKK4 is an upstream kinase activator of JNK and p38. The p38 protein can induce growth arrest and/or apoptosis, as well as promote drug resistance and cell survival [32]. We found that pp38α and pMKK4 levels were increased, in addition to pJNK in the cell growth recovery. There is evidence for positive and negative cross talk between p38 and JNK signaling, depending on the cell type [33].
After our JNK inhibitor treatments, the cells had decreased pSTAT3 levels and unexpectedly p38 dephosphorylation. This highlights a possible relationship between JNK and p38 activity in the recovery of cell proliferation, suggesting that cells protect themselves from drug insult by STAT3 activation via the JNK and p38 pathways [34].
Apoptosis and autophagy are critical survival mechanisms in cellular responses to a variety of cytotoxic stimuli including drug treatments. We found increases in anti-apoptotic protein levels, with unchanged or decreased pro-apoptotic markers during reversibility, together with down-regulation of autophagic Beclin-1 and LC3 II.
Conclusions
Growth-inhibited cells can recover after regorafenib removal. This recovery can be modulated by low concentrations of drugs and involves JNK and p38 actions.
Supplementary Material
Acknowledgments
Grant support: This work was supported (in part) by NIH Grant [# 82723 (BIC)].
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s00280-013-2269-8) contains supplementary material, which is available to authorized users.
Contributor Information
Rosalba D’Alessandro, Laboratory of Biochemistry, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy.
Maria G. Refolo, Laboratory of Biochemistry, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy
Catia Lippolis, Laboratory of Biochemistry, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy.
Caterina Messa, Laboratory of Biochemistry, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy.
Aldo Cavallini, Laboratory of Biochemistry, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy.
Roberta Rossi, Department of Pathological Anatomy, Faculty of Medicine, University of Bari, Giulio Cesare Square, 70100 Bari, BA, Italy.
Leonardo Resta, Department of Pathological Anatomy, Faculty of Medicine, University of Bari, Giulio Cesare Square, 70100 Bari, BA, Italy.
Antonio Di Carlo, Clinical Pathology Laboratory, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy.
Brian I. Carr, Email: brianicarr@hotmail.com, Laboratory of Biochemistry, National Institute for Digestive Diseases, IRCCS “Saverio de Bellis”, Via Turi, 27, 70013 Castellana Grotte, BA, Italy
References
- 1.Ahmad T, Eisen T. Kinase inhibition with BAY 43-9006 in renal cell carcinoma. Clin Cancer Res. 2004;10:6388S–6392S. doi: 10.1158/1078-0432.CCR-040028. [DOI] [PubMed] [Google Scholar]
- 2.Cervello M, Bachvarov D, Lampiasi N, Cusimano A, Azzolina A, McCubrey JA, Montalto G. Molecular mechanisms of sorafenib action in liver cancer cells. Cell Cycle. 2012;11:2843–2855. doi: 10.4161/cc.21193. [DOI] [PubMed] [Google Scholar]
- 3.Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, Cao Y, Shujath J, Gawlak S, Eveleigh D, Rowley B, Liu L, Adnane L, Lynch M, Auclair D, Taylor I, Gedrich R, Voznesensky A, Riedl B, Post LE, Bollag G, Trail PA. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64:7099–7109. doi: 10.1158/0008-5472.CAN-04-1443. [DOI] [PubMed] [Google Scholar]
- 4.Liu L, Cao Y, Chen C, Zhang X, McNabola A, Wilkie D, Wilhelm S, Lynch M, Carter C. Sorafenib blocks the RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer Res. 2006;66:11851–11858. doi: 10.1158/0008-5472.CAN-06-1377. [DOI] [PubMed] [Google Scholar]
- 5.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J SHARP Investigators Study Group . Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 6.Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 7.Otsuka T, Eguchi Y, Kawazoe S, Yanagita K, Ario K, Kitahara K, Kawasoe H, Kato H, Mizuta T The saga liver cancer study group . Skin toxicities and survival in advanced hepatocellular carcinoma patients treated with sorafenib. Hepatol Res. 2012;42:879–886. doi: 10.1111/j.1872-034X.2012.00991.x. [DOI] [PubMed] [Google Scholar]
- 8.Edmonds K, Hull D, Spencer-Shaw A, Koldenhof J, Chrysou M, Boers-Doets C, Molassiotis A. Strategies for assessing and managing the adverse events of sorafenib and other targeted therapies in the treatment of renal cell and hepatocellular carcinoma: recommendations from a European nursing task group. Eur J Oncol Nurs. 2012;16:172–184. doi: 10.1016/j.ejon.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Porta C, Paglino C, Imarisio I, Bonomi L. Uncovering Pandora’s vase: the growing problem of new toxicities from novel anticancer agents. The case of sorafenib and sunitinib. Clin Exp Med. 2007;7:127–134. doi: 10.1007/s10238-007-0145-8. [DOI] [PubMed] [Google Scholar]
- 10.Wilhelm SM, Dumas J, Adnane L, Lynch M, Carter CA, Schütz G, Thierauch KH, Zopf D. Regorafenib (BAY 73-4506): a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int J Cancer. 2011;129:245–255. doi: 10.1002/ijc.25864. [DOI] [PubMed] [Google Scholar]
- 11.Strumberg D, Schultheis B. Regorafenib and cancer. Expert Opinion Invest Drugs. 2012;21:879–889. doi: 10.1517/13543784.2012.684752. [DOI] [PubMed] [Google Scholar]
- 12.Demetri GD, Reichardt P, Kang YK, Blay JY, Rutkowski P, Gelderblom H, Hohenberger P, Leahy M, von Mehren M, Joensuu H, Badalamenti G, Blackstein M, Le Cesne A, Schöffski P, Maki RG, Bauer S, Nguyen BB, Xu J, Nishida T, Chung J, Kappeler C, Kuss I, Laurent D, Casali PG GRID study investigators . Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295–302. doi: 10.1016/S0140-6736(12)61857-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grothey A, Cutsem EV, Sobrero A, Siena S, Falcone A, Ychou M, Humblet Y, Bouché O, Mineur L, Barone C, Adenis A, Tabernero J, Yoshino T, Lenz HJ, Goldberg RM, Sargent DJ, Cihon F, Cupit L, Wagner A, Laurent D CORRECT Study Group . Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–312. doi: 10.1016/S0140-6736(12)61900-X. [DOI] [PubMed] [Google Scholar]
- 14.Brahimi F, Rachid Z, Qiu Q, McNamee JP, Li YJ, Tari AM, Jean-Claude BJ. Multiple mechanisms of action of ZR2002 in human breast cancer cells: a novel combi-molecule designed to block signaling mediated by the ERB family of oncogenes and to damage genomic DNA. Int J Cancer. 2004;112:484–491. doi: 10.1002/ijc.20383. [DOI] [PubMed] [Google Scholar]
- 15.Mancuso MR, Davis R, Norberg SM, O’Brien S, Sennino B, Nakahara T, Yao VJ, Inai T, Brooks P, Freimark B, Shalinsky DR, Hu-Lowe DD, McDonald DM. Rapid vascular regrowth in tumors after reversal of VEGF inhibition. J Clin Invest. 2006;116:2610–2621. doi: 10.1172/JCI24612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steeghs N, Rabelink TJ, Op’t Roodt J, Batman E, Cluitmans FH, Weijl NI, de Koning E, Gelderblom H. Reversibility of capillary density after discontinuation of bevacizumab treatment. Ann Oncol. 2010;21:1100–1105. doi: 10.1093/annonc/mdp417. [DOI] [PubMed] [Google Scholar]
- 17.Carr BI, Cavallini A, Lippolis C, D’Alessandro R, Messa C, Refolo MG, Tafaro A. Fluoro-Sorafenib (Regorafenib) effects on hepatoma cells: growth inhibition, quiescence and recovery. J Cell Physiol. 2013;228:292–297. doi: 10.1002/jcp.24148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma SV, Lee DY, Li B, Quinlan MP, Takahashi F, Maheswaran S, McDermott U, Azizian N, Zou L, Fischbach MA, Wong KK, Brandstetter K, Wittner B, Ramaswamy S, Classon M, Settleman J. A chromatin-mediated reversible drug tolerant state in cancer cell subpopulations. Cell. 2010;141:69–80. doi: 10.1016/j.cell.2010.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carr BI, D’Alessandro R, Refolo MG, Iacovazzi PA, Lippolis C, Messa C, Cavallini A, Correale M, Di Carlo A. Effects of low concentrations of Regorafenib and Sorafenib on human HCC cell AFP, migration, invasion and growth in vitro. J Cell Physiol. 2013;228:1344–1350. doi: 10.1002/jcp.24291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ebos JM, Lee CR, Cruz-Munoz W, Bjarnason GA, Christensen JG, Kerbel RS. Accelerated metastasis after short-term treatment with a potent inhibitor of tumor angiogenesis. Cancer Cell. 2009;15:232–239. doi: 10.1016/j.ccr.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cao H, Phan H, Yang LX. Improved chemotherapy for hepatocellular carcinoma. Anticancer Res. 2012;32:1379–1386. [PubMed] [Google Scholar]
- 22.Varela M, Real MI, Burrel M, Forner A, Sala M, Brunet M, Ayuso C, Castells L, Montaná X, Llovet JM, Bruix J. Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J Hepatology. 2007;46:474–481. doi: 10.1016/j.jhep.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 23.Wei G, Wang M, Hyslop T, Wang Z, Carr BI. Vitamin K enhancement of Sorafenib-mediated HCC cell growth inhibition in vitro and in vivo. Int J Cancer. 2010;127:2949–2958. doi: 10.1002/ijc.25498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paraiso KH, Fedorenko IV, Cantini LP, Munko AC, Hall M, Sondak VK, Messina JL, Flaherty KT, Smalley KS. Recovery of phospho-ERK activity allows melanoma cells to escape from BRAF inhibitor therapy. Br J Cancer. 2010;102:1724–1730. doi: 10.1038/sj.bjc.6605714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gedaly R, Angulo P, Chen C, Creasy KT, Spear BT, Hundley J, Daily MF, Shah M, Evers BM. The role of PI3 K/mTOR inhibition in combination with sorafenib in hepatocellular carcinoma treatment. Anticancer Res. 2012;32:2531–2536. [PubMed] [Google Scholar]
- 26.Ibrahim N, Yu Y, Walsh WR, Yang JL. Molecular targeted therapies for cancer: sorafenib mono-therapy and its combination with other therapies. Oncol Rep. 2012;27:1303–1311. doi: 10.3892/or.2012.1675. [DOI] [PubMed] [Google Scholar]
- 27.Kudo M. Targeted therapy for liver cancer: updated review in 2012. Curr Cancer Drug Targets. 2012;12:1062–1072. [PubMed] [Google Scholar]
- 28.Garlick DS, Greiner DL, Davis RJ. The role of JNK in the development of hepatocellular carcinoma. Genes Dev. 2011;25:634–636. doi: 10.1101/gad.1989311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bode AM, Dong Z. The functional contrariety of JNK. Mol Carcinog. 2007;46:591–598. doi: 10.1002/mc.20348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee YC, Chang AY, Lin-Feng MH, Tsou WI, Chiang IH, Lai MZ. Paxillin phosphorylation by JNK and p38 is required for NFAT activation. Eur J Immunol. 2012;42:2165–2175. doi: 10.1002/eji.201142192. [DOI] [PubMed] [Google Scholar]
- 31.Zhang YH, Wang SQ, Sun CR, Wang M, Wang B, Tang JW. Inhibition of JNK1 expression decreases migration and invasion of mouse hepatocellular carcinoma cell line in vitro. Med Oncol. 2011;28:966–972. doi: 10.1007/s12032-010-9568-2. [DOI] [PubMed] [Google Scholar]
- 32.Ranganathan AC, Zhang L, Adam AP, Aguirre-Ghiso JA. Functional coupling of p38-dependent protein kinase-like endoplasmatic reticulum kinase to drug resistance of dormant carcinoma cells. Cancer Res. 2006;66:1702–1710. doi: 10.1158/0008-5472.CAN-05-3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wagner EF, Nebreda AR. Signal integration by JNK and p38 MAPK pathway in cancer development. Nature Rev Cancer. 2009;9:537–549. doi: 10.1038/nrc2694. [DOI] [PubMed] [Google Scholar]
- 34.Kim JH, Lee SC, Ro J, Kang HS, Kim HS, Yoon S. Jnk signaling pathway-mediated regulation of Stat3 activation is linked to the development of doxorubicin resistance in cancer cell lines. Biochem Pharmacol. 2010;79:373–380. doi: 10.1016/j.bcp.2009.09.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.