Summary
Cytoadhesion of Plasmodium falciparum infected erythrocytes to host microvasculature is a key virulence determinant. Parasite binding is mediated by a large family of clonally variant adhesion proteins, termed P. falciparum erythrocyte membrane protein 1 (PfEMP1), encoded by var genes and expressed at the infected-erythrocyte surface. Although PfEMP1 proteins have extensively diverged under opposing selection pressure to maintain ligand binding while avoiding antibody-mediated detection, recent work has revealed they can be classified into different groups based on chromosome location and domain composition. This grouping reflects functional specialization of PfEMP1 proteins for different human host and microvascular binding niches and appears to be maintained by gene recombination hierarchies. In one extreme, a specific PfEMP1 variant is associated with placental binding and malaria during pregnancy, while other PfEMP1 subtypes appear to be specialized for infection of malaria naïve hosts. Here, we discuss recent findings on the origins and evolution of the var gene family, the structure-function of PfEMP1 proteins, and a distinct subset of PfEMP1 variants that have been associated with severe childhood malaria.
Introduction
Clonal antigenic variation is a strategy employed by many microbial pathogens to vary surface proteins to evade immunity. The human malaria parasite, Plasmodium falciparum, varies a family of adhesion proteins at the infected erythrocyte (IE) surface that it uses to bind to the endothelial lining of blood microvessels (Miller et al., 2002). During blood stage infection, P. falciparum merozoites sequentially invade and egress from red blood cells every 48 hours. As the parasite matures, IEs exhibit reduced deformability and sequester from blood circulation. This allows the parasite to avoid splenic clearance mechanisms, but comes at a cost to the host. Sequestered IEs disrupt microvascular blood flow (Dondorp et al., 2008) and cause localized endothelial dysfunction by damaging endothelial barrier integrity and inducing pro-inflammatory, pro-adhesive, and coagulation pathways (Francischetti et al., 2008; Miller et al., 2013; Moxon et al., 2009). This adhesive phenotype is also associated with organ-specific disease complications from IE adherence in brain (cerebral malaria) and placenta (placental malaria) microvasculature (Miller et al., 2002).
Cytoadhesion is mediated by specific interactions between members of the P. falciparum erythrocyte membrane protein 1 (PfEMP1) family encoded by var genes and receptors on the surfaces of endothelial cells (Rowe et al., 2010). Each parasite genotype encodes ~60 different var genes, which are expressed in a mutually exclusive fashion (Guizetti and Scherf, 2013). Switching between var genes facilitates parasite immune evasion and modifies IE binding specificity (Roberts et al., 1993). A specific PfEMP1 variant, VAR2CSA, interacts with chondroitin sulfate A, which is abundant within the placental intervillous space (Fried and Duffy, 1996; Salanti et al., 2004). In contrast, cerebral binding and severe childhood malaria is associated with specific PfEMP1 variants containing a combination of adhesion domains, termed domain cassettes (DC) 8 and 13 (Avril et al., 2012; Claessens et al., 2012; Lavstsen et al., 2012). The vast majority of P. falciparum infections do not lead to severe malaria, suggesting that IE sequestration is relatively well-adapted to limit host death and favor parasite transmission to mosquitoes. It is therefore interesting that potentially lethal adhesion traits persist in the parasite population. This review covers recent advances in the molecular mechanisms of PfEMP1 binding, integrating findings on protein structure-function, var gene evolution, and adhesion phenotypes associated with severe malaria.
Major adhesion traits of P. falciparum infected erythrocytes
P. falciparum IEs have evolved to bind a diverse array of receptors on different human cell types. Two major adhesion traits that may contribute to severe childhood malaria are endothelial binding and rosetting with uninfected erythrocytes. Adhesion also occurs to platelets, dendritic cells, B cells, monocytes and macrophages to modulate host immune functions, a topic reviewed elsewhere (Chua et al., 2013).
Cytoadhesion to microvascular endothelial cells
A common adhesion property of P. falciparum field isolates is CD36 binding (Newbold et al., 1997). CD36 is widely expressed on microvascular endothelia, as well as monocytes, macrophages, dendritic cells and platelets (Silverstein and Febbraio, 2009). CD36-binding not only mediates sequestration of IEs, but also plays a role in non-opsonic phagocytosis of IEs (McGilvray et al., 2000) and modulation of dendritic cell function (Urban et al., 1999). Binding to CD36 is associated with uncomplicated malaria (reviewed in (Rowe et al., 2010)), possibly by targeting sequestered IEs to non-pathogenic sites such as adipose tissue and skeletal muscles, rather than vital organs such as the brain. Indeed, human CD36 deficiency polymorphisms that reduce P. falciparum-binding do not protect against severe malaria (Fry et al., 2009).
A key endothelial cell cytoadherence receptor that has recently been discovered is the Endothelial Protein C receptor (EPCR) (Turner et al., 2013). EPCR is widely expressed on endothelial cells and leukocytes. The protein C-EPCR signalling pathway has anti-inflammatory activities on leukocytes and has anti-thrombotic and anti-inflammatory effects that protect endothelial cells and help maintain vascular integrity (Mosnier et al., 2007). Binding to EPCR is associated with severe malaria (Turner et al., 2013) and modifications in EPCR expression in cerebral malaria have been reported (Moxon et al., 2013). Parasites selected for binding to human brain microvascular endothelial cells express PfEMP1 variants (Avril et al., 2012; Claessens et al., 2012) that bind to EPCR (Turner et al., 2013).
Numerous other endothelial receptors have been described (reviewed in (Rowe et al., 2010)), but many are poorly understood and their role in malaria disease is unclear. Cytoadhesion studies under flow conditions show that while some interactions, such as CD36-binding, cause stationary adhesion, others, such as ICAM1-binding, promote rolling of IEs (Cooke et al., 1994). Interactions between IE and multiple receptors may co-operate in vivo to maximise adhesion and sequestration (Yipp et al., 2007).
Rosetting with uninfected erythrocytes
Binding of IEs to uninfected erythrocytes (rosetting), is an adhesion phenotype that varies between clinical isolates, with high levels of rosetting associated with severe malaria in African children (reviewed in (Rowe et al., 2010). Rosetting may contribute to malaria pathology by causing greater obstruction to microvascular blood flow than cytoadherence alone (Kaul et al., 1991). Rosetting is mediated by specific PfEMP1 variants binding to receptors on uninfected erythrocytes, including Complement Receptor 1 (CR1) (Rowe et al., 1997) and A and B blood group tri-saccharides (Carlson and Wahlgren, 1992). Some rosetting variants also bind the Fc region of human IgM (Ghumra et al., 2008), a process that strengthens rosetting interactions (Scholander et al., 1996). Naturally occurring polymorphisms in human erythrocyte rosetting receptors, such as CR1 deficiency and blood group O, impair rosette formation, and confer significant protection against severe malaria, confirming the importance of rosetting as a virulence factor in malaria (Cockburn et al., 2004; Rowe et al., 2007).
Molecular mechanisms of IE binding
PfEMP1 proteins contain a polymorphic ectodomain, linked through a single transmembrane helix to a relatively conserved cytoplasmic region (Baruch et al., 1995; Smith et al., 1995; Su et al., 1995). The cytoplasmic tail anchors PfEMP1 proteins at parasite-induced knob-like protrusions at the erythrocyte surface (Maier et al., 2009). The PfEMP1 ectodomain is built from a combination of Duffy binding-like (DBL) and cysteine-rich interdomain region (CIDR) adhesion domains (Smith et al., 2000). These binding modules are only found in Plasmodium. The DBL superfamily bridges two important adhesive properties of P. falciparum, having a key role in erythrocyte invasion (DBL-containing erythrocyte binding proteins, DBL-EBPs) and IE cytoadhesion interactions (DBL-PfEMP1) (Miller et al., 2002).
Evolutionary origins of var genes
Of the five Plasmodium spp. that infect humans, P. falciparum is responsible for nearly all deaths and is the only one that undergoes massive IE sequestration in host microvasculature (Smith and Deitsch, 2012). As homologs of DBL-EBP erythrocyte invasion ligands are found in human, rodent, and primate malaria species (Duraisingh et al., 2012), it is likely that this unique cytoadhesion trait evolved from parasite invasion ligands. Although it was originally postulated that P. falciparum was more virulent because it had recently jumped from avian malaria species into humans and was less well adapted (Waters et al., 1991), more recent phylogenetic and genome analysis does not support this interpretation and instead suggests that var genes have co-evolved for a long time with primates. At least six distinct falciparum-like species infect African Great Apes (chimpanzees and gorillas) (Prugnolle et al., 2011) and the var gene family is restricted to this subgenus of Plasmodium. One of the closest known relatives of P. falciparum is the chimpanzee malaria P. reichenowi. Both encode var genes (Rask et al., 2010) and are estimated to have diverged 6–10 million years ago (Escalante and Ayala, 1995). Little is known about the role of PfEMP1 proteins in non-human primate infections or pathogenesis, but these findings have important implications for our understanding of malaria pathogenesis. It indicates that the cytoadhesion trait is not a recent adaptation and it will be interesting to learn if there are ancestral PfEMP1 binding properties that may confer selective advantages for parasite growth and transmission.
Genomic organization of var genes
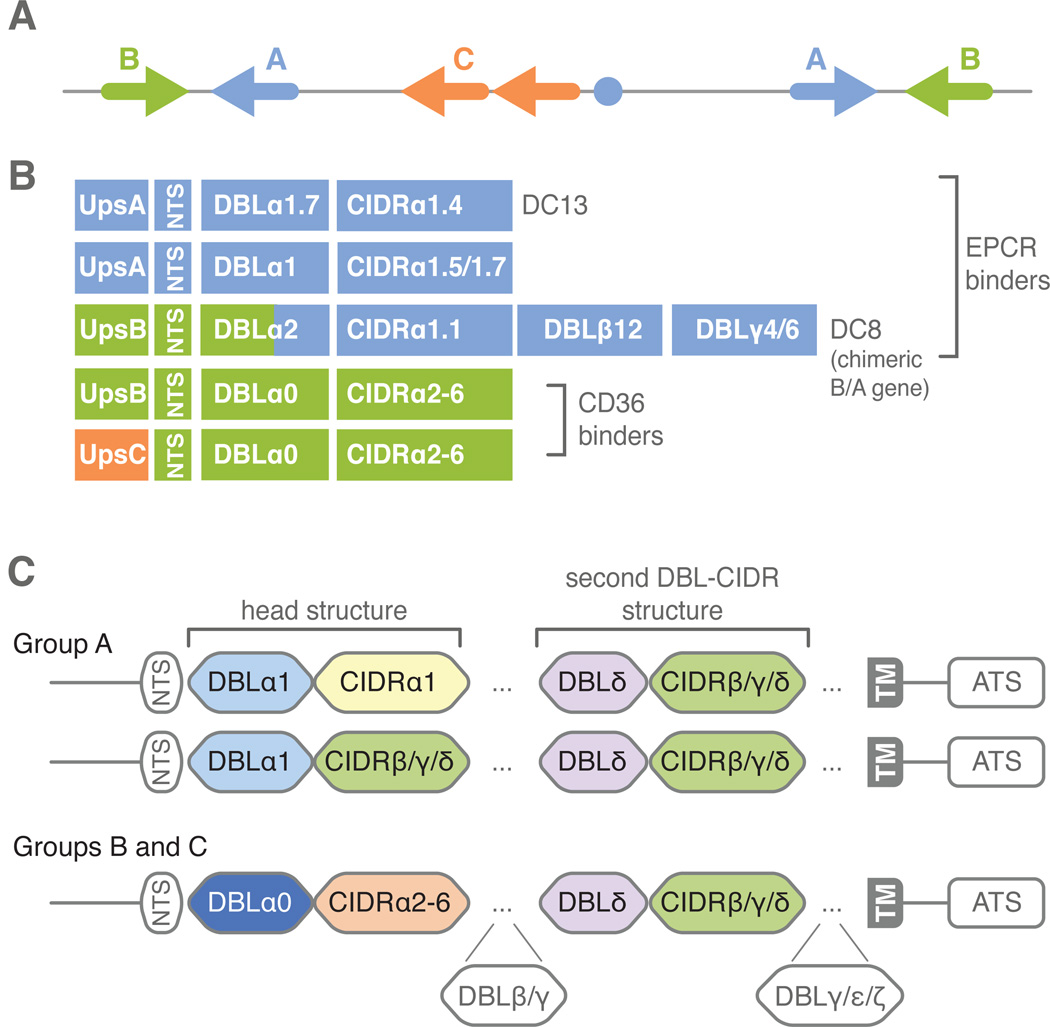
Members of the var gene family are concentrated in sub-telomeric regions of all chromosomes and internal regions on chromosomes 4, 7, 8, and 12 (Gardner et al., 2002). Comparison of the 3D7 genome reference isolate and six partial P. falciparum genomes highlights many commonalities between var repertoires (Rask et al., 2010). In particular, the majority of var genes can be classified into three main groups (A, B, and C) on the basis of upstream sequence (Ups), chromosome location, and direction of transcription (Fig. 1). Surprisingly, the var gene repertoire also contains three strain-transcendent variants (var1, var2csa, and type3 var) found in most or all parasite genotypes. It is thought that this genome organization contributes to gene recombination hierarchies and functional specialization of PfEMP1 proteins (Kraemer and Smith, 2006). Intriguingly, UpsA, UpsB, and UpsC var genes and partial var1 and var2csa homologs are present in the highly fragmentary P. reichenowi genome sequence (Rask et al., 2010). This reinforces the ancient origins of the var genome organization and suggests the possibility that functional specialization of proteins may have occurred early.
Fig. 1.
Var gene organization and protein domain architectures. A. Chromosomal organization of var genes. Group B and A var genes are located in the subtelomeric regions and transcribed in opposite orientations. Group C are typically found on central chromosome clusters. B. There is a recombination hot spot between subdomains 2 and 3 in the DBL domain of the PfEMP1 head structure. DC8 is an unusual chimeric gene between a group B and group A var gene. C. Different types of DBL and CIDR domains are located at the N- and C-terminus of proteins. Small PfEMP1 have four extracellular domains, large PfEMP1 have additional DBL domains after the head structure or the second DBL-CIDR structure.
Structure-Function of PfEMP1 proteins
The modular architecture of PfEMP1s and arrangement of ligand binding domains
Although PfEMP1 differ in size and number of extracellular domains, nearly all proteins have a tandem DBL-CIDR domain at the N-terminus, called the semi-conserved head structure. In small proteins, this is followed by a second DBL-CIDR tandem forming a 4 domain extracellular unit, while large proteins have additional types of DBL domains (Fig. 1). By sequence similarity, DBL and CIDR domains are classified into major types (α, β, γ, δ, etc.) and sub-types (e.g. CIDRα1.1) (Rask et al., 2010; Smith et al., 2000). Sequence classification likely reflects structural and functional specialization of domains. For instance, the PfEMP1 head structure is nearly always comprised of a DBLα-CIDRα tandem and other DBL and CIDR sequence types (β, γ, δ, etc.) are located C-terminal to these (Fig. 1) (Rask et al., 2010). Furthermore, group A head structures have diverged in sequence and binding properties from group B and C (Robinson et al., 2003) (Fig. 2).
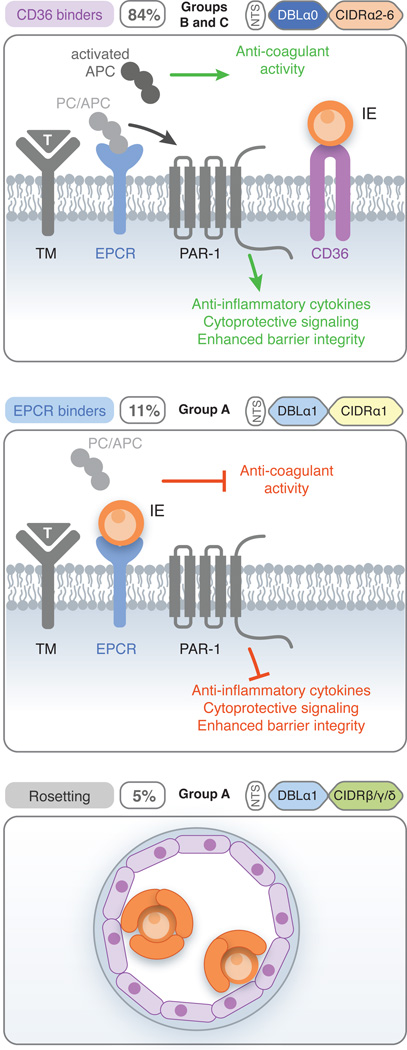
Fig. 2.
Model of PfEMP1 head structure divergence. The PfEMP1 head structure has diverged into three major binding groups under selection for EPCR-binding, CD36-binding, or to form rosettes with uninfected erythrocytes. The proportion of different head structure types in the 3D7 reference genome isolate and their predicted binding properties is shown. Note there may be some binding exceptions (e.g. only a subset of CIDRα1 domains bind EPCR, see Fig. 1). CD36 binding is the most common PfEMP1 adhesion trait and is associated with mild malaria. EPCR-binding and rosetting is linked to group A head structures. Group A PfEMP1 tend to be expressed in early childhood infections or malaria naïve, and are also associated with severe malaria. Under normal circumstances, protein C (PC) binds to EPCR and is activated by the thrombin (T)/thrombomodulin (TM) complex. Activated protein C (APC) that is released into the plasma has anti-coagulant activity and the APC/EPCR complex activates the protease activated receptor 1 (PAR1) to mediate intracellular signaling. The protein C-EPCR signalling pathway has anti-inflammatory, anti-thrombotic and endothelial cytoprotective activities that help maintain vascular integrity (Mosnier et al., 2007). The loss of EPCR at sites of P. falciparum IE sequestration (Moxon et al., 2013) and EPCR-binding parasites (Turner et al., 2013) may combine to interfere or subvert these pathways and contribute to disease pathogenesis.
The modular nature of PfEMP1s naturally led to the suggestion that they operate as strings of distinct ligand binding modules and that DBL-CIDR domains may form a structure-function unit. This prediction is supported in that many binding properties have been ascribed to single domains, with for example, ICAM1 binding to DBLβ domains (Howell et al., 2008) and CD36 to CIDRα in the PfEMP1 head structure (Baruch et al., 1997). However, specific adhesion traits, such as CSA binding, appear to involve a combination of domains (Clausen et al., 2012; Srivastava et al., 2011). Recent computational analysis identified 21 tandem domain arrangements of two or more domains (e.g. DC8 or DC13) (Fig. 1), which are highly conserved across parasite genotypes (Rask et al., 2010). This conservation suggests that DCs may be maintained as larger structure-function units, encoding one or more adhesion properties.
Several lines of evidence suggest PfEMP1 ectodomains have higher order organization. For instance, the structure of a DBL1α-CIDR1γ tandem domain reveals close packing between the DBL and CIDR domains to generate a rigid structural unit (Vigan-Womas et al., 2012). In addition, two small angle x-ray scattering (SAXS) studies show that full-length PfEMP1 ectodomains can adopt different shapes. Whereas full-length VAR2CSA ectodomain folds back on itself into a compact structure (Clausen et al., 2012; Srivastava et al., 2010), a CD36 and ICAM-1 binding PfEMP1 variant has an extended structure (Brown et al., 2013). These different arrangements may facilitate specific PfEMP1-receptor interactions and align pRBCs with cell surface receptors. Despite the availability of isolated DBL and CIDR structures, a major unanswered question is how PfEMP1 proteins recognize different protein or carbohydrate substrates. Additional sequencing and analysis of var genes paired with studies of PfEMP1 domain and ectodomain structures in complex with host receptors will be needed to fully understand which surface determinants are needed for PfEMP1 binding specificity and how PfEMP1 ectodomains are organized to present these binding surfaces to host receptors.
Binding properties of the PfEMP1 head structure and recombination hotspots
The PfEMP1 head structure plays a key role in binding and has diverged into three major adhesion properties. Whereas most group B and C PfEMP1 proteins appear to be under selection to bind CD36 (Robinson et al., 2003), many group A variants were recently shown to bind EPCR (Turner et al., 2013) or to form rosettes with uninfected erythrocytes (Fig. 2). Rosetting variants tend to encode CIDR sub-types (β, γ, δ) (Ghumra et al., 2012), which are more typically found in the membrane proximal DBL-CIDR tandem (Fig. 1).
Sequence analysis suggests there is a recombination hotspot between DBL subdomains 2 and 3 (Rask et al., 2010). From genome comparisons, recombination appears to be extremely rare between group A and non-group A genes (Kraemer et al., 2007; Rask et al., 2010). The reduced recombination between UpsA and UpsB genes is not unexpected given their inverted gene orientation would lead to a lethal event for a single exchange. However, DC8 is an unusual chimeric gene between an UpsB and group A var gene with the breakpoint between subdomain 2 and subdomain 3 in the DBLα domain (Lavstsen et al., 2012). By limiting recombination between var groups, the parasite is able to evolve specialized PfEMP1 subsets for different microvascular niches, which differ in CD36 and EPCR expression levels. For instance, CD36 is weakly expressed in brain and placental microvasculature. Platelets express CD36 and it has been speculated that these may bridge P. falciparum IE binding to CD36 negative endothelium (Wassmer et al., 2004). However, in the case of cerebral binding, the selective advantage for the parasite of this tissue location is puzzling because this adhesion trait may kill the host. This paradox is starting to be explained by recent findings on severe malaria variants.
Group A var genes and severe childhood malaria
African children with severe malaria suffer from four main complications — coma (cerebral malaria), respiratory distress, hypoglycaemia and severe anaemia. There is immunoepidemiological data that group A PfEMP1 variants are associated with early childhood infections (Cham et al., 2009; Jensen et al., 2004; Lavstsen et al., 2012) and that severe childhood malaria infections are linked to the expression of a restricted subset of PfEMP1 (Bull et al., 2000; Nielsen et al., 2002). The continuous release of var sequence data has enabled increasingly more sophisticated molecular tools to solve the challenge of detecting and typing transcript expression of this diverse gene family. Although different approaches are used for var profiling making it difficult to compare between studies, a consensus is emerging that group A-like var genes are increased in severe malaria infections. Within the group A, rosetting parasites were more strongly linked to respiratory distress, and non-rosetting, group A-like genes with cerebral malaria in Kenya (Warimwe et al., 2012). Furthermore, using new primers sets that are specific to different PfEMP1 domain types, DC8 and DC13 var genes (Lavstsen et al., 2012) and EPCR binding (Turner et al., 2013) are strongly linked to cerebral malaria and other severe malaria complications. Taken together, these findings suggest that PfEMP1 proteins have diverged into CD36 binding and non-CD36 binding subsets (Fig. 2). The non-CD36 binding group A subset may confer a growth and transmission advantage in malaria naïve hosts, although this is balanced by a greater risk of severe malaria outcomes. An important question is whether all EPCR-binding or rosetting variants carry the same risk of severe outcomes, or if the combination of adhesion traits associated with specific EPCR-binding or rosetting PfEMP1 variants influences the extent of cerebral sequestration or disease severity. Currently, most studies have used broadly cross-reactive DBLα primers for var profiling and the new PfEMP1 domain type specific primers (e.g. DC8) have been only been evaluated on patient isolates from Tanzania (Lavstsen et al., 2012). The two approaches amplify different regions of var genes and are subject to different limitations in detecting different var types (Lavstsen et al., 2012). In the future, further application of these combined molecular tools for profiling var gene expression in combination with EPCR binding and rosetting assays are needed to fully resolve the question of which PfEMP1 subtypes are most likely to cause severe disease in patients from different regions of the world.
Conclusions
Despite the extensive diversification of var genes, recent work suggests that different var gene repertoires encode similar compositions of proteins, which are under selection for different host or microvascular niches. These protein groups can be classified by chromosome location and domain composition and appear to be maintained by ancient gene recombination hierarchies. Analysis of the PfEMP1 head structure indicates it has diverged into CD36-binding, EPCR-binding, and rosetting variants, which have different roles in mild versus severe malaria. Intriguingly, many of the known parasite cytoadhesion receptors are shared between endothelial cells and leukocytes, and thus it will be important to understand if there is selection on PfEMP1s between strong endothelial adhesion and host inflammatory properties. The finding that DC8 and DC13 variants encode EPCR binding activity has important implications for malaria pathogenesis. The ability of DC8 and DC13 variants to bind avidly to diverse endothelial cell types (Avril et al., 2013) may benefit parasites by conferring a growth and transmission advantage in malaria naïve hosts. However, this adhesion trait may also interfere with protein C-EPCR signaling pathways (Moxon et al., 2013; Turner et al., 2013), resulting in deregulated inflammation and coagulation pathways and contribute to severe malaria complications. To design disease interventions, it will be important to better understand how IE-host receptor binding interactions may be manipulating the host environment to the parasite benefit.
Acknowledgements
This work was supported by RO1 AI47953 (JDS), Lundbeck Foundation and The Danish Medical Research Council (TL), and The Wellcome Trust (JAR grant no. 084226 and MKH). We thank the reviewers for their suggestions and apologize for not citing all relevant publications due to space limitations in the allowed number of references.
Footnotes
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- Avril M, Brazier AJ, Melcher M, Sampath S, Smith JD. DC8 and DC13 var Genes Associated with Severe Malaria Bind Avidly to Diverse Endothelial Cells. PLoS Pathog. 2013;9:e1003430. doi: 10.1371/journal.ppat.1003430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avril M, Tripathi AK, Brazier AJ, Andisi C, Janes JH, Soma VL, et al. A restricted subset of var genes mediates adherence of Plasmodium falciparum-infected erythrocytes to brain endothelial cells. Proc Natl Acad Sci U S A. 2012;109:E1782–E1790. doi: 10.1073/pnas.1120534109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baruch DI, Ma XC, Singh HB, Bi X, Pasloske BL, Howard RJ. Identification of a region of PfEMP1 that mediates adherence of Plasmodium falciparum infected erythrocytes to CD36: conserved function with variant sequence. Blood. 1997;90:3766–3775. [PubMed] [Google Scholar]
- Baruch DI, Pasloske BL, Singh HB, Bi X, Ma XC, Feldman M, et al. Cloning the P. falciparum gene encoding PfEMP1, a malarial variant antigen and adherence receptor on the surface of parasitized human erythrocytes. Cell. 1995;82:77–87. doi: 10.1016/0092-8674(95)90054-3. [DOI] [PubMed] [Google Scholar]
- Brown A, Turner L, Christoffersen S, Andrews KA, Szestak T, Zhao Y, et al. Molecular Architecture of a Complex between an Adhesion Protein from the Malaria Parasite and Intracellular Adhesion Molecule 1. J Biol Chem. 2013;288:5992–6003. doi: 10.1074/jbc.M112.416347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull PC, Kortok M, Kai O, Ndungu F, Ross A, Lowe BS, et al. Plasmodium falciparum-infected erythrocytes: agglutination by diverse Kenyan plasma is associated with severe disease and young host age. J Infect Dis. 2000;182:252–259. doi: 10.1086/315652. [DOI] [PubMed] [Google Scholar]
- Carlson J, Wahlgren M. Plasmodium falciparum erythrocyte rosetting is mediated by promiscuous lectin-like interactions. J Exp Med. 1992;176:1311–1317. doi: 10.1084/jem.176.5.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cham GK, Turner L, Lusingu J, Vestergaard L, Mmbando BP, Kurtis JD, et al. Sequential, ordered acquisition of antibodies to Plasmodium falciparum erythrocyte membrane protein 1 domains. J Immunol. 2009;183:3356–3363. doi: 10.4049/jimmunol.0901331. [DOI] [PubMed] [Google Scholar]
- Chua CL, Brown G, Hamilton JA, Rogerson S, Boeuf P. Monocytes and macrophages in malaria: protection or pathology? Trends Parasitol. 2013;29:26–34. doi: 10.1016/j.pt.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Claessens A, Adams Y, Ghumra A, Lindergard G, Buchan CC, Andisi C, et al. A subset of group A-like var genes encodes the malaria parasite ligands for binding to human brain endothelial cells. Proc Natl Acad Sci U S A. 2012;109:E1772–E1781. doi: 10.1073/pnas.1120461109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clausen TM, Christoffersen S, Dahlback M, Langkilde AE, Jensen KE, Resende M, et al. Structural and functional insight into how the Plasmodium falciparum VAR2CSA protein mediates binding to chondroitin sulfate A in placental malaria. J Biol Chem. 2012;287:23332–23345. doi: 10.1074/jbc.M112.348839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockburn IA, Mackinnon MJ, O'Donnell A, Allen SJ, Moulds JM, Baisor M, et al. A human complement receptor 1 polymorphism that reduces Plasmodium falciparum rosetting confers protection against severe malaria. PNAS. 2004;101:272–277. doi: 10.1073/pnas.0305306101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke BM, Berendt AR, Craig AG, MacGregor J, Newbold CI, Nash GB. Rolling and stationary cytoadhesion of red blood cells parasitized by Plasmodium falciparum : separate roles for ICAM-1, CD36 and thrombospondin. Br J Haematol. 1994;87:162–170. doi: 10.1111/j.1365-2141.1994.tb04887.x. [DOI] [PubMed] [Google Scholar]
- Dondorp AM, Ince C, Charunwatthana P, Hanson J, van KA, Faiz MA, et al. Direct in vivo assessment of microcirculatory dysfunction in severe falciparum malaria. J Infect Dis. 2008;197:79–84. doi: 10.1086/523762. [DOI] [PubMed] [Google Scholar]
- Duraisingh MT, Dvorin JD, Preiser PR. Invasion ligand diversity and pathogenesis in blood-stage malaria. In: Sibley LD, Howlett BJ, Heitman J, editors. Evolution of Virulence in Eukaryotic Microbes. Wiley-Blackwell; 2012. pp. 362–383. [Google Scholar]
- Escalante AA, Ayala FJ. Evolutionary origin of Plasmodium and other Apicomplexa based on rRNA genes. Proc Natl Acad Sci U S A. 1995;92:5793–5797. doi: 10.1073/pnas.92.13.5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francischetti IM, Seydel KB, Monteiro RQ. Blood coagulation, inflammation, and malaria. Microcirculation. 2008;15:81–107. doi: 10.1080/10739680701451516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried M, Duffy PE. Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science. 1996;272:1502–1504. doi: 10.1126/science.272.5267.1502. [DOI] [PubMed] [Google Scholar]
- Fry AE, Ghansa A, Small KS, Palma A, Auburn S, Diakite M, et al. Positive selection of a CD36 nonsense variant in sub-Saharan Africa, but no association with severe malaria phenotypes. Hum Mol Genet. 2009;18:2683–2692. doi: 10.1093/hmg/ddp192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner MJ, Hall N, Fung E, White O, Berriman M, Hyman RW, et al. Genome sequence of the human malaria parasite Plasmodium falciparum. Nature. 2002;419:498–511. doi: 10.1038/nature01097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghumra A, Semblat JP, Ataide R, Kifude C, Adams Y, Claessens A, et al. Induction of strain-transcending antibodies against Group A PfEMP1 surface antigens from virulent malaria parasites. PLoS Pathog. 2012;8:e1002665. doi: 10.1371/journal.ppat.1002665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghumra A, Semblat JP, McIntosh RS, Raza A, Rasmussen IB, Braathen R, et al. Identification of residues in the Cmu4 domain of polymeric IgM essential for interaction with Plasmodium falciparum erythrocyte membrane protein 1 (PfEMP1) J Immunol. 2008;181:1988–2000. doi: 10.4049/jimmunol.181.3.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guizetti J, Scherf A. Silence, activate, poise and switch! Mechanisms of antigenic variation in Plasmodium falciparum. Cell Microbiol. 2013;15:718–726. doi: 10.1111/cmi.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell DP, Levin EA, Springer AL, Kraemer SM, Phippard DJ, Schief WR, Smith JD. Mapping a common interaction site used by Plasmodium falciparum Duffy binding-like domains to bind diverse host receptors. Mol Microbiol. 2008;67:78–87. doi: 10.1111/j.1365-2958.2007.06019.x. [DOI] [PubMed] [Google Scholar]
- Jensen AT, Magistrado P, Sharp S, Joergensen L, Lavstsen T, Chiucchiuini A, et al. Plasmodium falciparum associated with severe childhood malaria preferentially expresses PfEMP1 encoded by group A var genes. J Exp Med. 2004;199:1179–1190. doi: 10.1084/jem.20040274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaul DK, Roth EF, Jr, Nagel RL, Howard RJ, Handunnetti SM. Rosetting of Plasmodium falciparum-infected red blood cells with uninfected red blood cells enhances microvascular obstruction under flow conditions. Blood. 1991;78:812–819. [PubMed] [Google Scholar]
- Kraemer SM, Kyes SA, Aggarwal G, Springer AL, Nelson SO, Christodoulou Z, et al. Patterns of gene recombination shape var gene repertoires in Plasmodium falciparum : comparisons of geographically diverse isolates. BMC Genomics. 2007;8:45. doi: 10.1186/1471-2164-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer SM, Smith JD. A family affair: var genes, PfEMP1 binding, and malaria disease. Current Opinion in Microbiology. 2006;9:374–380. doi: 10.1016/j.mib.2006.06.006. [DOI] [PubMed] [Google Scholar]
- Lavstsen T, Turner L, Saguti F, Magistrado P, Rask TS, Jespersen JS, et al. Plasmodium falciparum erythrocyte membrane protein 1 domain cassettes 8 and 13 are associated with severe malaria in children. Proc Natl Acad Sci U S A. 2012;109:E1791–E1800. doi: 10.1073/pnas.1120455109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier AG, Cooke BM, Cowman AF, Tilley L. Malaria parasite proteins that remodel the host erythrocyte. Nat Rev Microbiol. 2009;7:341–354. doi: 10.1038/nrmicro2110. [DOI] [PubMed] [Google Scholar]
- McGilvray ID, Serghides L, Kapus A, Rotstein OD, Kain KC. Nonopsonic monocyte/macrophage phagocytosis of Plasmodium falciparum- parasitized erythrocytes: a role for CD36 in malarial clearance. Blood. 2000;96:3231–3240. [PubMed] [Google Scholar]
- Miller LH, Ackerman HC, Su XZ, Wellems TE. Malaria biology and disease pathogenesis: insights for new treatments. Nat Med. 2013;19:156–167. doi: 10.1038/nm.3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LH, Baruch DI, Marsh K, Doumbo OK. The pathogenic basis of malaria. Nature. 2002;415:673–679. doi: 10.1038/415673a. [DOI] [PubMed] [Google Scholar]
- Mosnier LO, Zlokovic BV, Griffin JH. The cytoprotective protein C pathway. Blood. 2007;109:3161–3172. doi: 10.1182/blood-2006-09-003004. [DOI] [PubMed] [Google Scholar]
- Moxon CA, Heyderman RS, Wassmer SC. Dysregulation of coagulation in cerebral malaria. Mol Biochem Parasitol. 2009;166:99–108. doi: 10.1016/j.molbiopara.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moxon CA, Wassmer SC, Milner DA, Jr, Chisala NV, Taylor TE, Seydel KB, et al. Loss of endothelial protein C receptors links coagulation and inflammation to parasite sequestration in cerebral malaria in African children. Blood. 2013;122:842–851. doi: 10.1182/blood-2013-03-490219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbold C, Warn P, Black G, Berendt A, Craig A, Snow B, Msobo M, Peshu N, Marsh K. Receptor-specific adhesion and clinical disease in Plasmodium falciparum. Am J Trop Med Hyg. 1997;57:389–398. doi: 10.4269/ajtmh.1997.57.389. [DOI] [PubMed] [Google Scholar]
- Nielsen MA, Staalsoe T, Kurtzhals JA, Goka BQ, Dodoo D, Alifrangis M, et al. Plasmodium falciparum variant surface antigen expression varies between isolates causing severe and nonsevere malaria and is modified by acquired immunity. J Immunol. 2002;168:3444–3450. doi: 10.4049/jimmunol.168.7.3444. [DOI] [PubMed] [Google Scholar]
- Prugnolle F, Durand P, Ollomo B, Duval L, Ariey F, Arnathau C, et al. A Fresh Look at the Origin of Plasmodium falciparum the Most Malignant Malaria Agent. PLoS Pathog. 2011;7:e1001283. doi: 10.1371/journal.ppat.1001283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rask TS, Hansen DA, Theander TG, Gorm PA, Lavstsen T. Plasmodium falciparum Erythrocyte Membrane Protein 1 Diversity in Seven Genomes - Divide and Conquer. PLoS Comput Biol. 2010;6 doi: 10.1371/journal.pcbi.1000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts DJ, Biggs BA, Brown G, Newbold CI. Protection, pathogenesis and phenotypic plasticity in Plasmodium falciparum malaria. Parasitol Today. 1993;9:281–286. doi: 10.1016/0169-4758(93)90121-u. [DOI] [PubMed] [Google Scholar]
- Robinson BA, Welch TL, Smith JD. Widespread functional specialization of Plasmodium falciparum erythrocyte membrane protein 1 family members to bind CD36 analysed across a parasite genome. Mol Microbiol. 2003;47:1265–1278. doi: 10.1046/j.1365-2958.2003.03378.x. [DOI] [PubMed] [Google Scholar]
- Rowe JA, Handel IG, Thera MA, Deans AM, Lyke KE, Kone A, et al. Blood group O protects against severe Plasmodium falciparum malaria through the mechanism of reduced rosetting. Proc Natl Acad Sci U S A. 2007;104:17471–17476. doi: 10.1073/pnas.0705390104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe JA, Moulds JM, Newbold CI, Miller LH. P. falciparum rosetting mediated by a parasite-variant erythrocyte membrane protein and complement-receptor 1. Nature. 1997;388:292–295. doi: 10.1038/40888. [DOI] [PubMed] [Google Scholar]
- Rowe JA, Claessens A, Corrigan RA, Arman M. Adhesion of Plasmodium falciparum-infected erythrocytes to human cells: molecular mechanisms and therapeutic implications. Expert Rev Mol Med. 11:e16. doi: 10.1017/S1462399409001082. 5-26-2010. Ref Type: Generic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salanti A, Dahlback M, Turner L, Nielsen MA, Barfod L, Magistrado P, et al. Evidence for the involvement of VAR2CSA in pregnancy-associated malaria. J Exp Med. 2004;200:1197–1203. doi: 10.1084/jem.20041579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholander C, Treutiger CJ, Hultenby K, Wahlgren M. Novel fibrillar structure confers adhesive property to malaria-infected erythrocytes. Nat Med. 1996;2:204–208. doi: 10.1038/nm0296-204. [DOI] [PubMed] [Google Scholar]
- Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2:re3. doi: 10.1126/scisignal.272re3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Chitnis CE, Craig AG, Roberts DJ, Hudson-Taylor DE, Peterson DS, et al. Switches in expression of Plasmodium falciparum var genes correlate with changes in antigenic and cytoadherent phenotypes of infected erythrocytes. Cell. 1995;82:101–110. doi: 10.1016/0092-8674(95)90056-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Deitsch KW. Antigenic variation, adherence, and virulence in malaria. In: Sibley LD, Howlett BJ, Heitman J, editors. Evolution of virulence in eukaryotic microbes. Wiley-Blackwell; 2012. pp. 338–361. [Google Scholar]
- Smith JD, Subramanian G, Gamain B, Baruch DI, Miller LH. Classification of adhesive domains in the Plasmodium falciparum erythrocyte membrane protein 1 family. Mol Biochem Parasitol. 2000;110:293–310. doi: 10.1016/s0166-6851(00)00279-6. [DOI] [PubMed] [Google Scholar]
- Srivastava A, Gangnard S, Dechavanne S, Amirat F, Lewit BA, Bentley GA, Gamain B. Var2CSA minimal CSA binding region is located within the N-terminal region. PLoS ONE. 2011;6:e20270. doi: 10.1371/journal.pone.0020270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava A, Gangnard S, Round A, Dechavanne S, Juillerat A, Raynal B, et al. Full-length extracellular region of the var2CSA variant of PfEMP1 is required for specific, high-affinity binding to CSA. Proc Natl Acad Sci U S A. 2010;107:4884–4889. doi: 10.1073/pnas.1000951107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su XZ, Heatwole VM, Wertheimer SP, Guinet F, Herrfeldt JA, Peterson DS, et al. The large diverse gene family var encodes proteins involved in cytoadherence and antigenic variation of Plasmodium falciparum-infected erythrocytes. Cell. 1995;82:89–100. doi: 10.1016/0092-8674(95)90055-1. [DOI] [PubMed] [Google Scholar]
- Turner L, Lavstsen T, Berger SS, Wang CW, Petersen JE, Avril M, et al. Severe malaria is associated with parasite binding to endothelial protein C receptor. Nature. 2013;498:502–505. doi: 10.1038/nature12216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urban BC, Ferguson DJ, Pain A, Willcox N, Plebanski M, Austyn JM, Roberts DJ. Plasmodium falciparum-infected erythrocytes modulate the maturation of dendritic cells. Nature. 1999;400:73–77. doi: 10.1038/21900. [DOI] [PubMed] [Google Scholar]
- Vigan-Womas I, Guillotte M, Juillerat A, Hessel A, Raynal B, England P, et al. Structural basis for the ABO blood-group dependence of Plasmodium falciparum rosetting. PLoS Pathog. 2012;8:e1002781. doi: 10.1371/journal.ppat.1002781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warimwe GM, Fegan G, Musyoki JN, Newton CR, Opiyo M, Githinji G, et al. Prognostic indicators of life-threatening malaria are associated with distinct parasite variant antigen profiles. Sci Transl Med. 2012;4:129ra45. doi: 10.1126/scitranslmed.3003247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassmer SC, Lepolard C, Traore B, Pouvelle B, Gysin J, Grau GE. Platelets reorient Plasmodium falciparum-infected erythrocyte cytoadhesion to activated endothelial cells. J Infect Dis. 2004;189:180–189. doi: 10.1086/380761. [DOI] [PubMed] [Google Scholar]
- Waters AP, Higgins DG, McCutchan TF. Plasmodium falciparum appears to have arisen as a result of lateral transfer between avian and human hosts. Proc Natl Acad Sci U S A. 1991;88:3140–3144. doi: 10.1073/pnas.88.8.3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yipp BG, Hickey MJ, Andonegui G, Murray AG, Looareesuwan S, Kubes P, Ho M. Differential roles of CD36, ICAM-1, and P-selectin in Plasmodium falciparum cytoadherence in vivo. Microcirculation. 2007;14:593–602. doi: 10.1080/10739680701404705. [DOI] [PubMed] [Google Scholar]