Abstract
Background
The onset of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) typically involves reductions in activities of daily living and social interactions (jointly referred to as “illness burden”). Emotional distress has been linked to increased reported symptoms, and stress management skills have been related to lower fatigue severity in CFS patients. Symptom severity and illness burden are highly correlated. The ability to manage stress may attenuate this relationship, allowing individuals to feel less burdened by the illness independent of the severity of their symptoms.
Purpose
This study aimed to evaluate if perceived stress management skills affect illness burden via emotional distress, independent of ME/CFS symptom severity.
Methods
A total of 117 adults with ME/CFS completed measures of perceived stress management skills, emotional distress, ME/CFS symptom severity and illness burden.
Results
Regression analyses revealed that greater perceived stress management skills related to less social and fatigue-related illness burden, via lower emotional distress. This relationship existed independent of the association of symptom severity on illness burden, and was stronger among those not currently employed.
Conclusions
Ability to manage stress is associated with a lower illness burden for individuals with ME/CFS. Future studies should evaluate the efficacy of psychosocial interventions in lowering illness burden by targeting stress management skills.
Keywords: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, stress management, emotional distress, illness burden
Introduction
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a prevalent disabling disorder (estimated at 400,000 to 800,000; 1, 2) with a substantial physical, emotional and economic burden (estimated at $9.1 billion annually in lost productivity; 3). Symptoms of this disorder include profound fatigue, post-exertional malaise, sleep dysfunction, pain, and cognitive impairments. The onset of ME/CFS, typically involves a number of substantive decrements in an individual's day-to-day functioning (4, 5). These changes can include limitations on general activities of daily living, such as bathing and dressing oneself, as well as limitations on social interactions, such as visiting with others. These perceived limitations can be conceptualized as an individual's illness burden.
In the context of ME/CFS, one's illness burden can be further delineated into: a) fatigue-related illness burden, which encompasses general interference in activities of daily living due to fatigue, a cardinal symptom of the syndrome, and b) social illness burden, which encompasses limitations in social interactions. Across a variety of health conditions, there is a positive correlation between illness symptom severity and illness burden (6-8). Due to the multi-systemic and unpredictable nature of ME/CFS and because effective treatments are lacking, there is a need to identify factors that can reduce the burden of illness and improve daily functioning among ME/CFS patients who must deal with ongoing symptoms. The discovery of these factors capable of reducing the burden of illness in afflicted individuals is of utmost importance to clinical researchers as these factors can then be utilized as targets of interventions.
Psychosocial factors, such as coping skills, may impact the relationship between the severity of illness and the overall burden of the illness because such skills may mitigate the emotional distress associated with managing the illness. In the case of ME/CFS, individuals lacking the skills to manage the challenges of the illness may have low self-efficacy and underestimate their abilities to engage in activities, leading to withdrawal, greater distress, and a higher illness burden. In contrast, those with more adequate coping skills to manage such challenges may show better adaptation to illness, less distress, and a lower illness burden (9, 10).
It has been repeatedly observed that stressors and emotional distress may exacerbate ME/CFS symptoms (10-13) and we have formulated a model to explain this association (14). The hypothesized model follows the Folkman and Lazarus (15) definition of stress, which states that stress occurs when a situation is appraised by the individual as exceeding his or her personal resources. Therefore, emotional distress (decreases) would occur after the initial utilization of personal stress management resources. This model has been used in other cross-sectional studies involving clinical populations dealing with physical symptoms (16, 17).
Our research group previously found that greater perceived stress management skills were associated with lower levels of fatigue severity via lowered levels of emotional distress suggesting that fluctuations in emotional distress may mediate symptom severity (18). Other work demonstrated that teaching stress management skills (such as the effective use of relaxation techniques and cognitive restructuring) may reduce emotional distress and mitigate ME/CFS symptoms (19). Thus, increasing levels of perceived stress management skills may work on symptoms by reducing distress. It is also plausible that stress management skills are applied by CFS patients to reinterpret the impact of symptoms on their day-to-day illness burden as they reduce their emotional distress.
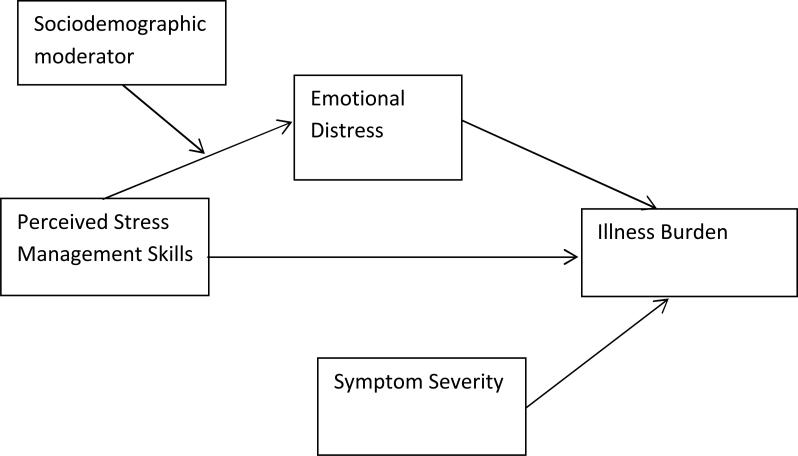
This study examined whether greater perceived stress management skills are associated with lower reports of both general and social illness burden, independent of ME/CFS symptom severity. Based on our theoretical model, we hypothesized that having greater perceived stress management skills relates to less fatigue-related and social illness burden via lower emotional distress (see Figure 1). Because individuals experiencing significant emotional distress may disengage from their social environment (20, 21), we hypothesized that these relationships would be greatest for social illness burden, which includes willing participation in social activities. Because coping skills and emotional distress processes have been found to differ across the lifespan (22, 23), among men and women (24-26), and among employed compared to unemployed persons, such that employed individuals may demonstrate more positive coping strategies (27, 28), age, gender and employment status were examined as moderators of the effects of perceived stress management skills on markers of illness burden via emotional distress.
Figure 1.
Theoretical model
Methods
Participants and Procedures
Participants in the present study were recruited primarily through physician referral for a larger telephone-delivered intervention study. Initial eligibility was determined by the presence of a physician-determined ME/CFS diagnosis according to the Centers for Disease Control (CDC) criteria (29). Participants were required to be fluent in English, live within the study area, have an active home telephone line, and be between the ages of 21 and 75 years. A telephone screening interview was used to determine eligibility. The Short Portable Mental Status Questionnaire (30) was used to determine cognitive impairment. Participants were excluded if they made four or more errors on this measure, as four or more errors indicate cognitive impairment. Potential participants were also excluded if they had a medical condition (e.g., AIDS, lupus, rheumatoid arthritis) that would influence biological processes associated with CFS symptomology, or if they had a past psychiatric hospitalization, met criteria for schizophrenia, bipolar disorder, or substance abuse, or were actively suicidal. Potential psychiatric exclusions were assessed using a brief screening adapted from the Structured Clinical Interview for the DSM-IV (31).
Interested participants who were deemed eligible for the study signed an informed consent form approved by a University-based Institutional Review Board. Following enrollment, participants received a home visit by a member of the study staff. During this visit, a battery of measures examining ME/CFS symptoms and participants’ psychosocial status was administered. Participants were each compensated $50 for their time and effort.
Measures
Perceived stress management skills
The Measure of Current Status (MOCS;32) was used to assess perceived stress management skills. Participants were asked to rate their perceived ability to appropriately respond to challenges and demands of daily life on a 5 point scale which ranged from “1 - I cannot do this at all” to “5 – I can do this extremely well.” Items on the MOCS are based on tendencies and behaviors that are associated with efficient stress management, such as “I am able to use mental imagery to reduce any tension I experience” and “I can clearly express my needs to other people who are important to me.” Higher scores on the MOCS indicate better perceived stress management skills. Consistent with past research using the MOCS for men with localized prostate cancer (33), the items on the MOCS were summed to create an overall stress management measure. In the present study, the MOCS demonstrated adequate psychometric properties and had a high degree of internal consistency (Cronbach's α = .85).
Emotional distress
The Perceived Stress Scale (PSS; 34), the Center for Epidemiologic Studies Depression Scale (CES-D; 35), and the Profile of Mood States (POMS) Depression-Dejection and Anxiety-Tension subscales (36) were administered to assess the degree of emotional distress during the prior week. Consistent with past research suggesting that feelings of perceived stress, depression and anxiety contribute to the total experience of emotional distress (37, 38), an emotional distress composite score was created by summing the z-scores of the PSS, CES-D, POMS Depression-Dejection and POMS Anxiety-Tension subscales. This composite score demonstrated a high degree of internal consistency in the present sample (Cronbach's α = .89).
ME/CFS symptom severity
The total score from the CDC Symptom Inventory (39) was used to measure ME/CFS symptom severity over the past month. Participants were asked to separately rate the frequency and intensity of 20 ME/CFS-related symptoms on 5 point scales. The frequency and intensity scales were then summed and multiplied to create the total symptom severity score. These 20 symptoms include the 8 case definition symptoms (29) as well as other common ME/CFS-related symptoms, such as sleeping problems, stomach or abdominal pain, and sensitivity to light. This measure has been shown to be a reliable measure of ME/CFS symptoms (39) and demonstrated a high degree of internal consistency in the present sample (Cronbach's α = .83).
Fatigue-related illness burden
The degree to which participants were generally burdened by their fatigue was measured using the Interference subscale of the Fatigue Symptom Inventory (FSI; 40). This scale consists of 7 items which are answered on an 11-point scale ranging from “0 – no interference” to “10 – extreme interference.” Items on this measure ask participants to rate how much, in the past week, fatigue interfered with various activities including their “ability to bathe and dress” independently, and their “ability to concentrate.” In the current study, the general illness burden measure demonstrated a high degree of internal consistency (Cronbach's α = .85).
Social illness burden
The degree to which participants experienced declines in social activities as a result of their illness was measured using the Social Interaction subscale from the Sickness Impact Profile (SIP; 41). Participants were asked whether or not they engaged in a range of socially-relevant behaviors as a result of their illness and provided dichotomous responses of “yes” or “no.” Sample items from this scale include “I isolate myself as much as I can from the rest of the family” and “I am doing fewer social activities with groups of people.” This measure demonstrated adequate internal consistency in the present sample (Cronbach's α = .74).
Statistical Analyses
Statistical analyses were performed using SPSS version 18.0. Linear regressions and Pearson correlations were conducted to examine the relationships between socio-demographic factors, perceived stress management skills, emotional distress and measures of illness burden. In order to examine the proposed indirect relationships between perceived stress management skills and illness burden via emotional distress, an SPSS macro developed by Preacher and Hayes (42) was used. This macro allows for the estimation of indirect effects with covariates included in the model, and calculates the bias-corrected bootstrapped confidence intervals for the indirect effect. Bootstrapped confidence intervals were used to assess for indirect effect because this method does not assume normality of the distribution of the indirect effect, which provides increased sensitivity to detecting effects compared to more traditional methods, such as Baron and Kenny (43) or the Sobel test (44). Further, this method is recommended for small to medium sample sizes (42). In the present study, perceived stress management skills served as the independent variable, emotional distress served as the mediator, and fatigue-related illness burden and social illness burden served as the dependent variables in two separate models. In order to examine these relationships independent of ME/CFS symptom severity, the total score from the CDC Symptom Inventory (39) was included as a covariate in both models. To examine potential sociodemographic (age, gender and employment status) moderators of the indirect effects models (see figure 1), another SPSS macro developed by developed by Preacher and colleagues (45) was used. This macro generates an omnibus interaction effect and provides a method for examining the significance of the indirect effect at different levels the proposed moderator. The total score from the CDC Symptom Inventory (39) was again included as a covariate in the moderated mediation model.
Results
Study Sample
Of the 161 men and women approached to participate in the study, 134 individuals were eligible and 17 declined participation in the study, primarily due to time constraints, resulting in a final sample of 117. Major reasons for ineligibility included living outside the study area (40%), not having a ME/CFS diagnosis (22%), and having an exclusionary medical condition (19%). None of the potential participants were excluded for cognitive impairment. The majority of participants in the sample were women (72%) and non-Hispanic White (79.5%). The average age was 50.7 years (SD = 11.5) and participants were highly educated, with 87.2% of the sample having had attended at least some college. At the time of assessment, approximately 42.7% of the sample was married. The majority of participants (66.2%) were not working, with 40.2% of participants on disability, 13.7% unemployed, and 10.3% retired.
Although official eligibility criteria for the study stated that participants needed to have a ME/CFS diagnosis based on the Fukuda (29) case definition, 109 participants were recruited from a clinic that also utilizes the Carruthers (2003) case definition for ME/CFS (46). Therefore, in addition to meeting the Fukuda criteria (fatigue of > 6 months duration and 4 of 8 symptom criteria including fatigue, myalgia, arthralgia, headache of a new and different type, nonrestorative sleep, cognitive complaints, sore throat and tender lymph nodes), these participants also met the Carruthers criteria—exercise-induced relapse and symptoms from at least of 3 categories (immune, autonomic, endocrine). The other 8 participants enrolled in the study had their ME/CFS diagnosis confirmed using solely the Fukuda (1994) definition. There were no differences on main study variables between those participants meeting both the Carruthers and the Fukuda case definitions, versus those meeting the Fukuda (29) case definition alone (all p's > .20)
Preliminary Analyses
Results of correlations examining the relationships between the study variables are presented in Table 1. As hypothesized, total ME/CFS symptom severity was positively associated with both fatigue-related illness burden and social illness burden (p's < .05). Significant relationships were found between employment status and age, symptom severity, and social illness burden such that unemployed participants were older, reported a greater symptom severity, and reported higher levels of social illness burden compared to currently employed participants (p's < .05).
Table 1.
Pearson correlations between study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1 Age | - | |||||||
| 2 Gender | .09 | - | ||||||
| 3 Partner Status | .04 | −.04 | - | |||||
| 4 Employment Status | −.29** | −.17 | −.08 | - | ||||
| 5 Total Symptom Severity | −.11 | .17 | −.00 | −.20* | - | |||
| 6 Social Illness Burden | −.02 | −.03 | .02 | −.19* | .253** | - | ||
| 7 General Illness Burden | −.01 | .02 | .01 | −.14 | .41** | .46** | - | |
| 8 Stress Management Skills | −.13 | −.13 | .05 | −.02 | −.06 | −.34** | −.16 | - |
| 9 Emotional Distress | −.07 | .15 | −.06 | −.13 | .25* | .44** | .46** | −.46** |
significant at 0.05 level
significant at 0.01 level
Stress Management Skills, Emotional Distress and Indicators of Illness Burden
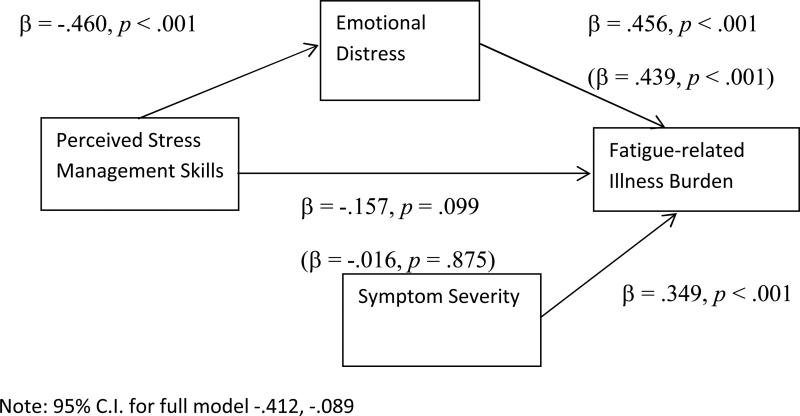
Fatigue-related illness burden
Perceived stress management skills were not directly related to fatigue-related illness burden (β = −.157, p = .099) while emotional distress was significantly related to fatigue-related illness burden (β = .456, p < .001). However, as seen in figure 2, greater perceived stress management skills were related to less emotional distress (β = −.460, p < .001). Using bootstrapping, statistical support was found for an indirect effect model. The 95% confidence interval for emotional distress as a mediator was −.412 to −.089. Mediation was indicated by the fact that this confidence interval did not contain zero, providing support that the indirect effect is significantly different than zero. These findings support the hypothesis that greater perceived stress management skills relate to lower fatigue-related illness burden reports via lower emotional distress. These paths existed independent of the effect of ME/CFS symptom severity, which remained a significant predictor in the model (β = .349, p < .001).
Figure 2.
The indirect effect of perceived stress management skills on fatigue-related illness burden
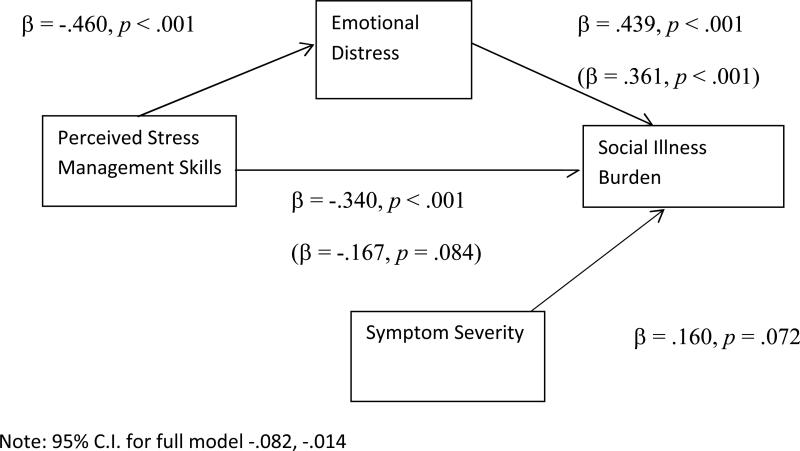
Social illness burden
Results of linear regression analyses indicated that perceived stress management skills were negatively correlated with social illness burden (β = −.340, p < .001). Conversely, emotional distress was positively related to social illness burden (β = .439, p < .001). As noted previously, greater perceived stress management skills related to less emotional distress. As seen in figure 3, the addition of emotional distress to the model in which perceived stress management skills predicted social illness burden created a non-significant relationship between perceived stress management skills and social illness burden (β = −.167, p = .084). Further, based on 1000 bootstrap resamples, the 95% confidence interval for emotional distress as a mediator was −.082 to −.014. Mediation was indicated by the fact that this confidence interval did not contain zero. These findings support the hypothesis that greater perceived stress management skills relate to lower social illness burden reports via lower emotional distress. These paths existed independent of the effect of ME/CFS symptom severity, which did not remain significant in this model (β = .160, p = .072).
Figure 3.
The indirect effect of perceived stress management skills on social illness burden
Sociodemographic Moderator Analyses
Age, employment status and gender were examined as possible moderators of the indirect effect of perceived stress management skills on illness burden via emotional distress. Due to the finding that older participants were less likely to be employed at time of assessment, age was included as an additional covariate when examining employment status as a moderator of the indirect effect model. Neither age, employment status nor gender served as a moderator in the indirect effect model predicting fatigue-related illness burden (p's > .05).
When examining the indirect effect model predicting social illness burden, employment status was a significant moderator (p < .01), such that the relationship between perceived stress management skills and social illness burden via lowered emotional distress was stronger for individuals who were not working at the time of assessment (p = .015) than for individuals who were employed (p = .051). Based on 1000 bootstrap resamples, the 95% confidence interval for emotional distress as a mediator was −.097 to −.015 for those who were not working, and was −.082 to −.016 for those who were employed, indicating that the indirect effect of perceived stress management skills on social illness burden was significantly different from zero in both groups. Gender and age did not serve as moderators in the indirect effect model predicting social illness burden (p's > .05).
Discussion
The present study examined relationships between perceived stress management skills, emotional distress, and illness burden among adults with ME/CFS. Our past work has demonstrated that having greater perceived stress management skills relates to a lower fatigue symptom severity via the influence of greater perceived stress management skills on emotional distress levels (18). These past findings were consistent with research on individuals with cancer diagnoses showing that greater perceived stress management skills relate to less distress and greater physical and emotional health-related quality of life (17, 37). Here, we demonstrate that having greater perceived stress management skills are associated with a lower illness burden, via lowered emotional distress, and that these relationships exist independent of total symptom severity. We also demonstrated that the relation between perceived stress management skills and one's social illness burden was stronger than the relation between perceived stress management skills and one's general fatigue-related illness burden.
Results of the present study indicated that the indirect effect model in which greater perceived stress management skills related to a lower fatigue-related illness burden was not moderated by age, gender or employment status. The lack of moderation in the aforementioned indirect effect model demonstrated that, regardless of age, gender or employment status, individuals with good perceived stress management skills reported a lower fatigue-related illness burden and were better able to maintain activities of daily living such as self-grooming and completing tasks in the home.
However, moderation was evident in the indirect effect model in which greater perceived stress management skills related to a lower social illness burden. Specifically, the indirect effect was found to be stronger among those who were not working at the time of assessment compared to those who were employed, although the relationship was significant for both groups. These results suggest people who are not currently employed may particularly benefit from stress management training. These are novel findings in the literature on stress management in ME/CFS, but are consistent with past research indicating differences in coping with stress and social adjustment between chronically ill individuals who are employed compared to those who are not currently working (27, 28). Contrary to our hypothesis, gender and age did not moderate the indirect effect model in which greater perceived stress management skills related to a lower social illness burden, indicating the men and women across the age continuum responded in similar patterns.
The moderation results should be interpreted with caution. Although the social interaction subscale of the SIP, used to quantify social illness burden does refer to work-related social activities, it is possible that work-related social contact, which is inherent in many work environments, influenced participants’ recall of their social activities (41). More sensitive assessments, such as calendar tracking of social activities, are needed to further elucidate the potential differential impact of stress management skills on individuals’ social illness burden among those who are employed and those who are not currently working. Based on commonly observed differences in stress and coping among different ethnic groups (48, 49), the indirect effect model in which greater perceived stress management skills related to a lower illness burden may be moderated by ethnicity. However, the ethnic homogeneity of the present sample did not provide us with the ability to reliably assess differences by ethnic group.
There are a few notable limitations of the present study. Information regarding the nature of participants’ illness onset (sudden versus gradual) was not collected. Given past research suggesting more severe symptoms in those with a sudden onset of illness compared to a gradual illness onset (50), the observed relationships should be separately examined in these subgroups of participants in the future. Analyses were based on a cross-sectional design; therefore caution should be used in interpreting the relationships. The associations between perceived stress management skills, emotional distress, and illness burden may be bi-directional, such that individuals who experienced a high illness burden responded with increased emotional distress and deemed themselves less able to manage current stressors. These relationships should be further examined longitudinally to more clearly delineate if greater stress management skills lead to lower emotional distress, or if less distressed individuals perceive themselves as more capable of managing stressors.
Additionally, the present study relied on self-report measures. Although the self-report measures of emotional distress, perceived stress management skills, and illness burden have been well validated, the reliance on self-report measures alone may have introduced a common methods bias that may account for some of the observed relationships between variables (51). The use of a dichotomous measure of social illness burden (SIP; 41) compared to the likert-type measure for fatigue-related illness burden (FSI; 40) may partially account for the observed differences in relation strength between perceived stress management skills and the illness burden variables. While the CDC Symptom Inventory (39) is a validated self-report measure of ME/CFS symptoms, there are more commonly used measures, such as the Chalder Fatigue Scale (52). The use of the CDC Symptom Inventory may be considered a limitation of this study as it is not directly comparable to research using the Chalder Fatigue Scale. Further, while fatigue is a central symptom of ME/CFS, fatigue-related illness burden may not encompass the full extent to which one's symptoms burden general life activities, since other symptoms (such as pain) may have separate and significant impacts. There is a definite need to develop more comprehensive and consistent measures of illness burden to further elucidate our understanding of various aspects of living with a chronic illness.
Despite these limitations, results of the present study contribute to the limited literature on modifiable psychological constructs that contribute to the illness burden of both men and women with ME/CFS. This is the first study to demonstrate the potential health benefits of stress management skills on day-to-day functioning with an illness, while accounting for the impact of illness symptom severity. Considering the long, continued search for appropriate medical treatments for individuals with ME/CFS, these findings offer hope that interventions which enhance stress management skills may reduce the burden of illness among individuals with ME/CFS. Previously, a small pilot study demonstrated cognitive-behavioral stress management (CBSM) group intervention's ability to decrease both symptom severity and perceived stress, while improving self-reported quality of life (19). However, the small sample size in the pilot study limited the investigators’ ability to adequately examine the mechanisms by which these benefits were attained. The present study offers a model to tailor psychosocial interventions to improve day-to-day functioning of individuals with ME/CFS.
References
- 1.Jason LA, Richman JA, Rademaker AW, Jordan KM, Plioplys AV, Taylor RR, McCready W, Huang CF, Plioplys S. A community-based study of Chronic Fatigue Syndrome. Arch Intern Med. 1999;159:2129–37. doi: 10.1001/archinte.159.18.2129. [DOI] [PubMed] [Google Scholar]
- 2.Reyes M, Nisenbaum R, Hoaglin DC, Unger ER, Emmons C, Randall B, Stewart JA, Abbey S, Jones JF, Gantz N, Minden S, Reeves WC. Prevalence and incidence of Chronic Fatigue Syndrome in Wichita, Kansas. Arch Intern Med. 2003;163:1530–6. doi: 10.1001/archinte.163.13.1530. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds KJ, Vernon SD, Bouchery E, Reeves WC. The economic impact of Chronic Fatigue Syndrome. Cost Eff Resour Alloc. 2004;2:e4. doi: 10.1186/1478-7547-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson JS, Ferrans CE. The quality of life of persons with chronic fatigue syndrome. J Nerv Ment Dis. 1997 Jun;185(6):359–67. doi: 10.1097/00005053-199706000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Hardt J, Buchwald D, Wilks D, Sharpe M, Nix WA, Egle UT. Health-related quality of life in patients with chronic fatigue syndrome: an international study. J Psychosom Res. 2001 Aug;51(2):431–4. doi: 10.1016/s0022-3999(01)00220-3. [DOI] [PubMed] [Google Scholar]
- 6.Amato MP, Ponziani G, Rossi F, Liedl CL, Stefanile C, Rossi L. Quality of life in multiple sclerosis: the impact of depression, fatigue and disability. Mult Scler. 2001 Oct;7(5):340–4. doi: 10.1177/135245850100700511. [DOI] [PubMed] [Google Scholar]
- 7.Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR. Fatigue in breast cancer survivors: Occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000 Feb;18(4):743–53. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 8.van de Port IG, Kwakkel G, Schepers VP, Heinemans CT, Lindeman E. Is fatigue an independent factor associated with activities of daily living, instrumental activities of daily living and health-related quality of life in chronic stroke? Cerebrovasc Dis. 2007;23(1):40–5. doi: 10.1159/000095757. [DOI] [PubMed] [Google Scholar]
- 9.Antoni MH, Brickman A, Lutgendorf S, Klimas N, Imia-Fins A, Ironson G, Quillan R, Miguez MJ, van Riel F, Morgan R, Patarca R, Fletcher MA. Psychosocial correlates of illness burden in Chronic Fatigue Syndrome. Clin Infectious Diseases. 1994;18(Suppl 1):S73–8. doi: 10.1093/clinids/18.supplement_1.s73. [DOI] [PubMed] [Google Scholar]
- 10.Lutgendorf SK, Antoni MH, Fletcher MA, Penedo F, Baum A, Schneiderman N, Klimas N. Physical symptoms of chronic fatigue syndrome are exacerbated by the stress of Hurricane Andrew. Psychosomatic Medicine. 1995;57(4):310–23. doi: 10.1097/00006842-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Gaab J, Rohleder N, Heitz V, Engert V, Schad T, Schürmeyer TH, Ehlert U. Stress-induced changes in LPS-induced pro-inflammatory cytokine production in chronic fatigue syndrome. Psychoneuroendocrinology. 2005;30:188–98. doi: 10.1016/j.psyneuen.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Faulkner S, Smith A. A longitudinal study of the relationship between psychological distress and recurrence of upper respiratory tract infections in chronic fatigue syndrome. British J of Health Psychol. 2008;13(1):177–86. doi: 10.1348/135910706X171469. [DOI] [PubMed] [Google Scholar]
- 13.Nas K, Cevik R, Batum S, Sarac AJ, Acar S, Kalkanli S. Immunologic and psychosocial status in Chronic Fatigue Syndrome. Bratislava Med J. 2011;112(4):208–12. [PubMed] [Google Scholar]
- 14.Antoni MH, Weiss DE. Stress, immunity and chronic fatigue syndrome: A conceptual model to guide the development of treatment and research. In: Jason PF LA, Taylor R, editors. Handbook of chronic fatigue syndrome and fatiguing illnesses. John Wiley & Sons, Inc.; New York: 2003. [Google Scholar]
- 15.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer Publishing Company; 1984. [Google Scholar]
- 16.Faul LA, Jim HS, Williams C, Loftus L, Jacobsen PB. Relationship of stress management skill to psychological distress and quality of life in adults with cancer. Psycho-Oncology. 2010;19:102–9. doi: 10.1002/pon.1547. [DOI] [PubMed] [Google Scholar]
- 17.Penedo FJ, Benedict C, Zhou ES, Rasheed M, Traeger L, Kava BR, Soloway M, Czaja S, Antoni MH. Association of stress management skills and perceived stress with physical and emotional well-being among advanced prostrate cancer survivors following androgen deprivation treatment. J Clin Psychol Med Settings. 2013 Mar;20(1):25–32. doi: 10.1007/s10880-012-9308-1. [DOI] [PubMed] [Google Scholar]
- 18.Lattie EG, Antoni MH, Fletcher MA, Penedo F, Czaja S, Lopez C, Perdomo D, Sala A, Nair S, Fu SH, Klimas N. Stress management skills, neuroimmune processes and fatigue levels in persons with chronic fatigue syndrome. Brain Behav Immun. 2012 Aug;26(6):849–58. doi: 10.1016/j.bbi.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez C, Antoni M, Penedo F, Weiss D, Cruess S, Segotas MC, Helder L, Siegel S, Klimas N, Fletcher MA. A pilot study of cognitive behavioral stress management effects on stress, quality of life, and symptoms in persons with chronic fatigue syndrome. J Psychosom Res. 2011;70:328–34. doi: 10.1016/j.jpsychores.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epping-Jordan JE, Compas BE, Osowiecki DM, Oppedisano G, Gerhardt C, Primo K, Krag DN. Psychological adjustment in breast cancer: processes of emotional distress. Health Psychol. 1999 Jul;18(4):315–26. doi: 10.1037//0278-6133.18.4.315. [DOI] [PubMed] [Google Scholar]
- 21.Holmes JA, Stevenson CAZ. Differential-Effects of Avoidant and Attentional Coping Strategies on Adaptation to Chronic and Recent-Onset Pain. Health Psychol. 1990;9(5):577–84. doi: 10.1037//0278-6133.9.5.577. [DOI] [PubMed] [Google Scholar]
- 22.Aldwin CM, Sutton KJ, Chiara G, Spiro A., 3rd Age differences in stress, coping, and appraisal: findings from the Normative Aging Study. The journals of gerontology Series B, Psychological sciences and social sciences. 1996;51(4):P179–88. doi: 10.1093/geronb/51b.4.p179. [DOI] [PubMed] [Google Scholar]
- 23.Folkman S, Lazarus RS, Pimley S, Novacek J. Age differences in stress and coping processes. Psychol Aging. 1987;2(2):171–84. doi: 10.1037//0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- 24.Brougham RR, Zail CM, Mendoza CM, Miller JR. Stress, Sex Differences, and Coping Strategies Among College Students. Curr Psychol. 2009 Jun;28(2):85–97. [Google Scholar]
- 25.Matud MP. Gender differences in stress and coping styles. Pers Indiv Differ. 2004 Nov;37(7):1401–15. [Google Scholar]
- 26.Ptacek JT, Smith RE, Dodge KL. Gender Differences in Coping with Stress - When Stressor and Appraisals Do Not Differ. Pers Soc Psychol B. 1994 Aug;20(4):421–30. [Google Scholar]
- 27.Lutgendorf SK, Antoni MH, Ironson G, Starr K, Costello N, Zuckerman M, Klimas N, Fletcher MA, Schneiderman N. Changes in cognitive coping skills and social support during cognitive behavioral stress management intervention and distress outcomes in symptomatic human immunodeficiency virus (HIV)-seropositive gay men. Psychosom Med. 1998 Mar-Apr;60(2):204–14. doi: 10.1097/00006842-199803000-00017. [DOI] [PubMed] [Google Scholar]
- 28.Pakenham KI, Rinaldis M. The role of illness, resources, appraisal, and coping strategies in adjustment to HIV/AIDS: the direct and buffering effects. J Behav Med. 2001 Jun;24(3):259–79. doi: 10.1023/a:1010718823753. [DOI] [PubMed] [Google Scholar]
- 29.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A, International Chronic Fatigue Syndrome Study Group The Chronic Fatigue Syndrome: A comprehensive approach to its definition and study. Ann Intern Med. 1994;121(12):953–9. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 30.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J of American Geriatrics Society. 1975;23(10):433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 31.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- 32.Carver CS. Measure of Current Status (MOCS) 2006 Available from: http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html.
- 33.Penedo FJ, Molton I, Dahn JR, Shen BJ, Kinsinger D, Traeger L, Siegel S, Schneiderman N, Antoni M. A randomized clinical trial of group-base cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine. 2006;31(3):261–70. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- 34.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–96. [PubMed] [Google Scholar]
- 35.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychol Measurement. 1977;1(3):385–401. [Google Scholar]
- 36.McNair D, Lorr M, Droppelman LF. Manual: Profile of Mood States. Educational and Industry Testing Service (EDITS); San Diego, CA: 1971. [Google Scholar]
- 37.Motivala SJ, Hurwitz BE, Llabre MM, Klimas NG, Fletcher MA, Antoni MH, LeBlanc WG, Schneiderman N. Psychological distress is associated with decreased memory helper T-cell and B-cell counts in pre-AIDS HIV seropositive men and women but only in those with low viral load. Psychosom Med. 2003;65(4):627–35. doi: 10.1097/01.psy.0000041549.72780.5b. Jul-Aug. [DOI] [PubMed] [Google Scholar]
- 38.Greeson JM, Hurwitz BE, Llabre MM, Schneiderman N, Penedo FJ, Klimas NG. Psychological distress, killer lymphocytes and disease severity in HIV/AIDS. Brain Behav Immun. 2008 Aug;22(6):901–11. doi: 10.1016/j.bbi.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Wagner D, Nisenbaum R, Heim C, Jones JF, Unger ER, Reeves WC. Psychometric properties of the CDC symptom inventory for assessment of Chronic Fatigue Syndrome. Population Health Metrics. 2005;(3)(8) doi: 10.1186/1478-7954-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hann DM, Jacobsen PB, Azzarello LM, Martin SC, Curran SL, Fields KK, Greenberg H, Lyman G. Measurement of fatigue in cancer patients: development and validation of the Fatigue Symptom Inventory. Quality of Life Research. 1998;7:301–10. doi: 10.1023/a:1024929829627. [DOI] [PubMed] [Google Scholar]
- 41.Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: Development and final revision of a health status measure. Medical Care. 1981;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 43.Baron RM, Kenny DA. Moderator-mediator variables distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 44.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological Methodology. Jossey-Bass; San Francisco, CA: 1982. [Google Scholar]
- 45.Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 46.Carruthers BM, Jain AK, De Meirleir KL, Peterson DL, Klimas NG, Lerner AM, Bested AC, Flor-Henry P, Joshi P, Powles ACP, Sherkey JA, van de Sande MI. Myalgic encephalomyelitis/chronic fatigue syndrome: clinical working case definition, diagnostic and treatment protocols. J. Chronic Fatigue Syndr. 2003;11:7–36. [Google Scholar]
- 47.Faul LA, Jim HS, Williams C, Loftus L, Jacobsen PB. Relationship of stress management skill to psychological distress and quality of life in adults with cancer. Psycho-Oncology. 2010;19:102–9. doi: 10.1002/pon.1547. [DOI] [PubMed] [Google Scholar]
- 48.Farley T, Galves A, Dickinson LM, Perez Mde J. Stress, coping, and health: a comparison of Mexican immigrants, Mexican-Americans, and non-Hispanic whites. J Immigr Health. 2005;7(3):213–20. doi: 10.1007/s10903-005-3678-5. [DOI] [PubMed] [Google Scholar]
- 49.Bjorck JP, Cuthbertson W, Thurman JW, Lee YS. Ethnicity, coping, and distress among Korean Americans, Filipino Americans, and Caucasian Americans. J Soc Psychol. 2001;141(4):421–42. doi: 10.1080/00224540109600563. [DOI] [PubMed] [Google Scholar]
- 50.DeLuca J, Johnson SK, Ellis SP, Natelson BH. Sudden vs gradual onset of chronic fatigue syndrome differentiates individuals on cognitive and psychiatric measures. J Psychiatr Res. 1997 Jan-Feb;31(1):83–90. doi: 10.1016/s0022-3956(96)00052-0. [DOI] [PubMed] [Google Scholar]
- 51.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003 Oct;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 52.Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace EP. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147–53. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]