TO THE EDITOR
Randomized controlled trials show that aerobic exercise training improves glycemic control in type 2 diabetics 1. However, inter-individual variability is large2. This may be explained by genetic variability3, but ambient hyperglycemia4 and pancreatic beta-cell function5 may also contribute. We examined whether changes in glycemic control following a 12-16-week aerobic exercise training intervention were influenced by the pre-training glycemic state in 105 individuals with impaired glucose tolerance or type 2 diabetes.
Methods
Before and following a 12-16 week period of aerobic exercise training, body composition, aerobic fitness (VO2max), and glycemic control (hemoglobin [Hb]A1c, fasting glucose, and oral glucose tolerance test [OGTT]) were determined in a total of 105 older (61±1 years; mean±S.E.M.), overweight/obese (33±1 kg/m2) subjects with impaired glucose tolerance (N=56) or type 2 diabetes (N=49; diagnosed 4.8±0.9 years prior and not insulin-treated). Relationships between pre-intervention variables and intervention-induced changes in variables were assessed by linear and non-linear regression. The study was approved by our institutional review board and subjects provided informed-consent. See eMethods (http://archinte.jamanetwork.com) for full details of the study design.
Results
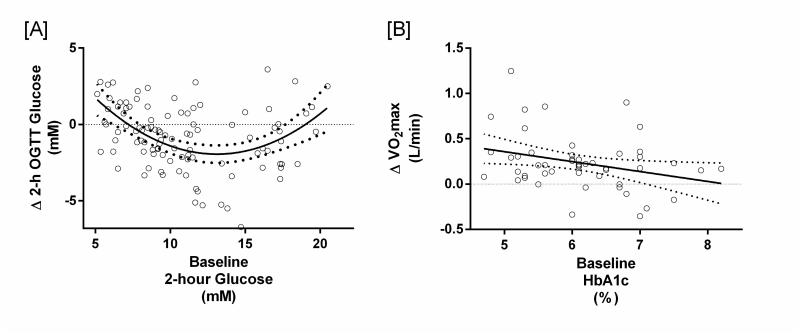
Body weight (−4.6±0.5 kg), whole-body adiposity (−1.9±0.3%), VO2max (+0.23±0.03 L/min), fasting plasma glucose (−0.35±0.08 mmol/L), and 2-hour OGTT glucose (−0.8±0.2 mmol/L) were significantly improved following exercise training (full data is shown in eTable 1). Pre-training fasting plasma glucose did not influence exercise-induced changes in glycemic control. However, there was a non-linear quadratic relationship between pre-training 2-hour OGTT glucose and exercise-induced changes in the 2-hour glucose response (r2=0.26, P=0.06; Fig. A). Subjects with a pre-training 2-hour OGTT glucose of less than 13.1 mM showed greater exercise-induced decreases in 2-hour glucose (r=-0.44, P<0.001); while subjects with a pre-training 2-hour OGTT glucose of greater than 13.1 mM had smaller improvements in 2-hour glucose (r=0.29, P=0.07). The same non-linear quadratic relationship existed between pre-training HbA1c and exercise-induced changes in HbA1c (r2=0.33, P<0.05; Fig. B); where subjects with pre-training HbA1c less than 6.2% had an exercise-induced decrease in HbA1c (r=−0.55, P<0.01), while subjects with pre-training HbA1c greater than 6.2% had smaller exercise-induced improvements in HbA1c (r=0.38, P<0.05). Furthermore, pre-training HbA1c was linearly and inversely related to the exercise-induced change in VO2max, such that high pre-training HbA1c predicted smaller exercise-induced increases in VO2max (r=−0.38, P<0.01; Fig. C).
Fig 1.
Subjects with impaired glucose tolerance or type 2 diabetes underwent 12-16 weeks of moderate-intensity exercise training, 5 d/wk, 60 min/d. Individual subject data points are plotted on both panels; the X-axis represents the pre-training variable and the Y-axis indicates the exercise-induced change such that data points above the axis indicate an exercise-induced increase, and vice versa. Open circles (○) represent impaired glucose tolerant subjects; open triangles (Δ) represent subjects with type 2 diabetes. The solid line represents the regression curve; the dotted line represents the 95% confidence interval. [A] There was a non-linear quadratic relationship between pre-training 2-hour OGTT glucose and the training-induced change in 2-hour OGTT glucose (y=0.06x2−1.5x+7.6; r2=0.26, P=0.06; N=105). For every 1 mM increase in pre-training 2-hour glucose above 13.1 mM (the inflection point of the curve), there was a 0.2 mM loss of improvement in 2-hour glucose following exercise. [B] There was also a non-linear quadratic relationship between pre-training HbA1c and the training-induced change in HbA1c (y=0.31x2−3.8x+11.7; r2=0.33, P<0.05; N=52). For every 1% point increase in pre-training HbA1c above 6.2% (the inflection point of the curve), there was a 0.2% point loss of improvement in HbA1c following exercise. [C] An inverse linear relationship between pre-training HbA1c and the training-induced change in aerobic fitness was found (y=−0.11x+0.91; r=−0.38, P=0.006; N=52). For every 1% increase in pre-training HbA1c, there was 0.11 L/min loss of improvement in VO2max following exercise training.
COMMENT
These findings emphasize that exercise-induced improvements in glycemic control are dependent on the pre-training glycemic level. We demonstrate that although moderate-intensity aerobic exercise can improve glycemic control, individuals with ambient hyperglycemia are the most likely to be non-responders. Our key observation is that pre-training hyperglycemia predicts exercise-induced improvements in glycemic control: for every 1 mM rise in pre-training 2-hour OGTT glucose above 13.1 mM (the curve inflection point in Fig. A) we predict a 0.2 mM loss of improvement in 2-hour OGTT glucose following exercise. Accordingly, for every 1% point increase in pre-training HbA1c above 6.2% (the curve inflection point in Fig. B), we predict a 0.2% point loss of improvement in HbA1c following exercise. Pre-training hyperglycemia also predicted the exercise-induced increment in aerobic fitness: for a 1% increase in pre-training HbA1c we predict a 0.11 L/min loss of improvement in VO2max following exercise.
Prior work shows that diabetes remission following exercise and diet intervention is more likely in individuals with a shorter disease history and lower HbA1c6. Here we show that aerobic exercise-induced improvements in glycemic control are blunted by ambient hyperglycemia, particularly in subjects with type 2 diabetes. Mechanistic studies are required to help us understand this phenomenon, but underlying impairments in beta-cell function are likely to be very important5. That hyperglycemia blunted the cardiovascular adaptations to exercise (VO2max) is in agreement with some prior reports7 and may be explained by the causal association between chronic hyperglycemia and micro- and macrovascular dysfunction8.
The clinical relevance of these new findings is paramount as they highlight the need to understand the metabolic “non-responder”. Because chronic hyperglycemia (>6.2% HbA1c; >13.1 mM glucose) potentially predicts a poor therapeutic effect of aerobic exercise upon glycemic control and fitness, using exercise to treat patients with poorly-controlled type 2 diabetes may have limited chances of a successful outcome.
ACKNOWLEDGEMENTS
We thank Lisbeth Andreasen (Rigshospitalet, Denmark) for assistance with biochemical analyses and Julianne Filion (Cleveland Clinic, USA) for her assistance with subject recruitment and patient screening. We also thank Marc Cook (Cleveland Clinic, USA), Thomas Grøndahl (Rigshospitalet, Denmark), and Kamilla Winding (Rigshospitalet, Denmark) for their help with exercise training.
FUNDING
The study was funded by a Paul Langerhans program grant from the European Foundation for the Study of Diabetes (TPJS), and supported by the National Institute of Health (NIH grant RO1 AG12834, JPK) and CTSA (UL1 RR024989). SKM was supported by NIH grant T32 DK007319. The funding sources played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Conflict of interest statement: There are no conflicts of interest.
REFERENCES
- 1.Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2010;304:2253–2262. doi: 10.1001/jama.2010.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boule NG, Weisnagel SJ, Lakka TA, et al. Effects of exercise training on glucose homeostasis: the HERITAGE Family Study. Diabetes Care. 2005;28:108–114. doi: 10.2337/diacare.28.1.108. [DOI] [PubMed] [Google Scholar]
- 3.Ruchat SM, Rankinen T, Weisnagel SJ, et al. Improvements in glucose homeostasis in response to regular exercise are influenced by the PPARG Pro12Ala variant: results from the HERITAGE Family Study. Diabetologia. 2010;53:679–689. doi: 10.1007/s00125-009-1630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malin SK, Kirwan JP. Fasting hyperglycaemia blunts the reversal of impaired glucose tolerance after exercise training in obese older adults. Diabetes Obes Metab. 2012;14:835–841. doi: 10.1111/j.1463-1326.2012.01608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dela F, von Linstow ME, Mikines KJ, Galbo H. Physical training may enhance beta-cell function in type 2 diabetes. Am J Physiol Endocrinol Metab. 2004;287:E1024–E1031. doi: 10.1152/ajpendo.00056.2004. [DOI] [PubMed] [Google Scholar]
- 6.Gregg EW, Chen H, Wagenknecht LE, et al. Association of an Intensive Lifestyle Intervention With Remission of Type 2 Diabetes. JAMA. 2012;308:2489–2496. doi: 10.1001/jama.2012.67929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burns N, Finucane FM, Hatunic M, et al. Early-onset type 2 diabetes in obese white subjects is characterised by a marked defect in beta cell insulin secretion, severe insulin resistance and a lack of response to aerobic exercise training. Diabetologia. 2007;50:1500–1508. doi: 10.1007/s00125-007-0655-7. [DOI] [PubMed] [Google Scholar]
- 8.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]