Abstract
Objective
To investigate the sagittal sacropelvic morphology and balance of the patients with SIJ pain following lumbar fusion.
Methods
Among 452 patients who underwent posterior lumbar interbody fusion between June 2009 and January 2013, patients with postoperative SIJ pain, being responded to SIJ block were enrolled. For a control group, patients matched for sex, age group, the number of fused level and fusion to sacrum were randomly selected. Patients were assessed radiologic parameters including lumbar lordosis, pelvic incidence (PI), pelvic tilt (PT) and sacral slope (SS). To evaluate the sagittal sacropelvic morphology and balance, the ratio of PT/PI, SS/PI and PT/SS were analyzed.
Results
A total of 28 patients with SIJ pain and 56 patients without SIJ pain were assessed. Postoperatively, SIJ pain group showed significantly greater PT (p=0.02) than non-SIJ pain group. Postoperatively, PT/PI and SS/PI in SIJ pain group was significantly greater and smaller than those in non-SIJ pain group respectively (p=0.03, 0.02, respectively) except for PT/SS (p=0.05). SIJ pain group did not show significant postoperative changes of PT/PI and SS/PI (p=0.09 and 0.08, respectively) while non-SIJ pain group showed significantly decrease of PT/PI (p=0.00) and increase of SS/PI (p=0.00).
Conclusion
This study presents different sagittal sacropelvic morphology and balance between the patients with/without SIJ pain following lumbar fusion surgery. The patients with SIJ pain showed retroversed pelvis and vertical sacrum while the patients without SIJ pain have similar morphologic features with asymptomatic populations in the literature.
Keywords: Sacroiliac joint pain, Lumbar fusion surgery, Sacropelvic morphology, Lumbopelvic parameters
INTRODUCTION
Despite a careful selection of patients, the failure rates associated with lumbar fusion surgery have been reported to range from 5 to 30%5,27). Among the different sources of low back pain following lumbar fusion surgery, the sacroiliac (SIJ) joint has been suggested as a possible source by several authors10,11,12,27). Maigne and Planchon27) suggested three possible causes of SIJ pain following lumbar fusion surgery : 1) mechanical load transfer on SIJ after fusion; 2) a consequence of bone graft harvesting in the iliac crest close the joint; and 3) the misdiagnosing of a sacroiliac syndrome before fusion (i.e., the lumbar spine being fused erroneously).
The adoption by humans of upright position resulted in the pelvis becoming a paramount structure within human motor apparatus. The pelvis forms the bond between the trunk and the posterior limbs by femoral head and can rotate around it (bicoxo-femoral axis). This rotatory ability of the pelvis around the femoral heads is one of mechanisms of regulation of sagittal balance. Because the position of lumbar spine, which is attached to the sacral plateau, is affected by the pelvic position19).
Recently, owing to their close relationship with the spine, many authors have raised the role of sacropelvic morphology and balance in the pathogenesis of various spinal disorders including degenerative spondylolisthesis3,28), adult spinal deformity14,17) and adolescent idiopathic scoliosis25). However, as far as we know, there has been no study specifically describing the sacropelvic morphology and balance of the patients with SIJ pain following lumbar fusion surgery.
This study aims to investigate the sagittal sacropelvic morphology and balance of the patients with SIJ pain following lumbar fusion surgery.
MATERIALS AND METHODS
Patient selection
The approval of the institutional review board at our hospital was obtained for the current study. Between June 2009 and January 2013, a total of 452 consecutive patients who underwent posterior lumbar interbody fusion (PLIF) at our institution were investigated. All cases of PLIF surgery were performed using a PEEK cage packed with autologous bones obtained from lamina or spinous process and pedicle screws were inserted. There were no injury to SIJ and all procedures of PLIF were done by the same surgeon.
Patients were included into SIJ pain group if their reported postoperative pain met following criteria16,26) : pain begins with standing or sitting position after surgery and it differs from preoperative one; unilateral or bilateral prevalence persistent pain which had compatible distribution with a sacroiliac joint (below the L5 spinous process, over the posterior aspect of one or both SIJs); with or without radiation to the posterior thigh or groin but not below the knee; with or without tenderness of the sacroiliac sulcus at palpation; and no evidence of lumbar cause (no breach of screw and no residual nerve root impingement on postoperative CT scan images. Then, for the patients whose symptoms were consistent with above mentioned criteria, a fluoroscopically guided SIJ block was performed and after block, the patient with positive response was classified into SIJ pain group. A positive response was defined as characteristic pain reduction of 75% or greater for 1-4 hours following the SIJ block22). All SIJ blocks were performed by two spine fellows and the procedures of SIJ block was performed as described in previously report31). We excluded patients with clear nerve root compression sign (motor or sensory deficits), with proven osteoarthritis of hip with clinical symptoms, with pain related to disc or facet origin, and with signs of sacroilitis (ankylosing spondylitis, reactive arthritis, or enteropathic arthritis).
To compare the characteristics of sagittal sacropelvic morphology and balance between patients with SIJ pain and those without SIJ pain after PLIF, one of spine fellows who was not informed of current study participated in extracting a control group (non-SIJ pain group consisted of patients without postoperative SIJ pain). At first, he randomly selected the patients who were matched for sex, age group, the number of fused level and fusion to sacrum. The ratio of case to control was 1 to 2 and we expected this frequency matching extraction would enhance statistical power6).
Data collection and assessment
Patient clinical data (including age, sex, diagnosis, BMD and BMI) was collected by chart review. Before and after operation, full-length lateral radiographs of the spine were taken. In the standing position, the patients were asked to stand straight but relaxed with elbows fully flexed, fists resting on the clavicles, and the knees fully extended as possible. Not knowing whether the patient belonged to SIJ pain or non-SIJ pain group, the other spine fellow who was not involved in patient selection performed radiological assessment on a digital radiographic image displayed on a Picture Archiving and Communication system (PACS) terminal (Marosis 2003, Seoul, Korea). Measuring angles of radiological parameters was done by using an automated program of the PACS computer software system and additionally, data regarding levels of fusion and involvement of sacrum were also collected.
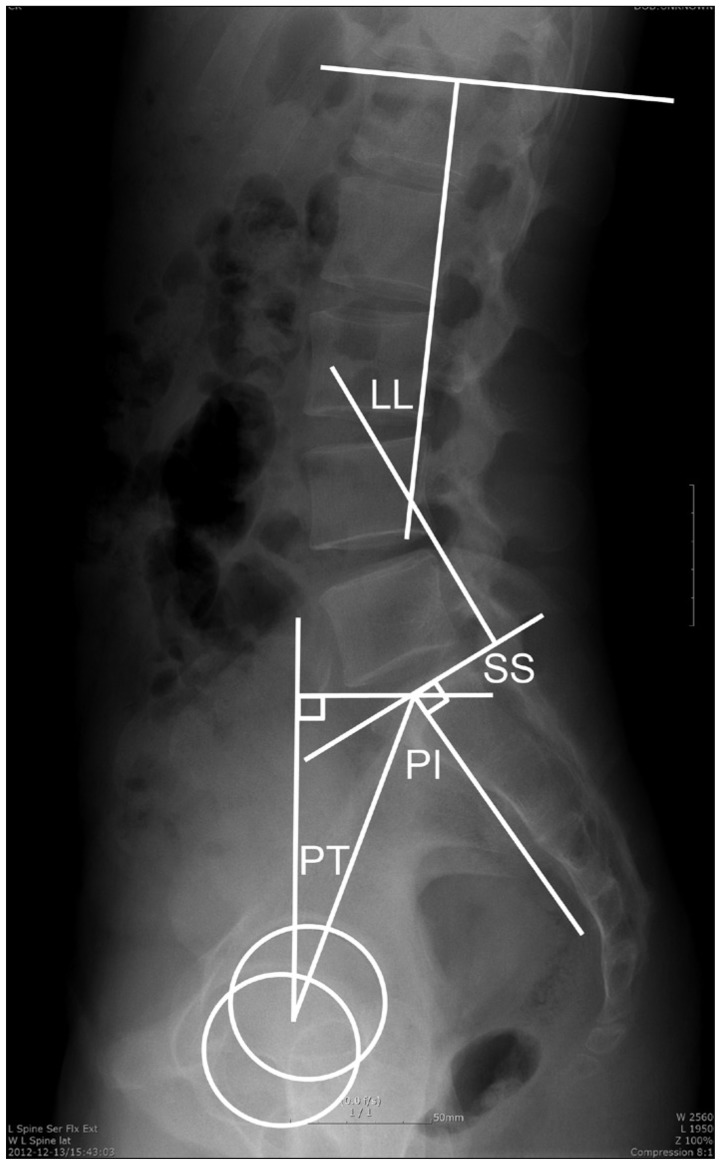
Lumbopelvic parameters
The lumbopelvic parameters including lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT) and sacral slope (SS), were assessed as reported by Duval-Beaupére et al.9) on the standing radiographs. The angle of LL was measured from the inferior endplate of T12 to the superior endplate of S1 using the Cobb method. PI was defined as the angle formed by a line drawn between the center of the femoral head and the sacral endplate. PT was defined as the angle formed by a line drawn from the midpoint of the sacral endplate to the center of the bicoxofemoral axis and a vertical and a vertical plumb line. SS was defined as the angle formed by a line drawn along the endplate of the sacrum and a horizontal reference line (Fig. 1).
Fig. 1.
Lumbopelvic parameters. LL : lumbar lordosis, PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope.
Ratios among pelvic parameters
In order to evaluated the sagittal sacropelvic morphology and balance, as advocated by Mac-Thiong et al.23), the ratio of PT to PI (PT/PI), SS to PI (SS/PI) and PT to SS (PT/SS) were calculated and compared between SIJ pain and non-SIJ pain group.
Statistical analysis
For comparisons of categorical variables, Pearson's chi-square test was used and continuous variables were compared either using Student's t-test after verification of normal distribution by the Kolmogorov-Smirnov test or using the non-parametric Mann-Whitney U test. To compare the changes between before and after PLIF surgery, paired t-test or Wilcoxon signed rank test was used depending on result of normality test. p value less than 0.05 was regarded to be statistically significant.
RESULTS
Patient population
Twenty-eight patients (10 males and 18 females) with postoperative SIJ pain, being response to SIJ block, were enrolled in SIJ pain group. By frequency matching by the ratio of 1 to 2, fifty-six patients (20 males and 36 females) without postoperative SIJ pain were selected for non-SIJ pain group. Totally, 84 patients were enrolled in this study. Table 1 shows the comparison of patients' clinical data between two groups. Patients in SIJ pain group were older and more osteoporotic than those in non-SIJ pain group however, they were statistically not significant (p=0.38 and 0.81, respectively) and the remaining BMI, number of fused level, involvement of sacrum, and diagnosis were similar as well (p=0.81, 0.92, 0.64, and 0.95, respectively).
Table 1.
Comparison of clinical data between SIJ pain and non-SIJ pain group after PLIF surgery
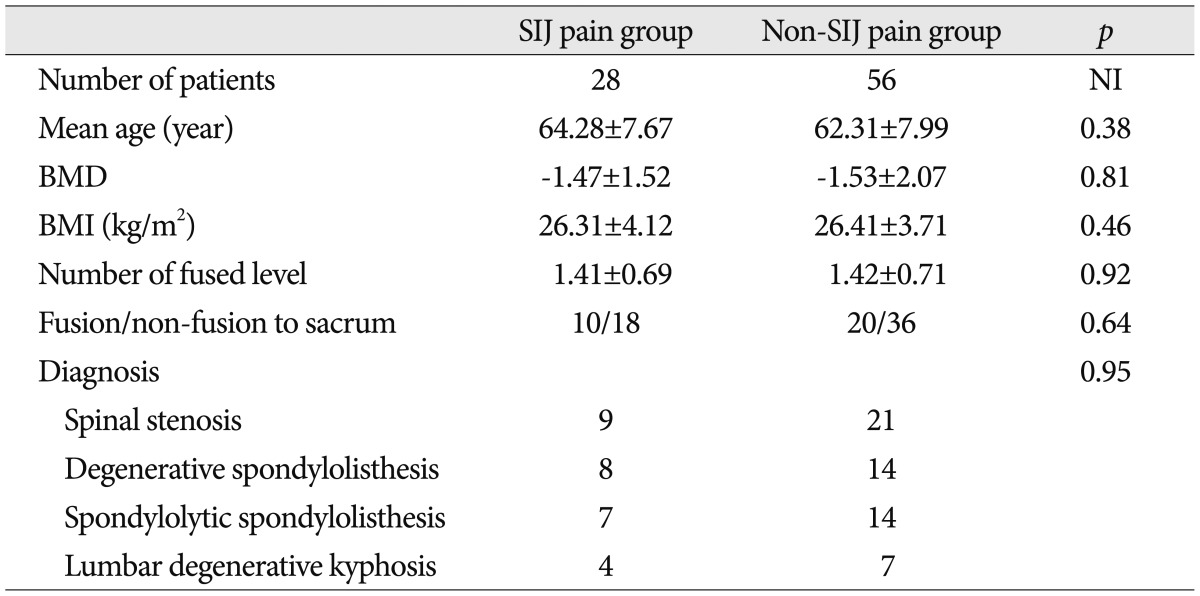
NI : not involved, PLIF : posterior lumbar interbody fusion
Lumbopelvic parameters
Table 2 shows the mean value of pre- and postoperative lumbopelvic parameters in two groups. Preoperatively, there were no statistically significant differences between SIJ pain and non-SIJ pain group in terms of lumbopelvic parameters including LL, PI, PT and SS (p=0.58, 0.47, 0.44 and 0.83, respectively). However, postopertively, PT of SIJ pain group were significantly greater (p=0.02) than that of non-SIJ pain group and the remaining values of lumbopelvic parameters were similar.
Table 2.
Comparison of lumboplevic parameters between SIJ pain and non-SIJ pain group
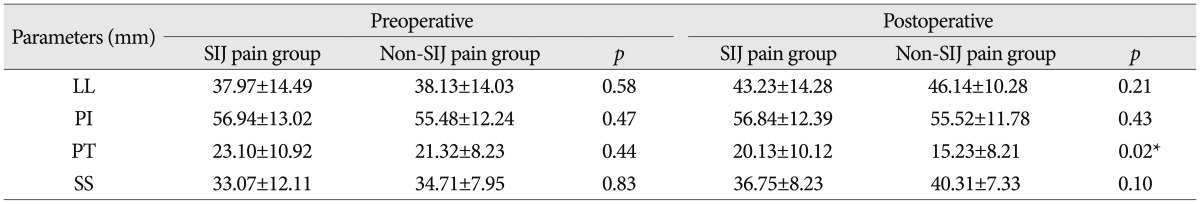
*Values are statistically significant. LL : lumbar lordosis, PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope
Ratios among pelvic parameters
Table 3 shows the comparison of ratios among pelvic parameters in SIJ pain and non-SIJ pain group. Of the calculated ratios, preoperative PT/PI, SS/PI and PT/SS showed no significant differences between SIJ pain and non-SIJ pain group (p=0.52, 0.52 and 0.28, respectively). However postoperatively, PT/PI and SS/PI in SIJ pain group was significantly greater and smaller than those in non-SIJ pain group respectively (p=0.03, 0.02, respectively) except for PT/SS (p=0.05).
Table 3.
Ratios of pelvic parameters between SIJP and non-SIJP group
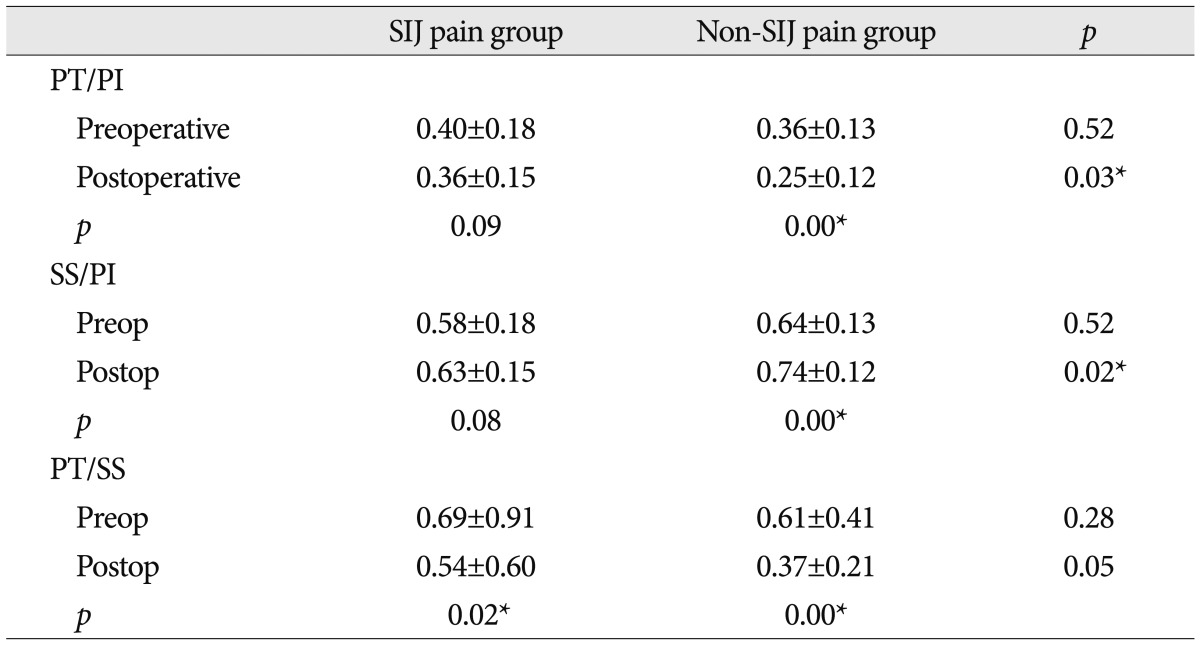
*Values are statistically significant. PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope, Postop : postoperatively, Preop : preoperative
SIJ pain group did not show significant postoperative changes of PT/PI and SS/PI (p=0.09 and 0.08, respectively) while non-SIJ pain group showed significantly decrease of PT/PI (p=0.00) and increase of SS/PI (p=0.00) postoperatively. In terms of PT/SS, both SIJ pain and non-SIJ pain group showed significant decrease of the ratio (p=0.02 and 0.00, respectively).
DISCUSSION
This study demonstrated the differences of sagittal sacropelvic morphology and balance between the patients with/without SIJ pain following lumbar fusion surgery. Several reports1,12,16,26) have discussed the etiology of SIJ pain following lumbar fusion surgery however, it is true that there lacks of postural analysis in terms of sagittal sacropelvic morphology and balance. In prior to this study, authors reported the differences of lumbopelvic parameters between the patients with/without SIJ pain following lumbar fusion surgery and pointed out the importance of restoring appropriate LL based on PI to prevent postoperative SIJ pain32). In current study, we tried to reveal the sagittal sacropelvic morphology and balance of patients with SIJ pain after lumbar fusion surgery by using the ratios among pelvic parameters proposed by Mac-Thiong et al.23) and discussed about the comparison with normative values in the literature.
The sagittal sacropelvic morphology can be defined by PI and its two component, namely PT and SS8). PI is a morphological, individually constant parameter that did not depends on the orientation of the pelvis and the patient's position, whereas the SS and PT are directly related to pelvic position4). PI is strongly correlated to the SS (r=0.80) and lumbar lordosis (LL, r=0.60), and the LL is strongly correlated to the SS (r=0.86)21). Through these strong correlations, PI plays a central role in the determination of pelvic orientation and sagittal curvature as a high PI necessitates a high LL. It is also known that, mathematically PI is the sum of PT and SS (PI=PT+SS)21). As PT increases, the SS decreases because the sacrum assumes a more vertical position about the femoral head axis namely, pelvic retroversion. Pelvic retroversion is a compensatory process to rebalance the spine and maintain upright posture in case of sagittal imbalance2). In current study, both pre- and postoperative lumbopelvic parameters including LL, PI and SS showed no statistically significant differences in SIJ pain and non-SIJ pain group. However, PT of SIJ pain group was significantly greater than that of SIJ pain group postoperatively, whereas this value was similar preoperatively. Lafage et al.18), after prospective investigation on 125 patients with spinal deformity, revealed increased PT was correlated with worsening health related quality of life (HRQOL). They explained this result as a compensatory mechanism of pelvis (increase PT, namely pelvic retroversion) to keep a balanced standing posture and insisted resetting the PT to normal values was important to restore ambulatory function. Schwab et al.30) reported correlation analysis between radiographic spinopelvic parameters and HRQOL revealed no significance in terms of coronal plane parameters and confirmed that pelvic position measured via PT correlated with HRQOL in adult deformity. They also regarded high values of PT expressed compensatory pelvic retroversion for sagittal spinal malalignment.
Compensatory increase in PT is considered as a part of the disease process. With retroversed pelvis, the femoral heads get forward and the sacrum and the spine get backward. This allows the C7 plumb line to be behind the vertical line passing through the center between the femoral heads and the gravity line. Although body is balanced, it is less economical because posterior back muscle should be strengthened to restore LL. This is an energy consuming process that becomes easily painful and could be one of reason for back pain in the line with facet constraints and over loading15). The findings in current study indicate that increased stress across SIJ articular surface by hip hyper-extension and a decrease in the anterior coverage of the hip caused by pelvic retroversion18) are attributable to the development of SIJ pain following lumbar fusion surgery.
Mac-Thiong et al.23) investigated large cohort of 709 asymptomatic adult (354 males and 355 females, mean age of 36.8 years) who did not have spinal pathology and reported the ratios among pelvic parameters. In their study, they used the ratios of PT to PI (PT/PI), SS to PI (SS/PI) and PT to SS (PT/SS) in order to evaluate the relationships between parameters of sagittal sacropelvic morphology and balance. They found PT/PI was less than 0.5 and SS/PI was more than 0.5, indicating that the PT value is normally at most half of the PI and the SS value is normally at least half of the PI in asymptomatic populations. Based on this result, they insisted the values outside those ranges could potentially predispose to the development of spinal pathology. In current study, pre- and post-operative PT/PI were less than 0.5 and SS/PI were more than 0.5 in both groups and we presumed this result is related with the fact that our data were not obtained from spinal deformed patients but from patients with degenerative spinal disease. However, comparison between SIJ pain and non-SIJ pain group showed significant differences of PT/PI and SS/PI. In SIJ pain group, postoperative PT/PI was greater and SS/PI was lesser than non-SIJ pain group. Moreover, in contrast to non-SIJ pain group, those values in SIJ pain group did not showed significant changes postoperatively. These data implicate that patients with SIJ pain have more vertical sacrum (decreased SS) and more retroversed pelvis (increased PT) than patients with non-SIJ pain. This finding is accordant with that of Lazennec et al's study. In their comparative study between 81 patients who underwent lumbosacral fusion pain and control group, they found PT was almost twice the normal value and sacrum was more vertical in post-fusion pain group. They insisted that achieving a strong fusion should not be the only goal and appropriate position of the fused vertebrae is also of paramount importance to minimize muscle work during posture maintenance.
The changes of ratios of PT/PI and SS/PI indicate the changes of the sagittal sacropelvic morphology and balance. The patients without SIJ pain showed postoperative significant decrease and increase of PT/PI and SS/PI respectively while the patients with SIJ pain did not show significant differences. The possible explanation for this could be that lumbar fusion surgery failed to achieve the balanced sacropelvic morphology in SIJ pain group. Although specific factors related to surgical procedure which bring out these differences could not be revealed in current study and we hope well designed investigation should be done in the future. Notably, the ratios of PT/SS were significantly decrease in both groups. The value of PI is fixed for a given patient and as PT decreases, SS necessarily decreases thus, it is natural that the postoperative ratio of PT/SS decreases in both groups. However, we assume that the decrease of PT/SS could be the actual sign of occurrence of the sagittal sacropelvic realignment by lumbar fusion surgery, regardless of its clinical significance.
So far, normative values of pelvic parameters have been reported by several authors13,23,29) and previously published studies have provided a basic understanding of the normative values that these parameters should fall within. However, most of these data has been obtained not from Asian but from whites. Considering the fact that there exist somewhat differences in spine between Asian and Whites20), it is more reasonable to use the calculated ratio rather than using absolute values for precise comparison. Table 4 shows ratios among pelvic parameters of asymptomatic populations, which was adopted from previously published data7,20,24,29,33). The ratios of SIJ pain group was notably different from those of normal populations while the ratios of non-SIJ pain group was similar with those of normal populations. This is because through the lumbar fusion surgery, sagittal sacropelvic morphology of non-SIJ pain group could become normal. On the contrary, the pelvis and sacrum of SIJ pain group were still abnormal postoperatively i.e., the pelvis was retroversed and the sacrum was vertical. We believe achieving a normal sagittal sacropelvic morphology and balance are important to avoid the development of SIJ pain following lumbar fusion surgery.
Table 4.
Comparison of the studies ratios among pelvic parameters in normal populations in the literature
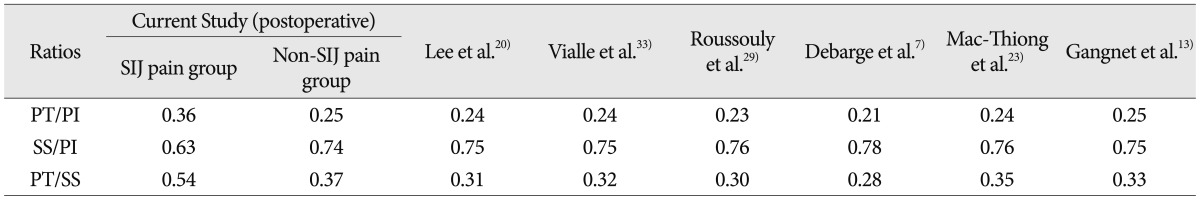
PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope
The present study has several limitations including small sample size and a retrospective case-control study rather than randomized controlled study. However, frequent matching extraction by uninformed spine fellow and radiologic measurement by the other spine fellow without information of patient's group could minimize the chances of bias.
CONCLUSION
This study demonstrated the different sagittal sacropelvic morphology and balance between the patients with/without SIJ pain following lumbar fusion surgery. The patients with SIJ pain showed retroversed pelvis and vertical sacrum compared with non-SIJ pain group. In addition, the patients without SIJ pain have similar sagittal sacropelvic morphology and balance with asymptomatic populations in the literature, while the patients with SIJ pain did not. The postoperative compensatory mechanism by sacropelvis and imbalance lead to great energy expenditure and give birth to the SIJ pain following lumbar fusion surgery.
References
- 1.Ahn Y, Lee S. Iatrogenic sacroiliac joint syndrome after percutaneous pedicle screw fixation at the L5-S1 level : case report. Neurosurgery. 2010;67:E865–E866. doi: 10.1227/01.NEU.0000374856.26808.80. [DOI] [PubMed] [Google Scholar]
- 2.Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, Deviren V, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults. J Neurosurg Spine. 2012;16:547–564. doi: 10.3171/2012.2.SPINE11320. [DOI] [PubMed] [Google Scholar]
- 3.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 4.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 5.Bose B. Outcomes after posterolateral lumbar fusion with instrumentation in patients treated with adjunctive pulsed electromagnetic field stimulation. Adv Ther. 2001;18:12–20. doi: 10.1007/BF02850247. [DOI] [PubMed] [Google Scholar]
- 6.Breslow NE, Day NE. Statistical methods in cancer research. Volume I - The analysis of case-control studies. Vol. 1. Lyons, France: IARC Sci Publ; 1980. pp. 5–338. [PubMed] [Google Scholar]
- 7.Debarge R, Demey G, Roussouly P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J. 2010;19:65–70. doi: 10.1007/s00586-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duval-Beaupère G, Robain G. Visualization on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop. 1987;11:261–269. doi: 10.1007/BF00271459. [DOI] [PubMed] [Google Scholar]
- 9.Duval-Beaupère G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis : the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Elgafy H, Semaan HB. Computed tomographic findings in patients with persistent sacroiliac pain after posterior iliac graft harvesting. Spine (Phila Pa 1976) 2000;25:2047–2051. doi: 10.1097/00007632-200008150-00008. [DOI] [PubMed] [Google Scholar]
- 11.Fritzell P, Hägg O, Wessberg P, Nordwall A. 2001 Volvo Award Winner in Clinical Studies : Lumbar fusion versus nonsurgical treatment for chronic low back pain : a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 2001;26:2521–2532. doi: 10.1097/00007632-200112010-00002. [DOI] [PubMed] [Google Scholar]
- 12.Frymoyer JW, Howe J, Kuhlmann D. The long-term effects of spinal fusion on the sacroiliac joints and ilium. Clin Orthop Relat Res. 1978:196–201. [PubMed] [Google Scholar]
- 13.Gangnet N, Dumas R, Pomero V, Mitulescu A, Skalli W, Vital JM. Three-dimensional spinal and pelvic alignment in an asymptomatic population. Spine (Phila Pa 1976) 2006;31:E507–E512. doi: 10.1097/01.brs.0000224533.19359.89. [DOI] [PubMed] [Google Scholar]
- 14.Gottfried O, Daubs M, Patel A, Dailey A, Brodke D. Spinopelvic parameters in postfusion flatback deformity patients. Spine J. 2009;9:639–647. doi: 10.1016/j.spinee.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S. Sagittal imbalance cascade for simple degenerative spine and consequences : algorithm of decision for appropriate treatment. Eur Spine J. 2011;20:699–703. doi: 10.1007/s00586-011-1938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz V, Schofferman J, Reynolds J. The sacroiliac joint : a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003;16:96–99. doi: 10.1097/00024720-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Kim YJ, Bridwell K, Lenke L, Rhim S, Cheh G. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1 : can we predict ideal lumbar lordosis? Spine (Phila Pa 1976) 2006;31:2343–2352. doi: 10.1097/01.brs.0000238970.67552.f5. [DOI] [PubMed] [Google Scholar]
- 18.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J. Pelvic tilt and truncal inclination : two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 19.Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters : origin and significance. Eur Spine J. 2011;20(Suppl 5):564–571. doi: 10.1007/s00586-011-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee CS, Chung S, Kang K, Park S, Shin S. Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine (Phila Pa 1976) 2011;36:E1648–E1654. doi: 10.1097/BRS.0b013e318216b0fd. [DOI] [PubMed] [Google Scholar]
- 21.Legaye J, Duval-Beaupre G, Hecquet J, Marty C. Pelvic incidence : a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liliang PC, Lu K, Liang C, Tsai Y, Wang K, Chen H. Sacroiliac joint pain after lumbar and lumbosacral fusion : findings using dual sacroiliac joint blocks. Pain Med. 2011;12:565–570. doi: 10.1111/j.1526-4637.2011.01087.x. [DOI] [PubMed] [Google Scholar]
- 23.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J. 2011;20(Suppl 5):572–577. doi: 10.1007/s00586-011-1923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mac-Thiong JM, Wang Z, de Guise JA, Labelle H. Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis. Spine (Phila Pa 1976) 2008;33:2316–2325. doi: 10.1097/BRS.0b013e318186b236. [DOI] [PubMed] [Google Scholar]
- 25.Mac-Thiong JM, Labelle H, Charlebois M, Huot M-P, de Guise J. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine (Phila Pa 1976) 2003;28:1404–1409. doi: 10.1097/01.BRS.0000067118.60199.D1. [DOI] [PubMed] [Google Scholar]
- 26.Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976) 1996;21:1889–1892. doi: 10.1097/00007632-199608150-00012. [DOI] [PubMed] [Google Scholar]
- 27.Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J. 2005;14:654–658. doi: 10.1007/s00586-004-0692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morel E, Ilharreborde B, Lenoir T, Hoffmann E, Vialle R, Rillardon L, et al. [Sagittal balance of the spine and degenerative spondylolisthesis] Rev Chir Orthop Reparatrice Appar Mot. 2005;91:615–626. doi: 10.1016/s0035-1040(05)84465-4. [DOI] [PubMed] [Google Scholar]
- 29.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 30.Schwab F, Lafage V, Patel A, Farcy J. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 31.Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995;20:31–37. doi: 10.1097/00007632-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Shin MH, Ryu KS, Hur JW, Kim JS, Park CK. Comparative Study of Lumbopelvic Sagittal Alignment Between Patients With and Without Sacroiliac Joint Pain After Lumbar Interbody Fusion. Spine (Phila Pa 1976) 2013 doi: 10.1097/BRS.0b013e3182a0da47. [DOI] [PubMed] [Google Scholar]
- 33.Vialle R, Ilharreborde B, Dauzac C, Lenoir T, Rillardon L, Guigui P. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J. 2007;16:1641–1649. doi: 10.1007/s00586-007-0348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]