Abstract
Objectives
Financial strain, defined as inadequate income to cover basic needs, is related to depression in minority populations. Unclear is whether interventions can improve depression in those reporting financial strain.
Design
Randomized Controlled Trial
Setting
Philadelphia Senior Center
Participants
208 African American adults ≥ 55 years old with mild to severe depressive symptoms.
Intervention
Beat the Blues (BTB) depression intervention which includes care management, referral/linkage, stress reduction, depression education, and behavioral activation
Measurements
Patient Health Questionnaire 9 (PHQ-9), financial strain, age
Results
Although financial strain was related to depressive symptoms at baseline, participants receiving BTB at all levels of financial strain showed reduced depressive symptoms compared to a waitlist control group at 4-months. BTB participants reporting financial strain decreased an average of 6.4 points (SD= 0.85)on the PHQ-9, reflecting a clinically meaningful improvement.
Conclusions
A nonpharmacologic intervention can reduce depressive symptoms in both African Americans with and without financial strain. However, screening for and helping people manage financial strain may boost the magnitude of intervention benefit for those with financial strain and should be explored as part of depression care.
Keywords: depression, financial strain, African-Americans
Objective
Financial strain, commonly defined as lacking adequate resources to cover basic needs, is associated with depression1–3 but is a neglected factor in depression care. Financial strain may be related to depression through lack of financial resources to meet challenges, or through the physiologic changes secondary to chronic psychological stress4,5 or both. Older adults with financial strain may have less access to resources to ameliorate depression, or may suffer depression from the psychological stress inherent in financial strain, or financial strain may limit the ability to participate in pleasant events and activities which in turn lead to lower mood and increased depressive symptoms.
Although financial strain has been consistently related to depression in the epidemiological literature,1–3 we have found no reports of depression interventions in those with financial strain. While solving the root causes of financial strain would be preferable, it may not be fiscally realistic and may not enhance coping mechanisms that are then transferable to other situations. Also, although financial strain is associated with depressive symptoms, it is not known whether evidence-based depression treatments are equally effective for those with or without financial struggles. It may be that depression treatments help people become activated to address factors contributing to their financial strain such as obtaining legal or financial counsel. Alternately, it may be that depression treatments are not as effective for people with financial strain as the intervention may not directly address finances as one of the sources for the depression. Therefore, this paper examines whether Beat the Blues (BTB), a non-pharmacological depression program, decreased depressive symptoms among those with financial strain.
Methods
Working with a cohort of older African-Americans with depressive symptoms, Gitlin et al developed and tested a program called “Beat the Blues,” that is delivered by licensed social workers in the home and composed of 5 components: depression education, care management, referral and linkage, stress reduction and behavioral activation. BTB builds on previous community and home-based interventions for depressive symptoms including “Healthy Ideas.”6 and “PEARLS.”7 The program is a partnership between an academic research center and a community senior center. The senior center participated in all aspects of study design and implementation including training care managers in depression screening and social work staff in supervising the interventionists. Senior Centers are ideal places to reach low-income older adults as a wide range of people attend who might not seek treatment from their primary care provider for their depressive symptoms. Additionally, because senior center staff is in greater contact with their members than primary care providers are, they may be more likely to identify signs of depression than primary care providers can in a brief patient encounter.
Study Sample/recruitment/randomization
The methods have been described elsewhere.8 Briefly, participants were recruited from two sources, the community at large and an in-home support program for people who were temporarily medically compromised. All recruitment and protocols were approved by the IRB of Thomas Jefferson University and Johns Hopkins University. Eligible individuals had a Patient Health Questionnaire (PHQ-9) score ≥5, consistent with depressive symptoms, in two testing occasions two weeks apart, were African American, ≥55 years of age, English speaking, and cognitively intact (Mini Mental Status Examination ≥24). Individuals were excluded who had a history of serious mental illness, life-limiting illness, involvement in another depression trial, or living in long-term care facilities. Participants were randomized to the BTB treatment group or a wait list group who received BTB following the 4 month followup assessment. This study uses data from the baseline and 4-month followup.
BTB intervention
The intervention involved up to 10, one hour sessions occurring initially weekly and then bi-weekly over 4-months. Initial visits were in the participants’ homes and were replaced with periodic check-in telephone calls if participants demonstrated steady progress in the intervention. Delivered by licensed social workers, BTB involved five components: depression education, care management, referral/linkage, stress reduction, and behavioral activation plans. Each component was tailored to participants’ prioritized care needs, depression knowledge level, preferred stress reduction technique, and personal activity goals. For more information on the content of each of these areas, please see Gitlin et al 2012 BMC.8
Measures
Depression
The primary dependent variable was the PHQ-9, a brief, psychometrically sound 9-item self-report diagnostic and severity measure which is frequently used in primary care. The main outcome was severity score (range=0–27). Diagnostic categories (0–4=minimal/none, 5–9=mild, 10–14=moderate, 15–19 moderately severe, 20–27=severe depression) map onto the DSM-IV, and can be examined for clinically meaningful change.9
Financial strain was measured along a 4-point response item: how difficult do you find it to pay for your basic needs (0 =not at all difficult very difficult to 3=very difficult paying for basics). This item has been used in many epidemiologic surveys.1,2,10
Functional difficulty in 18 self-care, mobility, and instrumental activities was assessed (1=no difficulty to 5=unable to do due to health problem).11 A total score was computed as mean difficulty across items (α=.904). Lower scores indicated less functional difficulties.
Age was measured in years.
Participants rated their feelings (“I felt calm,” “tense”) from 1=very much to 4=not at all on the 10-item State Anxiety Scale.12 A total anxiety score was computed as the mean across all items (α=.850). Lower scores indicated less anxiety.
Depression knowledge/efficacy, was assessed using 10-items reflecting symptom awareness (“can identify depression symptoms”) and efficacy (“know how to explain feelings”) rated from 1=not at all confident to 4=absolutely confident. A total mean score was derived by summing across items and dividing by number of items (range=10–40). Higher scores represented improved knowledge/efficacy (α=.721).13
Analysis
Chi-square and T tests were used to compare financially strained versus not financially strained participants on baseline characteristics. The normality assumption for the dependent measure (PHQ-9) was tested by examining distribution of residuals.
Statistical analyses were performed on a modified intention to treat basis; that is, all individuals in the study and available for follow-up were included in the analyses regardless of level of participation in the intervention. However, individuals who were not available for follow-up were not included and their data were not imputed. We used multiple regression to test whether financial strain was associated with depression severity at baseline and after completion of Beat the Blues, adjusting for employment status, recruitment source, and living arrangement (design variables). In the longitudinal analyses, we adjusted for baseline depression severity as well. We also tested an interaction between group assignment and dichotomized financial strain (“not at all” and “not very difficult” vs. “somewhat difficult” and “very difficult”). All analyses were performed using STATA 10 software (College Station, TX).
Results
Sample characteristics
At baseline, participants had a mean of 69 years (SD = 8.7). Thirty-eight percent of the overall 208 baseline sample stated it was “somewhat difficult” to pay for their basic needs. Thirty percent said it was very difficult. These two groups together formed the financially strained group (68% of the group). Twenty percent said it was not difficult at all and 13 percent said it was “not very difficult” to pay for their basic needs. These two groups together were the not financial strained group. Those with financial strain had an average depression severity score of 13.7 (SD=4.8) on the PHQ-9 compared to an average score of 12.5 (SD = 4.) for those without financial strain. Those with financial strain were younger (67.9 SD= 7.7 vs. 73.1 with SD = 9.5) on average than those without (see Table 1). For the groups of participants with and without financial strain, there were not statistically significant differences by sex, living status (alone or with others), or education level. They did differ on functional difficulties with those with financial strain having a mean of 2.1(SD=0.7) out of 5 potential difficulties while those without had only 1.7 (SD=0.7) out of the five.
Table 1.
| Characteristic | With financial strain N= 141 |
Without financial strain N = 67 |
Total N= 208 | X2 (p value) For categorical variablesa |
T statistics and P value for Continuous Variablesb |
|---|---|---|---|---|---|
| Age, mean (SD) | 67.9 (7.7) | 73.1 (9.5) | 69.6 (8.7) | −3.93 (0.0002) | |
| Female % (N) | 78.0 (110) | 79.1 (53) | 78.4 (163) | 0.0318 (0.8584) | |
| Percent living alone | 53.9(76) | 62.7 (42) | 53.7 (118) | 1.4282 (0.2321) | |
| Education level | 1.7291 (0.4212) | ||||
| %< HS | 23.40 (33) | 16.42 (11) | 21.15 (44) | ||
| %=HS | 29.79 (42) | 28.36 (19) | 29.33 (61) | ||
| %> HS | 46.81 (66) | 55.22 (37) | 49.52 (103) | ||
| Mean (SD) (PHQ-9 severity score at baseline | 13.8 (5.1) | 11.4 (4.1) | 13.0 (4.9) | 3.51 (0.0006) | |
| Percent at each diagnostic category of PHQ-9 (baseline values) | 17.2 (0.0006) | ||||
| Mild | 27.66 (39) | 31.34 (21) | 28.85 (60) | ||
| Moderate | 27.66 (39) | 50.75(34) | 35.10 (73) | ||
| Mod. Severe | 28.37 (40) | 14.93 (10) | 24.04 (50) | ||
| Severe | 16.31 (23) | 2.99 (2) | 12.02 (25) | ||
| Baseline Depression knowledge and Self-efficacy mean score (SD) | 3.1 (0.4) | 3.2 (0.4) | 3.1 (0.4) | −1.69 (0.0930) | |
| Functional difficulties, mean (SD) | 2.1(0.7) | 1.7 (0.6) | 2.0 (0.7) | 4.1 (<0.0001) | |
| Anxiety score, mean (SD) | 2.6 (0.6) | 2.4 (0.6) | 2.5 (0.6) | 2.1 (0.0346) | |
| Percent at each level of financial strain | NA | NA | |||
| Not difficult at all | 0.0 (0) | 61.2 (41) | 19.7 (41) | ||
| Not very difficult | 0.0 (0) | 38.8 (26) | 12.5 (26) | ||
| Somewhat difficult | 55.3 (78) | 0.00 (0) | 37.5 (78) | ||
| Very difficult | 44.7 (63) | 0.00 (0) | 30.3 (63) | ||
Pearson x2 (df=1)
t test (df=1)
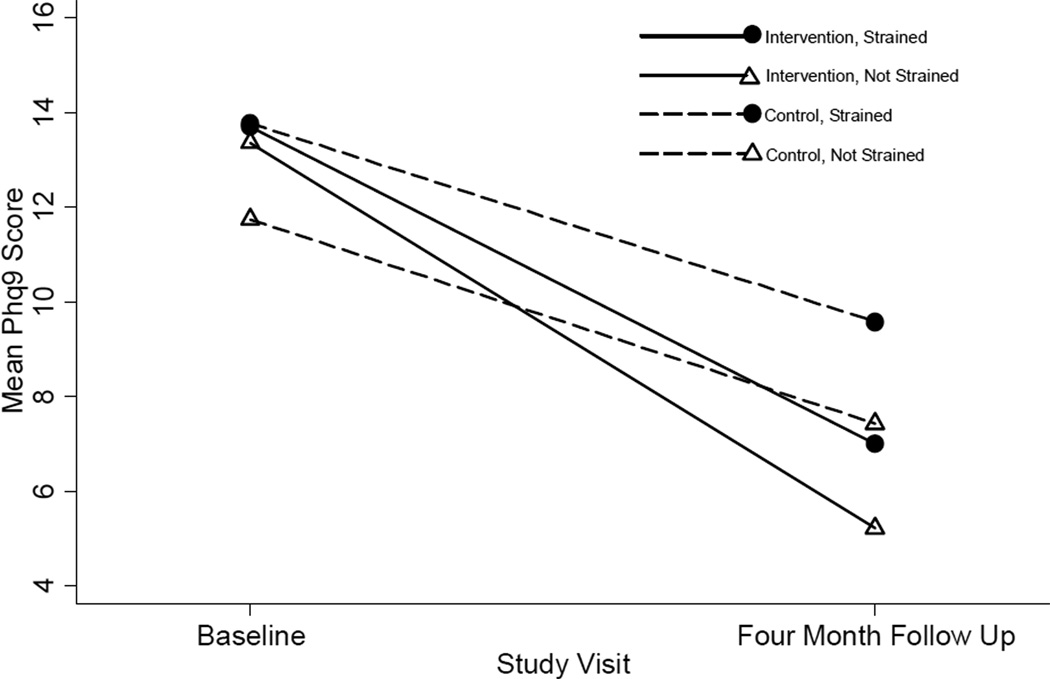
Treatment Effect by Financial Status
One hundred and eighty two participants completed the 4-month trial. Although financial strain was associated with depressive symptoms at baseline (Multiple regression Beta = 0.77, t = 2.42, df = 5, p<0.05), participants receiving the BTB intervention at all levels of financial strain showed reduced depressive symptoms compared to a waitlist control group. At 4-months, BTB participants who reported it “somewhat difficult” or “very difficult” to pay for basic needs decreased an average of 6.4 points (SD= 0.85) on the PHQ-9. A score reduction of ≥5 points on the PHQ-9 is considered a clinically meaningful change in depression severity. Those who did not have financial strain decreased on average 8.77 points (SD= 1.77) on the PHQ-9 from baseline to 4-months. Financial strain did not moderate the effect of the intervention in a statistically significant manner [Multiple regression Beta = 0.53, t= 0.32, df=7, p >0.05 95% CI = (−2.77,3.84)]. See Figure 1.
Figure 1.
Adjusted Means of Financially Strained and Not Financially Strained Participants, By Study Assignment
Conclusions
In this study, we found that those with financial strain were positively impacted by a low-cost depression intervention similar to those without financial strain. Although the literature consistently shows that those with financial strain are more likely to be depressed, this is the first study to our knowledge showing that a nonpharmacologic treatment approach can improve depressive symptoms for those with financial strain. The study was not designed to pinpoint which factors contribute to depression. The point of this analysis was to see whether those with depressive symptoms and financial strain could improve from a non-pharmacological intervention. And we found that both groups did improve in a clinically meaningful way.
The Beat the Blues (BTB) intervention emphasizes care management and behavioral activation and increasing mastery over contextual factors contributing to mood.14 Previous literature has shown that social networks can be stressed by financial strain which can then lead to social isolation (Krause, 1991). Lincoln et al found that overtaxed networks in financially vulnerable communities can limit social support15 but that mastery may mediate the relationship between stressors (such as financial strain) and depressive symptoms. An intervention like BTB which may enhance individual mastery is consistent with the findings of these observational studies. Future research is warranted to examine whether mastery mediates these relationships.
In contrast to pharmacological therapy for depression, BTB has two notable advantages. There are no known adverse side effects, and it is likely long lasting because it promotes learned behavior change and problem solving that can be continually applied after the end of the BTB program. Its care management component may directly address financial strain by helping participants identify legal and financial assistance to address their financial concerns or limitations.
The limitations of this study include that it took place in only one geographical location, Philadelphia, PA, and working with one engaged, active senior center staff which may not be representative of other senior centers and staffing across the nation. Also, the intervention took place during the recession of 2009–12 and so the financial strain may be different than other eras of financial strain. Third, it was impossible to measure outcomes on some people (N= 26 or 12.5%) so we followed modified intention to treat analysis methods, all participants with 4-motnh data for the PHQ-9 were included regardless of treatment exposure. Finally, we cannot evaluate whether the care management and behavioral activation components of the intervention directly addressed financial strain issues.
The strengths of the study are many. First, it had relatively high retention rates (182 of 208 or 88% completed the visits and data collection). Second, strong fidelity measures ensured that an equal “dose” of each component was offered to each participant based upon a comprehensive assessment of each individual’s need. A third strength was that BTB was culturally tailored to an urban older African-American population and so had high relevance to the community concerns.
Practice Implications: Participants with financial strain benefited from study participation although their strain may not have been directly addressed. BTB addresses depressive symptoms at the individual level. Addressing financial strain itself may require a societal/health policy level intervention. Programs such as Health Leads http://www.healthleadsusa.org/ and Economic Security Initiatives http://www.ncoa.org/enhance-economic-security/economic-security-Initiative/ are starting to do exactly that. However, depressive symptoms are not individually addressed in these programs. Because of this, participants may still suffer from the depressive symptoms that hinder taking meaningful action such as low energy, anxiety, and fatalism.
In conclusion, a nonpharmacologic intervention can reduce depression symptoms in African Americans with financial strain. Senior centers can have an important role in depression management with minority, low income older adults.
Acknowledgments
Beat the Blues was funded by the National Institute of Mental Health grants #RO1 MH 079814, R24 MH074779 and RC1MH090770 to Dr. Gitlin. Dr. Szanton was also funded by the Robert Wood Johnson Nurse Faculty Scholars program for analyses for this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A version of this paper was presented at the National Summit on Health Disparities 2012, National Harbor, MD December 17–19, 2012
References
- 1.Szanton SL, Allen JK, Thorpe RJ, Jr, Seeman T, Bandeen-Roche K, Fried LP. Effect of financial strain on mortality in community-dwelling older women. J Gerontol B Psychol Sci Soc Sci. 2008;63(6):S369–S374. doi: 10.1093/geronb/63.6.s369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angel RJ, Frisco M, Angel JL, Chiriboga DA. Financial strain and health among elderly mexican-origin individuals. J Health Soc Behav. 2003;44(4):536–551. [PubMed] [Google Scholar]
- 3.Aranda MP, Lincoln KD. Financial strain, negative interaction, coping styles, and mental health among low-income latinos. Race and Social Problems. 2011;3(4):280–297. [Google Scholar]
- 4.McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54(3):200–207. doi: 10.1016/s0006-3223(03)00177-x. [DOI] [PubMed] [Google Scholar]
- 5.Gibbs RA, Belmont JW, Hardenbol P, et al. The international HapMap project. Nature. 2003;426(6968):789–796. doi: 10.1038/nature02168. [DOI] [PubMed] [Google Scholar]
- 6.Casado BL, Quijano LM, Stanley MA, Cully JA, Steinberg EH, Wilson NL. Healthy IDEAS: Implementation of a depression program through community-based case management. Gerontologist. 2008;48(6):828–838. doi: 10.1093/geront/48.6.828. [DOI] [PubMed] [Google Scholar]
- 7.Ciechanowski P, Wagner E, Schmaling K, et al. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA. 2004;291(13):1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- 8.Gitlin LN, Harris LF, McCoy M, et al. A community-integrated home based depression intervention for older african americans: [corrected] description of the beat the blues randomized trial and intervention costs. BMC Geriatr. 2012;12:4. doi: 10.1186/1471-2318-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47(1):17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 11.Ettinger WH, Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. the fitness arthritis and seniors trial (FAST) JAMA. 1997;277(1):25–31. [PubMed] [Google Scholar]
- 12.Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, Jacobs GA. Manual for the state-trait anxiety inventory. Palo Alto, CA: onsulting Psychologists Press; 1983. [Google Scholar]
- 13.Cretin S, Shortell SM, Keeler EB. An evaluation of collaborative interventions to improve chronic illness care. framework and study design. Eval Rev. 2004;28(1):28–51. doi: 10.1177/0193841X03256298. [DOI] [PubMed] [Google Scholar]
- 14.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. [PubMed] [Google Scholar]
- 15.Lincoln KD, Chatters LM, Taylor RJ. Social support, traumatic events, and depressive symptoms among african americans. J Marriage Fam. 2005;67(3):754–766. doi: 10.1111/j.1741-3737.2005.00167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]