Abstract
Stromal cell-derived factor-1α (SDF-1α) mediated mobilization and homing of stem cells showed promising potential in stem cell based tissue engineering and regenerative medicine. However local and sustained release of SDF-1α is indispensable for stem cell mediated regenerative process due to its short half-life under inflammatory conditions. In this study, a gene activated collagen substrate (GAC) was formed via assembly of plasmid encoding SDF-1α into a collagen substrate to create a microenvironment favoring stem cell homing. Local release of SDF-1α from the transfected cells on GAC and its effect on CD117+ stem cell homing were investigated. Non-viral poly-ethyleneimine (25kDa PEI)/DNA complexes were mixed with rat tail collagen solution to form the GAC. Optimization of GAC was carried out based on collagen effects on the PEI/DNA complexes, viability and luciferase expression of COS7 cells on GAC. CD117+ stem cells homing in response to SDF-1α local expression from transfected cells on GAC were investigated in a flow chamber in vitro and in a mouse hind limb model in vivo. The gene expression, migration of CD117+ stem cells and the induced inflammation were investigated with immunostaining, reverse transcription polymerase chain reaction (RT-PCR) and H&E staining. The optimized parameters for GAC were DNA dosage 10 μg/cm2, molar ratio of PEI nitrogen in primary amine to DNA phosphate (N/P ratio) 4 and mass ratio of collagen to DNA (C/D ratio) 1.0. It kept cell viability above 75% and transfection efficiency around 5.8 × 105 RLU/mg protein. GAC allowed the sustained gene release up to 60 days. GAC mediated SDF-1α gene release induced migration and homing of CD117+ stem cells in vitro and in vivo significantly, and the inflammation of GAC reduced significantly two weeks after transplantation. GAC is a promising stem cell based therapeutic strategy for regenerative medicine.
Keywords: collagen, gene activated substrate, localized gene delivery, stem cells migration
Introduction
Stem cell therapy is a promising approach to treat degenerative disease, which provides therapeutic options to replace or repair damaged tissues or organs [1, 2]. However, transplantation of stem cells directly to the arduous microenvironment of the injured organ incurred from ischaemia, inflammatory response and pro-apoptotic factors may comprise the attempt to achieve the optimal therapeutic efficacy [3, 4]. Whereas various tissue intrinsic stem cells are capable of maintaining, generating, and replacing terminally differentiated cells within their own specific tissue as a consequence of physiologic cell turnover or tissue damage because of injury [5, 6], the limited tissue intrinsic stem cell pools are clearly not sufficient to mediate tissue repair and regeneration [7]. Hence, local delivery of chemotactic factors to recruit the circulating stem cell population from other tissues represents a promising new therapeutic approach to tissue regeneration [8].
SDF-1α is widely recognized as a pivotal chemokine to direct stem cell recruitment into damaged organs [9, 10]. Numerous studies in animals have documented that SDF-1α-mediated stem cells homing following tissue injury is associated with a tissue repair and functional improvements [11–17]. However, SDF-1α has very short half-life (<15 min.). It could be inactivated and cleaved by both matrix metalloproteinase-2 (MMP-2) and CD26/dipeptidyl peptidase IV, which are two abundant proteases under inflammatory conditions [18–20]. Thus, precisely controlled and sustained delivery of SDF-1α may be crucial for driving stem cells homing to the injured site and enhancing tissue regeneration.
Gene activated matrix allows local and sustained release of plasmid DNA to the desired site. It has been used effectively in a variety of applications, including regeneration of injured bone, blood vessel and heart tissue [21–24]. It offers an effective platform of controlled and prolonged chemotactic factors release to enhance the beneficial efficacy of homing circulating stem cell population to the injured site for tissue regeneration.
In the present study, we formed a gene-activated collagen substrate (GAC) via assembly of plasmid encoding SDF-1α into a biocompatible and biodegradable collagen substrate to create a microenvironment favouring stem cell homing. The SDF-1α was sustainably expressed in situ by the adhesive cells on the GAC. The sustained SDF-1α release from the transfected cells promoted CD117+ stem cells tethering and homing both in a flow chamber and after implantation into mouse hindlimb.
Materials and methods
All used animals received humane care and animal experiments conformed to the ‘guide for the care and use of laboratory animals’ published by the U.S. National Institutes of Health (NIH Publication No. 85-23, revised 1996).
Chemicals and reagents
Branched polyethyleneimine (PEI) with average molecular weight (MW) of 25 kDa, MTT (3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) and Ethidium bromide (EB) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Dimethyl sulfoxide (DMSO) with high purity (≥99.5%) was purchased from ROTH (Roth Chemical, Karlsruhe, Germany). Rat tail collagen was purchased from Millipore (Billerica, MA, USA). All chemicals and reagents were used directly without further purifications.
Amplification and purification of plasmid DNA
Plasmid pRE-Luciferase (pREP4-Luc) and pcDNA3.1-LacZ (Invitrogen, Carlsbad, CA, USA) were used as received without further modification. Plasmid (pEGFP-N3-SDF-1α) was cloned by our laboratory by encoding SDF-1α gene into pEGFP-N3 vector (Clonetech, Palo Alto, CA, USA). The co-expression of EGFP and SDF-1α has been confirmed in our previous work [25]. Thus, EGFP can be regarded as a marker gene of SDF-1α.
All plasmids were transformed in Escherichia coli DH5α strain and amplified in LB medium at 37°C for overnight at 200 rpm. The amplified plasmid DNA was purified by plasmid DNA purification kit (Macherey-Nagel, Diiren, Germany). The purified plasmid DNA was dissolved in Tris–EDTA (TE) buffer and condensed in a lyophilizer (BETA 1-16, Christ, Osterode, Germany).
The concentration and purity of plasmids were determined by ultraviolet (UV) absorbance at 260 and 280 nm with a spectrophotometer (Thermo Electron, Waltham, MA, USA). Finally, the purified plasmid DNA was resuspended in TE buffer and stored in aliquots at a concentration of 2 or 4 mg/ml and stored at −20°C prior to use.
Preparation and characterization of GAC
The PEI/DNA complex was prepared according to Li et al. [26]. Briefly, plasmid DNA was diluted to the chosen concentration (usually less than 0.5 mg/ml) with 5% glucose. Then, PEI with appropriate concentration (usually less than 3.75 mM primary amine), in 5% glucose solution, was added drop-wise into DNA solution and the mixture was vortexed immediately for 30 sec. and incubated at room temperature for 30 min. N/P ratio was calculated by taking into account that 1 μg DNA contains 3 nmol of phosphate and that 43 ng PEI (1 nmol of C2H5N repeat units) holds 0.25 nmol of primary amine nitrogen. To prepare the GAC complex, the PEI/DNA complex solution was mixed with collagen water solution (usually less than 1 mg/ml), vortexed 30 sec. and incubated at room temperature for another 30 min. The collagen/DNA mass ratio was presented as C/D ratio.
The retardation of DNA by PEI and collagen were studied, respectively, by gel electrophoresis. PEI/DNA or collagen/DNA mixtures were prepared, mixed with loading buffer and loaded onto an ethidium bromide containing gel (1% agarose). Electrophoretic mobility of the samples was measured at room temperature in TBE buffer at 100 V. The DNA bands were visualized using an UV illuminator (Gel Doc 2000 system, Bio-Rad, Hercules, CA, USA).
GAC complex size was measured with a N4 Plus Submicron Particle Sizer (Beckman Coulter, Fullerton, CA, USA) at 20°C. GAC complex solution was diluted with 5% glucose to the final DNA concentration of 0.025 mg/ml for measurement. The scattering light was detected at 90° angle, running time 200 sec. and the data were analyzed with the Unimodal Analysis mode. The refractive index medium (1.332) of 5% glucose at 20°C was used for data analysis.
The time-dependent release speed of PEI/DNA complex from collagen substrate was investigated according to the method similar to Guo et al. [27]. Briefly, GAC (PEI/pcDNA3.1-LacZ/collagen, N/P ratio = 4, C/D ratio = 1) complexes were added into 24-well cell culture plate at the final DNA dose of 100 μg/well. The aqueous solvent was evaporated by air-drying at room temperature under a sterile condition. Then, 600 μl 1 × PBS was added into each well and the plate was incubated at 37°C. At the specific time points, 300 μl supernatant of each sample was removed and replaced with 300 μl fresh 1 × PBS was added. The complex concentration in the supernatant was measured by mixing with ethidium bromide. In brief, 100 μl released PEI/DNA complexes were mixed with 50 μl 1 × PBS and 100 μl ethidium bromide (0.02 mg/ml). The mixtures were visualized under the UV illuminator and the intensities of the emitted fluorescence were analyzed with Quantity One 1-D Analysis Software (Bio-Rad). A standard curve was made by a series of PEI/DNA complexes (N/P ratio = 4) with known concentration. The amounts of released PEI/DNA complexes were quantified via the standard curve.
MTT cytotoxicity
The kidney fibroblast (African green monkey) cell line, COS7 (ATCC) was cultured in Dulbecco’s minimum essential medium (DMEM) supplemented with 10% foetal bovine serum (FBS) and the antibiotics streptomycin (100 μg/ml) and penicillin G (100 IU/ml). The cells were grown at 37°C in a humidified atmosphere of air and 5% CO2. GAC (PEI/pREP4-Luc/collagen) complex solution was coated into a 96-well plate by air-drying at room temperature under sterile condition for 96 hrs. Then, COS7 cells were seeded into the coated plates with the density of 1.2 × 104 cells/well. Collagen free group was used as control. The cells were seeded at 1.2 × 104 cells/well and the PEI/DNA complex solution was added immediately after seeding to make the cells have the same complexes-treated time as that in GAC group. After 40 hrs of incubation at 37°C, 15 μl MTT (5 mg/ml in 1χPBS) was added into each well. And after another 4 hrs of incubation at 37°C, the medium was removed and the purple crystals were dissolved in 100 μl dimethylsulfoxide (DMSO). Absorbance was measured at a wavelength of 550 nm and a reference wavelength of 655 nm using a microplate reader (Model 680, Bio-Rad). The results were expressed as the percentage of viability with respect to the control cells, which were cultured without complexes treatment. Cell viability was calculated using the equation below:
In vitro transfection
The in vitro transfection with GAC was optimized using COS7 cell line. GAC (PEI/pREP4-Luc/collagen) complex solution was coated into 48-well plates by air-drying at room temperature under sterile condition for 96 hrs. The cells were seeded at the density of 0.4 × 105 cells/well. In addition, collagen substrate free group was also investigated as comparison. COS7 cells were pre-seeded into 48-well plate at the density of 0.2 × 105 cells/well. After 24 hrs of culture, the PEI/DNA complexes were added into the cell culture medium directly. After 60 hrs of transfection the culture medium was removed. The cells were washed twice by 1 × PBS and permeabilized by 100 μl cell lysis buffer (Promega, Madison, WI, USA). The luciferase activity in cell extracts was measured using a luciferase assay kit (Bright-Glo, Promega) on a 96-well microplate luminometer (MicroLumatPlus LB 96V, EG&G Berthold, Bad Wildbad, Germany) for 5 sec. The relative light units (RLU) were normalized against protein concentration in the cell extracts, which was measured using a protein assay kit with microplate reader (Model 680, Bio-Rad).
Based on the optimized parameters the EGFP expression was investigated for confirmation. GAC (PEI/pEGFP-N3-SDF-1α/collagen) was prepared with the optimized N/P ratio and C/D ratio. The GAC was coated into cell culture dish. In brief, one drop of solution was dropped onto the pre-designed coated area in dish bottom and aspirated with pipette after 5 min. of incubation at room temperature. After another 5 min., the procedure was repeated for additional four times with ‘dropping-5 min. of incubation-aspirating-5 min. of drying’. After coating COS7 cells were seeded with the density of 2.0 × 104 cells/cm2. After 24 hrs, the cells were observed under fluorescence microscope (Axiovert40 CFL, Carl Zeiss, Goettingen, Germany).
Localized transfection mediated by GAC was tested with pcDNA3.1-LacZ and pEGFP-N3-SDF-1α gene, respectively. GAC (PEI/pcDNA3.1-LacZ/collagen, N/P = 4, C/D = 1) was patterned into a well of 6-well plate with the pre-designed pattern (three dots with each containing 1.0 μg DNA). After drying, COS7 cells were seeded into the well with the density of 2.4 × 105 cells/well. After 48 hrs, the transfection was evaluated by X-gal staining [26]. For pEGFP-N3-SDF-1α gene, GAC complexes (PEI/pEGFP-N3-SDF-1α/collagen, N/P = 4, C/D = 1) were pre-coated on a glass coverslip with the DNA dosage of 10 μg/cm2. After drying of the GAC, the coverslip was put into a 6-well plate and COS7 cells were seeded with the density of 2.1 × 105 cells/well. After 48 hrs, the transfection was evaluated under fluorescence microscope (Axiovert40 CFL, Carl Zeiss).
CD117+ stem cells isolation and co-culture
Mice (C57BL/6N/Crl, Charles River, Germany) were sacrificed and the femurs were cleaned by carefully removing the tissue. Then, CD117+ cells were isolated by mouse CD117 microbeads (Miltenyi Biotec, Gladbach, Germany) following the given protocol. The purity of the CD117+ cells was evaluated with fluorescence-activated cell sorting machine (FACS, Becton Dickinson, Heidelberg, Germany). Briefly, the cells were labelled with mouse CD117 PE (Miltenyi Biotec) and suspended in 1 × PBS. Then the cells were analyzed with FACS and unlabeled cells were used as control. For each running, 1.0 × 104 cells were counted. Only the cells having the purity of more than 90% were used.
To characterize the effect of CD117+ stem cells homing in response to SDF-1α, the statistic analysis was carried out with a flow chamber (Fig. 6A). The flow chamber was employed to simulate the in vivo circulating environment and designed to eliminate the influence of gravity on the cells homing. It was composed of a tubing pump (REGLO Digital MS-2/8, ISMATEC SA, Glattbrugg, Switzerland), a silicone tubing (Inner diameter 0.89 mm, ISMATEC SA, Glattbrugg, Switzerland) and a cylindrical plastic chamber (Inner diameter 26.5 mm). GAC (PEI/pEGFP-N3-SDF-1α/collagen, N/P = 4, C/D = 1) was coated onto a glass slide. As a control, GAC (PEI/pEGFP-N3/collagen, N/P = 4, C/D = 1) was coated onto the same slide side by side. After drying of the GAC, the slide was put flatwise into a 100-mm tissue culture dish, and COS7 cells were added into the dish with the total number of 7.0 × 105 cells. After 24 hrs for cells attachment and transfection, the slide was vertically fixed in the flow chamber which was filled with cells culture medium (50 ml DMEM with antibiotics, 10% FBS and 10 mM HEPES). 3.52 × 106 CD117+ cells labelled with CellTracker Probe-Red CMTPX (Invitrogen) were added into the flow chamber. The flowing rate of the medium was set as 2 ml/min. After 36 hrs of circulation, the slide was taken out and observed with fluorescence microscopy (Leica, Wetzlar, Germany). For each GAC-coated area, more than 20 eyeshots with more than 4000 COS7 cells were photographed. The numbers of COS7 cells and CD117+ cells on the photographs were counted for statistic analysis.
Fig 6.
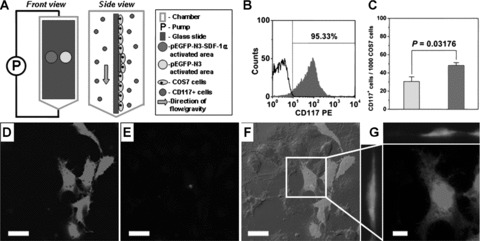
In vitro statistic analysis of migration and homing of CD117+ cells. (A) Flow chamber employed to simulate the circulating environment. (B) Representative FACS histogram of CD117+ cells purity assay. (C) The number of CD117+ cells on the GAC-coated area normalized by the number of COS7 cells. (D) EGFP expression of COS7 cells cultured on the GAC (PEI/pEGFP-N3-SDF-1α/collagen)-coated area, (E) a CD117+ cell labelled with CellTracker Probe-Red CMTPX. (F) Merged picture of fluorescence and phase-contrast microscopic picture and (G) enlarged 3D-picture that indicates a homed CD117+ cell on a transfected COS7 cell. (Bars in D–F = 30 μm; Bar in G = 10 μm).
In vivo transfection
The GAC solutions ((PEI/pEGFP-N3-SDF-1α/collagen, N/P = 4, C/D = 1) and (PEI/pEGFP-N3/collagen, N/P = 4, C/D = 1)) were prepared as before. The mixed cellulose ester membrane (Whatman, Maidstone, Kent, UK) was cut to small pieces (3 mm × 4 mm) and sterilized before use. The GAC solutions were concentrated under vacuum pressure and coated onto the membrane subsequently by layer-by-layer method. The final DNA dosage was 40 μg/piece of membrane. Operations were performed on mice (C57BL/6N/Crl, Charles River, Sulzfeld, Germany) by transplanting the membranes into quadriceps. Mice were anaesthetized by intraperitoneal injection with avertin and shaved to facilitate the incision. The area was swabbed with 70% ethanol. Then, incisions were made with scissors, and pockets adjacent to the incision site were created with the aid of scissors and forceps. The mixed cellulose ester membrane pieces were transplanted into the pockets. The incisions were closed and the mice were put back to the cages. After 3, 7 and 14 days, the mice were sacrificed. The quadriceps were excised and frozen in O.C.T tissue blocking compound (Sakura Finetek Europe B.V., Zoeterwoude, The Netherlands) in liquid nitrogen. To evaluate the gene expression, the cryosections of the frozen tissue were incubated with rabbit polyclonal anti-EGFP and goat polyclonal anti-SDF-1α (Santa Cruz Biotechnology, Santa Cruz, CA, USA) overnight, then stained with second antibodies: Alexa fluor 488 donkey anti-rabbit and Alexa fluor 568 donkey anti-goat (Invitrogen).
RT-PCR
To evaluate the expression of CD117, reverse transcription PCR (RT-PCR) was performed using a mouse specific primer. Briefly, muscle samples around the membranes were snap-frozen in liquid nitrogen and powdered. Totoal mRNA was extracted with RNeasy Fibrous Tissue Kit (Qiagen, Hilden, Germany). For reverse transcription of total mRNA and first-strand synthesis of cDNA, SuperScriptTM III Reverse Transcriptase (Invitrogen) and oligo (dT)15 Primer (Promega) were applied. Specific (mouse CD117) and house-keeping (GAPDH) cDNA sequences were amplified via PCR with GoTaq Green Master Mix (Promega), specific oligonucleotide primers (0.8 μM) and house-keeping oligonucleotide primers (0.02 μM) in a DNA Engine Cycler (PTC-0200, Bio-Rad). Employed specific primer sets were designed with DNASTAR PrimerSelect Software (Lasergene) and were as follows: 5′-CAC- GCG-CCT-GCC-GAA-ATG-TA-3′ upper primer and 5′-CTG-CTG-CCC-ACC-GAG-TTG-ACC-3′ lower primer. PCR cycles were set as 30, which has been proved by pre-test that it would not induce the saturated amplification. The cycle conditions were: initial denaturation (95°C for 2 min.), denaturation (95°C for 1 min.), annealing (58.8°C for 1 min.), extension (72°C for 1 min.), and one final extension cycle (72°C for 5 min.). Then amplified gene fragments were separated in 2% agarose gel and photographed under UV illumination using Gel Doc XR system (Bio-Rad). The quantitative analyses were performed by Quantity One 1-D Analysis Software (Bio-Rad).
Histological staining
Identification of the CD117+ cells was made by immunostaining the cryosections. The sections were washed and fixed with 1% PFA. Then, the sections were washed again and treated with DakoCytomation protein block (Dako, Glostrup, Denmark). After incubated with primary antibody-rabbit polyclonal anti-c-kit (Santa Cruz Biotechnology) overnight, the cryosections were incubated with Alexa fluor 488 donkey anti-rabbit (Invitrogen) for 2 hrs at room temperature. For nuclei staining, TOPRO-3 (Invitrogen) was used for a 20 min. of incubation at room temperature. The stained sections were observed with laser confocol microscope (TCS SP2, Leica).
The inflammatory response to the transplantation of GAC was examined by H&E staining. Tissue samples excised after days 3, 7 and 14 were frozen in O.C.T. tissue blocking compound. Then, cryosections were cut, fixed with 4% formalin and stained with hematoxylin and eosin (H&E) according to the standard histological protocol.
Statistical analysis
Statistical analysis was performed with one-way analyses of variance (ANOVA). Results were expressed as average ± standard deviation. A P-value < 0.05 was considered to be statistically significant.
Results
Characterization of GAC
Besides plasmid DNA, GAC is composed of PEI and collagen. To investigate whether collagen affects the DNA condensing abilities of PEI, DNA condensing abilities of PEI and collagen were studied by gel retardation assay. Electrophoretic mobility of DNA after being condensed by PEI and collagen are shown in Fig. 1A and B. Both of PEI and collagen can retard DNA motility. And the retardation ability increased with the PEI or collagen amount. At PEI/DNA ratio (N/P ratio) 1 and collagen/DNA mass ratio (C/D ratio) 6, the DNA was retarded completely. Hence we select C/D ratio 1 as the optimal ratio for GAC assembly to reduce the effect of collagen on condensing ability of PEI.
Fig 1.
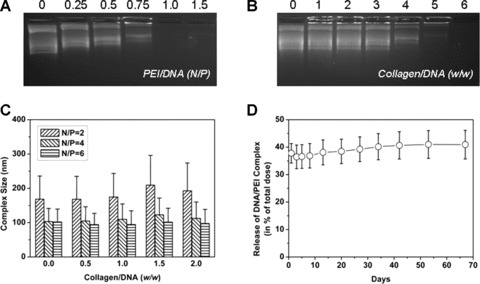
Characterization of GAC. Plasmid DNA (pREP4-Luc) retardation by (A) PEI at various N/P ratios and (B) collagen at various C/D ratios. (C) GAC (PEI/pEGFP-N3-SDF-1α/collagen) complexes size influenced by N/P and C/D ratios. (D) Released speed of PEI/DNA (pcDNA3.1-LacZ) complex from collagen substrate. The results were expressed as average ± standard deviation (N= 6).
The effect of collagen on the complexes size of PEI/DNA is shown in Fig. 1C. There were no apparent effects of collagen on the size of PEI/DNA complexes under N/P ratios ranging from 2 to 6.
PEI/DNA complex release speed from the GAC, one crucial property of the substrate, was investigated and the result is shown in Fig. 1D. On the first day, about 37% of complexes were released from GAC. After that, the release speed slowed down and sustained release up to 2 months was observed. The cumulative amount of released complexes after 67 days was approximately 41%.
Cytotoxicity and in vitro transfection
The optimization of GAC was carried out by measuring the cytotoxicity and transfeciton efficiency at different N/P ratios ranging from 1 to 12 and DNA dosages ranging from 2.5 to 15.0 μg/cm2. The collagen free group was used to evaluate the effect of collagen substrate. For GAC group, both of the cell viability and transfection efficiency were statistically analyzed.
MTT analysis results (Fig. 2) showed that the cell viability cultured on the GAC was significantly improved or comparable to the cells from the collagen free group at N/P ratios ranging from 2 to 12 and DNA dosages ranging from 2.5 to 15.0 μg/cm2; whereas the transfection efficiency of the GAC (Fig. 3) was comparable to PEI/DNA complexes in the collagen free group at all investigated N/P ratios and DNA dosages ranging from 5.0 to 15.0 μg/cm2. The optimal parameters of GACs corresponding to the highest cell viability and transfection efficiency were 7.5 μgDNA/cm2, N/P = 2 and 10.0 μgDNA/cm2, N/P = 4, respectively. Considering both of the cell viability and transfection efficiency, we selected the N/P ratio of 4 and DNA dosage of 10 μg DNA/cm2 as the optimal parameters for GAC which kept cell viability above 75% and transfection efficiency around 5.8 × 105 RLU/mg protein.
Fig 2.
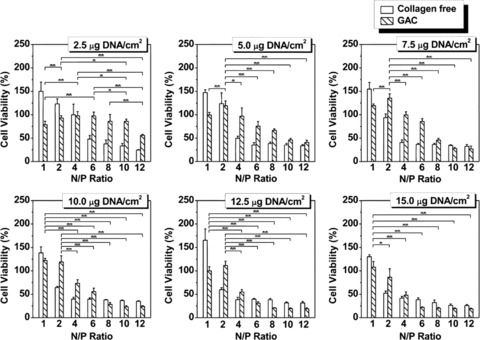
Cytotoxicity of PEI/DNA complexes at the absence (collagen free) and presence of collagen (GAC). N/P ratios and DNA dosages (expressed as DNA amount in unit area (μg/cm2)) were varied. Collagen dosage was constant (10 μg/cm2). The result was given as average ± standard deviation (N= 6). One way-ANOVA analysis was carried out to determine the optimal parameters corresponding to the highest cell viability for GAC group (*P < 0.05, **P < 0.01). Cells growing on GAC (7.5 μgDNA/cm2, N/P= 2) have the highest viability comparing with cells on other GACs (P < 0.05).
Fig 3.
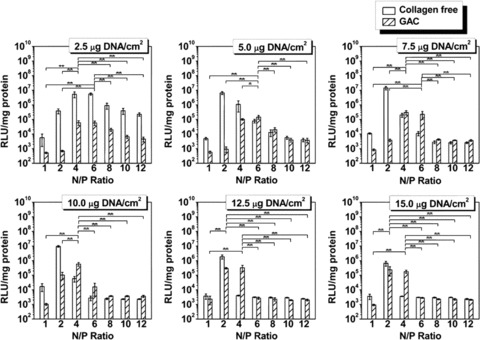
Luciferase expression of COS7 cells transfected by PEI/DNA (pREP4-Luc) complexes at the absence (collagen free) and presence of collagen (GAC). N/P ratios and DNA dosages (expressed as DNA amount in unit area (μg/cm2)) were varied. Collagen dosage was constant (10 μg/cm2). The result was given as average ± standard deviation (N= 6). One way-ANOVA analysis was carried out to determine the optimal parameters corresponding to the highest transfection efficiency for GAC group (*P < 0.05, **P < 0.01). Cells growing on GAC (10.0 μgDNA/cm2, N/P= 4) have the highest transfection efficiency comparing with cells on other GACs (P < 0.05).
The transfection was further confirmed by seeding COS7 cells on GAC (PEI/pEGFP-N3-SDF-1α/collagen, N/P = 4, C/D = 1) assembled with above optimized parameters (Fig. 4), suggesting the GAC could efficiently deliver genes into the cells cultured on it.
Fig 4.

EGFP expression of COS7 cells transfected by GAC (PEI/pEGFP-N3-SDF-1α/collagen) assembled with optimized parameters (DNA dosage 10 μg/cm2, N/P ratio 4 and C/D ratio 1). (A) Cells expressing EGFP, (B) phase contrast image of cells, (C) merged image. (Bar = 100 μm).
Localized gene delivery is an expected property of gene-activated substrate. Localized gene delivery from GAC was evaluated by (PEI/pcDNA3.1-LacZ/collagen)-GAC and (PEI/pEGFP-N3-SDF-1α/collagen)-GAC, respectively. As shown in Fig. 5, the transfected cells were confined to the GAC-coated area. The expression of reporter genes, LacZ and EGFP, was detected and formed a clear border between the transfected and untransfected cells as indicated by dotted lines in Fig. 5B and E.
Fig 5.
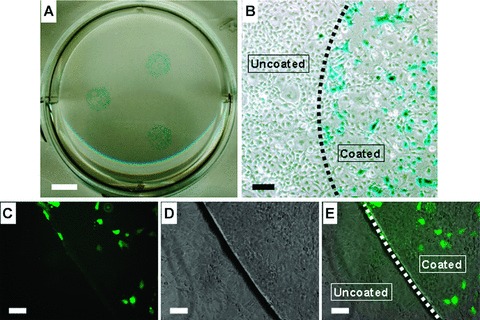
Localized gene delivery mediated by GAC. X-gal staining of pcDNA3.1-LacZ transfected COS7 cells appeared blue in (A) complete view and (B) enlarged view. Transfected COS7 cells locally expressed EGFP in designed areas. (C) Fluorescence microscopic picture, (D) phase-contrast microscopic picture and (E) merged picture. The dotted lines indicate the border of the GAC-coated and uncoated areas. (Bar in A = 5 mm; Bars in B–E = 100 μm).
In vitro CD117+ stem cells migration and homing
To investigate the attraction of (PEI/pEGFP-N3-SDF-1α/collagen)-GAC on CD117+ cells, COS7 cells were seeded on a (PEI/pEGFP-N3-SDF-1α/collagen)-GAC and (PEI/pEGFP-N3/collagen)-GAC-coated glass slide and put in a flow chamber (Fig. 6A). CD117+ cells isolated from mice with purity ≥90% (Fig. 6B) were circulating in the flow chamber. After 36 hrs of circulation, the number of CD117+ cells mobilized and homed onto the (PEI/pEGFP-N3-SDF-1α/collagen)-GAC was significantly higher (1.6 fold) than that onto (PEI/pEGFP-N3/collagen)-GAC area (Fig. 6C). Figure 6D, E, F and G showed the confocol microscopic images of a CD117+ cell attached on a transfected COS7 cell. Interestingly, some homed CD117+ cells were infused with COS7 cells although in an extremely low frequency.
In vivo experiment
The in vivo co-expression of EGFP and SDF-1α was evaluated 3 days after transplantation of the (PEI/pEGFP-N3-SDF-1α/collagen)-GAC-coated membrane by triple-immunostaining of EGFP, SDF-1α and nuclei of the cryosections. Figure 7 showed co-expression of both EGFP and SDF-1α. No expression of EGFP or SDF-1α, was found in control group transplanted with naked membranes.
Fig 7.
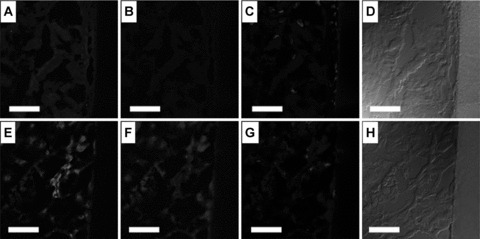
In vivo co-expression of EGFP and SDF-1α induced by GAC (PEI/pEGFP-N3-SDF-1α/collagen) was evaluated by triple staining of EGFP, SDF-1α and nuclei. The GAC was pre-coated on mixed cellulose ester membrane, and then transplanted into the quadriceps of mice. The cryosections were evaluated after 3 days of transplantation (E, F, G, H) by comparing with a negative control which was transplanted with a naked membrane (A, B, C, D). Fluorescence microscopic pictures of (A, E) EGFP staining, (B, F) SDF-1α staining and (C, G) nuclei staining and phase-contrast microscopic pictures (D, H). (Bar = 100 μm).
RT-PCR result showed that CD117 was up-regulated in the tissue transplanted with (PEI/pEGFP-N3-SDF-1α/collagen)-GAC-coated membrane (Fig. 8A and B). Comparing with the group transplanted with (PEI/pEGFP-N3/collagen)-GAC-coated mem branes, CD117 expression showed statistically significant enhancement in the group transplanted with (PEI/pEGFP-N3-SDF-1α/collagen)-GAC-coated membranes.
Fig 8.
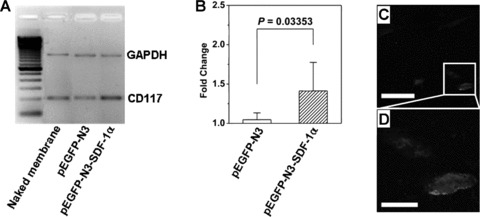
The in vivo up-regulation of CD117 expression induced by GAC was evaluated by RT-PCR. The group transplanted with naked membrane was used as control group. The result was expressed as the fold change over the average value of the control group, which was set as 1. (A) Representative bands visualized under UV illuminator. (B) CD117 mRNA levels were given with respect to control group (naked membrane, N= 6) and expressed as average ± standard deviation (pEGFP-N3 group: N= 6; pEGFP-N3-SDF-1α group: N= 8). The CD117+ cells were identified by immunostaining in the tissues transplanted with GAC-coated membranes, as shown in (C) fluorescence microscopic picture (Bar = 30 μm) and (D) enlarged picture (Bar = 10 μm).
To further confirm the RT-PCR result, CD117+ cells in the tissue transplanted with (PEI/pEGFP-N3-SDF-1α/collagen)-GAC-coated membrane were identified by immunostaining (Fig. 8C and D). There were no CD117+ cells found in the tissues transplanted with (PEI/pEGFP-N3/collagen)-GAC-coated membrane and naked membrane (data not shown). It suggested that (PEI/pEGFP-N3-SDF-1α/collagen)-GAC-coated membrane could home the CD117+ cells for regenerative process.
Inflammation induced by GAC was studied by H&E staining. Figure 9A and B showed that, comparing with the naked membrane, GAC-coated membrane did not induce obvious extra inflammation. There was inflammation still observed after 1 week of transplantation (Fig. 9C). However, after 2 weeks, the inflammation significantly diminished and remained only at the zone surrounding the membrane (Fig. 9D).
Fig 9.
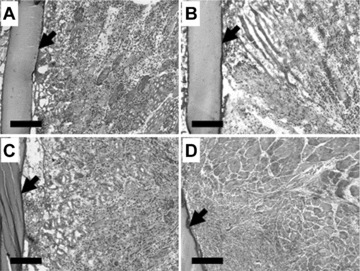
The inflammation induced by GAC (PEI/pEGFP-N3-SDF-1α/collagen, N/P = 4, C/D = 1) was evaluated with H&E staining. GAC was coated onto the mixed cellulose ester membrane with 40 μg DNA/membrane (3 mm × 4 mm), and then the membrane was transplanted into the quadriceps of mice. The tissues transplanted with naked membrane were used as control and harvested 3 days after transplantation (A). The tissues transplanted with GAC-coated membrane were harvested, respectively, at days 3 (B), 7 (C) and 14 (D) after transplantation. (Bar = 200 μm). The arrows indicate the naked membrane (A) and GACs-coated membranes (B, C, D).
Discussion
In this study, we have fabricated a collagen-based gene active substrate to provide the homing signals that promoted stem cell homing and recruitment. The SDF-1α/PEI complex was immobilized into the collagen scaffold for localized release of homing signal SDF-1α protein. Efficient transfection was achieved within the patterned area based on the optimized collagen amount, N/P ratio and DNA dosage. SDF-1α secreted by the transfected cells enhanced stem cell recruitment in flow chamber. In vivo, the SDF-1α gene activated matrix could recruit CD117+ stem cells after the hindlimb implantation.
Stem cell tissue engineering aimed at generating new tissue to repair damaged tissues or organs by combining biofunctional materials with stem cells. The new tissue could be generated either by direct transplantation of stem cells or stimulating stem cell homing to the injured site. SDF-1α is a pivotal signal that guides mature and immature stem/progenitor directional migration towards the high SDF-1α gradient and protect the stem cell from apoptosis [28, 29]. Bone marrow, with the highest SDF-1α level compared with other tissues, harbours a heterogeneous stem and progenitor cells positive for CXCR4 receptor under physiological condition. During regeneration process after injury, the up-regulation of SDF-1α level in damage organ stimulates stem cell mobilization from bone marrow to the injured area [8]. However, it has been well documented that SDF-1α is easily proteolytically degraded in very short time by matrix metalloproteinases and other proteinases, which are up-regulated after inflammation and hypoxia insult [18–20]. Therefore, it is important to have the active SDF-1α sustainedly released with a controlled manner. In this study, we successfully demonstrated that SDF-1α plasmid release could be sustained as long as 60 days. Furthermore, the manner of the stem cell homing to the SDF-1α active area was found with a refined spatial localization. Interestingly, our study showed that homed CD117+ cells may infuse with COS7 cells in an extremely low frequency. It suggested that endogenous somatic cells could acquire stem cell markers through simple fusion events. This result could provide an alternative interpretation for the evidence that engraftments of marked bone marrow stem cells (BMSCs) apparently displayed remarkable lineage plasticity following engraftment [3, 30].
For successful stem cell-based therapy, one major obstacle is the low cell engraftment. Stem cell microenvironment especially extracellular matrix (ECM) is a determined factor for stem cell local activity, such as adhesion, differentiation and proliferation. Many functional molecules of ECM and their interaction with stem cells were crucial to regulate stem cell survival, self-renewal and maintaining of stemness. Tissue engineered matrice for the delivery and support of transplanted cells is of great interest recently [21]. To this end, a wide range of natural and synthetic extracellular matrix with good biocompatibility, have been selected for stem cell tissue engineering purposes. However, synthetic materials could be rigid, elicit a mechanical or frictional irritation, limit cell mobility and vascularization, and have been inferior to extracellular matrix scaffolds that allow regeneration to occur; whereas collagen scaffold is a promising gene delivery system that offers good cytocompatibility and known structural physical and chemical properties. In addition, it offers a wide range of advantages for stem cell homing and migration. First, collagen gels provide a three-dimensional microenvironment in which stem cells can grow naturally. Second, collagen is a natural material, which minimizes the foreign body inflammatory response to the surrounding tissue and favours stem cell engraftment. Third, the degradation rate of collagen can be easily controlled with noncytotoxic cross-linking agents such as carbodiimide [31]. Furthermore, collagen is also chemotactic to mesenchymal stem cells [32], fibroblast [33] and other cell types [34]. In present study, SDF-1α plasmid condensed by PEI was readily incorporated into collagen matrix. We found that GAC significantly promote the cell proliferation. In vivo, no evidence of inflammation was found to be associated with GAC implantation, suggesting the GAC implantation would not increase the inflammation-induced matrix metalloproteinases and other proteinases, consequently the local released SDF-1α from transfected cells on the GAC could home the stem cells to the GAC for stem cell adhesion and proliferation on the surface of the matrices. All the findings demonstrated that GAC is an outstanding platform for stem cell tissue engineering.
In summary, gene-activated collagen substrate in this study may open up an important prospect to create a microenvironment for local and sustained stem cell recruitment. This gene-activated substrate for stem cell recruitment may be useful for regenerating a variety of tissue types that could also apply by combining with other chemokine genes. This gene delivery system may be therapeutically effective or serve as a model system to study the molecular interplay between cytokines and/or adhesion molecules involved in stem cell recruitment.
Acknowledgments
This work was supported by the German Helmholtz Association, Mecklenburg-Vorpommern (Nachwuchsgruppe Regenerative Medizin Regulation der Stammzellmigration 0402710), German Research Foundation, Sonderforschungsbereich/Transregio 7, B5, B2 and A4. We thank Ms. Margit Fritsche, Mr. Eric Pittermann, for their excellent technical assistance. We are grateful to Prof. Brigitte Vollmar, Prof. Eberhard
Burkel, Prof. Thomas Gerber, Dr. Faming Zhang, Dr. Gerd Holzhueter for their kind help.
References
- 1.Mimeault M, Batra SK. Recent progress on tissue-resident adult stem cell biology and their therapeutic implications. Stem Cell Rev. 2008;4:27–49. doi: 10.1007/s12015-008-9008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tateishi K, Takehara N, Matsubara H, et al. Stemming heart failure with cardiac- or reprogrammed-stem cells. J Cell Mol Med. 2008;12:2217–32. doi: 10.1111/j.1582-4934.2008.00487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li W, Ma N, Ong LL, et al. Bcl-2 engineered MSCs inhibited apoptosis and improved heart function. Stem Cells. 2007;25:2118–27. doi: 10.1634/stemcells.2006-0771. [DOI] [PubMed] [Google Scholar]
- 4.Nesselmann C, Ma N, Bieback K, et al. Mesenchymal Stem Cells and Cardiac Repair. J Cell Mol Med. 2008;12:1795–810. doi: 10.1111/j.1582-4934.2008.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slack JM. Stem cells in epithelial tissues. Science. 2000;287:1431–3. doi: 10.1126/science.287.5457.1431. [DOI] [PubMed] [Google Scholar]
- 6.Kørbling M, Estrov Z. Adult stem cells for tissue repair – a new therapeutic concept. N Engl J Med. 2003;349:570–82. doi: 10.1056/NEJMra022361. [DOI] [PubMed] [Google Scholar]
- 7.Shi Q, Hodara V, Butler SD, et al. Differential bone marrow stem cell mobilization by G-CSF injection or arterial ligation in baboons. J Cell Mol Med. 2008 doi: 10.1111/j.1582-4934.2008.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klopsch C, Furlani D, Gäbel R, et al. Intracardiac injection of erythropoietin induces stem cell recruitment and improves cardiac functions in a rat myocardial infarction model. J Cell Mol Med. 2009;13:664–79. doi: 10.1111/j.1582-4934.2008.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lapidot T, Dar A, Kollet O. How do stem cells find their way home? Blood. 2005;106:1901–10. doi: 10.1182/blood-2005-04-1417. [DOI] [PubMed] [Google Scholar]
- 10.Ma N, Stamm C, Kaminski A, et al. Human cord blood cells induce angiogenesis following myocardial infarction in NOD/scid-mice. Cardiovasc Res. 2005;66:45–54. doi: 10.1016/j.cardiores.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Zhang G, Nakamura Y, Wang X, et al. Controlled release of stromal cell-derived factor-1 alpha in situ increases c-kit+ cell homing to the infarcted heart. Tissue Eng. 2007;13:2063–71. doi: 10.1089/ten.2006.0013. [DOI] [PubMed] [Google Scholar]
- 12.Askari AT, Unzek S, Popovic ZB, et al. Effect of stromal-cell-derived factor 1 on stem-cell homing and tissue regeneration in ischaemic cardiomyopathy. Lancet. 2003;362:697–703. doi: 10.1016/S0140-6736(03)14232-8. [DOI] [PubMed] [Google Scholar]
- 13.Schantz JT, Chim H, Whiteman M. Cell guidance in tissue engineering: SDF-1 mediates site-directed homing of mesenchymal stem cells within three-dimensional polycaprolactone scaffolds. Tissue Eng. 2007;13:2615–24. doi: 10.1089/ten.2006.0438. [DOI] [PubMed] [Google Scholar]
- 14.Dar A, Goichberg P, Shinder V, et al. Chemokine receptor CXCR4-dependent internalization and resecretion of functional chemokine SDF-1 by bone marrow endothelial and stromal cells. Nat Immunol. 2005;6:1038–46. doi: 10.1038/ni1251. [DOI] [PubMed] [Google Scholar]
- 15.Bonig H, Priestley GV, Papayannopoulou T. Hierarchy of molecular-pathway usage in bone marrow homing and its shift by cytokines. Blood. 2006;107:79–86. doi: 10.1182/blood-2005-05-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dar A, Kollet O, Lapidot T. Mutual, reciprocal SDF-1/CXCR4 interactions between hematopoietic and bone marrow stromal cells regulate human stem cell migration and development in NOD/SCID chimeric mice. Exp Hematol. 2006;34:967–75. doi: 10.1016/j.exphem.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Blades MC, Manzo A, Ingegnoli F, et al. Stromal cell-derived factor 1 (CXCL12) induces human cell migration into human lymph nodes transplanted into SCID mice. J Immunol. 2002;168:4308–17. doi: 10.4049/jimmunol.168.9.4308. [DOI] [PubMed] [Google Scholar]
- 18.McQuibban GA, Butler GS, Gong JH, et al. Matrix metalloproteinase activity inactivates the CXC chemokine stromal cell-derived factor-1. J Biol Chem. 2001;276:43503–8. doi: 10.1074/jbc.M107736200. [DOI] [PubMed] [Google Scholar]
- 19.De La Luz Sierra M, Yang F, Narazaki M, et al. Differential processing of stromal-derived factor-1alpha and stromal-derived factor-1beta explains functional diversity. Blood. 2004;103:2452–9. doi: 10.1182/blood-2003-08-2857. [DOI] [PubMed] [Google Scholar]
- 20.Peterson JT, Li H, Dillon L, et al. Evolution of matrix metalloprotease and tissue inhibitor expression during heart failure progression in the infarcted rat. Cardiovasc Res. 2000;46:307–15. doi: 10.1016/s0008-6363(00)00029-8. [DOI] [PubMed] [Google Scholar]
- 21.Bonadio J, Smiley E, Patil P, et al. Localized, direct plasmid gene delivery in vivo: prolonged therapy results in reproducible tissue regeneration. Nat Med. 1999;5:753–9. doi: 10.1038/10473. [DOI] [PubMed] [Google Scholar]
- 22.Endo M, Kuroda S, Kondo H, et al. Bone regeneration by modified gene-activated matrix: effectiveness in segmental tibial defects in rats. Tissue Eng. 2006;12:489–97. doi: 10.1089/ten.2006.12.489. [DOI] [PubMed] [Google Scholar]
- 23.Kyriakides TR, Hartzel T, Huynh G, et al. Regulation of angiogenesis and matrix remodeling by localized, matrix-mediated antisense gene delivery. Mol Ther. 2001;3:842–9. doi: 10.1006/mthe.2001.0336. [DOI] [PubMed] [Google Scholar]
- 24.Labhasetwar V, Bonadio J, Goldstein S, et al. A DNA controlled-release coating for gene transfer: transfection in skeletal and cardiac muscle. J Pharm Sci. 1998;87:1347–50. doi: 10.1021/js980077+. [DOI] [PubMed] [Google Scholar]
- 25.Wang W, Li W, Ong LL, et al. Localized and sustained SDF-1 gene release mediated by fibronectin films – A potential method to recruit stem cells. Int J Artif Organs. 2009;32:141–9. doi: 10.1177/039139880903200304. [DOI] [PubMed] [Google Scholar]
- 26.Li W, Ma N, Ong LL, et al. Enhanced thoracic gene delivery by magnetic nanobead-mediated vector. J Gene Med. 2008;10:897–909. doi: 10.1002/jgm.1208. [DOI] [PubMed] [Google Scholar]
- 27.Guo T, Zhao J, Chang J, et al. Porous chitosan-gelatin scaffold containing plasmid DNA encoding transforming growth factor-beta1 for chondrocytes proliferation. Biomaterials. 2006;27:1095–103. doi: 10.1016/j.biomaterials.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 28.Ma N, Stamm C, Kaminski A, et al. Human cord blood cells induce angiogenesis following myocardial infarction in NOD/scid-mice. Cardiovasc Res. 2005;66:45–54. doi: 10.1016/j.cardiores.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 29.Jaleel MA, Tsai AC, Sarkar S, et al. Stromal cell-derived factor-1 (SDF-1) signalling regulates human placental trophoblast cell survival. Mol Hum Reprod. 2004;10:901–9. doi: 10.1093/molehr/gah118. [DOI] [PubMed] [Google Scholar]
- 30.Ambrosi DJ, Rasmussen TP. Reprogramming mediated by stem cell fusion. J Cell Mol Med. 2005;9:320–30. doi: 10.1111/j.1582-4934.2005.tb00358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Wachem PB, Plantinga JA, Wissink MJ, et al. In vivo biocompatibility of carbodiimide-crosslinked collagen matrices: Effects of crosslink density, heparin immobilization, and bFGF loading. J Biomed Mater Res. 2001;55:368–78. doi: 10.1002/1097-4636(20010605)55:3<368::aid-jbm1025>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 32.Lewus KE, Nauman EA. In vitro characterization of a bone marrow stem cell-seeded collagen gel composite for soft tissue grafts: effects of fiber number and serum concentration. Tissue Eng. 2005;11:1015–22. doi: 10.1089/ten.2005.11.1015. [DOI] [PubMed] [Google Scholar]
- 33.Gentleman E, Nauman EA, Dee KC, et al. Short collagen fibers provide control of contraction and permeability in fibroblast-seeded collagen gels. Tissue Eng. 2004;10:421–7. doi: 10.1089/107632704323061780. [DOI] [PubMed] [Google Scholar]
- 34.Gentleman E, Nauman EA, Livesay GA, et al. Collagen composite biomaterials resist contraction while allowing development of adipocytic soft tissue in vitro. Tissue Eng. 2006;12:1639–49. doi: 10.1089/ten.2006.12.1639. [DOI] [PubMed] [Google Scholar]


