Abstract
Objectives:
Discharge against medical advice (DAMA) is a major problem in healthcare delivery as it can complicate the health problems from which patients are suffering. The aim of this study was to understand DAMA among children in a tertiary teaching hospital in Oman and to evaluate the documentation of the events in the medical records.
Methods:
A retrospective survey of the medical records of patients discharged against medical advice over a two-year interval was performed (2004–2006).
Results:
Of the 11,802 admissions, there were 38 cases of DAMA, giving a prevalence rate of 0.32%. In 39.5% of the cases, the discharge happened within 24 hours of hospital admission. The majority of the cases were infants (n = 24; 63.25%). The diagnosis at discharge in some cases included life-threatening conditions. However, in 57.9% of the cases, the reasons for DAMA were neither reported nor documented in the patients’ medical records.
Conclusion:
Although the results of this study yielded a low prevalence rate compared to the rates reported in other studies, the occurrence of DAMA for children in a tertiary hospital is a distressing phenomenon. It was evident that the documentation of the DAMA process was poor. More studies should be conducted to understand the details of the problem. Policies should be established and implemented in order to attempt to reduce DAMA among child patients and to protect them from the consequences of such discharges.
Keywords: Children, Patient Discharge, Hospitals, Oman
Advances in Knowledge
- This is the first study in Oman that highlights discharge against medical advice (DAMA) among children. This study identified that, in Oman, DAMA occurs more frequently among children younger than 3 years old and that the majority happens within a week of admission. It also reveals the seriousness of some of the health conditions that children are suspected of having at the time of DAMA.
Application to Patient Care
- This study highlights the need for proper documentation of the occurences of DAMA.
- The results of this study also indicate the need to implement policies to control DAMA, especially in children with life-threatening health conditions.
Discharge against medical advice (DAMA) happens when a patient (or the parents or caregivers, in the case of a young patient) decides the timing of the discharge without a treating doctor’s approval. The clinical, ethical and legal implications of DAMA are a major problem for doctors. DAMA is reported among adults and has also been reported in younger patients.1–6 In children, the decision to undertake DAMA is a liability for the care provider and can have immediate or long-term health consequences for the child.
The prevalence rate of DAMA is estimated to be around 1% in most studies, but has been reported to reach up to 25.85% in other studies.3–5,7,8 In one study, DAMA was mainly reported among children aged under one year, followed by children aged 1–5 years.9 One alarming trend is that even critically ill children with life-threatening complications were reported to have been discharged against medical advice.3,5,10 Perceived improvement, financial problems and the parents’ dissatisfaction with the care provided are some of the reasons that parents often claim to justify the DAMA of a child.11
DAMA can endanger the patient’s life and could further complicate the patient’s clinical outcome. It could also result in readmissions with longer hospital stays, prolonged illness and ultimately lead to higher costs of care.12–14
The problem of DAMA has been reported in different countries worldwide.1–6 However, this subject has rarely been studied in Arab countries, much less in Oman. DAMA is an important issue to address; thus, the associated factors, reasons and outcomes of DAMA must be recognised and possible solutions must be determined. This study will describe the prevalence rate, and the clinical and sociodemographic factors of paediatric DAMA at Sultan Qaboos University Hospital (SQUH), Oman.
Methods
This was a retrospective descriptive study on paediatric DAMA in SQUH, a tertiary teaching hospital attached to the College of Medicine & Health Sciences at Sultan Qaboos University, Muscat, Oman. During the study period, SQUH was a 649-bed hospital with 4 paediatric wards consisting of 115 beds, among other wards and specialties. The study was based on paediatric patients who left the hospital against medical advice over a two-year period (July 2004–June 2006). Ethical approval for the study was obtained from the Sultan Qaboos University (SQU) College of Medicine & Health Sciences, Medical Ethics & Research Committee (MREC #259). Cases were identified from the ward registry books which contain basic information about patient demographics and the modes of admission and discharge. All medical files and available discharge summaries of DAMA during the study period were reviewed. The following information was collected from patients’ medical records: date of birth, admission, DAMA, diagnosis at discharge and other social factors (age of parents, education and working status of parents, and number of siblings). The number of admissions and discharges in the paediatric wards during the study period were collected from the computerised hospital information system. Due to the small number of cases, a simple descriptive analysis using the Statistical Package for the Social Sciences (SPSS), Version 19 (IBM, Corp., Chicago, Illinois, USA) was used to present the data (frequency tables and graphs, mean and median of continuous data). Further statistical analysis was not possible; hence, no correlation could be construed.
Results
A review of the ward registry books identified a total of 44 cases of DAMA during the study period. During the same interval, a total of 11,802 discharges were reported from all paediatric wards. After reviewing the medical records of the identified patients, only 38 cases had detailed information in their medical records about the cause of the DAMA. On the other hand, DAMA could not be confirmed from the medical records in the remaining 6 cases, and they were hence excluded from the study. Thus, the rate of DAMA was 0.32%.
Female patients comprised 60.5% (n = 23) of the discharged patients, and almost all the study patients were Omani (n = 35; 92.1%). The duration of admission ranged from a few hours to 36 days, with a median of two days (interquartile range = 4.25 days) [Table 1]. The majority of cases of DAMA were infants (n = 24; 63.2%) with an age range of one day to 12 years, with the median age being one month (first quartile 6 days and third quartile 3 years) [Table 1].
Table 1:
Age of patient and duration of admission before discharge against medical advice
| Characteristics | Total (n = 38) n (%) |
|---|---|
| Age of child | |
| 1–30 days | 19 (50) |
| 1–12 months | 5 (13.1) |
| 13 months–3 years | 8 (21) |
| 4–6 years | 2 (5.3) |
| 7–10 years | 2 (5.3) |
| 11–12 years | 2 (5.3) |
| Duration of admission in days | |
| 1 | 15 (39.5) |
| 2–5 | 15 (39.5) |
| 6–10 | 4 (10.5) |
| 11–36 | 4 (10.5) |
Other demographic factors concerning the parents were missing from the files for most of the patients, and thus were not reported. The diagnosis/symptoms varied among the study cases [Table 2]. Some of the patients were discharged against medical advice with life-threatening health conditions such as septicaemia, acute abdomen pain and inflammatory diseases of the central nervous system. While some patients exhibited a number of health problems, this was mainly observed among the neonatal group. Furthermore, only two patients were known to have chronic diseases (rheumatoid arthritis and immunodeficiency), while 28 (73.7%) did not have any chronic diseases; however, it was not possible to confirm or exclude the presence of chronic diseases at the time of DAMA from the health records in 8 patients (21.1%).
Table 2:
Diagnosis upon discharge against medical advice
| Diagnosis | n (%) |
|---|---|
| Life-threatening diseases | |
| Septicaemia | 6 (15.8) |
| Immunodeficiency | 2 (5.3) |
| Hypoglycaemia | 1 (2.6) |
| Inflammatory diseases of the central nervous system | 4 (10.5) |
| Convulsion, cerebellar ataxia | 2 (5.3) |
| Acute abdomen pain, inguinal hernia | 3 (7.9) |
| Diarrhoea and gastroenteritis of presumed infectious origin | 3 (7.9) |
| Poisoning by drugs | 1 (2.6) |
| Other diseases | |
| Acute bronchitis, bronchopneumonia | 5 (13.2) |
| Failure to thrive | 1 (2.6) |
| Jaundice | 2 (5.3) |
| Urinary tract infection | 1 (2.6) |
| Anaemia | 2 (5.3) |
| Visceral leishmaniasis | 1 (2.6) |
| Gastroesophageal reflex | 1 (2.6) |
| Prematurity | 6 (15.8) |
The data showed that 11 cases (28.9%) were admitted through the emergency room; two (5.3%) were admitted through the hospital’s outpatient clinic; 8 cases (21.1%) were referred from other health institutions; two (5.2%) were booked admissions, and 10 (26.3%) were referred from the SQUH postnatal ward. For 5 cases (13.2%), it was not possible to identify the source of admission from the medical records.
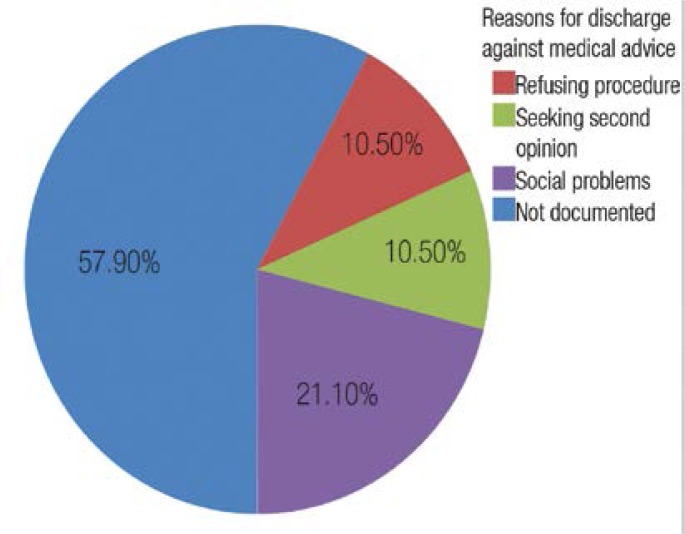
The reasons for DAMA were not documented in 57.9% of the studied cases; for the rest of the cases however, the care provider reported alleged justifications for the DAMA in the patients’ hospital records, as illustrated in Figure 1.
Figure 1:
Reasons for discharge against medical advice.
Discussion
This was a descriptive study conducted to assess the number and types of cases of DAMA in a tertiary teaching hospital in Oman. To our knowledge, this is the first study of this type highlighting DAMA among minors in Oman. Although this study presented retrospective data from approximately 6 years ago, this study constituted the groundwork for more comprehensive research utilising a prospective approach. DAMA is an existing problem among paediatric patients and it is more common among infants; this is a finding which has been similarly reported in other studies.9 The study shows that most DAMA patients were neonates; this is an alarming observation considering the possible complications and subtle symptoms that can affect this particular patient group. The diagnosis/symptoms at discharge were startling in some cases.
As with other studies, this study found a slightly higher rate of DAMA among female patients. It is difficult to explain this finding given the current study design.7 The issue of gender discrimination may be considered; however, it is unlikely to be the reason since gender discrimination is not so pervasive in Oman, as for instance, there are no major differences in school enrolment between boys and girls.15
The majority of patients discharged against medical advice had acute problems but did not exhibit chronic diseases. Whether the parents of children with chronic diseases are more adjusted and tolerant to hospitalisation needs to be considered. Moreover, around two-thirds of the study’s patients were discharged against medical advice within 5 days (40% within 24 hrs) with a median of 2 days; this is slightly longer compared to other studies which reported the mean duration of hospital stay to be 3.1 days.7 Healthcare is free for Omani citizens; thus, it is less likely to contribute to the decision of DAMA. However, the financial burden of admissions (such as transportation, losing working days and the arrangement of alternative care for other children) should be considered as possible rationales for DAMA.
The explanations that parents gave for the DAMA of a child was usually related to a medical management plan, such as the refusal of a procedure, while others stated “seeking a second opinion” to be the main reason. In such circumstances, it is important to consider the healthcare characteristics that could contribute to DAMA (for example, trust, communication barriers or satisfaction with the care provided). The fact that there are few other governmental tertiary care hospitals in Oman makes the availability of local options for a second opinion very limited.
There is a need to conduct prospective studies on DAMA to assess the reasons behind such discharges. Other studies have reported financial problems, parents’ perceptions of a child’s medical improvement, a cultural belief in seeking traditional therapies and dissatisfaction with the care provided by the treating team as the main causes of DAMA.16,17 In 21.1% of the cases in this study, the documented reasons for DAMA were related to social factors without specifying the details. Some of the possible reasons could be arranging care for other children at home, transportation from different regions and the work commitments of the parents. It would be useful to define such reasons and try to find solutions for such problems through the available governmental institutions, such as the Ministry of Social Development.
The fact that the reason for DAMA was not documented in the patients’ medical files in 57.9% of cases is of profound legal, ethical and medical importance. In many cases, the effort of the treating team to prevent such discharges was not documented. What is more worrying is that 6 cases were reported in the ward registry books as DAMA, but no other details pertaining to DAMA were recorded in the patients’ medical files. Similar poor documentation practices on standardised DAMA forms have been reported in other studies.18 Documentation in patients’ medical records is usually the responsibility of junior doctors, and assuring their proper documentation of DAMA is a necessity.
Due to the retrospective nature of this study, one of the limitations is that it was difficult to control for the quality of data collected and for missing data. The second limitation has to do with conducting the study in a single health institute, which resulted in a small sample size and an inability to generalise the results. The third limitation is that no information about the prognosis and eventual outcome of the patients was available. Finally, it would be important to collect more recent data, and this obviously constitutes one of the important limitations of this study. Therefore, a future study could expand the time period studied as well as include a more recent dataset. Similarly, in order to circumvent the present limitation, a prospective study would be an added asset so that evidence-based groundwork for informed policy might be contemplated.
Conclusion
DAMA is an existing problem in tertiary care hospitals in Oman, and infants are the most common victims. The discharge diagnoses in some patients were fatal and the children’s lives or health outcomes could have been placed at risk. It is also apparent that the amount of information reported in the medical records for the DAMA episodes in some cases was incomplete. It is a fundamental right of every child to receive healthcare; hence, DAMA deprives a child of this right. In cases of DAMA, suboptimal healthcare is provided instead. This is a violation of the child’s rights, and the parent’s authority over a child needs to be considered when a child’s welfare is at risk of being negatively affected.
Considering the size of this problem in a tertiary hospital, an assessment of the magnitude of the problem in secondary hospitals and primary health services should be considered. The impact of this problem on children and health services needs to be thoroughly examined. Actions should be taken to control life-threatening DAMA, and serious efforts should be implemented as stated to ensure the child’s right to receive appropriate healthcare. We recommend ensuring that more details concerning DAMA be included in patients’ hospital records for medico-legal reasons. Ideally, the discharging doctor should complete specific forms detailing the patient’s medical information, factors contributing to discharge, the process of counselling and an explanation of the risks involved in such a discharge. Finally, we advocate a prospective study in more health institutes to evaluate and provide more information about the factors contributing to DAMA and the outcome of DAMA among children in Oman.
References
- 1.Seaborn Moyse H, Osmun WE. Discharges against medical advice: A community hospital’s experience. Can J Rural Med. 2004;9:148–53. [PubMed] [Google Scholar]
- 2.Akpede GO. Presentation and outcome of sporadic acute bacterial meningitis in children in the African meningitis belt: Recent experience from northern Nigeria highlighting emergent factors in outcome. West Afr J Med. 1995;14:217–26. [PubMed] [Google Scholar]
- 3.Okoromah CN, Egri-Qkwaji MT. Profile of and control measures for paediatric discharges against medical advice. Niger Postgrad Med J. 2004;11:21–5. [PubMed] [Google Scholar]
- 4.Aliyu ZY. Discharge against medical advice: Sociodemographic, clinical and financial perspectives. Int J Clin Pract. 2002;56:325–7. [PubMed] [Google Scholar]
- 5.Gloyd S, Koné A, Victor AE. Pediatric discharge against medical advice in Bouaké Cote d’Ivoire, 1980–1992. Health Policy Plan. 1995;10:89–93. doi: 10.1093/heapol/10.1.89. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Pub Health. 2007;97:2204–8. doi: 10.2105/AJPH.2006.100164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Onyiriuka AN. Discharge of hospitalized under-fives against medical advice in Benin City, Nigeria. Niger J Clin Pract. 2007;10:200–4. [PubMed] [Google Scholar]
- 8.Parkash J, Das N. Pattern of admissions to neonatal unit. J Coll Physicians Surg Pak. 2005;15:341–4. [PubMed] [Google Scholar]
- 9.Hong LE, Ling FC. Discharges of children from hospital against medical advice. J Singapore Paediatr Soc. 1992;34:34–8. [PubMed] [Google Scholar]
- 10.Mahadi, Pasaribu S, Lubis M, Lubis CP. Acute hepatitis at the Department of Pediatrics, School of Medicine, University of North Sumatra/Dr Pirngadi Hospital Medan. Paediatr Indones. 1991;31:145–9. [PubMed] [Google Scholar]
- 11.Roodpeyma S, Hoseyni SAE. Discharge of children from hospital against medical advice. World J Pediatr. 2010;6:353–6. doi: 10.1007/s12519-010-0202-3. [DOI] [PubMed] [Google Scholar]
- 12.Choi M, Kim H, Qian H, Palepu A. Readmission rates of patients discharged against medical advice: A matched cohort study. PloS One. 2011;6:e24459. doi: 10.1371/journal.pone.0024459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): Risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25:926–9. doi: 10.1007/s11606-010-1371-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pennycook AG, McNaughton G, Hogg F. Irregular discharge against medical advice from the accident and emergency department--A cause for concern. Arch Emerg Med. 1992;9:230–8. doi: 10.1136/emj.9.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United Nations Educational, Scientific, and Cultural Organization Institute for Statistics Literacy Statistics. From: http://stats.uis.unesco.org/unesco/TableViewer/document.aspx?ReportId=121&IF_Language=eng&BR_Country=5800&BR_Region=40525</eref> Accessed: Feb 2012.
- 16.Onukwugha E, Saunders E, Mullins CD, Pradel FG, Zuckerman M, Weir MR. Reasons for discharges against medical advice: A qualitative study. Qual Saf Health Care. 2010;19:420–4. doi: 10.1136/qshc.2009.036269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macrohon BC. Pediatrician’s perspectives on discharge against medical advice (DAMA) among pediatric patients: A qualitative study. BMC Pediatr. 2012;18:12. doi: 10.1186/1471-2431-12-75. :75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reinke DA, Walker M, Boslaugh S, Hodge D. Predictors of pediatric emergency patients discharged against medical advice. Clin Pediatr (Phila) 2009;48:263–70. doi: 10.1177/0009922808323109. [DOI] [PubMed] [Google Scholar]