Abstract
Purpose
Integrated urology-radiation oncology (RO) practices have been advocated as a means to improve community-based prostate cancer care by joining urologic and radiation care in a single-practice environment. However, little is known regarding the scope and actual physical integration of such practices. We sought to characterize the emergence of such practices in Texas, their extent of physical integration, and their potential effect on patient travel times for radiation therapy.
Methods and Materials
A telephone survey identified integrated urology-RO practices, defined as practices owned by urologists that offer RO services. Geographic information software was used to determine the proximity of integrated urology-RO clinic sites with respect to the state’s population. We calculated patient travel time and distance from each integrated urology-RO clinic offering urologic services to the RO treatment facility owned by the integrated practice and to the nearest nonintegrated (independent) RO facility. We compared these times and distances using the Wilcoxon-Mann-Whitney test.
Results
Of 229 urology practices identified, 12 (5%) offered integrated RO services, and 182 (28%) of 640 Texas urologists worked in such practices. Approximately 53% of the state population resides within 10 miles of an integrated urology-RO clinic site. Patients diagnosed with prostate cancer at an integrated urology-RO clinic site travel a mean of 19.7 miles (26.1 minutes) from the clinic to reach the RO facility owned by the integrated urology-RO practice versus 5.9 miles (9.2 minutes) to reach the nearest nonintegrated RO facility (P < 0.001).
Conclusions
Integrated urology-RO practices are common in Texas and are generally clustered in urban areas. In the majority of integrated practices, the urology clinics and the integrated RO facility are not at the same location, and driving times and distances from the clinic to the integrated RO facility exceed those from the clinic to the nearest nonintegrated RO facility.
Keywords: Integrated, Urology, Radiation Oncology, Convenience
Introduction
The advent of urologist-owned radiation treatment facilities has become a controversial topic among physicians, economists, and legislators in the United States (1-4). Various arguments have been made for and against the integrated urology–radiation oncology (RO) practice model (5-8). One argument in favor of the integrated practice model is that physical integration of urology and RO services can allow for more efficient care in certain situations, such as the identification and treatment of severe urologic side effects from radiation therapy (2). Another possible advantage of integrated urology-RO practices is that they allow for increased access in medically underserved areas (1). While the news media have reported on integrated urology-RO practices (9, 10), limited data are available in the medical literature regarding this practice model. With the United States Government Accountability Office opening an investigation into this trend because of the potential financial conflict of interest of such practices (4), there is a need to establish accurate data regarding the advent and characteristics of these practices, their prevalence throughout the state, and the extent to which they influence prostate cancer care patterns.
With these goals in mind, we conducted a survey of urology practices in Texas to characterize the emergence of integrated urology-RO practices, their extent of physical integration, and their potential effect on patient travel times for radiation therapy.
Methods and Materials
Using publicly available data from the Texas Medical Board, a database was compiled of all licensed urologists in Texas. A member of our team used this database to identify and call each urology practice with at least four physicians. A scripted survey was used to identify integrated urology-RO practices. Specifically, we asked the following question of each practice’s clinic manager: “Does your clinic offer any radiation treatments within your practice, or do you have to refer to an outside radiation oncology practice?” Data elements collected for the integrated practices included the location of each clinic that offered urologic services, the location of each treatment facility that offered RO services, the number of urologists in the practice, and the year that radiation equipment was acquired.
For this study, an integrated practice was defined as a practice owned by urologists who had invested in a radiation therapy linear accelerator as part of their practice. Academic institutions, Veterans Affairs hospitals, county-funded hospitals and outpatient clinics, large multispecialty practices, and private hospitals were not included.
ArcGIS v9.3 geographic information software (ESRI, Redlands, CA) was used to map each integrated urology-RO clinic location (inclusive of sites that offered urologic services, RO services, or both) and determine the number of Texas residents residing within 10-mile, 20-mile, and 30-mile buffers based on data from the 2000 US census. For comparison, the same analysis was performed using the location of each RO treatment facility in the state of Texas that was not affiliated with a urology group, herein referred to as nonintegrated RO clinic. These nonintegrated RO clinics were identified using information from the Radiological Physics Center, the American Hospital Association, and the Texas Department of Health. This methodology has been described in detail previously (11). Each of these nonintegrated RO clinics has a linear accelerator at the physical address of the clinic.
All of the integrated urology-RO practices had multiple clinic locations offering urologic services but only one clinic location offering RO services. We calculated patient travel time and distance from each integrated urology-RO clinic offering urologic services to the RO treatment facility owned by the integrated urology-RO practice. We also calculated patient travel time and distance from each integrated urology-RO clinic offering urologic services to the nearest nonintegrated RO clinic. The driving time and distance between these sites were calculated using Google Maps 2011 (Google Inc., Mountain View, CA).
Differences between patient driving time and distance to the nearest integrated RO treatment facility and patient driving time and distance to the nearest nonintegrated RO facility were compared using the two-tailed Wilcoxon-Mann-Whitney test in SAS v9.2 (Cary, NC).
This study was reviewed and granted an exempt status by our institution’s Institutional Review Board.
Results
Data from the Texas Medical Board listed 640 licensed urologists in Texas. A total of 229 urology practices in the state were identified, of which 29 had four or more physicians and were contacted by telephone survey. The response rate was 100%. Twelve urology practices (5.2%) were identified that offered integrated RO services, and 182 (28%) of the 640 urologists in Texas worked in such practices. For the 12 integrated urology-RO practices, 108 unique clinic sites offering urologic and/or RO care were identified. Of these sites, only one had an affiliated urology clinic and RO treatment facility at the same physical address.
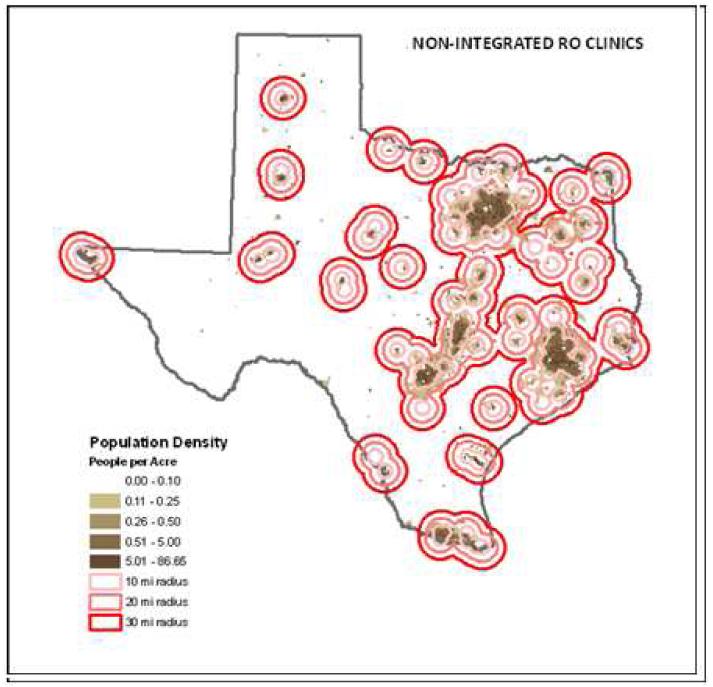
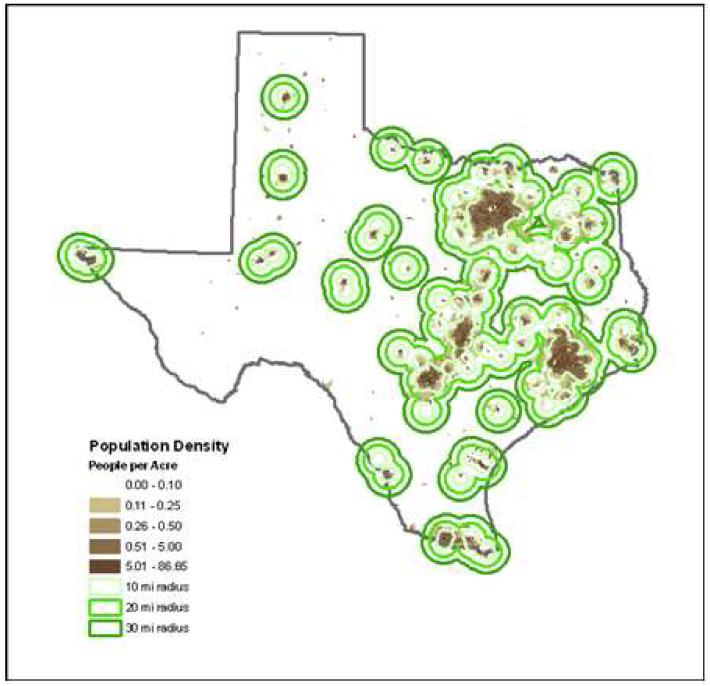
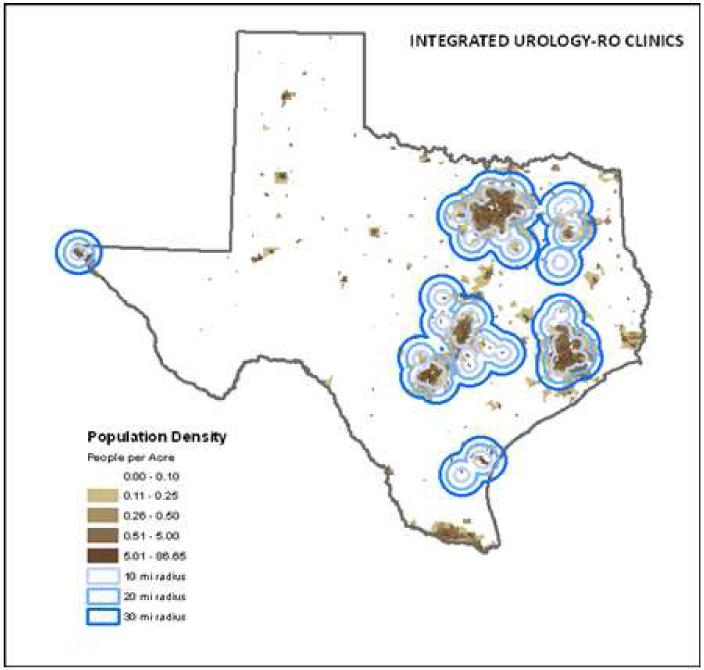
Figures 1-3 show the 10-mile, 20-mile, and 30-mile buffers around nonintegrated RO clinics (n = 290) (Fig. 1); integrated urology-RO clinics (n = 108), which include each urology clinic and their associated radiation therapy site (Fig. 2); and nonintegrated RO and integrated urology-RO clinics combined (n = 398) (Fig. 3) in relation to population density. Individual practice locations are not shown. Approximately 53% of the state population were found to reside within 10 miles of an integrated urology-RO practice. Approximately 71% of the state population were found to reside within 10 miles of a nonintegrated RO clinic (Table 1). The addition of all integrated urology-RO clinic locations increased the percentage of the state population residing within 10 miles of a practice that offers radiation therapy by 2%, from 71% to 73%.
Fig. 1.
Geographic distribution of nonintegrated radiation oncology services. Maps were created using ArcGIS v9.3 software. Colored circles represent 10-mile, 20-mile, and 30-mile buffers around documented locations of radiation oncology treatment facilities that are not integrated with a urology practice. Brown pixels represent population density per the graph legend. Individual practice locations are not shown.
Fig. 3.
Geographic distribution of both integrated and nonintegrated radiation oncology services. When data from Figure 2 are added to the data from Figure 1, the distribution of practices in relation to population density is visually similar to Figure 1, indicating a minimal impact of integrated urology–radiation oncology practices on the spatial distribution of radiation oncology services in the state. The maps were created using ArcGIS v9.3 (ESRI, Redlands, CA). Colored circles represent 10-mi, 20-mi, and 30-mi buffers around documented practice locations. Brown pixels represent population density per the graph legend. Individual practice locations are not shown.
Fig. 2.
Geographic distribution of integrated radiation oncology services. Maps were created using ArcGIS v9.3 (ESRI, Redlands, CA). Colored circles represent 10-mi, 20-mi, and 30-mi buffers around documented locations of clinics and radiation treatment facilities operated by integrated urology–radiation oncology practices. Brown pixels represent population density per the graph legend. Individual practice locations are not shown.
Table 1. Absolute number of individuals and percent of the total state population living within 10, 20, and 30 miles of each practice type.
| Non-integrated radiation oncology clinics |
Integrated urology- radiation oncology clinics |
Integrated and non- integrated clinics combined |
||||
|---|---|---|---|---|---|---|
| Distance | # of individuals |
% of total population |
# of individuals |
% of total population |
# of individuals |
% of total population |
| 10 miles | 18,423,752 | 71.3 | 13,544,805 | 53.9 | 18,423,752 | 73.3 |
| 20 miles | 21,825,653 | 85.5 | 16,537,136 | 65.8 | 21,825,653 | 86.8 |
| 30 miles | 23,239,123 | 91.3 | 18,156,165 | 72.2 | 23,239,123 | 92.4 |
As shown in Table 2, the mean distance for a patient to drive from an integrated urology-RO clinic offering urologic services to the RO treatment facility owned by the integrated practice was 19.7 miles (95% CI, 16.5-22.9 miles) compared with 5.9 miles (95% CI, 3.7-8.1 miles) to the nearest nonintegrated RO clinic (P < 0.001). Similarly, the mean estimated driving time was 26.1 minutes (95% CI, 22.3-29.9 minutes) to the integrated RO treatment facility compared with 9.2 minutes (95% CI, 6.2-12.1 minutes) to the nearest nonintegrated RO clinic (P < 0.001).
Table 2. Time and Distance from integrated urology clinics to radiation oncology services.
| Integrated urology clinic to integrated radiation oncology treatment facility |
Integrated urology clinic to non- integrated radiation oncology treatment facility |
P* | |
|---|---|---|---|
| Mean Distance | 19.70 miles | 5.88 miles | p< 0.001 |
| Mean Time | 26.11 minutes | 9.15 minutes | p< 0.001 |
• - From Wilcoxon rank sum test.
Discussion
Our results indicate that more than half of Texas residents live within 10 miles of an integrated urology-RO practice and more than one quarter of the urologists in the state work in such practices. These findings suggest that urologist-owned radiation therapy facilities are a meaningful contributor to cancer treatment delivery in the state. However, this contribution is limited to densely populated urban areas, as shown in Figures 2 and 3, and does not appear to improve access to radiation therapy for the rural population.
Additionally, our data reveal that in the state of Texas, integrated urology-RO practices may be administratively integrated but usually are not physically integrated, meaning that urology and RO services are rarely offered at the same physical address. The extent to which this lack of physical integration has the potential to mitigate the purported benefits of integrated prostate cancer care models (2,10,11) requires further research. Our data also indicate that patients diagnosed with prostate cancer at an integrated urology clinic would have to drive substantially farther to reach the integrated RO facility than they would to reach the nearest nonintegrated RO clinic. The potential effect of increased patient driving times on the perceived convenience of care merits further study; this is particularly important for a treatment such as radiation therapy for prostate cancer, which often entails more than 8 weeks of daily treatment.
Since the inception of a specific Medicare current procedural terminology code for intensity-modulated radiation therapy (IMRT), the use of this treatment modality has increased substantially. Currently, approximately one in three Medicare beneficiaries with prostate cancer is treated with IMRT (10). IMRT has been reimbursed at three to four times the rate of other treatment options for prostate cancer, including radical prostatectomy, interstitial brachytherapy, and active surveillance.
Additionally, radiation therapy falls under the in-office ancillary services exception of the Stark self-referral law. As a result, at least 37 urology groups nationally have obtained their own linear accelerator and started referring their patients with prostate cancer to their own radiation treatment center (9). Critics of the integrated urology-RO practice model state that it creates financial incentives for urologists to recommend IMRT over other less expensive treatment options, particularly active surveillance (1,2,4,10,12). This financial incentive and its effect on practice patterns and possible overutilization of IMRT are currently being investigated by the US Government Accountability Office as well as a number of state governments (4,9).
However, there are various arguments that support the integrated urology-RO practice model. Proponents state that integrated practices offer patients convenient access to experts in all treatment options for prostate cancer (10). Additionally, though IMRT use has increased with the advent of integrated urology-RO practices, an argument can be made that advances in radiation therapy delivery and treatment have made radiation therapy a more attractive option for most patients with prostate cancer, independent of their seeking care at urologist-owned radiation therapy practices (3).
Texas is a vanguard state in which to examine this phenomenon; since 2004 one of the pioneering companies that helped urology practices acquire radiation services has been headquartered in the state (12). In the intervening years, the number of urologists participating in these integrated clinics has expanded considerably; currently nearly 30% of urologists licensed in Texas are invested in a radiation therapy linear accelerator. Texas and other states in which this type of practice has flourished do not require a certificate of need to open a radiation therapy center. Certificate-of-need laws, which have been adopted in 36 states that we know of, restrict ownership of linear accelerators by requiring state approval before the purchase of equipment or construction of a health care facility (13). As reported by the Government Accountability Office, the presence of these restrictions is associated with a decrease in specialty integrated hospitals (14) and likely has the same effect on the prevalence of integrated clinics.
This study is limited in that only practice arrangements in Texas are considered. It is quite possible that in a state with a smaller geographic area and a higher population density, the difference between the travel times to the nearest integrated RO treatment facility and to the nearest nonintegrated RO clinic would be less. Additionally, the evaluation of rural access in this study is based on qualitative visual inspection of the geographic distribution. Further, although the integrated urology-RO practice structure may offer other unique advantages, such as integration of medical records or unified billing, our study was not designed to quantify these features.
Another limitation of this study is that it was not designed to identify or be applied to more subtle practice arrangements, which can include urologist investment, along with other physicians, in a multispecialty hospital that includes radiation services or in a radiation treatment center that is co-owned by a radiation oncologist. Such arrangements are known to occur, but are often opaque and thus difficult to identify with certainty. Finally, our survey was limited in that only practices with four or more urologists were contacted. Although it is possible that small urology practices may also offer integrated RO services, we cross-checked our survey findings with a complete list of linear accelerators in the state of Texas. After examining each linear accelerator’s record, we did not identify any small urology practices in explicit possession of a linear accelerator.
In summary, this is the first study to evaluate the prevalence and geographical structure of integrated urology-RO practices in Texas. Most of these practices are clustered in urban areas with high population density, and the urology and RO clinics usually are not physically integrated in the same geographical location. Future studies are needed to determine how this new practice model affects prostate cancer care patterns, quality, and patient satisfaction.
Acknowledgement
The authors would like to thank the following individuals for reviewing this manuscript: Laurel R. Hyle, JD, MPH, and Angele T. White, JD, Department of Legal Services, The University of Texas MD Anderson Cancer Center.
Funding: Dr. Smith is supported by a grant from the Cancer Prevention & Research Institute of Texas (RP101207). This work was funded in part by the National Institutes of Health through grant CA010953 and through MD Anderson’s Cancer Center Support Grant, CA016672.
Dr. Smith receives research funding from Varian Medical Systems, but this support was not used for the current project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mitchell JM, Sunshine JH. Consequences of physicians’ ownership of health care facilities—joint ventures in radiation therapy. N Engl J Med. 1992;327(21):1497–1501. doi: 10.1056/NEJM199211193272106. [DOI] [PubMed] [Google Scholar]
- 2.Falit BP, Gross CP, Roberts KB. Integrated prostate cancer centers and over-utilization of IMRT: A close look at fee-for-service medicine in radiation oncology. Int J Radiat Oncol Biol Phys. 2010;76(5):1285–1288. doi: 10.1016/j.ijrobp.2009.10.060. [DOI] [PubMed] [Google Scholar]
- 3.Zimberg SH, Olsson CA. Response to “Integrated prostate cancer centers and overutilization of IMRT: A close look at fee-for-service medicine in radiation oncology.”. Int J Radiat Oncol Biol Phys. 2010;78(5):1607. doi: 10.1016/j.ijrobp.2010.07.1998. Int J Radiat Oncol Biol Phys 2010;78:1285-1288. author reply 1607-1608. [DOI] [PubMed] [Google Scholar]
- 4.Furlow B. US urology clinics overprescribe prostate radiotherapy. Lancet Oncology. 2011;12:122. doi: 10.1016/s1470-2045(11)70022-5. [DOI] [PubMed] [Google Scholar]
- 5.Rickles DJ. Integrated prostate cancer centers and over-utilization of IMRT: In regard to Falit et al. Int J Radiat Oncol Biol Phys. 2011;79(4):1280. doi: 10.1016/j.ijrobp.2010.09.063. Int J Radiat Oncol Biol Phys 2010;76:1285-1288. author reply 1280-12281. [DOI] [PubMed] [Google Scholar]
- 6.Board of Chancellors American College of Radiation Oncology Quality cost of Medicare law: ACRO statement on physician self-referral. Am Coll Radiat Oncol Bull. 2007;14:1–13. [Google Scholar]
- 7.Anscher MS, Anscher BM, Bradley CJ. The negative impact of Stark law exemptions on graduate medical education and health care costs: The example of radiation oncology. Int J Radiat Oncol Biol Phys. 2010;76(5):1289–1294. doi: 10.1016/j.ijrobp.2009.11.061. [DOI] [PubMed] [Google Scholar]
- 8.Olsson CA. Response to “The negative impact of Stark law exemptions on graduate medical education and health care costs: The example of radiation oncology.”. Int J Radiat Oncol Biol Phys. 2010;78(4):1282. doi: 10.1016/j.ijrobp.2010.05.069. Int J Radiat Oncol Biol Phys 2010;76;1289-1294. author reply 1282. [DOI] [PubMed] [Google Scholar]
- 9.Carreyrou J, Tamman M. [Accessed Nov 8, 2011];A device to kill cancer, lift revenue. Wall Street Journal. 2010 Dec 7; Health. http://online.wsj.com/article/SB10001424052748703904804575631222900534954.html. [Google Scholar]
- 10.Stein R. [Accessed November 8, 2011];Doctor-owned centers spark criticism, scrutiny. Washington Post. 2011 Feb 28; http://www.washingtonpost.com/wp-dyn/content/article/2011/02/28/AR2011022805378.html.
- 11.Ballas LK, Elkin EB, Schrag D, et al. Radiation therapy facilities in the United States. Int J Radiat Oncol Biol Phys. 2006;66(4):1204–1211. doi: 10.1016/j.ijrobp.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 12.Saul S. [Accessed November 8, 2011];Sales pitch for a treatment. New York Times. 2006 Dec 1; Business. http://www.nytimes.com/2006/12/01/business/01beamside.html.
- 13.National Conference of State Legislatures [Accessed November 8, 2011];Certificate of need: state health laws and programs. http://www.ncsl.org/IssuesResearch/Health/CONCertificateofNeedStateLaws/tabid/14373/Default. Updated 2009.
- 14.US Government Accountability Office [Accessed November 7, 2011];Specialty hospitals: geographic location, services provided, and financial performance. http://www.gao.gov/new.items/d04167.pdf. Updated 2003.