Abstract
Bow hunter's syndrome (BHS) is rare cause of vertebrobasilar insufficiency that arises from mechanical compression of the vertebral artery by head rotation. There is no standardized diagnostic regimen or treatment of BHS. Recently, we experienced 2 cases resisted continues medication and treated by surgical approach. In both cases, there were no complications after surgery and there were improvements in clinical symptoms. Thus, we describe our cases with surgical decompression with a review of the relevant medical literature.
Keywords: Bow hunter's syndrome, Rotational vertebral artery stroke, Vertebrobasilar insufficiency, Decompression, Surgical treatment
INTRODUCTION
Rotational vertebral artery stroke is an uncommon cause of vertebral basilar insufficiency. Bow hunter's syndrome (BHS) is caused by the compression of the dominant vertebral artery (VA) against a fibrous band or osseous prominence by rotational head movement2,6,10), leading to ischemic insult in the vertebrobasilar territory8,14). BHS presents as recurrent attacks of paroxysmal vertigo, nystagmus, and ataxia caused by head rotation5,8,10). Due to the rarity of this pathology, there are no guidelines for its diagnosis and treatment. Recently, we encountered 2 cases, which we present herein along with our surgical approach. In these 2 cases, we were able to achieve successful decompression of the VA; the two patients recovered completely without further clinical symptoms. Therefore, we present these cases with a review of the relevant medical literature.
CASE REPORT
Case 1
A 50-year-old woman had been experiencing paroxysmal vertigo attacks for a 10 month period prior to visiting our institute. The patient's vertigo was aggravated when she turned her head to the left side. The patient underwent an inner ear exam, which was unremarkable. She was treated with conservative medication for 10 months but did not improve.
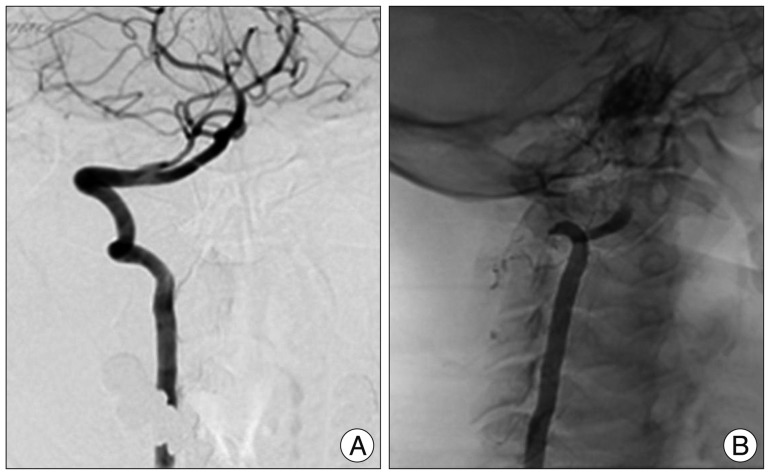
Cerebrovascular images were checked for further evaluation. From angiographic computerized tomography (CT) scans, we observed no definitive abnormal findings except for hypoplastic left VA in the neutral position (Fig. 1). In dynamic vertebral angiography, no steno-occlusive lesions were found in the neutral position (Fig. 2A), but complete occlusion of right VA was found at atlanto-axial level when the patient turned her head to the left side (Fig. 2B).
Fig. 1.
There is no definite vascular lesion on neck angiography 3D CT scans.
Fig. 2.
A 50 year-old woman's right VA angiography with the head in a neutral position. B : The vertebral angiography is complete occluded when the head is fully rotated to the left.
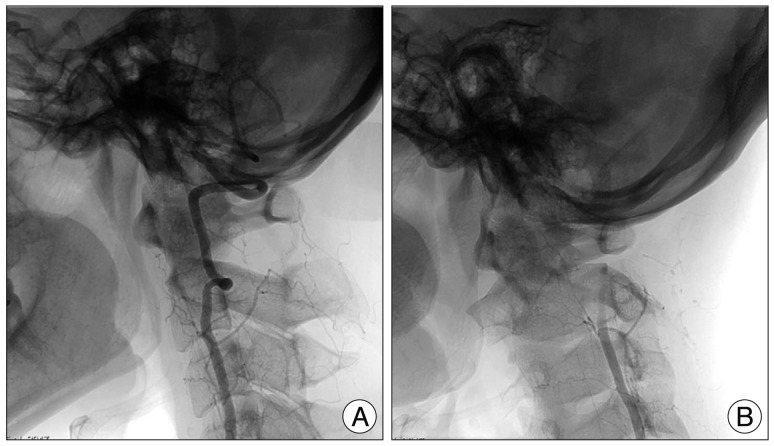
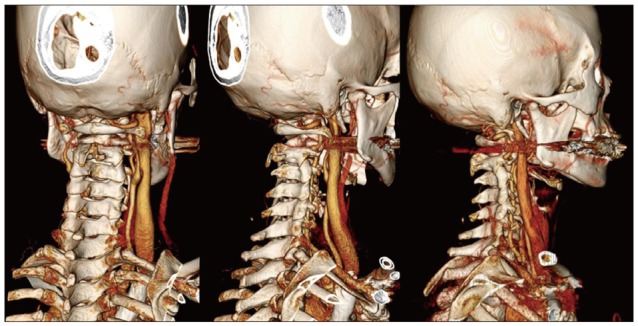
We decided on a surgical decompression of the left VA at the cross transverse foramen of the first cervix as the surgical approach. We placed an adhesive, fibrous bandage between the left VA and the transverse foramen. During the surgical procedure, the bandage was gently dissected and released with decompression of the surrounding bony structure. After surgery, the patient's symptoms improved, and her neck three-dimensional angiography CT scans demonstrated complete decompression of the right vertebral artery (Fig. 3, 4). There were no follow-up complications.
Fig. 3.
Hypoplastic left VA on angiography.
Fig. 4.
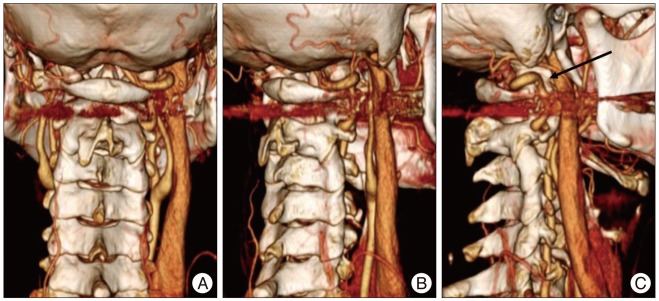
Right transverse process of atlas was removed and right VA is decompressed sufficiently on neck three-dimensional angiography CT scans.
Case 2
A 42-year old woman reported severe vertigo, dizziness, right upper extremity tingling sensations and aggravated syncope when she turned her head to the right. Upon otolaryngological examination, she presented right beating nystagmus when her head was rotated to the right in the sitting or supine position. There were no abnormal findings except for hypoplasia of the posteroinferior cerebellar artery termination of the left VA on magnetic resonance angiography. No significant changes were observed with neck rotational positions.
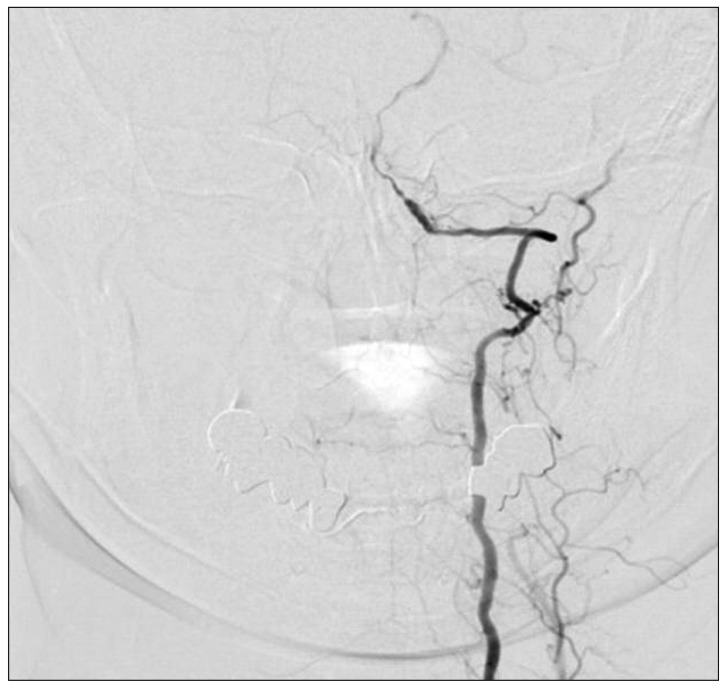
However, dynamic cerebroangiography showed no steno-occlusive lesions of left VA in the neutral position (Fig. 5A), but an occlusion of the left VA was observed at the C1-2 level from right head rotation (Fig. 5B). We performed decompressive surgery based on a diagnosis of BHS. We selected a surgical approach and found an adhesion between the left VA and transverse foramen. We performed a decompressive transversarium foraminectomy.
Fig. 5.
At dynamic cerebroangiography, there are no steno-occlusive lesions of left VA in the neutral position. B: When the patient turns her head to the right, an occlusion of the left VA is observed at the C1-2 level.
After the surgery, CT angiography showed a released left VA. The patient experienced a complete recovery.
DISCUSSION
BHS is syndrome characterized by symptoms such as dizziness, vertigo, and blurred vision when the patient rotates his neck. BHS is defined as symptomatic vertebrobasilar insufficiency by a mechanical occlusion of the vertebral artery during head rotation9). However, because of the collateral blood flow through the contralateral VA and the circle of Willis, VA occlusion does not cause symptoms in most individual cases11). Thus, symptomatic BHS is rare. Because of its rarity, no large-scale established protocols exist for its research, treatment, or diagnosis. We recently encountered 2 cases of BHS. The compressive occlusion of the VA is occurs due to a variety of reasons, including the fibrous band tethering of the VA at the transverse foramina of the C1-C2 junction, as in our cases, and at the point of dural penetration, which is located above the atlantooccipital membrane.
A pathognomonic finding of BHS is the improvement of symptoms when the patient is in a neutral position, even after he claims to have dizziness or blackout when he turns his head to one side. When BHS is suspicious, considerable authors used digital subtraction angiography as the diagnostic modality1). In our cases, clinical symptoms were aggravated when patients turned their head to one side; symptoms were improved when the patients' heads returned to a neutral position. Prior otolaryngological evaluations were unremarkable. Furthermore, we conducted dynamic angiography to confirm occlusive VA lesions toward a diagnosis of BHS. Because of the rarity of this pathology, there are no long term follow-up studies; only prospective studies exist for BHS treatment. Thus, there is no guideline to support the decision to proceed medically or operatively. Because of post-operative complications and the impact on quality of life, some authors have suggested medical treatment (anticoagulation, neck collar applied not to rotate the head, etc.12). However, other patients with BHS who were treated conservatively with medication required surgery because of repeated, aggravated symptoms; after surgery, these patients showed clinical improvement3).
Patients who had vascular decompression for BHS at the atlanto-axial level had shown signs of improvement in several case reports1,4,7,13). Further, many authors also recommend operative treatment for BHS1,7,14).
As mentioned above, there is no definitive guideline for the diagnosis and treatment of BHS because of its rarity. Thus, further studies of BHS are needed to standardize its diagnosis and treatment.
CONCLUSION
Dynamic angiography represents a diagnostic method for the accurate diagnosis of BHS. The surgical decompression of mechanical VA compressions constitutes an appropriate treatment with a good prognosis.
References
- 1.Cornelius JF, George B, N'Dri Oka D, Spiriev T, Steiger HJ, Hanggi D. Bow-hunter's syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction--a management algorithm based on a systematic review and a clinical series. Neurosurg Rev. 2012;35:127–135. doi: 10.1007/s10143-011-0343-4. discussion 135. [DOI] [PubMed] [Google Scholar]
- 2.Diaz FG, Ausman JI, Shrontz C, Pearce J, Gehring R, Mehta B, et al. Surgical correction of lesions affecting the second portion of the vertebral artery. Neurosurgery. 1986;19:93–100. doi: 10.1227/00006123-198607000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Grossmann RI, Davis KR. Positional occlusion of the vertebral artery : a rare cause of embolic stroke. Neuroradiology. 1982;23:227–230. doi: 10.1007/BF00342548. [DOI] [PubMed] [Google Scholar]
- 4.Horowitz M, Jovin T, Balzar J, Welch W, Kassam A. Bow hunter's syndrome in the setting of contralateral vertebral artery stenosis : evaluation and treatment options. Spine (Phila Pa 1976) 2002;27:E495–E498. doi: 10.1097/00007632-200212010-00015. [DOI] [PubMed] [Google Scholar]
- 5.Kuether TA, Nesbit GM, Clark WM, Barnwell SL. Rotational vertebral artery occlusion : A mechanism of vertebrobasilar insufficiency. Neurosurgery. 1997;41:427–432. doi: 10.1097/00006123-199708000-00019. discussion 432-423. [DOI] [PubMed] [Google Scholar]
- 6.Lu DC, Gupta N, Mummaneni PV. Minimally invasive decompression of a suboccipital osseous prominence causing rotational vertebral artery occlusion. Case report. J Neurosurg Pediatr. 2009;4:191–195. doi: 10.3171/2009.3.PEDS08270. [DOI] [PubMed] [Google Scholar]
- 7.Matsuyama T, Morimoto T, Sakaki T. Comparison of c1-2 posterior fusion and decompression of the vertebral artery in the treatment of bow hunter's stroke. J Neurosurg. 1997;86:619–623. doi: 10.3171/jns.1997.86.4.0619. [DOI] [PubMed] [Google Scholar]
- 8.Shimizu T, Waga S, Kojima T, Niwa S. Decompression of the vertebral artery for bow-hunter's stroke. Case report. J Neurosurg. 1988;69:127–131. doi: 10.3171/jns.1988.69.1.0127. [DOI] [PubMed] [Google Scholar]
- 9.Sorensen BF. Bow hunter's stroke. Neurosurgery. 1978;2:259–261. doi: 10.1227/00006123-197805000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Strupp M, Planck JH, Arbusow V, Steiger HJ, Bruckmann H, Brandt T. Rotational vertebral artery occlusion syndrome with vertigo due to "labyrinthine excitation". Neurology. 2000;54:1376–1379. doi: 10.1212/wnl.54.6.1376. [DOI] [PubMed] [Google Scholar]
- 11.Tominaga T, Takahashi T, Shimizu H, Yoshimoto T. Rotational vertebral artery occlusion from occipital bone anomaly : a rare cause of embolic stroke. Case report. J Neurosurg. 2002;97:1456–1459. doi: 10.3171/jns.2002.97.6.1456. [DOI] [PubMed] [Google Scholar]
- 12.Wakayama K, Murakami M, Suzuki M, Ono S, Shimizu N. Ischemic symptoms induced by occlusion of the unilateral vertebral artery with head rotation together with contralateral vertebral artery dissection--case report. J Neurol Sci. 2005;236:87–90. doi: 10.1016/j.jns.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Wang S, Wang C, Liu Y, Yan M, Zhou H. Anomalous vertebral artery in craniovertebral junction with occipitalization of the atlas. Spine (Phila Pa 1976) 2009;34:2838–2842. doi: 10.1097/BRS.0b013e3181b4fb8b. [DOI] [PubMed] [Google Scholar]
- 14.Yang PJ, Latack JT, Gabrielsen TO, Knake JE, Gebarski SS, Chandler WF. Rotational vertebral artery occlusion at c1-c2. AJNR Am J Neuroradiol. 1985;6:96–100. [PMC free article] [PubMed] [Google Scholar]