Abstract
Importance
With growing national focus on reducing readmissions, there is a need to comprehensively assess the quality of transitional care, including discharge practices, patient perspectives, and patient understanding.
Objective
To conduct a multifaceted evaluation of transitional care from a patient-centered perspective.
Design
Prospective observational cohort study, May 2009-April, 2010
Setting
Urban, academic medical center
Participants
Patients 65 and older discharged home after hospitalization for acute coronary syndrome, heart failure or pneumonia.
Main outcome measures
Discharge practices, including presence of follow-up appointment and patient-friendly discharge instructions; patient understanding of diagnosis and follow-up appointment; and patient perceptions of and satisfaction with discharge care.
Results
The 395 enrolled patients (66.7% of eligible) had a mean age of 77.2 years. Although 349 (95.6%) patients reported understanding the reason they had been in the hospital, only 218 (59.6%) patients were able to accurately describe their diagnosis in post-discharge interviews. Discharge instructions routinely included symptoms to watch out for (98.4%), activity instructions (97.3%) and diet advice (89.7%) in lay language; however, 99 (26.3%) written reasons for hospitalization did not use language likely to be intelligible to patients. Of the 123 (32.6%) patients discharged with a scheduled primary care or cardiology appointment, 54 (43.9%) accurately recalled details of either appointment. During post-discharge interviews, 118 (30.0%) of patients reported receiving less than one day’s advance notice of discharge, and 246 (66.1%) reported that staff asked if they would have the support they needed at home before discharge.
Conclusions
Patient perceptions of discharge care quality and self-rated understanding were high and written discharge instructions were generally comprehensive though not consistently clear. However, follow-up appointments and advance discharge planning were deficient, and patient understanding of key aspects of post-discharge care was poor. Patient perceptions and written documentation do not adequately reflect patient understanding of discharge care.
Keywords: discharge process, follow up appointment, patient understanding, transition of care, quality assessment, heart failure, acute MI, pneumonia
Introduction
In 2013, approximately two thirds of US hospitals will suffer financial penalties from the Centers for Medicare and Medicaid Services (CMS) because of excessively high 30-day readmission rates after hospitalizations for acute myocardial infarction, heart failure and pneumonia.1 There has been a corresponding groundswell of interest on the part of hospitals in improving transitions of care. Nonetheless, not only are the best strategies for improving transitions still uncertain,2 comprehensive assessments of transition quality are also still lacking.
Safely transitioning patients from hospital to home is a complex process that requires successfully completing a number of tasks, from coordinating care with outside physicians to educating patients.3 In part related to the complexity of this transition, the adverse event rate post-hospital discharge is high, even apart from readmissions.4 Evaluation of hospital discharge practice has often focused on chart documentation of specific processes5,6 and more recently, on patient satisfaction with discharge care.7 Although these assessments are important, simply documenting that information is conveyed or that patients are satisfied with practice may not be a sufficient measure of transition success. A successful transition also depends on whether hospitals have adequately educated patients about key elements of care such as diagnosis and follow-up plans.8
A safe and patient-centered passage from the hospital should therefore include consistent and high quality provision of transitional care (e.g., follow-up appointments, comprehensive and intelligible discharge instructions),9,10 should ensure that patients understand key aspects of the transition, and should be patient-centered (e.g., provide adequate notice of and preparation for discharge, result in high levels of satisfaction). Although studies have been conducted of individual aspects of the patient experience (for example, patient understanding of medication changes,11–15 or proportion of patients discharged with follow-up appointments10), we lack a comprehensive assessment incorporating all three domains of process, understanding and patient-centeredness.
To address these issues, we conducted the DIagnosing Systemic failures, Complexities and HARm in GEriatric discharges (DISCHARGE) study of older patients discharged to the community after hospitalization for three common conditions – heart failure, pneumonia, and acute coronary syndrome. We studied the comprehensiveness and quality of hospital discharge practices, determined understanding of diagnosis and post-discharge follow-up compared to chart data, and assessed patient or caregiver satisfaction.
Methods
Study cohort
The DISCHARGE study was a prospective, observational cohort study of patients 65 years or older discharged to home from a medicine service at Yale-New Haven Hospital (YNHH) between May 1, 2009 and April 4, 2010 who were admitted with acute coronary syndrome (ACS), heart failure (HF), or pneumonia. We defined ACS as unstable angina, non-ST elevation myocardial infarction, or ST elevation myocardial infarction. We followed the American College of Cardiology/American Heart Association 2007 guidelines for unstable angina and non-ST elevation myocardial infarction: chest pain (or anginal equivalent) plus positive biomarkers or EKG changes. For ST elevation myocardial infarction we used the European Society of Cardiology and American College of Cardiology definition; in brief: elevated troponin, and ischemic EKG changes or positive imaging. We defined heart failure using the 2008 European Society of Cardiology guidelines; in brief: the presence of symptoms and of signs typical of heart failure, and objective evidence of a structural of functional abnormality of the heart at rest. We defined pneumonia using the American Thoracic Society 2007 guideline of a demonstrable infiltrate by chest radiograph or other imaging technique and suggestive clinical features such as cough, fever, sputum production, pleuritic chest pain, rales, and bronchial breath sounds.16–19
On a daily basis, physicians reviewed the admission note and/or sign-out note for all new admissions to the medical service of patients over 64 years in order to identify eligible patients. Eligible patients had one of the three target conditions, spoke English or Spanish, and were not enrolled in hospice care. In addition, patients were ineligible to participate if they failed the mini-COG mental status screen20 while in the hospital. All patients determined at this stage to be eligible for the study were telephoned at home within one week of discharge. A maximum of five attempts were made to reach patients. At this time, some additional patients who appeared confused or delirious during the telephone interview or who did not speak English or Spanish were found to be ineligible. In these cases, caregivers of patients were asked to enroll instead if the patient provided permission. After the interviews were completed, physicians conducted chart reviews of the patients and determined that the diagnosis for some patients had changed during hospitalization (i.e., some patients initially categorized as pneumonia were later determined to have COPD exacerbation instead). We therefore post-hoc excluded some additional patients on the basis of not meeting diagnosis eligibility criteria.
Eligible patients were interviewed by telephone within one week of discharge, at which time they were consented for participation in the telephone interview and at the same time, separately, for permission to review charts. The Yale Human Investigation Committee approved the study and we obtained verbal informed consent from all study participants.
Study setting
At the time of the study, YNHH was a 944-bed urban, tertiary care hospital with statistically lower than national average mortality for all three target conditions, but statistically higher than average 30-day readmission rates for pneumonia and heart failure. Patients with pneumonia were admitted to the general medicine service and were cared for either by hospitalist attending physicians and physician assistants or nurse practitioners (“hospitalist team”), or by house staff under the supervision of university attending physicians (“house staff team”). Patients with acute coronary syndrome or heart failure may have been admitted to a specialized cardiology service or to a general medicine service. All patients received a printed discharge instruction sheet jointly produced by physicians and nurses (Appendix A). This discharge instruction sheet was reviewed with the patient by the nurse prior to discharge and includes information on diagnosis, medications, appointments and symptoms to monitor. There was no standard “teach-back” practice for patient education.
Data collection
Upon enrollment (within one week of discharge), patients or caregivers underwent a telephone interview by trained, non-clinical personnel. Experienced nurse abstractors reviewed the medical charts of those who consented. Chart review included review of the signed copy of the discharge instructions given to patients prior to discharge.
The interview included approximately 50 questions, addressing diagnosis, discharge instructions, communication with primary physicians, arrangement of follow-up appointments, understanding of medications, and patient education (Appendix B). Where available, we used standardized, validated questions, including the 3-Item Care Transitions Measure® (CTM-3) for assessment of patient perceptions about discharge process, and the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) questions about discharge education.21
Measures
To assess the quality of the discharge process, we assessed: 1) whether an appointment was made for the patient before discharge, 2) whether reason for hospitalization included any language likely to be intelligible to patients (defined below), 3) whether recommendations for diet and activity were written in lay language (e.g., no credit for “cardiac diet” or “2g Na diet”), 4) whether appropriate “call your doctor” instructions were provided, 5) patient report of amount of notice before discharge, and 6) perceived adequacy of home services. In large part, these were based on national standards and guidelines.22 To define “intelligible language,” we recorded every reason for hospitalization, and all study investigators collectively categorized them. Disagreements were resolved through iterative discussion. We defined intelligible language for hospitalization reason as: any term that was commonly used in spoken English (e.g., pneumonia, heart attack), any medical jargon for chronic diseases that we felt patients would likely be familiar with (e.g., CHF, COPD, atrial fibrillation), and any medical jargon for acute events that was commonly used by patients in the study to describe their hospitalization (e.g., catheterization). Remaining terms were defined as medical jargon (Appendix C). We describe accuracy of medication reconciliation and quality of discharge summary documentation in separate reports.23,24
Our measures of patient understanding were self-assessment of understanding key post-discharge care (reason for hospitalization, self-care, follow-up appointments, who to call with questions, and symptoms to watch for), and verified understanding of reason for hospitalization and post-discharge appointments, compared to chart documentation. To determine patient understanding of discharge diagnosis we compared patient’s responses to the question “please tell me the reason you were in the hospital” with administrative billing data of principal diagnosis, the wording in the diagnosis section of the discharge instructions, and our assignment of the patient to HF, pneumonia or ACS cohorts. If the patient had several main diagnoses, we credited description of any of them. We considered patient understanding of discharge diagnosis to be complete if the patient’s language would make it clear to a medical professional what the diagnosis for the hospitalization was. We considered patient understanding of diagnosis to be partially complete if the patient could identify non-specific symptoms consistent with the discharge diagnosis (for example, for heart failure, “breathing problem,” “problem with heart”), and we considered patient understanding to be lacking if they provided vague or unspecified symptoms, an incorrect diagnosis, or reported they did not know (Appendix E). We considered patient report of an appointment to be fully accurate if the patient report matched at least two of the name, date or time of an appointment on the discharge instructions; partially accurate if patient report matched one; and inaccurate if an appointment was listed in the discharge instructions but the patient reported no follow-up (Appendix D). We gave credit for highest level of understanding of either the primary care or cardiology follow-up appointment. We described patient understanding of medication changes in a separate report.25
Our measures of patient-centered care were patient satisfaction with: preparation for discharge, discharge care (including the CTM-3), discharge instructions, and post-discharge needs assessment. The CTM-3 includes three questions: whether patient/family preferences were taken into account in discharge planning, whether patients understand post-discharge self-care needs, and whether patients understand the purpose of each of their medications. It is scored on a 1–100 scale with higher scores indicating better quality.26,27
Statistical analysis
We double-abstracted 18 charts to determine reliability of coding practices. We used descriptive statistics to report measures of discharge process quality, patient understanding and patient perceptions. We constructed word clouds of the 30 most common phrases used by physicians and of the 100 most common phrases used by patients to describe the reason for hospitalization using Wordle™ (www.wordle.net). Word clouds represent frequency by font size. We dichotomized questions about patients’ perceived understanding into agree (strongly agree and agree) versus disagree (strongly disagree and disagree). All analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
Results
Enrollment and study sample
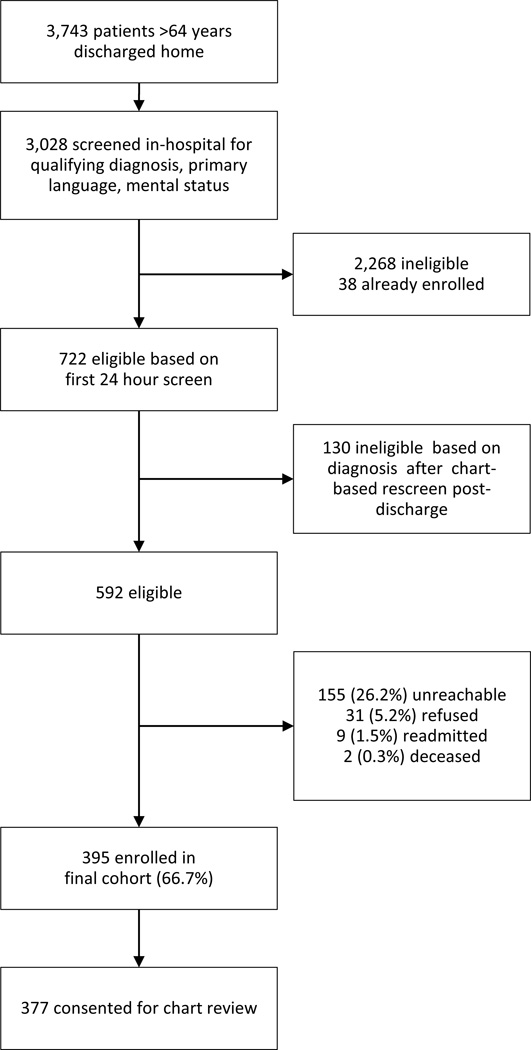
A total of 3,743 patients 65 years and older were discharged home from the medical service at YNHH during the study period; 592 were screened as eligible. All eligible patients were called at home within one week of discharge, at which time we enrolled 395 (66.7%) (Figure 1). The primary reason for failure to enroll patients was unreachability. Only 31 (5.2%) refused consent. Of these, 377 additionally provided consent for chart review.
Figure 1.
Flow diagram of enrolled participants
The study sample had a mean age of 77 years, and was 54.2% male (Table 1). Overall the study population was predominately white, English-speaking and well-educated. A total of 52.2% had acute coronary syndrome, 39.0% had heart failure, and 23.8% had pneumonia. Some patients had more than one qualifying condition. A total of 38 (9.6%) interviews were conducted with caregivers rather than patients.
Table 1.
Study sample characteristics
| Characteristic | N (%) or Mean (SD) |
|---|---|
| Condition* | |
| Acute coronary syndrome | 206 (52.2) |
| Heart failure | 154 (39.0) |
| Community-acquired pneumonia | 94 (23.8) |
| Medical Team | |
| Hospitalist team | 114 (30) |
| House staff | 123 (33) |
| Cardiology | 140 (37) |
| Age, mean years | 77.2 (7.2) |
| Male | 214 (54.2) |
| English-speaking | 384 (98.0) |
| Race/ethnicity | |
| Non-Hispanic white | 310 (82.5) |
| Non-Hispanic black | 44 (11.7) |
| Hispanic | 15 (4.0) |
| Other | 7 (1.9) |
| Education | |
| <9th grade | 41 (10.9) |
| 9–12th grade | 56 (14.9) |
| High school grad/GED | 109 (28.9) |
| College degree | 111 (29.4) |
| Graduate school degree | 60 (15.9) |
| Admission source | |
| Emergency department | 248 (66.0) |
| Direct transfer from hospital or nursing facility | 94 (25.0) |
| Direct admission from office | 34 (9.0) |
| Length of stay, mean days | 3.4 (2.5) |
| Identify a usual source of care | 377 (95.9) |
| Readmission rate | |
| Overall | 65 (17.3) |
| Acute coronary syndrome (ACS)* | 34 (16.5) |
| Heart failure (HF)* | 31 (20.1) |
| Community-acquired pneumonia (PNA)* | 11 (11.7) |
| Readmission rate for all patients 65 years and older during study period | |
| Acute myocardial infarction | 13.1% |
| HF | 27.9% |
| PNA | 17.2% |
Not mutually exclusive
Coding reliability was very high. We found 100% agreement about activity, presence of reason for hospitalization, notation about which doctor to call with problems, contact info of doctor, and the six measures of warning signs for all three conditions. Nurses agreed about 17/18 diet instructions (94%) and 15/18 primary care appointments (83%).
Discharge process: discharge instruction content and quality
Table 2 details the discharge process metrics and patient understanding metrics by topic area. A summary of key findings follows here. Every patient received discharge instructions. Reason for hospitalization, activity, name and contact information of a follow-up physician and warning signs were included in more than 97% of discharge instructions. A total of 338 (89.7%) included information about diet and 315 (83.6%) included follow-up information.
Table 2.
Comparison of content, content quality, patient perceived understanding, and actual patient understanding for key elements of transitional care
| Discharge instruction content (N=377) | Content quality (N=377 unless specified) | Self-reported understanding | Verified understanding | ||||
|---|---|---|---|---|---|---|---|
| Content item | N (%) | Content item | N (%) | Topic | N (%) | Degree of understanding | N (%) |
| Reason for hospitalization | 370 (98.1) | Includes any language likely to be understood by patients | 271 (73.7) | Strongly agree or agree clearly understand reason for hospitalization | 349/365 (95.6) | Complete | 218 (59.6) |
| Symptoms only | 118 (32.2) | ||||||
| None | 30 (8.2) | ||||||
| Activity | 367 (97.3) | N/A | Strongly agree or agree understand “things responsible for in managing health” | 345/360 (95.8) | N/A | ||
| Diet | 338 (89.7) | Describes low salt for HF | 92/146 (63.0) | N/A | |||
| Follow-up | Follow-up appointment scheduled with PMD or cardiology | 123 (32.6) | Had a follow-up appointment | 201/395 (51.0) | Complete* | 54/123 (43.9) | |
| Partial* | 41/123 (33.3) | ||||||
| None* | 28/123 (22.8) | ||||||
| Advised to follow up in certain time frame | 192 (50.9) | Complete* | 107/192 (55.7) | ||||
| Partial* | 25/192 (13.0) | ||||||
| None* | 60/192 (31.3) | ||||||
| No follow-up appointment with PMD or cardiology | 62 (16.4) | Made appointment* | 35/62 (56.5) | ||||
| Name/contact info of follow up MD | 371 (98.4) | Specific section indicating who to call in case of problems | 0 (0) | Know who to call | 330/382 (86.4) | N/A | |
| Reason to call doctor/warning signs | 371 (98.4) | ACS: dyspnea | 182/193 (94.3) | Symptoms to look out for | 330/395 (83.5) | N/A | |
| ACS: cardiac pain | 181/193 (93.8) | ||||||
| Pneumonia: fever | 77/91 (84.6) | ||||||
| Pneumonia: shortness of breath | 81/91 (89.0) | ||||||
| HF: weight gain | 133/146 (91.1) | ||||||
| HF: orthopnea, edema, any kind of dyspnea | 139/146 (95.2) | ||||||
Credit given for highest knowledge of either primary care or cardiology appointment
N/A: Not assessed; ACS: acute coronary syndrome; HF: heart failure; PMD: primary medical doctor
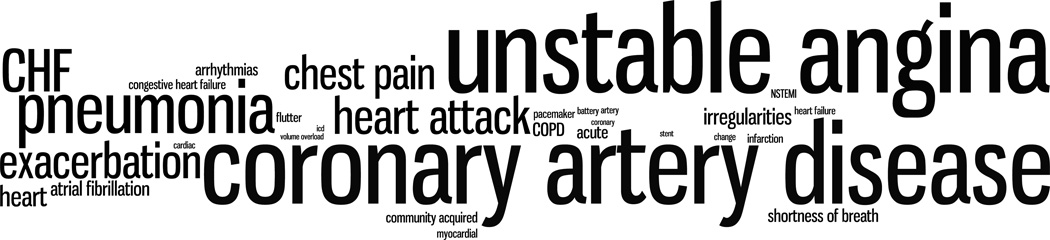
With respect to content quality, we found that 99 (26.3%) of the reasons for hospitalization were not written in language likely to be intelligible to patients. Furthermore, the most commonly used phrases were medical jargon such as “coronary artery disease,” and “unstable angina.” See Figure 2 Panel A, a word cloud of the 30 most common words or phrases written in discharge paperwork as the reason for hospitalization.
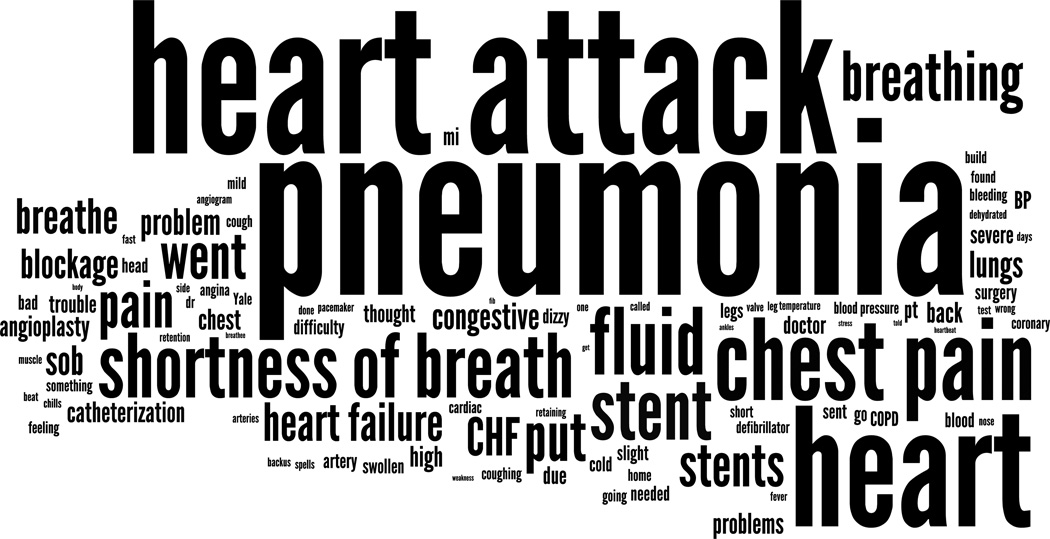
Figure 2.
Panel A: Word cloud of 30 most common phrases describing reason for hospitalization in written discharge instructions to patients
Panel B: Word cloud of 100 most common phrases describing reason for hospitalization used by patients
Less than two thirds of diet instructions for patients with HF recommended a low salt diet, and only 123 (32.6%) of patients were discharged with a documented follow-up appointment with either a primary care physician or cardiologist. The six specific warning signs we assessed (two for each of the included conditions) were included in more than 90% of instructions with the exception of fever in pneumonia patients (84.6%).
Patient understanding
Patients rated their own understanding highly, with over 90% agreeing that they understood the reason for hospitalization and self-care, and over 80% agreeing that they knew who to call with problems, and symptoms to look out for (Table 2). Half of patients reported receiving a scheduled follow-up appointment prior to discharge, substantially higher than the 32.6% who had a documented follow-up appointment in the chart.
Verified patient understanding was lower (Table 2). Comparing patient description of the reason for hospitalization with medical records, we determined that 218 (59.6%) fully understood the diagnosis, 118 (32.2%) could describe related symptoms (most commonly, “short of breath”), and 30 (8.2%) had no understanding. See Figure 2 Panel B for a word cloud of the 100 most common phrases used by patients to describe their diagnosis. Similarly, of the 123 patients with documented primary care or cardiology appointments, 54 (43.9%) could fully describe either appointment, 41 (33.3%) knew some details about at least one of them and 28 (22.8%) reported not having any appointment. Just over half of the 192 patients who were not given any appointments but were told to make their own appointment at a specified interval understood the instruction (Table 2).
Patient centered care
Patients rated discharge care highly. The mean CTM-3 score was 77.2 (SD 18.3). A total of 354/392 (90.3%) patients reported receiving written discharge instructions prior to discharge: 325/371 (87.4%) found them easy to read, 319/370 (86.0%) found them easy to understand, and 306/371 (82.5%) reported being able to ask questions about them.
During post-discharge interviews, 118 (30.0%) of patients reported receiving less than one day’s advance notice of discharge, and 246 (66.1%) reported that staff asked if they would have the support they needed at home before discharge. In addition, 297 (83.4%) of patients agreed that hospital staff took their preferences and that of their family into account in determining post-hospitalization care needs. However, after arriving home, 42 (10.9%) reported that they would have liked the hospital to provide additional services.
Discussion
In this study of discharge practices, understanding and patient-centered care, conducted at a typical large teaching hospital, we found that practices were inadequate: only one third of patients were given a follow-up appointment before discharge, less than two thirds of patients with heart failure were advised to limit salt intake in discharge instructions, and more than a quarter of discharge instructions did not use intelligible language to describe the reason for hospitalization. We also found that patient understanding was suboptimal: over a third of patients could not clearly describe their diagnosis, and less than half could recall follow-up appointments that had been made for them. Nonetheless, despite these gaps, patients were uniformly positive in their assessments of discharge care and education, overwhelmingly reporting that they found their discharge instructions easy to read and understand, and that they understood their diagnoses. In fact, the average CTM-3 score in this study was substantially higher than in previous studies, and the answers to the HCAHPS questions were slightly higher than for the hospital as a whole.26,27
The disjunction between actual and perceived understanding in this study and in a companion report23 is marked and has important implications. Current evaluations primarily assess patient perceptions of understanding (e.g., CTM-3) because it is cumbersome to assess actual understanding. Our findings suggest that assessing perceptions alone may produce a falsely optimistic picture. On the other hand, patients were able to identify several gaps in discharge practices, including little notice to prepare for discharge, limited assessment of needed home supports and a low rate of follow-up appointment provision. We were not able to verify these perceived gaps aside from provision of follow-up care. Nonetheless, our results suggest that patient perceptions may be useful in assessing the quality of discharge practices in general, even if they are not necessarily a reliable indicator of factual understanding in particular. In order to better assess what was actually done, questions should be constructed to ask about practice rather than perceived understanding, and the reliability of patients’ reports on practice should be assessed.
Several studies of emergency department patients have found they lack understanding of key elements of transitional care, including diagnosis and medications,28–34 but we had expected that understanding after hospitalization might be higher given the longer period of time available to educate patients. Consistent with other, smaller, studies of hospitalized patients,14,15 however, patient misunderstanding was still widespread. We suspect that several factors contributed. First, clinicians do not reliably use patient-friendly language, as evidenced by the wording on patients’ discharge instructions, and by other studies of verbal instructions.32,35 This might in part explain why previous studies have not found an association between content of discharge instructions and patient outcomes.5,6 Second, while a minority of older patients becomes delirious during hospitalization,36 it appears likely that many develop subtle cognitive deficits because of illness, sleep deprivation, physical dislocation and other stressors.37 In one study, 79% of hospitalized medicine patients aged 55–85 showed evidence of mild cognitive impairment.38 These deficits are often not recognized by clinicians and may impair understanding.39–42 Third, families, caregivers and outside clinicians are often left out of the transitional process, making it difficult for them to reinforce new knowledge. Lastly, both physicians and nurses overestimate patients’ knowledge, which may make them less likely to provide sufficient education.43,44
A variety of interventions will likely be necessary to improve discharge practices, patient understanding and the patient-centeredness of the care transition. Improving advance discharge planning, follow-up appointment rates, medication reconciliation, and communication with outside clinicians are critical and may require fundamental changes in hospital systems. Improving patient understanding, on the other hand, requires fundamental changes in the way clinicians interact with patients. For example, having the patient “teach-back” key information so that the clinician can verify understanding or correct misperceptions has been widely promoted as a means of improving patient comprehension.45 In a recent study, we found that nearly 70% of hospitals reported using teach-back, although it remains to be seen how successfully.46 Some also recommend treating every patient as if he were cognitively impaired or of low health literacy (the “universal precautions” approach).47,48 Indeed, misunderstanding spans all literacy and education levels.15,33
Our study has several limitations. As a single-site study at a large urban medical center, it may not be generalizable to small, non-teaching settings, although our results are consistent with other studies. Our study population was limited to three major medical diseases, and further restricted only to patients who were discharged home and consented to enroll by telephone, likely making this population more functional and less ill than an unselected group of patients with the same conditions. In addition, we assessed understanding of diagnosis, follow-up and medications, but not understanding of warning signs or self-care (which would have required numerous subjective scoring decisions). Literature suggests patients are least likely to understand the latter.29 For all these reasons we suspect our assessments of understanding likely represent a best case scenario. On the other hand, we treated the chart as a gold standard, whereas it might be that patients were actually more accurate – for example in reporting follow-up appointments. We assessed quality of the discharge process based on content of written discharge instructions; many patients also receive verbal instruction, which we could not capture. We therefore cannot assess this aspect of discharge care. Nonetheless, while the verbal part of the discharge process may have addressed some of the gaps we describe, a best practice would be to include the information in the written materials. We did not routinely interview family members, who might have had higher or lower levels of understanding. Lastly, we had an insufficient number of readmissions to correlate practice or understanding with readmission rates, which is an important area for future study.
In conclusion, we found that patient perceptions of discharge practices and self-rated understanding may be more optimistic than direct evaluations of practice or understanding would warrant. It may therefore be useful to supplement existing evaluations of transitional care with questions about practice and/or tests of factual knowledge. Furthermore, it may be best to reorganize patient education efforts around the premise that all patients will have difficulty understanding, remembering and enacting key aspects of transitional care.
Supplementary Material
Acknowledgements
Funding: At the time this study was conducted, Dr. Horwitz was supported by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research, and was a Centers of Excellence Scholar in Geriatric Medicine by The John A. Hartford Foundation and the American Federation for Aging Research. Dr. Horwitz is now supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. This work was also supported by a grant from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (P30AG021342 NIH/NIA). Dr. Krumholz is funded by grant 1U01HL105270-02 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute.
Footnotes
Prior presentations: An earlier version of this work was presented as a poster presentation at the Society of General Internal Medicine Annual Meeting in Orlando, FL on May 11, 2012.
Access to data: Leora Horwitz had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of interest: The authors declare they have no conflicts of interest.
References
- 1.Rau J. Medicare Revises Readmissions Penalties - Again. Kaiser Health News. 2013 Mar 14; [Google Scholar]
- 2.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Annals of Internal Medicine. 2011 Oct 18;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 3.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009 Feb 3;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Feb 4;138(3):161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 5.Hansen LO, Strater A, Smith L, et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Quality & Safety. 2011 Sep;20(9):773–778. doi: 10.1136/bmjqs.2010.048470. [DOI] [PubMed] [Google Scholar]
- 6.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009 Dec 31;361(27):2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 7.Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. American Journal of Managed Care. 2011 Jan;17(1):41–48. [PubMed] [Google Scholar]
- 8.Chugh A, Williams MV, Grigsby J, Coleman EA. Better transitions: improving comprehension of discharge instructions. Front Health Serv Manage. 2009 Spring;25(3):11–32. [PubMed] [Google Scholar]
- 9.VanSuch M, Naessens JM, Stroebel RJ, Huddleston JM, Williams AR. Effect of discharge instructions on readmission of hospitalised patients with heart failure: do all of the Joint Commission on Accreditation of Healthcare Organizations heart failure core measures reflect better care? Qual Saf Health Care. 2006 Dec;15(6):414–417. doi: 10.1136/qshc.2005.017640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010 May 5;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 11.Holloway A. Patient knowledge and information concerning medication on discharge from hospital. J Adv Nurs. 1996 Dec;24(6):1169–1174. doi: 10.1111/j.1365-2648.1996.tb01022.x. [DOI] [PubMed] [Google Scholar]
- 12.Kerzman H, Baron-Epel O, Toren O. What do discharged patients know about their medication? Patient Educ Couns. 2005 Mar;56(3):276–282. doi: 10.1016/j.pec.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 13.Louis-Simonet M, Kossovsky MP, Sarasin FP, et al. Effects of a structured patient-centered discharge interview on patients' knowledge about their medications. Am J Med. 2004 Oct 15;117(8):563–568. doi: 10.1016/j.amjmed.2004.03.036. [DOI] [PubMed] [Google Scholar]
- 14.Makaryus AN, Friedman EA. Patients' understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005 Aug;80(8):991–994. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 15.Maniaci MJ, Heckman MG, Dawson NL. Functional health literacy and understanding of medications at discharge. Mayo Clin Proc. 2008 May;83(5):554–558. doi: 10.4065/83.5.554. [DOI] [PubMed] [Google Scholar]
- 16.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) Developed in Collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007 Aug 14;50(7):e1–e157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 17.Thygesen K, Alpert JS, White HD Joint ESCAAHAWHFTFftRoMI. Universal definition of myocardial infarction. European Heart Journal. 2007 Oct;28(20):2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 18.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) European Journal of Heart Failure. 2008 Oct;10(10):933–989. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(17278083) Suppl 2:27–72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sunderland T, Hill JL, Mellow AM, et al. Clock drawing in Alzheimer's disease. A novel measure of dementia severity. J Am Geriatr Soc. 1989 Aug;37(8):725–729. doi: 10.1111/j.1532-5415.1989.tb02233.x. [DOI] [PubMed] [Google Scholar]
- 21.Giordano LA, Elliott MN, Goldstein E, Lehrman WG, Spencer PA. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010 Feb;67(1):27–37. doi: 10.1177/1077558709341065. [DOI] [PubMed] [Google Scholar]
- 22.Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients--development of a discharge checklist for hospitalists. J Hosp Med. 2006 Nov;1(6):354–360. doi: 10.1002/jhm.129. [DOI] [PubMed] [Google Scholar]
- 23.Ziaeian B, Araujo KL, Van Ness PH, Horwitz LI. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012 Nov;27(11):1513–1520. doi: 10.1007/s11606-012-2168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. doi: 10.1002/jhm.2021. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ziaeian B, Araujo KLB, Van Ness PH, Horwitz LI. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. doi: 10.1007/s11606-012-2168-4. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure. Med Care. 2005 Mar;43(3):246–255. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Coleman EA, Parry C, Chalmers SA, Chugh A, Mahoney E. The central role of performance measurement in improving the quality of transitional care. Home Health Care Serv Q. 2007;26(4):93–104. doi: 10.1300/J027v26n04_07. [DOI] [PubMed] [Google Scholar]
- 28.Crane JA. Patient comprehension of doctor-patient communication on discharge from the emergency department. J Emerg Med. 1997 Jan-Feb;15(1):1–7. doi: 10.1016/s0736-4679(96)00261-2. [DOI] [PubMed] [Google Scholar]
- 29.Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient Comprehension of Emergency Department Care and Instructions: Are Patients Aware of When They Do Not Understand? Ann Emerg Med. 2008 Jul 10; doi: 10.1016/j.annemergmed.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 30.Hastings SN, Barrett A, Weinberger M, et al. Older patients' understanding of emergency department discharge information and its relationship with adverse outcomes. Journal of patient safety. 2011 Mar;7(1):19–25. doi: 10.1097/PTS.0b013e31820c7678. [DOI] [PubMed] [Google Scholar]
- 31.Logan PD, Schwab RA, Salomone JA, 3rd, Watson WA. Patient understanding of emergency department discharge instructions. South Med J. 1996 Aug;89(8):770–774. doi: 10.1097/00007611-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Spandorfer JM, Karras DJ, Hughes LA, Caputo C. Comprehension of discharge instructions by patients in an urban emergency department. Ann Emerg Med. 1995 Jan;25(1):71–74. doi: 10.1016/s0196-0644(95)70358-6. [DOI] [PubMed] [Google Scholar]
- 33.Waisman Y, Siegal N, Chemo M, et al. Do parents understand emergency department discharge instructions? A survey analysis. Isr Med Assoc J. 2003 Aug;5(8):567–570. [PubMed] [Google Scholar]
- 34.Zavala S, Shaffer C. Do patients understand discharge instructions? Journal of Emergency Nursing. 2011 Mar;37(2):138–140. doi: 10.1016/j.jen.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Vashi A, Rhodes KV. "Sign right here and you're good to go": a content analysis of audiotaped emergency department discharge instructions. Annals of Emergency Medicine. 2011 Apr;57(4):315–322. e311. doi: 10.1016/j.annemergmed.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 36.Inouye SK. Delirium in hospitalized older patients. Clin Geriatr Med. 1998 Nov;14(4):745–764. [PubMed] [Google Scholar]
- 37.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013 Jan 10;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Marchis GM, Foderaro G, Jemora J, et al. Mild cognitive impairment in medical inpatients: the Mini-Mental State Examination is a promising screening tool. Dement Geriatr Cogn Disord. 2010;29(3):259–264. doi: 10.1159/000288772. [DOI] [PubMed] [Google Scholar]
- 39.Joray S, Wietlisbach V, Bula CJ. Cognitive impairment in elderly medical inpatients: detection and associated six-month outcomes. Am J Geriatr Psychiatry. 2004 Nov-Dec;12(6):639–647. doi: 10.1176/appi.ajgp.12.6.639. [DOI] [PubMed] [Google Scholar]
- 40.Laurila JV, Pitkala KH, Strandberg TE, Tilvis RS. Detection and documentation of dementia and delirium in acute geriatric wards. Gen Hosp Psychiatry. 2004 Jan-Feb;26(1):31–35. doi: 10.1016/j.genhosppsych.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 41.Torisson G, Minthon L, Stavenow L, Londos E. Cognitive impairment is undetected in medical inpatients: a study of mortality and recognition amongst healthcare professionals. BMC Geriatr. 2012 Aug 24;12(1):47. doi: 10.1186/1471-2318-12-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chodosh J, Petitti DB, Elliott M, et al. Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc. 2004 Jul;52(7):1051–1059. doi: 10.1111/j.1532-5415.2004.52301.x. [DOI] [PubMed] [Google Scholar]
- 43.Reiley P, Iezzoni LI, Phillips R, Davis RB, Tuchin LI, Calkins D. Discharge planning: comparison of patients and nurses' perceptions of patients following hospital discharge. Image J Nurs Sch. 1996 Summer;28(2):143–147. doi: 10.1111/j.1547-5069.1996.tb01207.x. [DOI] [PubMed] [Google Scholar]
- 44.Calkins DR, Davis RB, Reiley P, et al. Patient-physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan. Arch Intern Med. 1997 May 12;157(9):1026–1030. [PubMed] [Google Scholar]
- 45.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Archives of internal medicine. 2003 Jan 13;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 46.Bradley EH, Curry L, Horwitz LI, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol. 2012 Aug 14;60(7):607–614. doi: 10.1016/j.jacc.2012.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paasche-Orlow MK, Schillinger D, Greene SM, Wagner EH. How health care systems can begin to address the challenge of limited literacy. J Gen Intern Med. 2006 Aug;21(8):884–887. doi: 10.1111/j.1525-1497.2006.00544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Action Plan to Improve Health Literacy. Washington, D.C.: 2010. U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.