Abstract
Background & Aims
Defecatory disorders can be diagnosed by rectal balloon expulsion (BE) and anorectal manometry, which are traditionally evaluated in the seated and left lateral (LL) positions respectively. The aims of this study were to compare BE in the LL and seated positions and to compare anorectal manometric parameters to BE performed in the seated and left lateral positions.
Methods
220 women (healthy [62], chronic constipation [158]) had anorectal high resolution manometry and BE, summarized by time required (seated position, normal ≤60s) or external traction to facilitate expulsion (LL position, normal ≤100g).
Results
BE results in both positions were either concordant (normal [141], or abnormal [32]), or discordant (only LL abnormal [30], only seated abnormal [17]). There was modest agreement (κ =0.44 [95%CI 0.30–0.57]) between seated and LL BE. Compared to subjects with normal BE in both positions, anal pressure during simulated evacuation (SE) was higher, and the rectoanal gradient (rectal-anal pressure) during simulated evacuation was more negative in the other 3 categories (i.e., abnormal LL only, abnormal seated only, and both abnormal). High anal pressure during SE (OR=1.02, 95%CI 1.00–1.04) and high rectal sensory threshold for desire to defecate (OR=1.01, 95% CI 1.00–1.02) were associated with increased risk of abnormal BE in both positions, whereas high rectal pressure during SE (OR=0.96, 95% CI 0.93- 0.98) was associated with lower risk.
Conclusions
There is modest agreement between rectal BE in left lateral and seated positions. In addition to abnormal seated BE, which is considered indicative of pelvic floor dysfunction, HRM findings suggest that even some patients with abnormal BE in the left lateral position have pelvic floor dysfunction.
BACKGROUND
The rectoanal gradient (i.e., difference between or ratio of rectal and anal pressure) measured by manometry during simulated evacuation and the rectal balloon expulsion test are widely used to diagnose defecatory disorders (DD) in patients with chronic constipation (1, 2). In contrast to proctography, these tests do not assess for structural disturbances. Moreover, the correlation between the rectoanal gradient during simulated evacuation and the rectal balloon expulsion test is modest and there is no criterion standard for diagnosing DD (3, 4). While an abnormal anorectal gradient (i.e., higher anal than rectal pressures) during simulated evacuation is recommended for diagnosing defecatory disorders (1, 5), this gradient, can also be “abnormal” in asymptomatic subjects (3). Indeed, high resolution manometry revealed a negative gradient in all 30 asymptomatic women aged ≤ 50 years (3). Hence, an abnormal rectal balloon expulsion test may be more useful than anorectal manometry for diagnosing DD. Indeed, in one study, an abnormal balloon expulsion test was 88% sensitive and 89% specific for identifying pelvic floor dysfunction compared to defecography (6). However, the positive predictive value of an abnormal balloon expulsion test versus defecography, albeit an imperfect criterion standard for DD, was only 64% (6, 7). Hence, it is necessary to explore alternative approaches to enhance the utility of a rectal balloon expulsion test for diagnosing DD.
In the original description, rectal balloon expulsion was evaluated in the left lateral position (8), which is similar to anorectal manometry. Currently, rectal balloon expulsion is typically evaluated by measuring the time required for patients to expel a rectal balloon in the seated position (2). Conceivably, evaluating rectal balloon expulsion in the left lateral position may result in false-positive results since this position is not physiological. However, anorectal manometry is also conducted in the left lateral position. Moreover, gravity might be anticipated to aid expulsion in the seated but not in the left lateral position. Indeed, intraabdominal pressure is higher in the seated than in the recumbent position (9). It is conceivable that gravity or a higher BMI, which is associated with increased abdominal pressure [16], may facilitate balloon expulsion in the seated position even in patients with pelvic floor dysfunction resulting in a “false negative” test. Hence, the aims of this study were to compare balloon expulsion in the left lateral and seated positions, to compare anorectal pressures measured by manometry in the left lateral position with rectal balloon expulsion evaluated in the seated and left lateral positions. We also sought to assess the relationship between BMI and balloon expulsion, and to evaluate the utility of symptoms for predicting the results of rectal balloon expulsion. Our primary hypotheses were that (i) there is significant agreement between the results of rectal balloon expulsion in the seated and left lateral positions; (ii) patients with abnormal balloon expulsion only in the left lateral position also have manometric evidence of rectoanal dysfunctions; and (iii) a higher proportion of patients with abnormal balloon expulsion in both positions will have symptoms suggestive of disordered evacuation (e.g., anal digitation).
METHODS
Study Design
These studies were approved by the Institutional Review Board at Mayo Clinic. Between August 2010 and September 2011, 158 women (age 51 ± 1.3 years, Mean ± SEM) with chronic constipation were referred for assessment of anorectal functions with manometry with a rectal balloon expulsion test in left lateral and seated positions, provided research authorization, and completed questionnaires. Of 158 patients, 142 had symptoms of chronic constipation and 16 had symptoms of constipation-predominant IBS. In addition, 62 healthy asymptomatic women aged 21 to 80 years (44 ± 2.1 years, Mean ± SEM) were recruited by public advertisement. With the exception of 3 healthy subjects who reported hard stools only, no controls had any symptoms of constipation. All participants had a clinical interview and physical examination. The results of anorectal manometry in the left lateral position and rectal balloon expulsion test in the seated position have been detailed elsewhere (10). However, the results of rectal balloon expulsion test in the left lateral position and the other analyses presented herein have not been published previously.
Study Subjects
Healthy asymptomatic women and female patients were aged 18 to 85 years; only patients had Rome III symptom criteria for functional constipation or constipation-predominant IBS. Exclusion criteria included prior pelvic floor retraining, opiate use, diabetes mellitus, inflammatory bowel disease, full thickness rectal prolapse, and left colon surgery (e.g., total or subtotal colectomy, rectocele repair). However, patients who had other abdominal surgeries (e.g., right hemicolectomy, appendectomy, cholecystectomy or hysterectomy) were not excluded. Exclusion criteria for healthy participants included significant cardiovascular, respiratory, neurological, psychiatric or endocrine disease, functional bowel disorders as assessed by a validated bowel disease questionnaire (11), medications (with the exception of oral contraceptives or thyroid supplementation), and abdominal surgery (other than appendectomy, cholecystectomy or hysterectomy).
Procedures
Anorectal manometry
Anal pressures were assessed by a high-resolution anorectal manometry catheter (4.2-mm outer diameter; SierraScientific Instruments; Los Angeles, CA), in the left lateral position. This catheter comprises 10 circumferential sensors, i.e., 8 sensors at 6 mm intervals along the anal canal and 2 sensors in the rectal balloon. At each level, 36 circumferentially-oriented pressure-sensing elements detect pressure using proprietary pressure transduction technology (TactArray) over a length of 2.5 mm. The 36 sector pressures are then averaged to obtain a mean pressure measurement. The response characteristics of each sensing element are suchthat they can record pressure transients in excess of 6,000 mmHg/s and are accurate to within 1 mmHg of atmospheric pressure for measurements obtained for at least the final 5 min of thestudy, immediately before thermal recalibration. The data-acquisition frequency is 35 Hz for each sensor.
Each study comprised in the following chronological order an assessment of anorectal pressures at rest, during squeeze (3 attempts), and simulated evacuation with an empty rectal balloon. Thereafter the rectoanal inhibitory reflex and rectal sensation were simultaneously evaluated by progressively distending a rectal balloon in 20 ml increments from 0 to 200 ml and thereafter in 40 ml increments until a maximum volume of 400 ml or until patients reported severe urgency.
Rectal Balloon Expulsion Test
The balloon expulsion test was performed with subjects in left lateral and seated positions. The order of testing was randomized in controls but not in patients. In the left lateral position, the test was performed by asking subjects to expel a balloon filled with 50 mL of water. If subjects could not expel the balloon spontaneously, the balloon was connected over a pulley to external weights, starting with 50 gm and increasing, if subjects could not expel the balloon, in increments of 47 gm up to a maximum of 564 gm. The test was considered abnormal if more than 100 gm of external traction was required (12, 13). Thereafter, a 4 cm long latex balloon tied to a 2mm diameter plastic tubing was inserted into rectum and filled with 50 cc of warm water. The time required for balloon expulsion while subjects were seated on a commode in privacy was noted. No weights were added. The balloon was removed if subjects could not expel it in 3 minutes.
Barium and MR Proctography
Forty patients also had barium or MR proctography. Proctography assessed anorectal and pelvic floor motion during pelvic floor contraction and simulated defecation (14). The rectum was filled with barium paste (barium proctography) or 180 mL of ultrasound gel (MRI) (13, 15). The small intestine was also opacified with oral barium for barium proctography (14). Disordered defecation was identified by the presence of one or more of the following features during evacuation: reduced (i.e., < 2 cm) or increased perineal descent (> 4 cm for barium and > 5.1 cm for MRI), reduced (< 50%) rectal emptying, impaired puborectalis relaxation, enteroceles and significant rectoceles (i.e., ≥ 2 cm in size with incomplete emptying) (16).
Statistical Analysis
Agreement between balloon expulsion results (left lateral vs. seated), overall, and separately by subject status (patient vs. control) was assessed by the kappa (κ [95%CI]) coefficient. Because a low κ value may reflect a low prevalence of that trait in the cohort and not lack of agreement, the proportion of positive agreement was also calculated (17, 18). Associations between the rectal balloon expulsion test and bowel symptoms were assessed by a Kruskal Wallis test. An analysis of covariance was used to assess associations between the rectal balloon expulsion test and anorectal manometry variables; BMI and subject status were covariates. The relationships between BMI and anorectal variables as also between balloon expulsion weight and time were evaluated by Spearman’s correlation coefficient. A multiple variable logistic regression model (generalized logit link function) evaluated whether selected anorectal manometry variables (and BMI) could discriminate between the four rectal balloon expulsion groups: abnormal balloon expulsion in the left lateral position only, abnormal balloon expulsion in the seated position only, and abnormal balloon expulsion in both positions (the reference group being normal in both positions). Statistical significance was defined by a p value of less than 0.05.
RESULTS
Demographic Features
Based on the results of rectal balloon expulsion in both positions, subjects were categorized into 4 groups. Fifty five of 62 (89%) asymptomatic women and 86 of 158 (54%) patients had normal rectal balloon expulsion in both positions (Table 1). The age was comparable among these 4 groups. While the BMI was higher in patients with an abnormal balloon expulsion test in the seated position only, differences among groups were not significant.
Table 1.
Comparison of Symptoms and Anorectal Parameters among Groups Categorized by Results of Rectal Balloon Expulsion Test
| Normal seated and left lateral (n=141) | Normal seated and abnormal left lateral (n=30) | Abnormal seated and normal left lateral (n=17) | Abnormal seated and left lateral (n=32) | ||
|---|---|---|---|---|---|
| N (Healthy Participants) | N (Patients) | ||||
| N (Healthy Participants) | 55 | 2 | 3 | 2 | |
| N (Patients) | 86 | 28 | 14 | 30 | |
| Demographic Variables | |||||
| Age, years | 44.4 ± 2.1 | 54.6 ±1.8 | 45.3 ± 3.2 | 47.7 ± 3.9 | 45.6 ± 3 |
| BMI, kg/m2 | 25.5 ± 0.6 | 25.9 ±0.6 | 25.3 ±. 0.8 | 30.4 ± 2.3 | 26.3 ± 1.2 |
| Anorectal pressures | |||||
| Length of anal high pressure zone at rest (cm) | 3.6 ± 0.1 | 3.4 ± 0.1 | 3.5 ± 0.1 | 3.2 ± 0.2 | 3.5 ± 0.1 |
| Anal pressure – rest | 79 ± 3 | 73 ± 3 | 70 ± 4 | 79 ± 5 | 81 ± 4 |
| Anal pressure – squeeze | 167 ± 7 | 121 ± 5 | 127 ± 8 | 121 ± 10 | 140 ± 10 |
| Anal squeeze duration | 12 ± 1 | 13 ±1 | 14 ± 1 | 14 ± 2 | 13 ± 1 |
| Anal relaxation – simulated evacuation (%) | 33 ± 5 | 16 ± 3 | 1 ± 7 | 8 ± 6 | 3 ± 5 |
| Rectal pressure – simulated evacuation | 25 ± 3 | 29 ± 3 | 20 ± 4 | 22 ± 4 | 15 ± 2 |
| Anal pressure – simulated evacuation | 53 ± 4 | 58 ± 3 | 66 ± 4 | 71 ± 6 | 76 ± 4 |
| Rectoanal gradient – simulated evacuation | −25 ± 5 | −29 ± 3 | −46 ± 6 | −49 ± 9 | −58 ± 5 |
| Rectal sensory thresholds (ml) | |||||
| First sensation | 33 ± 1 | 34 ± 4 | 36 ± 7 | 32 ± 3 | 35 ± 4 |
| Desire to defecate | 56 ± 2 | 58 ± 4 | 61 ± 7 | 65 ± 11 | 78 ± 8 |
| Urgency | 90 ± 4 | 88 ± 5 | 82 ± 8 | 101 ± 17 | 123 ± 13 |
All values are in mmHg except where stated otherwise.
Rectal Balloon Expulsion Test
In 173/220 subjects (79%), the results of rectal balloon expulsion in the seated and left lateral positions were in agreement, i.e. normal (141 subjects) or abnormal (32 subjects) in both positions. For this comparison, the mean κ value was 0.44 [95% CI, 0.30, 0.57], which indicates modest agreement. In the remaining 21%, results were discordant i.e. only abnormal in the left lateral (30 subjects) or seated position (17 subjects) (Table 1). Of note, test results were in agreement in 57/62 (92%) controls with a κ of 0.40 (95% CI −0.02, 0.83) and in 116/158 (73%) patients (κ of 0.40 [95% CI 0.25, 0.55]). Balloon expulsion times (seated position) and weights (left lateral position) expressed as continuous variables were also correlated (r = 0.46, p < 0.0001).
Relationship between Anorectal Pressures and Balloon Expulsion
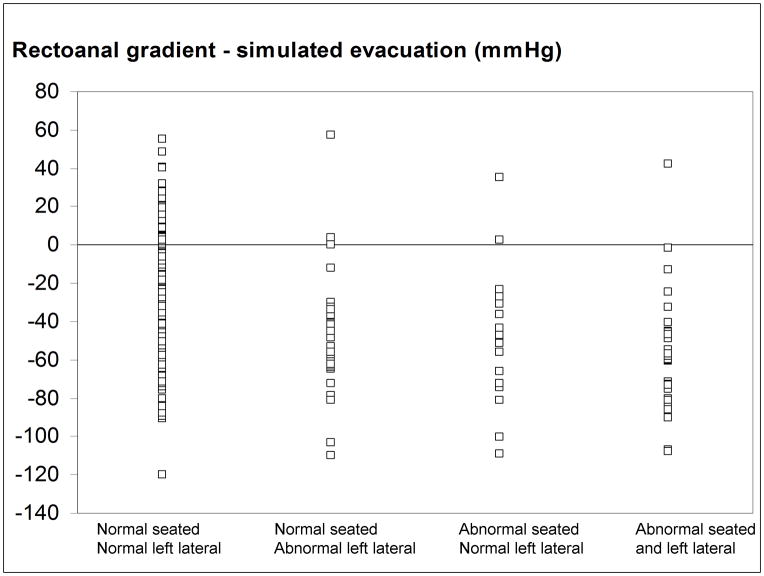
Table 1 provides anorectal pressures and rectal sensory thresholds in 4 groups categorized by rectal balloon expulsion. Among patients with normal rectal balloon expulsion in the seated and left lateral positions, values for anorectal parameters in healthy participants and patients are very similar. The univariate association between balloon expulsion group and anal resting and squeeze pressures, length of high pressure zone, and anal squeeze duration was not significant (Table 1). During simulated evacuation, (i) patients with abnormal expulsion in both positions had lower rectal pressure (p = 0.058, Kruskal Wallis test); (ii) patients with abnormal balloon expulsion in either and both positions had less anal relaxation, higher anal pressures, and a more negative rectoanal gradient than subjects with normal balloon expulsion in both positions; these variables were all associated (p ≤ 0.0004) with group status (Figure 1); and (iii) BMI was associated with rectal pressure (r = 0.25, p = 0.0002), but not with anal pressure or the rectoanal gradient.
Figure 1. Comparison of rectoanal gradient during simulated evacuation versus balloon expulsion.
The rectoanal gradient was invariably negative in subjects with abnormal rectal balloon expulsion in one or both positions. However, there is considerable overlap among groups.
Relationship between Rectal Sensation and Balloon Expulsion
The rectal sensory threshold for first sensation was not significantly associated with balloon expulsion (Table 1). However, compared to patients with normal balloon expulsion in both positions, the threshold for the desire to defecate was higher in patients with abnormal balloon expulsion in one position and more so with abnormal balloon expulsion in both positions, the association between balloon expulsion category and group status was significant (p = 0.03). A similar pattern was observed for the urgency threshold but the association (p = 0.07) with group status was not significant.
Multiple Variable Predictor Model for Predicting Rectal Balloon Expulsion
Relative to the reference group (i.e., subjects with normal balloon expulsion in both positions) (Table 2) (i) a higher BMI was associated (OR 1.11, 95% CI 1.03 – 1.21) with abnormal balloon expulsion in the seated position only, (ii) higher rectal pressure during simulated evacuation was associated with a lower (OR 0.96, 95% CI 0.93 – 0.98) risk of abnormal balloon expulsion in both positions, (iii) greater anal relaxation during simulated evacuation was associated with a lower risk (OR 0.98, 95% CI 0.96 – 0.99) of abnormal balloon expulsion in the left lateral position only, and (iv) higher anal pressure during simulated evacuation (OR 1.02, 95% CI 1.00–1.04) and a higher rectal sensory threshold for the desire to defecate had an increased risk (OR 1.01, 95% CI 1.00–1.02) of abnormal balloon expulsion in both positions. These statistically significant OR were numerically small.
Table 2.
Multiple variable Logistic Regression Models for Rectal Balloon Expulsion Test in Seated and Left Lateral Positions.
| Variable | OR (95% CI) for normal seated and abnormal left lateral | OR (95% CI) for abnormal seated and normal left lateral | OR (95% CI) for abnormal seated and left lateral |
|---|---|---|---|
| BMI (per unit) | 0.99 (0.91–1.07) | 1.11 (1.03–1.21)* | 1.04 (0.96 –1.12) |
| Rectal pressure – simulated evacuation (per mmHg) | 0.97 (0.95–1.00) | 0.98 (0.95–1.01) | 0.96 (0.93–0.98)* |
| Anal pressure – simulated evacuation | 1.00 (0.98–1.02) | 1.02 (0.99–1.05) | 1.02 (1.00–1.04)* |
| Anal relaxation – simulated evacuation (%) | 0.98 (0.96–0.99)* | 0.99 (0.97–1.02) | 0.98 (0.97–1.00) |
| Rectal sensory threshold - desire to defecate | 1.00 (0.98–1.01) | 1.00 (0.99–1.02) | 1.01 (1.00–1.02)* |
All odds ratios (OR) are expressed in comparison to the reference group (i.e., normal balloon expulsion in seated and left lateral positions).
p<0.05
Barium and MR Proctography
Forty patients (18%) had defecating (23 patients) or MR proctography (17 patients). Among these patients, 23 and 6 patients had normal and abnormal balloon expulsion respectively in both positions while 7 and 4 had abnormal balloon expulsion in left lateral and seated positions only, respectively. Nineteen of 23 patients had an abnormal defecating proctogram; predominant findings included impaired evacuation (7 patients), an enterocoele and/or increased perineal descent (8 patients) or a significant rectocele (4 patients). MR proctography revealed pelvic floor dysfunction in 13 patients. Predominant findings included impaired evacuation (4 patients), enterocoele and/or increased perineal descent (6 patients) or a significant rectocele (3 patients). Taken together, MR or defecating proctography disclosed features of disordered defecation in 19 patients with normal balloon expulsion in both positions, 6 patients with abnormal left lateral balloon expulsion only, 3 with abnormal seated balloon expulsion only, and 4 with abnormal balloon expulsion in both positions.
Relationship between Symptoms and Balloon Expulsion
Individual symptoms of constipation, including symptoms suggestive of a defecatory disorder (e.g., sense of anorectal blockage during defecation), were not significantly associated with balloon expulsion categories. While a higher proportion (43%) of patients with abnormal rectal balloon expulsion in the seated and separately, in both positions, reported anal digitation than patients who had normal rectal balloon expulsion in both positions (22%), these differences were not significant (p = 0.08) (Table 3).
Table 3.
Comparison of Bowel Symptoms in Patients by Rectal Balloon Expulsion Categories
| Symptom | Normal Left lateral and Seated (n=86) | Normal Seated and Abnormal Left lateral (n=28) | Abnormal seated and normal left lateral (n=14) | Abnormal Left lateral and Seated (n=30) |
|---|---|---|---|---|
| Reduced stool frequency | 38 (44%) | 20 (71%) | 9 (64%) | 19 (63%) |
| Hard stools | 57 (66%) | 23 (82%) | 10 (71%) | 24 (80%) |
| Excessive straining | 61 (71%) | 25 (89%) | 11 (79%) | 22 (73%) |
| Sense of incomplete evacuation | 66 (77%) | 22 (79%) | 12 (86%) | 24 (80%) |
| Anorectal blockage | 54 (63%) | 19 (68%) | 10 (71%) | 24 (80%) |
| Anal digitation | 19 (22%) | 3 (11%) | 6 (43%) | 13 (43%) |
DISCUSSION
There is limited concurrence between anorectal manometry and the rectal balloon expulsion test for identifying pelvic floor dysfunction (3, 10, 19). To what extent this disagreement is attributable to differences in body position during these 2 tests is unclear. There are 2 main findings in this study. First, the results of evaluating rectal balloon expulsion in the seated and left lateral positions were concordant (i.e., the test was normal or abnormal in both positions) in 79% of people and the κ statistic indicated modest agreement. Of note, in controls, the lower bound of the 95th percentile CI for this κ crossed zero despite substantial agreement because the κ can be low when the prevalence of a trait, in this instance an abnormal balloon expulsion test in asymptomatic subjects, is low (17, 18). Second, the rectoanal gradient during simulated evacuation was even negative in asymptomatic subjects and progressively more negative in subjects who had abnormal rectal balloon expulsion in left lateral only, seated only, and both positions respectively. These observations suggest a gradient of anorectal dysfunctions during evacuation ranging from least, in patients with normal rectal balloon expulsion in both positions, to most, in patients with abnormal rectal balloon expulsion in both positions.
Two prior studies evaluated the effects of body position on rectal evacuation (8, 19). The first study, which was conducted in 15 healthy subjects and 31 constipated patients, evaluated balloon expulsion was evaluated in the left lateral position in all subjects and thereafter in the seated position only in subjects who could not expel a balloon in the left lateral position (8). Because balloon expulsion was not evaluated in both positions in all subjects, the assessment of concordance between left lateral and seated positions was incomplete. The second study by Rao et al evaluated rectal expulsion of balloon and a stool substitute as also rectoanal pressures during evacuation in both positions in 25 healthy subjects but not in constipated patients (19). Both these studies used traditional (water-perfused or solid state). This study used high-resolution manometry catheters, which have sensors that straddle the entire anal canal but traditional catheters do not. Hence, high-resolution catheters may be more accurate for characterizing anal pressures during evacuation.
Confirming the original description of the rectal balloon expulsion test, most (55 of 62) asymptomatic subjects in the present study expelled the balloon in the left lateral position (8). In contrast to healthy subjects, only 5 of 31 constipated patients could expel a balloon in the left lateral position; however 11 of 31 could in the seated position. Likewise, in the present study, approximately 50% of controls and separately 50% of patients who were unable to expel a balloon in the left lateral position could expel it in the seated position. While we did not evaluate rectoanal pressures in the seated position, Rao et al studied rectal expulsion of balloon and a stool substitute as also rectoanal pressures during evacuation in the left lateral and seated positions in 25 healthy subjects (19). The key finding was that rectal pressures and the rectoanal gradient during evacuation were higher in the seated than the left lateral position. However, dyssynergia did not explain abnormal balloon expulsion. Nonetheless, taken together, these findings suggest that higher rectal and lower anal pressures during simulated evacuation in the seated than in the left lateral position may explain, at least in part, why some subjects who cannot expel a balloon in the left lateral position can do so in the seated position (8, 19). Even the pelvic floor is lower, probably due to gravity and intraabdominal pressure exerted by viscera, in the seated than the left lateral positions (20). Thus, it is conceivable that in patients with increased perineal laxity, the effects of gravity and intra-abdominal pressure somehow overcome pelvic floor dysfunction during the balloon expulsion test. Indeed, 5 of 6 patients who had barium or MR proctography in this group had proctographic features of disordered defecation, of which 4 had an enterocoele or increased perineal descent. Moreover, the anorectal gradient during simulated evacuation was more negative in patients with abnormal balloon expulsion in the left lateral position only than in subjects with normal balloon expulsion in both positions. Taken together, these observations suggest that at least some patients with abnormal balloon expulsion in the left lateral position only have a defecatory disorder. Assessing rectal balloon expulsion test in the left lateral position may be useful for identifying pelvic floor dysfunction particularly in patients with increased perineal descent. Other studies have also documented normal balloon expulsion in the seated position in patients with an evacuation disorder documented by another technique. For example, 3 of 24 patients (12.5%) with pelvic floor dysfunction by defecography had normal BE in the seated position (6). Likewise Bordeianou et al reported that 30 of 63 patients with dyssynergia and impaired rectal evacuation during defecography had normal rectal balloon expulsion in the seated position (21). Together, these findings suggest that normal balloon expulsion in the seated position does not always exclude an evacuation disorder.
In the multiple variable predictor model, patients with abnormal rectal balloon expulsion in both positions had higher anal pressures during rectal evacuation and reduced rectal sensation relative to patients with normal rectal balloon expulsion in both positions. However, the odds ratios for these parameters were very close to unity, suggesting that anorectal pressures during simulated evacuation and rectal sensory thresholds are not particularly useful for predicting the results of a rectal balloon expulsion test. One limitation of this approach is that the results of multiple variable predictor models are influenced by correlations among predictor variables (e.g., between anal resting and squeeze pressures) which can adversely affect, forward or backward elimination variable selection methods. These effects can be mitigated by using an alternative approach (i.e., principal components analysis), which transforms variables to uncorrelated dimensions that may represent independent physiological domains. Indeed a principal components analysis of anorectal variables in this dataset identified 3 discrete patterns, represented by high anal pressures during evacuation, low rectal pressures during evacuation, and a combination of low rectal and high anal pressures during evacuation, which discriminated between subjects with normal and abnormal rectal balloon expulsion (10).
Rectal and anal pressures during evacuation were similar in patients with abnormal rectal balloon expulsion in the seated position only and abnormal rectal balloon expulsion in both positions. However, in contrast to patients with abnormal balloon expulsion in both positions, these anorectal variables were not useful for predicting abnormal seated balloon expulsion only perhaps because the sample size in this group was small. Of interest, patients in this group had the highest BMI of all groups. Moreover BMI was positively correlated with rectal pressures during simulated evacuation. Since rectal pressures partly reflect intra-abdominal pressure, this observation is consistent with a systematic review, which observed that intra-abdominal pressures were higher, averaging 9–14 mmHg, in morbidly obese patients than in non-obese subjects (i.e., average of 5–7 mmHg) [16]. While the evidence for increased intra-abdominal pressure in overweight subjects is mixed, two studies suggest that obesity is also associated with a higher intra-abdominal pressure. The increase in intra-abdominal pressure in the upright relative to the left lateral position is also more pronounced in morbid obesity suggesting that the abdominal cavity may function as a hydraulic system in which intra-abdominal contents may exert pressure on pelvic viscera. To the extent that intra-abdominal pressure is transmitted to the rectum, rectal pressure during evacuation, particularly in the seated position, should be higher in obese subjects. Hence, the association between higher BMI and abnormal balloon expulsion in the seated position only is somewhat counterintuitive. Further studies are necessary to ascertain if increased intra-abdominal pressure in obese subjects distorts pelvic anatomy and impedes balloon expulsion, more so in the seated position, in obese subjects.
While the rectoanal gradient during simulated evacuation was measured with an empty balloon and rectal balloon expulsion was performed with an inflated balloon. we previously observed that the relationship between this gradient and rectal BET in healthy subjects was similar regardless of whether the gradient was measured with an empty or an inflated balloon (3, 4).
Patients with abnormal balloon expulsion in both positions had a higher rectal sensory threshold for the desire to defecate, which suggests reduced rectal sensation. Reduced rectal sensation in defecatory disorders may be primary or secondary to increased compliance (22, 23). Because reduced rectal sensation may affect rectal evacuation, Minguez et al recommended that the balloon be inflated until patients perceive the desire to defecate during a rectal balloon expulsion test (6). In that study, the balloon was inflated to an average volume of 185 ml. However, some people may find it more difficult to expel a larger balloon. For example, in 1 study only 6 of 8 subjects who expelled a 50 ml balloon were able to expel 100 and 150 ml balloons (8). The main weaknesses of this study are that evacuation proctograms were only performed in a minority of patients and that the rectoanal gradient during evacuation was only evaluated in the left lateral and not in the seated position. The assessors were not blinded to subject status. Report bias is possible but seems unlikely given the nature of these objective assessments. Since the order of balloon expulsion testing (i.e., left lateral versus seated positions) was not randomized in patients, it is conceivable the outcome in the seated position was influenced prior testing in the left lateral position. However, 52% of patients who could not expel the balloon in the left lateral position were unable to expel the same in the seated position, which argues against a systematic bias. Only a subset of patients had proctography, which was performed with barium in some and with MRI in other patients. Because a proctogram was only obtained in a minority of patients, we do not know if the proportion of patients who had disordered defecation by proctography was significantly different among balloon expulsion categories. The correlation between dynamic MRI and colposystoproctography for quantifying prolapse in all three pelvic floor compartments (anterior, middle, and posterior) is excellent (24). However, subtle or transitory intussusception or prolapse may not be evident on MRI (25).
In summary, there is modest agreement between rectal balloon expulsion tests performed in the left lateral and seated positions. Relative to subjects with normal balloon expulsion in both positions, the rectoanal gradient during simulated evacuation was progressively more negative in patients with abnormal balloon expulsion in left lateral only, seated only, and both positions. Proctography demonstrated disordered defecation, notably excessive perineal descent, in some subjects who had abnormal balloon expulsion in the left lateral position only. Taken together, these findings suggest that evaluating rectal balloon expulsion in the seated position probably suffices for identifying DD in a majority of patients. However, among patients with a high clinical index of suspicion for DD but normal balloon expulsion in the seated position, consideration should be given to also assessing balloon expulsion in the left lateral position if feasible, particularly in patients with increased perineal descent.
Acknowledgments
This study was supported in part by USPHS NIH Grants R01 DK78924.
Footnotes
Contributions
Shiva Ratuapli, M.D. - analysis and interpretation of data; drafting of the manuscript
Adil E. Bharucha, M.D. - study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content
Doris Harvey, R.N1. - acquisition of data
Alan R. Zinsmeister, PhD2. - statistical analysis
Competing Interests: The authors have no competing interests.
None of the authors have conflicts of interests.
References
- 1.Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006;130:1510–1518. doi: 10.1053/j.gastro.2005.11.064. [DOI] [PubMed] [Google Scholar]
- 2.Bharucha AE, Wald AM. Anorectal disorders. American Journal of Gastroenterology. 2010;105:786–794. doi: 10.1038/ajg.2010.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noelting J, Ratuapli SK, Bharucha AE, Harvey D, Ravi K, Zinsmeister AR. Normal Values For High-Resolution Anorectal Manometry In Healthy Women: Effects Of Age And Significance Of Rectoanal Gradient. American Journal of Gastroenterology. 2012;107:1530–1536. doi: 10.1038/ajg.2012.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bharucha AE. Difficult defecation: difficult problem assessment and management; what really helps? Gastroenterology Clinics of North America. 2011;40:837–844. doi: 10.1016/j.gtc.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. American Journal of Gastroenterology. 1998;93:1042–1050. doi: 10.1111/j.1572-0241.1998.00326.x. [DOI] [PubMed] [Google Scholar]
- 6.Minguez M, Herreros B, Sanchiz V, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology. 2004;126:57–62. doi: 10.1053/j.gastro.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 7.Noelting J, Bharucha AE, Lake DS, et al. Semi-automated vectorial analysis of anorectal motion by magnetic resonance defecography in healthy subjects and fecal incontinence. Neurogastroenterol Motil. 2012;24:e467–475. doi: 10.1111/j.1365-2982.2012.01962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnes PR, Lennard-Jones JE. Balloon expulsion from the rectum in constipation of different types. Gut. 1985;26:1049–1052. doi: 10.1136/gut.26.10.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Keulenaer BL, De Waele JJ, Powell B, Malbrain MLNG. What is normal intra-abdominal pressure and how is it affected by positioning, body mass and positive end-expiratory pressure? Intensive Care Medicine. 2009;35:969–976. doi: 10.1007/s00134-009-1445-0. [DOI] [PubMed] [Google Scholar]
- 10.Ratuapli S, Bharucha AE, Noelting J, Harvey D, Zinsmeister AR. Phenotypic Identification and Classification of Functional Defecatory Disorders Using High Resolution Anorectal Manometry. Gastroenterology. 2013;144:314–322. doi: 10.1053/j.gastro.2012.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bharucha AE, Locke GR, Seide B, Zinsmeister AR. A New Questionnaire for Constipation and Fecal Incontinence. Alimentary Pharmacology & Therapeutics. 2004;20:355–364. doi: 10.1111/j.1365-2036.2004.02028.x. [DOI] [PubMed] [Google Scholar]
- 12.Pezim ME, Pemberton JH, Levin KE, Litchy WJ, Phillips SF. Parameters of anorectal and colonic motility in health and in severe constipation. Dis Colon Rectum. 1993;36:484–491. doi: 10.1007/BF02050015. [DOI] [PubMed] [Google Scholar]
- 13.Bharucha AE, Fletcher JG, Seide B, Riederer SJ, Zinsmeister AR. Phenotypic Variation in Functional Disorders of Defecation. Gastroenterology. 2005;128:1199–1210. doi: 10.1053/j.gastro.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 14.Diamant NE, Kamm MA, Wald A, Whitehead WE. American Gastroenterological Association Medical Position Statement on Anorectal Testing Techniques. Gastroenterology. 1999;116:732–760. doi: 10.1016/s0016-5085(99)70194-0. [DOI] [PubMed] [Google Scholar]
- 15.Bharucha AE, Fletcher JG. Recent advances in assessing anorectal structure and functions. Gastroenterology. 2007;133:1069–1074. doi: 10.1053/j.gastro.2007.08.051. [DOI] [PubMed] [Google Scholar]
- 16.Bharucha AE. Update of tests of colon and rectal structure and function. Journal of Clinical Gastroenterology. 2006;40:96–103. doi: 10.1097/01.mcg.0000196190.42296.a9. [DOI] [PubMed] [Google Scholar]
- 17.Cicchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving the paradoxes. Journal of Clinical Epidemiology. 1990;43:551–558. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- 18.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. Journal of Clinical Epidemiology. 1990;43:543–549. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- 19.Rao SSC, Kavlock R, Rao S. Influence of body position and stool characteristics on defecation in humans. American Journal of Gastroenterology. 2006;101:2790–2796. doi: 10.1111/j.1572-0241.2006.00827.x. [DOI] [PubMed] [Google Scholar]
- 20.Habib FI, Corazziari E, Viscardi A, Badiali D, Torsoli A. Role of body position, gender, and age on pelvic floor location and mobility. Digestive Diseases & Sciences. 1992;37:500–505. doi: 10.1007/BF01307570. [DOI] [PubMed] [Google Scholar]
- 21.Bordeianou L, Savitt L, Dursun A. Measurements of pelvic floor dyssynergia: which test result matters? Diseases of the Colon & Rectum. 2011;54:60–65. doi: 10.1007/DCR.0b013e3181fd2373. [DOI] [PubMed] [Google Scholar]
- 22.Gladman MA, Lunniss PJ, Scott SM, Swash M. Rectal hyposensitivity. American Journal of Gastroenterology. 2006;101:1140–1151. doi: 10.1111/j.1572-0241.2006.00604.x. [DOI] [PubMed] [Google Scholar]
- 23.Gladman MA, Dvorkin LS, Lunniss PJ, Williams NS, Scott SM. Rectal hyposensitivity: a disorder of the rectal wall or the afferent pathway? An assessment using the barostat. American Journal of Gastroenterology. 2005;100:106–114. doi: 10.1111/j.1572-0241.2005.40021.x. [DOI] [PubMed] [Google Scholar]
- 24.Kelvin FM, Maglinte DD, Hale DS, Benson JT. Female pelvic organ prolapse: a comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. American Journal of Roentgenology. 2000;174:81–88. doi: 10.2214/ajr.174.1.1740081. [DOI] [PubMed] [Google Scholar]
- 25.Kaufman HS, Buller JL, Thompson JR, et al. Dynamic pelvic magnetic resonance imaging and cystocolpoproctography alter surgical management of pelvic floor disorders. Diseases of the Colon & Rectum. 2001;44:1575–1583. doi: 10.1007/BF02234374. discussion 1583–1574. [DOI] [PubMed] [Google Scholar]