Abstract
Objectives To identify sinuses demonstrating postoperative radiographic mucosal thickening after endoscopic exposure of the cranial base through the transsphenoidal corridor.
Design Retrospective review.
Setting University-based medical center.
Participants Patients undergoing endoscopic transnasal transsphenoidal approaches to the skull base who had both preoperative and postoperative imaging.
Main Outcome Measures Change in preoperative and postoperative imaging scores for each sinus and side at 3 and 6 months. The left-sided undissected sinuses served as internal controls for comparison.
Results Fifty-one patients were identified with the aforementioned inclusion and exclusion criteria. The mean difference in preoperative and postoperative imaging scores for the right anterior ethmoid sinus was significantly different from the left-sided equivalents (p = 0.0020). The difference in the frontal sinuses approached significance (p = 0.0625).
Conclusions Resection of the lower half of the middle turbinate and maxillary antrostomy and harvest of a nasoseptal flap are associated with an increased radiographic incidence of mucosal thickening of the ipsilateral anterior ethmoids compared with the undissected contralateral side. When accessing the transnasal transsphenoidal corridor for skull base surgery, preservation of native anatomy is associated with a lower incidence of mucosal thickening on postoperative imaging.
Keywords: endoscopic skull base, middle turbinate, sinusitis, maxillary sinus, radiographic
Introduction
The purely endoscopic transnasal transsphenoidal (ETNTS) surgical approach to the cranial base has greatly increased in popularity since its first description in the 1990s.1 2 ETNTS offers comparable short-term resection outcomes when compared with more traditional approaches and microscopic approaches.3 Endoscopic approaches also carry less morbidity with faster recovery times.4 However, we have previously presented the clinical sinonasal consequences of this approach, including persistently elevated postnasal discharge5 and reduced sinonasal quality of life. The long-term sinonasal consequences of the disruption of the normal anatomy for an endoscopic transnasal transsphenoidal approach to the skull base are still not well understood.
Partial resection of one or both of the middle turbinates has been described to provide improved visualization and surgical access to the transsphenoidal skull base.6 The middle turbinates are known to affect sinonasal physiology, including olfaction,7 humidification, nasal airway resistance, and sensation of nasal airway resistance.8 In addition, the role of the middle turbinate in the ostiomeatal complex and the functioning of the frontal, maxillary, and anterior ethmoid sinuses are inherently linked by their anatomic relationships. The consequences of a partially resected middle turbinate are controversial but have been investigated in the context of inflammatory sinus disease.9 10 There is a theoretical risk of lateralization and obstruction of the frontal recess,11 loss of an important surgical landmark, risk of atrophic rhinitis, crusting, and bleeding. In addition, the need for middle turbinate resection to achieve adequate visualization may be overstated.12 Similarly, a large maxillary antrostomy can be used to facilitate storage and protection of a raised nasoseptal flap during surgery. The goal of this study is to radiographically characterize the sinonasal consequences of the surgical approach to the skull base in an effort to better understand the morbidity associated with endoscopic transsphenoidal surgery. Specifically, we seek to characterize the radiographic consequences of resection of the middle turbinate, performance of a maxillary antrostomy, and harvest of the nasoseptal flap.
Methods
Our retrospective study was approved by the institutional review board of the University of California at Los Angeles, and the requirement for informed consent was waived. Our study was Health Insurance Portability and Accountability Act compliant.
All consecutive patients who underwent an endoscopic transnasal transsphenoidal approach to the skull base were identified through operative logs of a two-surgeon team, composed of two otolaryngologists (MBW and JDS) and a neurosurgeon (MB), from August 2007 to June 2011. This approach included resection of the lower half of the right middle turbinate (for improved access), raising of a right-sided nasoseptal flap, a right-sided maxillary antrostomy in which to house the flap, and bilateral posterior ethmoidectomies with marsupialization of the sphenoid sinuses. In cases of a significant cerebrospinal fluid (CSF) leak, an abdominal fat graft was harvested and bolstered by the nasoseptal flap. Packing consisted of Nasopore sponges (Stryker, Kalamazoo, Michigan, USA), and in cases of a significant CSF leak requiring an abdominal fat graft, the closure was bolstered with petrolatum-impregnated gauze strips removed on postoperative day 3 to 5. Postoperative care included twice daily nasal saline irrigation, antibiotics, and regular in-office sinus debridement.
All patients had preoperative magnetic resonance imaging (MRI), with a follow-up postoperative MRI at a minimum of 3 months postoperatively for tumor surveillance. Lesions addressed through only a transsphenoidal approach with partial resection of a right middle turbinate, right maxillary antrostomy, and harvest of a right nasoseptal flap—as confirmed by both operative report and postoperative imaging—were included in the study group. A 3-month postoperative follow-up time allows for remucosalization of large mucosal defects13 while also optimizing the sample size. Furthermore, a post hoc subset analysis was also performed on patients with 6-month follow-up scans to confirm 3-month findings. Additionally, it has been shown that quality-of-life findings after endoscopic sinus surgery stabilize 6 months after surgery.14 Patients with a history of chronic rhinosinusitis, a history of prior sinus or skull base surgery, or septal or turbinate surgery were excluded. In addition, patients who underwent resection of bilateral middle turbinates, a left middle turbinate, no turbinate, or who had intervention beyond a transsphenoidal approach were also excluded.
A Lund-Mackay analog (LMA) score was developed to grade mucosal thickening to MRI and applied to all imaging. In the LMA scoring system, a score of 0 was defined as normal mucosa without any thickening, a score of 2 was assigned to any sinus with complete opacification, and a score of 1 was given to sinuses demonstrating any mucosal thickening without complete opacification (Fig. 1). For each subject, contralateral sinuses were used as controls by comparing the preoperative and postoperative imaging score of each right-sided sinus with the corresponding left-sided (unresected middle turbinate) sinus. Patient age, gender, and time from surgical intervention to last available postoperative scan were also included in the review to assess their potential influence on postoperative imaging.
Fig. 1.
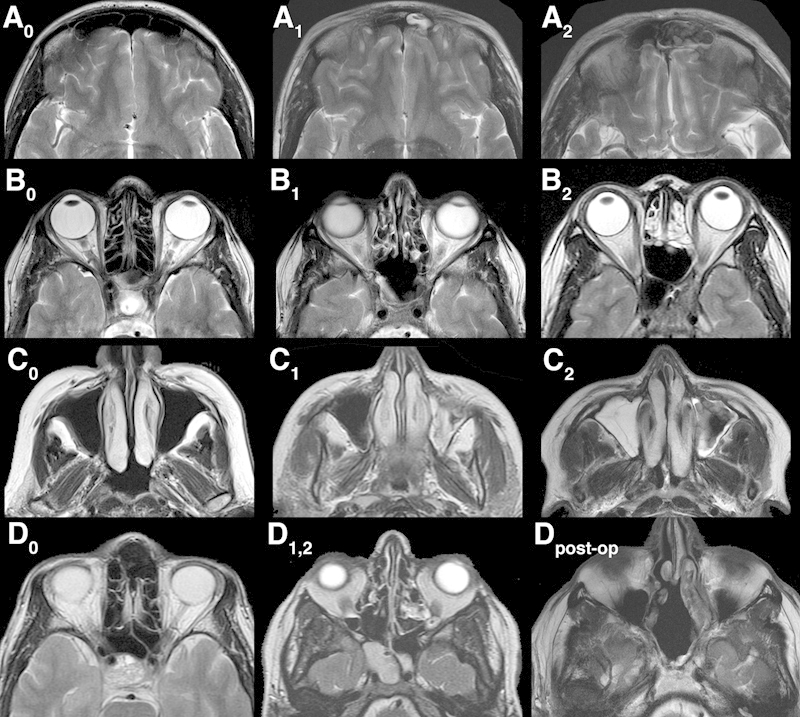
Examples of the Lund-Mackay analog (LMA) scoring system used to grade mucosal thickening of the paranasal sinuses on magnetic resonance imaging (MRI). Each sinus was assigned a score from 0, 1, or 2, with 0 defined as no mucosal thickening, 1 as any mucosal thickening but not completely opacified, and 2 as complete opacification. Rows A, B, C, and D show examples of opacification LMA scores for the frontal, ethmoid, maxillary, and sphenoid sinuses, respectively. Row D shows a score of 0 (D0), a left sphenoid with a score of 1, and a right sphenoid with a score of 2 (D1,2). Also included is a postoperative example of the sphenoids, which becomes a common cavity during a transsphenoidal approach. In this case, left- and right-sidedness was determined by the midline. In Dpost-op, this image received a 0 for no mucosal thickening on the right sphenoid and a 1 for mucosal thickening of the left side.
Statistical Analysis
The postoperative and preoperative LMA scores were compared using the Wilcoxon signed-rank test by sinus location and side. In addition, we computed the change in imaging score at each sinus location and side after ETNTS:
Δ LMA is defined over the range of (-2, 2) where -2 represents resolution of preoperative radiographic sinus opacification after surgery and 2 represents a normal sinus preoperatively developing complete radiographic opacification after surgery. We then compared the Δ LMA of each right-sided sinus to the corresponding left-sided sinus, also using the Wilcoxon signed-rank test. Odds ratios for the effect of middle turbinate resection on radiographic evidence of sinus disease were also calculated for each sinus.
To assess the potential impact of gender, age, and time to postoperative scan on sinus disease worsening after ETNTS, we used the general estimating equations (GEE) logistic model using Δ LMA as the dependent variable and side (right and left), sinus location, gender, age, and time to postoperative scan as the independent variables. The above GEE model takes into account that observations within the same patient are correlated. To determine whether the differences in sinus disease worsening between the two sides significantly varied by gender, age, time to postoperative scan, or location, the above model also allowed for interactions between side versus each of the other factors by including the appropriate interaction terms in the model. Interaction effects were tested using a p < 0.05 level of significance.
A post hoc power calculation was performed to determine if our study was capable of detecting a difference between the left and right frontal sinuses. A subset analysis was also performed on patients with imaging obtained greater than 6 months postoperatively to ensure that the findings at 3 months were sustained. All calculations were done using SAS version 0.2 (copyright 2002 to 2008 by SAS Institute Inc., Cary, North Carolina, USA).
Results
A total of 51 patients were identified who met the aforementioned inclusion and exclusion criteria. Table 1 shows the descriptive summary statistics of the study sample. Table 2 demonstrates the frequencies of the preoperative and postoperative LMA scores by sinus and side, as well as the distribution of calculated change of LMA scores in individual sinuses; p values reported are the result of comparing preoperative and postoperative distributions of LMA scores. As demonstrated in Table 2, there was a difference beyond chance in the preoperative and postoperative LMA scores in the right anterior ethmoids (p = 0.0074), right maxillary sinus and right sphenoid sinus (p = 0.0065 and 0.0078, respectively), and the left maxillary and sphenoid sinus (p = 0.0391 and 0.0469, respectively).
Table 1. Descriptive characteristics of the study sample.
| Characteristic | TNTS patients |
|---|---|
| No. | 51 |
| Female gender | 36 (71%) |
| Age (years) | |
| Min | 19 |
| Median | 51 |
| Max | 81 |
| Time to postoperative scan (weeks) | |
| Min | 14 |
| Median | 32 |
| Max | 145 |
Abbreviation: TNTS, transnasal transsphenoidal surgical.
Table 2. Pre and postoperative change in Lund-MacKay Analog Scores by sinus.
| Right side | Left side | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sinus | LMA score | Pre-op (%) | Post-op (%) | Δ LMA | Frequency (%) | P value | LMA score | Pre-op (%) | Post-op (%) | Δ LMA | Frequency (%) | P value |
| Frontal | 0 | 100.0 | 92.2 | -2 | – | 0.1250 | 0 | 98.0 | 100.0 | -2 | – | 0.9999 |
| 1 | – | 5.9 | -1 | – | 1 | 2.0 | – | -1 | 2.0 | |||
| 2 | – | 2.0 | 0 | 92.2 | 2 | – | – | 0 | 98.0 | |||
| 1 | 5.9 | 1 | – | |||||||||
| 2 | 2.0 | 2 | – | |||||||||
| Anterior ethmoid | 0 | 90.2 | 68.6 | -2 | – | 0.0074 | 0 | 90.2 | 88.2 | -2 | – | 0.9999 |
| 1 | 9.8 | 31.4 | -1 | 3.9 | 1 | 9.8 | 11.8 | -1 | 7.8 | |||
| 2 | – | – | 0 | 70.6 | 2 | – | – | 0 | 82.4 | |||
| 1 | 25.5 | 1 | 9.8 | |||||||||
| 2 | – | 2 | – | |||||||||
| Maxillary | 0 | 84.3 | 60.8 | -2 | – | 0.0065 | 0 | 90.2 | 78.4 | -2 | – | 0.0391 |
| 1 | 15.7 | 37.3 | -1 | 5.9 | 1 | 9.8 | 19.6 | -1 | 2.0 | |||
| 2 | – | 2.0 | 0 | 64.7 | 2 | – | 2.0 | 0 | 82.4 | |||
| 1 | 27.5 | 1 | 15.7 | |||||||||
| 2 | 2.0 | 2 | – | |||||||||
| Posterior ethmoid | 0 | 96.1 | 84.3 | -2 | 2.0 | 0.1719 | 0 | 94.1 | 94.1 | -2 | – | 0.3984 |
| 1 | 2.0 | 11.8 | -1 | 2.0 | 1 | 5.9 | 5.9 | -1 | 5.9 | |||
| 2 | 2.0 | 3.9 | 0 | 80.4 | 2 | – | – | 0 | 82.4 | |||
| 1 | 11.8 | 1 | 9.8 | |||||||||
| 2 | 3.9 | 2 | 2.0 | |||||||||
| Sphenoid | 0 | 100.0 | 84.3 | -2 | – | 0.0078 | 0 | 98.0 | 86.3 | -2 | – | 0.0469 |
| 1 | – | 11.8 | -1 | – | 1 | 2.0 | 7.8 | -1 | 2.0 | |||
| 2 | – | 3.9 | 0 | 84.3 | 2 | – | 5.9 | 0 | 84.3 | |||
| 1 | 11.8 | 1 | 7.8 | |||||||||
| 2 | 3.9 | 2 | 5.9 | |||||||||
Abbreviations: Δ LMA, postoperative LMA score - preoperative LMA score; LMA, Lund-Mackay analog.
The change in LMA scores in the right-sided sinuses was then compared with the change of LMA score in the left-sided sinuses. Table 3 displays the mean change in sinus by site and side, as well as the odds ratio for effect of side on LMA. The right anterior ethmoid sinuses demonstrated a statistically significant difference from the left side (p = 0.0020). Similarly, the odds of having sinus disease worsening on the right side compared with the left side in the anterior ethmoids and maxillary sinus was 3.15 (1.45, 6.80). The change in LMA scores between the left and right frontal sinuses approached statistical significance (p = 0.0625). However, a sample size of 51 patients (right-left pairs) achieves only 59% power to detect this difference at p < 0.05 using the above test. An odds ratio could not be calculated, as there was no worsening of left-sided frontal sinuses and therefore the odds ratio tends to infinity.
Table 3. Mean pre and postoperative change in Lund-MacKay Analog Scores by side.
| Right side | Left side | ||||
|---|---|---|---|---|---|
| Sinus | μ Δ LMA | μ Δ LMA | P value | OR (Lower CI, Upper CI) | P value |
| Frontal | 0.10 | −0.02 | 0.0625 | ∞ | ND |
| Anterior ethmoid | 0.22 | 0.02 | 0.0020 | 3.15 (1.46, 6.80) | 0.0035 |
| Maxillary | 0.25 | 0.04 | 0.2657 | 2.24 (0.94, 5.34) | 0.0690 |
| Posterior ethmoid | 0.14 | 0.08 | 0.6512 | 1.40 (0.55, 3.51) | 0.4794 |
| Sphenoid | 0.20 | 0.18 | 0.9999 | 1.17 (0.52, 2.63) | 0.7053 |
Abbreviations: μ, mean; Δ LMA, postoperative LMA score - preoperative LMA score; CI, confidence interval; LMA, Lund-Mackay analog; ND, not defined; OR, odds ratio.
A subset analysis of patients with postoperative scans greater than 6 months was also performed to confirm the 3-month findings. Thirty-seven patients had scans greater than 6 months postoperatively for review. Comparison of the change between left- and right-sided sinuses revealed significantly different changes in the anterior ethmoids (odds ratio [OR] = 3.07 [1.40, 6.76], p = 0.0053) and maxillary sinuses (OR = 3.47 [1.23, 9.81], p = 0.0192). The frontal sinuses failed to reach significance (OR = 4.36 [0.76, 25.03], p = 0.0983).
Comment
The ETNTS approach to the skull base has allowed for shorter hospital stays and decreased patient discomfort with comparable outcomes.3 4 12 15 These prior successes allow us to focus on minimizing this approach's impact on sinonasal physiology. Our institution has previously demonstrated that the ETNTS approach contributes to both short- and long-term sinonasal morbidity. Early morbidity included thick nasal discharge, postnasal discharge, runny nose, sneezing, ear fullness, and facial pain. Although most symptoms resolved, postnasal discharge above baseline persisted beyond 6 months postoperatively on Sinonasal Outcomes Test-20 questionnaires.5 This study implies that there is an inherent disruption of normal sinonasal physiology with a real clinical impact on the patient from the endoscopic ETNTS approach to the skull base. Our current study seeks to elucidate the underlying sinonasal pathology that might contribute to these persistent sinonasal symptoms as related specifically to the resection of the middle turbinate, maxillary antrostomy and elevation of a nasoseptal flap.
The consequences of resection of the middle turbinate are controversial, and to date all studies on the subject are in the context of inflammatory disease. Theoretically, preservation of healthy middle turbinates preserves the normal sinonasal physiology in which these structures participate, including the nasal cycle, humidification, maintenance of transitional airflow, and olfaction.9 In addition, of utmost concern is the risk of an exposed surface of a partially resected middle turbinate causing an adhesion to the lateral wall of the nasal cavity, which can lead to an iatrogenic frontal sinusitis.11 These concerns have been allayed by further studies showing no significant difference in incidence of frontal sinusitis, endoscopic findings, and quality-of-life surveys with the judicious resection of the middle turbinate when it appears to be contributing to the disease process.10 16 However, the consequences of the routine sacrifice of a healthy middle turbinate in an effort to expose the skull base have yet to be established.
The present study retrospectively compared preoperative and postoperative radiographic findings of patients that underwent an ETNTS approach to the skull base that included a right-sided middle turbinate partial resection. The unresected middle turbinate on the left side served as an internal control. We did not find a statistically significant increased incidence of radiographic frontal sinus disease (p = 0.0625) as we had expected based on similar studies in recurrent inflammatory disease11; however, our sample size was underpowered and in all likelihood was not able to detect a difference between the frontal sinuses. It could also be that the partial resection of the middle turbinate done in our approach was low enough to not affect the frontal recess outflow tract, although resection height has been shown previously not to increase the risk of frontal sinusitis.11 In addition, our patient population, unlike prior studies of middle turbinate resection, had normal frontal sinus function preoperatively.
The right anterior ethmoid sinus (p = 0.0020) did show an increased LMA score compared with the left-sided control sinuses, and the maxillary sinus showed a worsening of the right side in the 6-month subset analysis (p = 0.0192). As the middle turbinate forms part of the medial wall of the ostiomeatal complex, we would expect that both of these sinuses would have correlated imaging findings. The maxillary sinus dysfunction could be further exacerbated by the maxillary antrostomy that we used to store the nasoseptal flap through inadvertent failure to include natural “true” maxillary sinus ostia in the surgical antrostomy, predisposing the sinus to mucous recirculation.17 Regardless, in cases amenable to a less-extensive exposure, placement of the nasoseptal flap in the nasopharynx would obviate the need for a maxillary antrostomy, decreasing the risk of postoperative sinus dysfunction. Sphenoid sinuses on both the left and right sides showed statistically significant worsening of LMA scores postoperatively but no difference between the two sides. This finding is the direct result of surgery in a newly created common cavity with the expected increased healing time due to loss of mucosa from drilling.
Our study is not without limitations. Using radiographic evidence of mucosal thickening can locate points of inflammation, but it does not necessarily correlate to patient symptoms.18 Further study with endoscopic data and quality-of-life scores could better clarify this issue. Additionally, a 3-month postoperative follow-up may not be a sufficient time to regain baseline sinus function after follow-up. However, a 3-month follow-up period has been shown to be sufficient for complete remucosalization of the septal donor site,13 and our subset analysis at 6 months postoperatively maintains our findings of worsening imaging in the right anterior ethmoid and maxillary sinuses.
This study is the only evidence examining the consequences of partial middle turbinate resection, maxillary antrostomy, and nasoseptal flap harvest in skull base surgery. We have demonstrated that disruption of the sinonasal anatomy in an endoscopic transnasal transsphenoidal approach to the skull base is associated with worsened radiographic findings in the right anterior ethmoid and maxillary sinuses compared with the left-sided sinuses at 3 and 6 months postoperatively. Given that previous study has shown that the vast majority of skull base pathology can be addressed without resection of the middle turbinate,12 we recommend preservation of the middle turbinate if adequate access to the anterior skull base can be obtained by lateralization alone. In addition, placing the nasoseptal flap in the nasopharynx would avoid the need for a maxillary antrostomy, potentially reducing the risk of iatrogenic maxillary and ethmoid sinus disease.
Acknowledgments
Daniela Markovic, MS, of the Statistical Biomathematical Consulting Clinic in the UCLA Department of Biostatistics contributed to the review of the statistical analysis and presentation of the data.
Authorship
Adam S. DeConde, corresponding author: drafted manuscript, acquisition of data, final approval of the version to be published; Darshni Vira: revising article, acquisition of data, final approval of the version to be published; Christopher Thompson: revising the article, acquisition of data, final approval of the version to be published; Marilene Wang: edited and approved manuscript, conception, and design, analysis and interpretation of data, final approval of the version to be published; Marvin Bergsneider: edited and approved manuscript, conception and design, analysis and interpretation of data, final approval of the version to be published; Jeffrey D. Suh: edited and approved manuscript, conception and design, analysis and interpretation of data, final approval of the version to be published.
References
- 1.Jho H D Carrau R L Ko Y Daly M A Endoscopic pituitary surgery: an early experience Surg Neurol 1997473213–222., discussion 222–223 [DOI] [PubMed] [Google Scholar]
- 2.Carrau R L, Jho H D, Ko Y. Transnasal-transsphenoidal endoscopic surgery of the pituitary gland. Laryngoscope. 1996;106(7):914–918. doi: 10.1097/00005537-199607000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Tabaee A, Anand V K, Barrón Y. et al. Endoscopic pituitary surgery: a systematic review and meta-analysis. J Neurosurg. 2009;111(3):545–554. doi: 10.3171/2007.12.17635. [DOI] [PubMed] [Google Scholar]
- 4.Cappabianca P, Cavallo L M, Colao A. et al. Endoscopic endonasal transsphenoidal approach: outcome analysis of 100 consecutive procedures. Minim Invasive Neurosurg. 2002;45(4):193–200. doi: 10.1055/s-2002-36197. [DOI] [PubMed] [Google Scholar]
- 5.Balaker A E, Bergsneider M, Martin N A, Wang M B. Evolution of sinonasal symptoms following endoscopic anterior skull base surgery. Skull Base. 2010;20(4):245–251. doi: 10.1055/s-0030-1249248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kassam A, Snyderman C H, Mintz A, Gardner P, Carrau R L. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus. 2005;19(1):E3. [PubMed] [Google Scholar]
- 7.Leopold D A, Hummel T, Schwob J E, Hong S C, Knecht M, Kobal G. Anterior distribution of human olfactory epithelium. Laryngoscope. 2000;110(3 Pt 1):417–421. doi: 10.1097/00005537-200003000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Nurse L A Duncavage J A Surgery of the inferior and middle turbinates Otolaryngol Clin North Am 2009422295–309., ix [DOI] [PubMed] [Google Scholar]
- 9.Kennedy D W. Middle turbinate resection: evaluating the issues—should we resect normal middle turbinates? Arch Otolaryngol Head Neck Surg. 1998;124(1):107. doi: 10.1001/archotol.124.1.107. [DOI] [PubMed] [Google Scholar]
- 10.Soler Z M, Hwang P H, Mace J, Smith T L. Outcomes after middle turbinate resection: revisiting a controversial topic. Laryngoscope. 2010;120(4):832–837. doi: 10.1002/lary.20812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swanson P B, Lanza D C, Vining E M, Kennedy D W. The effect of middle turbinate resection upon the frontal sinus. Am J Rhinol. 1995;9(4):191–195. [Google Scholar]
- 12.Nyquist G G, Anand V K, Brown S, Singh A, Tabaee A, Schwartz T H. Middle turbinate preservation in endoscopic transsphenoidal surgery of the anterior skull base. Skull Base. 2010;20(5):343–347. doi: 10.1055/s-0030-1253582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kassam A B Thomas A Carrau R L et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap Neurosurgery 200863101ONS44–ONS52., discussion ONS52–ONS53 [DOI] [PubMed] [Google Scholar]
- 14.Soler Z M, Smith T L. Quality-of-life outcomes after endoscopic sinus surgery: how long is long enough? Otolaryngol Head Neck Surg. 2010;143(5):621–625. doi: 10.1016/j.otohns.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jho H-D, Carrau R L. Endoscopic endonasal transsphenoidal surgery: experience with 50 patients. J Neurosurg. 1997;87(1):44–51. doi: 10.3171/jns.1997.87.1.0044. [DOI] [PubMed] [Google Scholar]
- 16.Fortune D S, Duncavage J A. Incidence of frontal sinusitis following partial middle turbinectomy. Ann Otol Rhinol Laryngol. 1998;107(6):447–453. doi: 10.1177/000348949810700601. [DOI] [PubMed] [Google Scholar]
- 17.Ramadan H H. Surgical causes of failure in endoscopic sinus surgery. Laryngoscope. 1999;109(1):27–29. doi: 10.1097/00005537-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Stewart M G, Johnson R F. Chronic sinusitis: symptoms versus CT scan findings. Curr Opin Otolaryngol Head Neck Surg. 2004;12(1):27–29. doi: 10.1097/00020840-200402000-00008. [DOI] [PubMed] [Google Scholar]


