Abstract
Context
Eating disorders, an important health problem among college-age women, may be preventable, given that modifiable risk factors for eating disorders have been identified and interventions have been evaluated to reduce these risk factors.
Objective
To determine if an Internet-based psychosocial intervention can prevent the onset of eating disorders (EDs) in young women at risk for developing EDs.
Setting and Participants
College-age women in San Diego and the San Francisco Bay Area. Women with high weight and shape concerns were recruited via campus e-mails, posters and mass media. Six hundred thirty-seven eligible participants were identified, of whom 157 were excluded, for a total sample of 480. Recruitment occurred between 11/13/00 and 10/10/03.
Design and Intervention
A randomized controlled trial of an eight-week Internet-based cognitive-behavioral intervention (Student Bodies; SB) that included a moderated online discussion group. Participants were followed for up to three years.
Main Outcome Measures
The main outcome measure was time to onset of a subclinical or clinical ED. Secondary measures included change in Weight Concerns Scale (WCS) scores, Global EDE-Q, EDI Drive for Thinness, EDI Bulimia, and depressed mood. Moderators of outcome were examined.
Results
There was a significant reduction in WCS scores in the SB intervention group compared to the control group at post intervention (p < 0.001), one year (p < 0.001) and two years (p <0.001). The slope for reducing WCS was significantly greater in the treatment compared to the control group (p = 0.023). Over the course of follow-up, 43 participants developed subclinical or clinical EDs. While there was no overall significant difference in onset of EDs between intervention and control groups, the intervention significantly reduced the onset of EDs in two subgroups identified through moderator analyses: 1) participants with an elevated body mass index (BMI ≥ 25) at baseline; and 2) at one site, participants with baseline compensatory behaviors (e.g. self-induced vomiting, laxative use, diuretic use, diet pill use, driven exercise). No intervention participant with an elevated baseline BMI developed an ED, while the rates of onset of ED in the comparable BMI control group (based on survival analysis) were 4.7% at one year and 11.9% at two years (CI = 2.7%–21.1%). In the BMI ≥ 25 subgroup, the cumulative survival incidence was significantly lower at two years for the intervention compared to the control group (CI = 0% for intervention; 2.7% – 21.1% for control). For the San Francisco Bay Area site sample with baseline compensatory behaviors, 4% of participants in the intervention group developed EDs at one year and 14.4% by two years. Rates for the comparable control group were 16% and 30.4%, respectively.
Conclusions
Among college-age women with high weight and shape concerns, an eight-week Internet-based cognitive-behavioral intervention can significantly reduce weight and shape concerns for up to two years and decrease risk for the onset of EDs, at least in some high-risk groups. This is the first study to show that EDs can be prevented in high risk groups.
Keywords: Eating disorders, prevention, risk-factors, moderators, Internet delivered interventions
Approximately 2–4 % of the young adult female population suffers from full syndrome eating disorders (EDs) (anorexia nervosa, bulimia or binge eating disorder) (1,2). The peak age of onset appears to be around 16–20 years, about the time when young women begin leaving home and starting college (2). In addition, rates of subthreshold or partial syndrome EDs likely exceed those of full syndrome EDs (3), suggesting that the combined rates easily exceed 4%. Furthermore, subthreshold or partial syndrome EDs exist on a continuum with full syndrome EDs, and represent similar levels of functional impairment (3).
Unhealthful weight regulation methods and body image concerns, which predispose people to clinical and subclinical EDs (4, 5), are common among high school and college students. For instance, 9% of high school females in the United States reported self-induced vomiting or laxative use to control their weight in the past month according to a national study by the Centers for Disease Control and Prevention (6). The number of college women with body image concerns is even more prevalent. Overall, 35% to 45% of adolescent females report difficulties with weight control, regard themselves as too fat, or aspire to become thinner (7). Eating disorders are known to be chronic, persistent, and refractory to treatment (8).
Eating disorder attitudes and behaviors can have serious psychological and physical consequences. These attitudes and behaviors are associated with low confidence and self-esteem, shame and other psychological problems (9–11). Self-induced vomiting and laxative use can lead to significant physical consequences, including dental erosion, esophageal tears, and other medical problems (12) and also are risk factors for the development of EDs (5).
In recent years, a number of potentially modifiable risk factors for EDs have been identified. Across populations and in longitudinal studies, excessive weight and shape concerns have been consistently associated with the onset of subclinical and clinical level EDs (4,5). Given their importance as a risk factor, many investigators have attempted to reduce weight and shape concerns (13). We have shown that Student Bodies (SB) an Internet-based cognitive-behavioral intervention is effective in reducing weight and shape concerns (14–17). However, all of these previous studies were short-term with small sample sizes. Thus, the goals of the present study were to: 1) replicate these findings in a large sample of college women; 2) evaluate the intervention’s long-term impact on reducing weight and shape concerns in college women at risk for developing EDs; 3) determine if the intervention could increase survival as a non-ED case; and 4) examine moderators and mediators of outcome.
METHODS
Participants
Participants were female college-age women between 18 and 30 years of age who were at high risk for developing an ED, who had a BMI ≥ 18 and < 32, and resided in the San Diego and the San Francisco Bay areas. Potential participants were recruited from flyers posted at local academic institutions, campus mailings and mass media. Potential participants completed a brief screening questionnaire delivered by e-mail. Interested and eligible women gave informed consent for their participation, completed several self-report assessments and underwent a semi-structured diagnostic clinical interview. The study was approved by the human subjects committees at each of the participating institutions and by the human subjects committees at Stanford University and San Diego State University. Women who met clinical criteria for a DSM-IV diagnosed ED at baseline were excluded from the study and referred to appropriate providers. Participant randomization was stratified by school and random number sequences were generated by the study coordinator using SPSS.
The Weight Concerns Scale (WCS) (18) was used to determine preliminary eligibility for high-risk participants. The WCS consists of five questions that assess worry about weight and shape, fear of gaining 3 pounds, last time on a diet, importance of weight and feelings of fatness. The WCS has test-retest reliability of 0.85, and good predictive validity (18,19). A ROC analysis found that a WCS score ≥ 47 had sensitivity of 79%, specificity of 67% and PPV value of 13% for identifying adolescents who developed partial or full syndrome EDs (20). Participants were considered potentially eligible for this study if they scored ≥ 50 on the WCS, reported they were moderately or very afraid of gaining 3 pounds, or reported that their weight was the most important thing in their life.
Women were excluded from participation in the study if they had a current diagnosis of a subclinical or clinical ED or had been in treatment for an ED within the past six months, if they acute suicidal ideation and/or evidence of drug or alcohol abuse or dependence. ED diagnoses and assessment of ED behaviors were made with the EDE interview adapted to include the diagnostic criteria for binge eating disorder (BED). The EDE (21) is a semi-structured interview that generates ED diagnoses based on DSM-IV criteria. It has demonstrated high internal consistency (22), sensitivity to change (22, 23), and inter-rater reliability (22, 23). The EDE assesses objective bulimic episodes (OBE; objective overeating with loss of control [LOC]), subjective bulimic episodes (SBE; LOC without objective overeating as judged by the interviewer, but perceived as excessive by the interviewee), objective overeating (OO; overeating without LOC), self-induced vomiting, laxative, diuretic or diet pill use, and driven exercise. At each yearly follow-up, the interviewers retrospectively assessed eating behaviors for each month in the previous year with a structured timeline follow-back approach. Interviewers first identified the most recent, if any, OBEs/SBEs, and these episodes were used as prototypes throughout the interview. A 12-month calendar was used as a reference and the occurrence of OBEs, SBEs and OOs was assessed for each month. The frequency of compensatory behaviors was assessed using the same interview format. At baseline only, participants underwent a structured clinical interview for DSM-IV diagnoses (24) conducted by experienced interviewers. Women who reported current prescription medication use for mood or anxiety disorders were included if their medication was stable for at least two months, and they were not disqualified by other exclusion criteria.
Intervention
The SB intervention was an eight-week, Internet-based, structured cognitive-behavioral program combined with an on-line, asynchronous, moderated discussion group. The primary goal of the program was to reduce body dissatisfaction and excessive weight concerns. The program incorporated elements of interventions previously shown in controlled studies to be effective at reducing ED attitudes and behaviors. The core goals of the program were to reduce weight and shape concerns, enhance body image, promote healthy weight regulation, reduce binge eating, and increase knowledge about the risks associated with EDs. Each week, when a participant logged onto the program, she was directed to the updated weekly program content. Participants were expected to read the content and complete accompanying assignments that included participating in the online discussion group, self-monitoring, and/or writing entries in the Personal Journal or Body Image Journal. Discussion groups were moderated by a clinical psychologist or psychology graduate student who was supervised by a clinical psychologist. Weekly e-mails were sent to participants to reinforce program participation and encourage participants who failed to comply with study expectations for participation. About nine months following the 8-week intervention, participants were notified by e-mail that the program would be available for two weeks to review material from the initial eight sessions. The control group was given the opportunity to complete the SB intervention at the end of follow-up.
Measures
Participants reported their age, year in school, ethnicity, and mother’s and father’s highest level of education.
All participant interviews were audiotaped. Audiotapes were periodically reviewed by senior interviewers at each site and interviewers received written and/or verbal feedback. At follow-up, EDE interviews were conducted in-person if the participant resided near one of the two sites. Otherwise, interviews were conducted by telephone, a method shown to be reliable for assessing a number of Axis I psychiatric disorders (25,26). Interviewers were blind to participant group assignment.
Diagnoses of anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED) corresponded with the DSM-IV and were consistent with previous studies (27). Subclinical AN was diagnosed if the participant met all AN criteria except amenorrhea. Subclinical BN was diagnosed if the binge eating and inappropriate compensatory behaviors occurred at a frequency of less than twice a week or for a duration of less than three months, and one OBE or SBE and one purge behavior occurred at least once per week on average for three months, or purge behavior occurred two or more times per week on average for at least one month. Subclinical BED was diagnosed if the participant had an OBE at least once per week, on average, for at least three months accompanied by marked distress. Participants were considered cases when they first met the criteria for subclinical or clinical EDs, were referred by the research team for ED treatment, or started seeing a mental health provider for an ED. To determine potential cases, a committee of four experts who were blind to the participants’ group assignment assessed the monthly data including occurrence of OBE, SBE, and compensatory behaviors, and made independent diagnoses. The research team reviewed diagnoses and disagreement was resolved by consensus. Because diagnostic criteria were predetermined, only cases referred for treatment or referral required review.
Post intervention assessment occurred immediately following the cessation of the intervention, and follow-up assessments were approximately one, two, and three years after cessation of the intervention.
Eating disorder attitudes and behaviors were assessed using the WCS (18,19), the Eating Disorder Inventory (EDI) Drive for Thinness and Bulimia subscales, and the Eating Disorder Examination Questionnaire (EDE-Q), a self-report version of the EDE. The EDI subscales are widely used and have good internal consistency (28). The EDE-Q is a 41-item self-report version of the EDE that yields four subscales: Restraint, Weight Concerns, Shape Concerns, and Eating Concerns. The EDE-Q has good internal and temporal consistency (29). For these measures higher scores indicate worse symptom severity.
The Center for Epidemiologic Studies Depression Scale (CESD), a 20-item self-report questionnaire, was used to assess depressed mood (30). The CESD has high internal consistency, adequate test-retest reliability, and convergent validity (31).
Social support was measured with the Multidimensional Social Support Scale (MSPSS) 32, a 12-item self-report measure of perceived social support (33).
Standing height was measured to the nearest millimeter. Weight was determined to the nearest 0.1 kg using a digital stand-on scale with participants wearing light indoor clothing without shoes or coats. Height and weight were converted to body mass index (BMI = weight kg/height m2).
Adherence
Each week, participation in the intervention was monitored for each participant. Adherence was defined as the percent of assigned “Web pages” accessed each week averaged by the eight weeks of the intervention period.
Statistical Analysis
The sample size was based on having sufficient power to detect a 5% difference at two years, with the assumption that 10% of participants would develop an ED and the intervention would reduce the rate by 50% to 5%. Cox Regression models were the primary analysis to predict time to onset of clinical or subclinical EDs. The primary outcome measure was survival as a non-ED case. The model for examining potential moderators follows statistical recommendations by Kraemer and colleagues (34). Potential moderators were identified a priori and their univariate effect on the intervention outcome was examined. Significant variables were examined in terms of their interaction with outcome. The authors hypothesized that the intervention would lead to significantly reduced weight and shape concerns as a prerequisite to the primary hypothesis, survival as a non-ED case. Secondary measures including, weight and shape concern variables, were examined with an ANCOVA, controlling for baseline values. All models included site and site interactions. Controlled effect sizes were calculated using Cohen’s d statistic.
RESULTS
Participant Flow
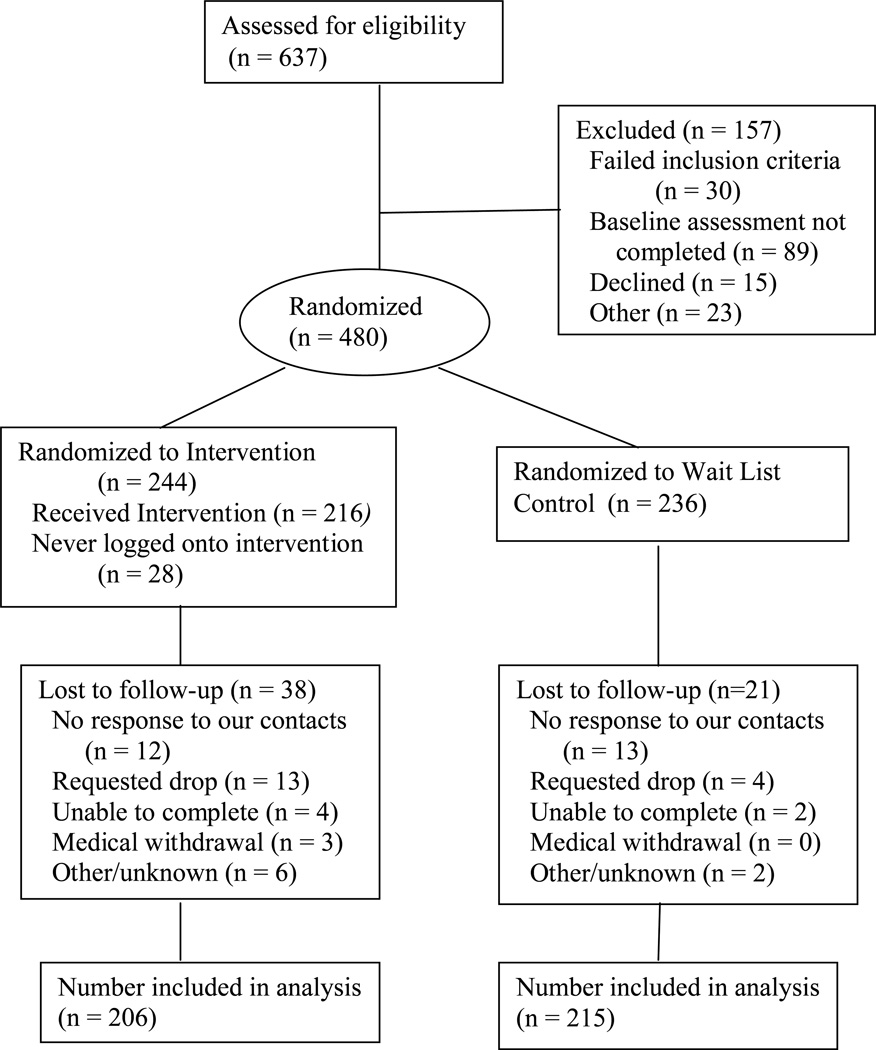
Participant flow can be seen in Figure 1. Recruitment occurred between 11/13/00 and 10/10/03, in three waves (wave 1, 11/13/00 – 10/14/01; wave 2, 10/15/01 to 10/11/02; wave 3, 10/14/02 to 10/10/03). Participants recruited during wave 1 were assessed annually for up to three years, participants recruited during wave 2 were assessed annually for up to two years, and participants recruited during wave 3 were assessed at one year. Overall, 637 eligible participants were identified after screening, of whom 157 were excluded. Four hundred eighty women were eligible, interested, and randomized following diagnostic interviewing. Fifty-nine (14%) participants had no follow-up data and, hence, were not available for the survival analysis. The follow-up response rates by recruitment/intervention waves were as follows: Wave 1: post = 91% (145/159), one year = 81% (129/159), two years = 81% (128/159), three years = 69% (110/159); Wave 2: post = 92% (170/185), one-year = 86% (160/185), two years = 82% (151/185); Wave 3: post = 95% (129/136), one year = 90% (122/136). Overall, compliance with follow-up assessments was quite high. Only 38 (16%) of the intervention participants did not complete any follow-up assessments compared to 21 (9%) of control participants. There were no dropout differences on demographic, eating psychopathology or eating behavior variables.
Figure 1.
Flowchart for subject recruitment, randomization and follow-up
Ethnicity of the final sample was 60% Caucasian, 2% African-American, 10% Hispanic, 17% Asian, and 11% other/unknown. By year in school, the sample was 31% freshman, 20% sophomore, 22% junior, 18% senior, and 8% graduate student. The average age was 20.8 (range 17–31; SD = 2.6).
Participants randomly assigned to the intervention had significantly lower WCS scores, F(1,414) = 3.9, p = .048 and Global EDE-Q scores, F(1,417) = 4.9, p = .027. There were no other significant differences between the intervention and control groups on demographics, baseline measures of psychopathology or ED behaviors. The Bay Area site had parents with higher levels of education, F(1,275)=41.0 p=.000, fewer negative life events, F(1,478)=8.2 p=.004, higher prevalence of diuretic use, F(1,478)=6.5 p=.01, lower prevalence of driven exercise, F(1,478)=10.0 p=.002, and diet pills F(1,478)=6.9 p=.000, higher prevalence of objective binges, F(1,478)=4.4, p=.037, and lower motivation F(1,473)=74.0, p=.000.
Intervention Implementation
The intervention was provided to 13 groups and ranged in size from 14 to 24 members per group. Of the 244 participants who were randomized to the intervention, 28 (11%) never logged onto the program. For the remaining 216, adherence to the intervention protocol was high: the mean percent of pages read was 79% (range 6–99%; SD = 24.2). There was a significant difference on adherence between study sites. Adherence was higher for participants with higher WCS scores, t(1) = 2.2, p = .029, EDI Drive for Thinness, t(1) = 3.5, p = .020, Global EDE-Q, t(1) = 2.8, p = .005, and EDI Bulimia, t(1) = 2.3, p = .024. Higher adherence resulted in reduced post test scores on WCS scores,. (t(209)=−2.3 p=.022; EDE-Q Restraint, (t(211)=−3.0 p=.003, and the EDE-Q Weight Concerns, t(211)=−2.3 p=.025. Ninety-seven participants (40%) of the treatment group used the booster session at least once following completion of the core 8-week program. Use of the booster sessions was not related to outcome.
Change in ED Attitudes and Behaviors
As seen in Table 1, there were statistically significant baseline to post intervention and baseline to one-year follow-up differences between intervention and control groups on the WCS scores, Global EDE-Q and EDI Drive for Thinness. In addition, there was a significant reduction in the intervention group on EDI Bulimia from baseline to post intervention. The WCS slope was significantly steeper for treatment compared to control (F(1,450) = 5.2, p = 0.023). There were no significant wave, wave×center, wave×treatment, wave×treatment×center effects on slope. Participant BMIs remained remarkably stable for all cohorts across all years. No adverse events were reported.
Table 1.
Changes in Eating Disorder Attitudes, Mood, and BMI from baseline to post and one year follow-up
| N | Baseline | Post test | 12 months | Post test significance |
12 months significance |
||
|---|---|---|---|---|---|---|---|
| WCS | C | 199 | 62.7 (12.5) | 62.5 (13.4) | 56.4 (16.5) | F(1,386)=89.7, p<.001, d = .81 |
F(1,386)=16.1, p<.001, d = .42 |
| T | 192 | 60.5 (13.5) | 49.7 (15.9) | 48.8 (17.9) | |||
| Global EDE-Q | C | 201 | 2.7 (.9) | 2.6 (1.0) | 2.3 (1.0) | F(1,392)=76.7 p<.001, d =.70 |
F(1,392)=10.7, p=.001, d =.36 |
| T | 196 | 2.5 (1.0) | 1.9 (1.0) | 1.9 (1.1) | |||
| EDI Drive for thinness | C | 195 | 8.5(5.0) | 8.7(5.5) | 7.1(5.8) | F(1,383)=54.7, p=.001, d = .61 |
F(1,383)=17.1, p<.001, d = .39 |
| T | 193 | 8.1(5.3) | 5.2(5.2) | 5.0(5.2) | |||
| EDI Bulimia | C | 197 | 1.2(2.0) | 1.4(2.8) | 1.2(2.5) | F(1,386)=10.0, p=.002, d = .22 |
F(1,386)=2.5, p=.112, d = .11 |
| T | 194 | 1.3(2.4) | 0.9(1.5) | 0.9(2.2) | |||
| BMI* | C | 171 | 23.4 (2.6) | 23.5 (2.7) | 23.4 (2.8) | F (1,338) = 23, p =.65,d = 0.0 |
F (1,338) = .04, p =.83, d = −.04 |
| T | 172 | 23.5 (2.8) | 23.5 (3.1) | 23.5 (2.8) | |||
| CESD | C | 198 | 14.8 (9.0) | 14.8 (9.6) | 15.2 (11.7) | F(1,384)=1.2, p=.27, d = .16 |
F(1,384)=3.3, p=.07, d = .21 |
| T | 191 | 13.6 (8.9) | 13.2 (9.7) | 12.9 (9.8) | |||
Abbreviations: WCS = Weight and Shape Concerns, EDE-Q = Eating Disorder Examination-Questionnaire, CESD = Center for Epidemiology Scale-Depression, C = control, T = Treatment
BMI not collected for participants assessed by phone at follow-ups.
Clinical cases
Over the course of follow-up, 43 participants were classified as becoming a subclinical or clinical eating disorder case. Ten participants were classified as being cases on the basis of reporting entering therapy for treatment of an eating disorder. Of the remaining 33, the diagnoses were 2 with BN, 27 with subclinical BN and 14 with subcinical BED.
Moderators
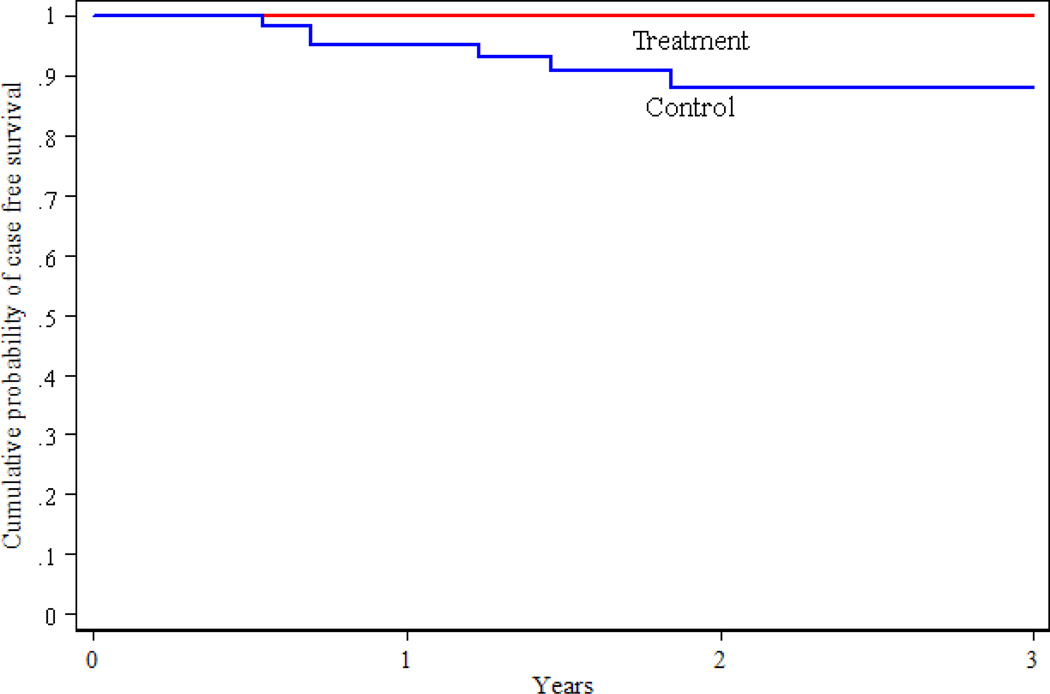
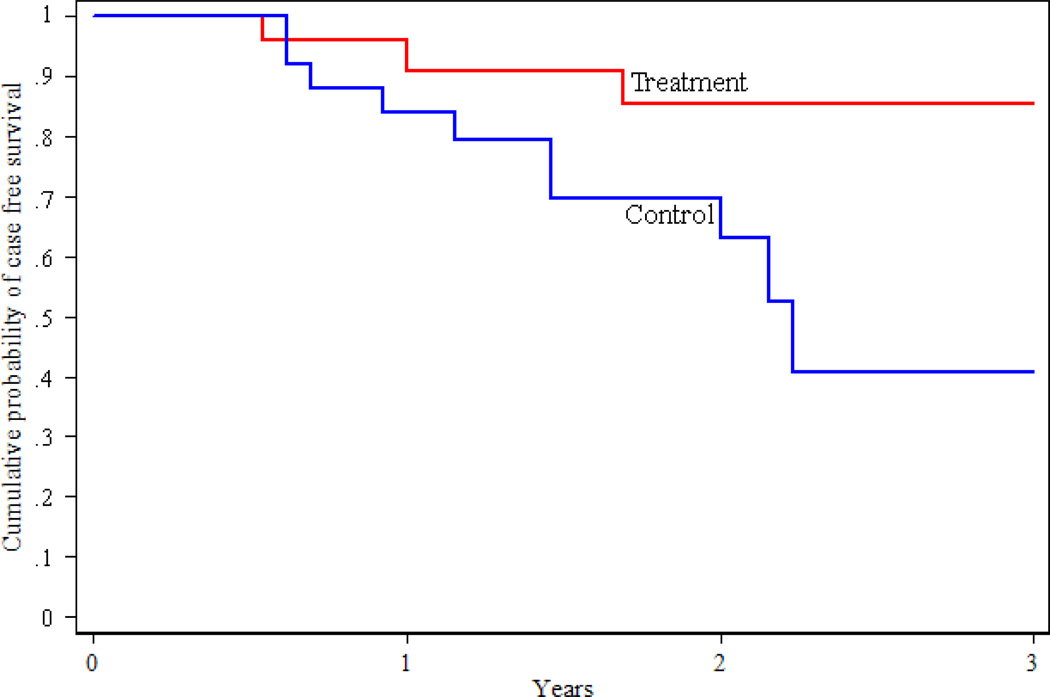
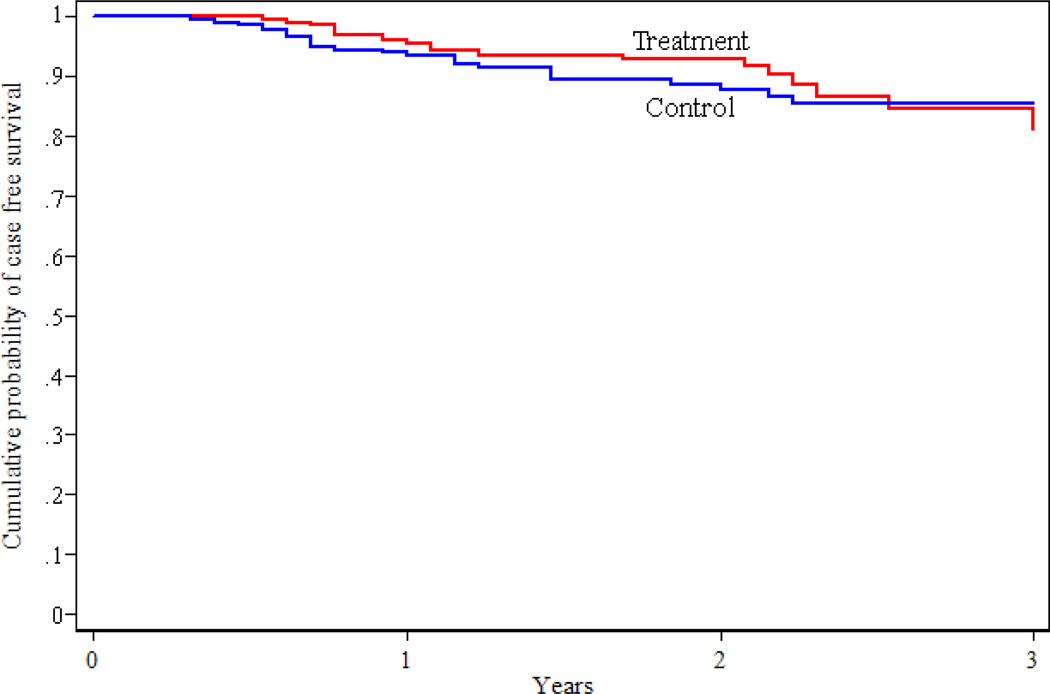
The moderator analysis (34) identified a number of non-specific predictor variables including year in school, W(1) = 5.3, p = .02, with participants further in school being less likely to develop an ED and, as expected, all ED attitude variables. Baseline BMI and use of compensatory behaviors (SF Bay Area site) both predicted outcome and interacted with treatment. The intervention significantly increased survival as a non-ED case in participants with an elevated baseline BMI, W(1) = 11.2, p = .001, and participants with baseline compensatory behaviors (self-induced vomiting, laxative use, diuretic use, diet pill use, driven exercise) at one site, W(1) = 4.0, p = .046. No participants with BMI ≥ 25 who received the intervention developed an ED, whereas the rates of onset of EDs were 4.7% at one year and 11.9% at two years in the comparable BMI control group. For the SF Bay Area sample with baseline compensatory behaviors, 4% of participants developed EDs at one year and 14.4% by two years. The rates for the comparable control group were 16% and 30.4%. Figures 3 and 4 display the survival curves for the moderator subgroups. The numbers of participants in the groups are as follows: BMI < 25 and no compensatory behaviors, n = 215; BMI ≥ 25 and no compensatory behaviors, n = 85; BMI < 25 with compensatory behaviors, n = 88; BMI ≥ 25 with compensatory behaviors, n = 30. In total, about 49% (203/418) of the overall sample fell into one of the groups where the intervention was effective.
Figure 3.
Survival as a non-ED case for participants with a BMI≥25 at baseline. Note that there were no cases in the treatment group.
Figure 4.
Survival as a non-ED case for San Francisco Bay Area participants with compensatory behaviors at baseline
The one and two year incidence based on the cumulative survival curves can be seen in Table 2. The two year incidence rates were lower in the intervention compared to control in all cohorts at all times. The one year overall incidence in the control group was lower than expected, although the two year incidence was close to prediction (10% in the control group; 5% in the intervention group). There was a significant difference in the incidence of EDs in the BMI ≥ 25 subgroup (CI = 0%) compared to 11.9% (CI = 2.7–21.1%) in the BMI < 25 group.
Table 2.
One and two year Incidence Rates from the Survival Data for Onset of Eating Disorders
| San Francisco Bay Area |
San Diego | Total | |||||
|---|---|---|---|---|---|---|---|
| Year 1 | Year2 | Year 1 | Year2 | Year 1 | Year2 | ||
| Overall | Control | 7.7% (2.8%–12.5%) N=107 |
12.8% (6.1%–19.5%) N=60 |
4.1% (.2%–8.1%) N=91 |
9.5% (3.1%–15.9%) N=57 |
6.6% (3.4%–9.8%) N=198 |
11.3% (6.6%–16%) N=117 |
| Treatment | 5.4% (1.2%–9.6%) N=104 |
10.0% (5.8%–14.2%) N=60 |
2.2% (−.8%–5.3%) N=89 |
3.7% (−.5%–7.9%) N=57 |
4.0% (1.3%–6.7%) N=193 |
7.2% (3.4%–11%) N=116 |
|
| BMI ≥ 25 kg at baseline | Control | 5.6% (−1.9%–13.0%) N=32 |
10.8% (−1.5%–23.1%) N=15 |
3.6% (−3.3%–10.4%) N=26 |
12.5% (−.9% – 26%) N=18 |
4.7% (−.5% – 9.9%) N=58 |
11.9% (2.7%–21.1%) N=33 |
| Treatment | 0% (0%) N=26 |
0% (0%) N=14 |
0% (0%) N=22 |
0% (0%) N=11 |
0% (0%) N=48 |
0%* (0%) N=25 |
|
| Compensatory behaviors at baseline | Control | 16% (1.6%–30.4%) N=22 |
30.4% (11.3%–49.4%) N=12 |
2.6% (−2.5%–7.7% N=37 |
11.6% (.9%–22.3%) N=27 |
8% (1.3%–14.7%) N=59 |
19% (8.8%–29.2%) N=39 |
| Treatment | 4% (−3.7%–11.7%) N=22 |
14.4% (−.8%–29.6%) N=14 |
3.2% (−2.9%–9.3%) N=32 |
6.9% (−2.4%–16.2%) N=22 |
3.6% (−1.3%–8.5%) N=54 |
10.1% (1.6%–18.5%) N=36 |
|
Significantly different with no overlap of confidence intervals.
At baseline, only 14 subjects were taking antidepressants, and 11 of these continued to be on meds during the follow-up period. Only 11 subjects started medications. Of the 25 who were on meds, 5 developed EDs: 4 controls and 1 treatment.
Discussion
The most important finding of this study is that a brief, eight-week, Internet-based cognitive-behavioral intervention led to sustained reductions in weight and shape concerns in college-age women who were at high risk for developing EDs. While there was no overall decrease in the onset of EDs, participation in the intervention was associated with a decrease in the onset of EDs in two subgroups constituting about half the sample: those who had baseline compensatory behaviors (self-induced vomiting, laxative use, diuretic use, diet pill use, driven exercise) and those who had elevated baseline BMIs. The data provide further evidence that elevated weight and shape concerns identifies college-age women who are at risk of subsequently developing EDs and/or who engage in unhealthy weight regulation practices. The overall rate of ED onset was at least 9% (43 of 480 participants).
Reductions in weight and shape concerns, the primary risk factor, were impressive. The short-term, post intervention effect size on the main risk factor, d = .81, was similar to those for comparable pre-post time periods in efficacy studies (14,15,17). Intervention and control differences on WCS scores remained significant at one year with an effect size in the moderate range, d = .41.
Although the slope of the decline in WCS was significantly greater in intervention compared to control group participants, both groups continued to improve over time. This improvement may be the result of statistical regression to the mean or normal developmental processes for college women. With experience and maturity, weight and shape concerns may become less important to many women. The sustained improvement in weight and shape concerns, and the improvement in the control group, occurred with no overall changes in BMI suggesting participants were not feeling better about their weight and shape because of weight loss which was not advocated in the intervention.
This study provides some evidence that elevated weight and shape concerns is a causal risk factor for the onset of EDs on the basis that reduction of weight and shape concerns was associated with reduced onset of EDs, at least in one subgroup- women with elevated baseline BMIs. However, these findings need confirmation in a prospective trial with these subgroups randomized to treatment or control.
While there was a significant reduction in weight and shape concerns, the median WCS scores at two years remained above the threshold entry criteria for the study. How could the intervention be improved? The overall adherence to the intervention was high (e.g. 79% of assigned pages were read), thus it is unlikely that adherence could be significantly improved. A face-to-face intervention might be more effective although the effect sizes are comparable to those reported in studies that used face-to-face interventions (15,35). Another potential modification would be to add a post-intervention monitoring feedback component that would monitor weight and shape concerns, binge eating, and compensatory behaviors so participants could receive an additional intervention when they might most need it.
The results for the subgroup with BMI ≥ 25 are exciting but need to be replicated in a prospective study using a sample selected on this basis. We arbitrarily picked a BMI of <32. We thought a higher BMI cut-off would allow us to include participants with higher weights where weight maintenance and not weight loss would be acceptable. There were 17 subjects (about 4% of the sample) with a BMI in the range of 30–31.
The subgroup of participants who, at baseline, had high weight and shape concerns, BMI < 25, and no compensatory behaviors might have other characteristics that differentiate them from participants in the subgroups in which the intervention was effective. They may have a stronger and more refractory internalization of a thin-body ideal or other characteristics less amenable to change or that were not addressed in SB. It may also be the case that providing the intervention when women are struggling with weight management, as evidenced by use of inappropriate compensatory behaviors, might make it more immediately relevant to them and thus more effective.
An Internet-based program can provide relatively inexpensive electronic reminders and be made available for "booster sessions" after completion of an intervention such as Student Bodies. In this study, participants were allowed access to the core program about nine months after completion of the core 8-week program. Less than half did so and there was no significant benefit for those who did. Booster or maintenance sessions may be important to prevent relapse and sustain benefits but probably need to be actively incorporated into a program.
Differences in ED attitudes, behaviors and outcomes were noted between the two sites. We do not know if these differences represent different populations reached through recruitment or if regional differences affect the presentation of EDs. Differences between the types of compensatory behaviors used by participants at the two sites might also explain why there was a significant effect at the SF Bay Area site but not the SD Area site for prevention of EDs in participants with baseline compensatory behaviors. Participants in the the SF Bay Area were more apt to report using laxatives, diuretics and vomiting whereas participants in SD reported higher levels of diet pill use and driven exercise (36).
The criteria for subclinical eating disorders were those we have used in other studies (27,37) and were developed to operationalize "case" criteria that are clinically considered to be EDNOS. Overall, most studies have found a continuity between subclinical and clinical symptoms (e.g. 37–38).
The results of this study should be considered in the context of several limitations. First, although our targeted participant pool was within the typical age of onset (2) and we recruited from both public and private academic institutions that ranged considerably in size, generalizability is restricted to college women in Northern and Southern California. Our data showed differences between the two sites in baseline characteristics and in treatment response. Thus, sampling from different regions, age groups, diverse groups, and/or the general population might have lead to different outcomes. Second, participants were highly motivated to participate in the study and enhance their body image, as evidenced by the high rates of adherence to the intervention protocol. Women who are less motivated, have more barriers to participation, or are more diverse might show different outcomes. For example, in this study, participants were required to have Internet access and a minimum level of competency with computers. Restricted computer access and lesser competency might affect adherence to the intervention protocol and subsequent treatment outcome. The use of a self-report measure and a retrospective self-report are other limitations. Although we used the timeline follow-back approach, which has been shown to be reliable for measuring a number of behaviors over the preceding year (39, 40), the method includes data "remembered" from as long as 12 months before. The diagnoses of bulimia and binge-eating require the target behaviors occur for at least 3 months, inherently requiring a relatively long-term recollection. Some of the remembered events, such as going into therapy, however, are likely to be accurately recalled. A prospective monthly assessment would be ideal to avoid this problem but might also generate its own bias such as underreporting, aside from the increased measurement costs incurred. Ravaldi et al (41) gave the EDE to 25 female patients who had previously been assessed a year or more earlier. The test-retest of the subscales was 0.7 or greater, suggesting that the EDE is a reliable interview even when administered retrospectively.
An Internet-based intervention has the advantage of facilitating rapid dissemination. The most significant cost is related to group moderation. Discussion group moderators need to be selected, trained, and in some cases, supervised. In our studies, about 1–2 hours per week was required to moderate groups of 10–20 participants. Future studies might examine the benefit of or need for moderation and explore ways that moderation can be provided less expensively. Furthermore, Internet-based programs can be used as a first step in a stepped-care program to screen women for possible ED risk and classify women with high ED risk as early as possible to facilitate further assessment and treatment recommendations (42). There are a number of research and delivery issues related to a stepped-care program (42) but this study provides an important initial step in that direction. Overall, this research lends support that Internet-based interventions can significantly reduce weight and shape concerns for two years among college-age women with high weight and shape concerns. This is the first study to show that EDs can be prevented in a high risk group: the intervention significantly reduced the risk of ED in college-age women who had elevated baseline BMIs and/or low-level baseline compensatory behaviors. The results from this investigation also suggest that reducing risk factors in high-risk groups can lead to reductions in the onset of EDs.
Figure 2.
Survival as a non-ED case: Intervention v. control through three years
Acknowledgement
The study was funded by NIMH Grant R01 MH60453. We want to thank Ruth Striegel-Moore, PhD and Alison Field, ScD for serving on the Data Safety and Monitoring Board. Dr. Wilfley is also supported by grant 1K24MH070446-01 from the National Institute of Mental Health, National Institutes of Health.
References
- 1.Fairburn CG, Beglin SJ. Studies of the epidemiology of bulimia nervosa. Am J Psychiatry. 1990;147(4):401–408. doi: 10.1176/ajp.147.4.401. [DOI] [PubMed] [Google Scholar]
- 2.Striegel-Moore RH, Dohm FA, Kraemer HC, Taylor CB, Daniels S, Crawford PB, Schreiber GB. Eating disorders in white and black women. Am J Psychiatry. 2003;160(7):1326–1331. doi: 10.1176/appi.ajp.160.7.1326. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgibbon ML, Sanchez-Johnsen LA, Martinovich Z. A test of the continuity perspective across bulimic and binge eating pathology. Int J Eat Disord. 2003;34(1):83–97. doi: 10.1002/eat.10160. [DOI] [PubMed] [Google Scholar]
- 4.Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 5.Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004;130(1):19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- 6.MMWR. Youth Risk Behavioral Surveillance--United States. Morb Mortal Wkly Rep. 2000 Jun;9(SS05):1–96. [Google Scholar]
- 7.Klemchuk HP, Hutchinson CB, Frank RI. Body dissatisfaction and eating-related problems on the campus: Usefulness of the Eating Disorder Inventory with a nonclinical population. J Couns Psychol. 1990;37:297–305. [Google Scholar]
- 8.Fairburn CG, Harrison PJ. Eating disorders. Lancet. 2003;361:407–416. doi: 10.1016/S0140-6736(03)12378-1. [DOI] [PubMed] [Google Scholar]
- 9.Stice E, Killen JD, Hayward C, Taylor CB. Support for the continuity hypothesis of bulimic pathology. J Consult Clin Psychol. 1998;66(5):784–790. [PubMed] [Google Scholar]
- 10.Taylor CB, Altman T, Shisslak C, Bryson S, Estes LS, Gray N, McKnight KM, Kraemer HC, Killen JD. Factors associated with weight concerns in adolescents. Int J Eat Disorders. 1998;24:31–42. doi: 10.1002/(sici)1098-108x(199807)24:1<31::aid-eat3>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 11.Killen JD, Hayward C, Wilson DM, Taylor CB, Hammer LD, Litt I, Simmonds B, Haydel F. Factors associated with eating disorder symptoms in a community sample of 11- and 12-year-old girls. Int J Eat Disorders. 1994;15:357–367. doi: 10.1002/eat.2260150406. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell JE, Myers TC, Glass JB. Pharmacotherapy and medical complications of eating disorders in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2002;11(2):365–385. doi: 10.1016/s1056-4993(01)00012-8. [DOI] [PubMed] [Google Scholar]
- 13.Stice E, Shaw H. Eating disorder prevention programs: a meta-analytic review. Psychol Bull. 2004;130(2):206–227. doi: 10.1037/0033-2909.130.2.206. [DOI] [PubMed] [Google Scholar]
- 14.Winzelberg J, Eppstein D, Eldredge KL, Wilfley D, Dasmahapatra R, Dev P, Taylor CB. Effectiveness of an Internet-based program for reducing risk factors for eating disorders. J Consult Clin Psychol. 2000;68:346–350. doi: 10.1037//0022-006x.68.2.346. [DOI] [PubMed] [Google Scholar]
- 15.Celio AA, Winzelberg AJ, Wilfley DE, Eppstein-Harald D, Springer EA, Dev P, Taylor CB. Reducing risk factors for eating disorders: comparison of an Internet- and a classroom-delivered psychoeducation program. J Consult Clin Psychol. 2000;68:650–657. [PubMed] [Google Scholar]
- 16.Zabinski MF, Wilfley DE, Calfas KJ, Winzelberg AJ, Taylor CB. An interactive psychoeducational intervention for women at risk of developing an eating disorder. J Consult Clin Psychol. 2004;72(5):914–919. doi: 10.1037/0022-006X.72.5.914. [DOI] [PubMed] [Google Scholar]
- 17.Jacobi C, Morris L, Bronisch-Holtze J, Winter J, Winzelberg A, Taylor CB. Reduktion von Risikofaktoren für gestörtes Essverhalten: adaptation und erste Ergebnisse eines Internet-gestützten Präventionsprogramms. Zeitschrift für Gesundheitspsychologie. 2005;13:92–101. [Google Scholar]
- 18.Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel F, Hammer LD, Robinson TN, Litt I, Varady A, Kraemer H. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: a three-year prospective analysis. Int J Eat Disorders. 1994;16:227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 19.Killen JD, Taylor CB, Hayward CH, Haydel F, Wilson D, Hammer L, Kraemer H, Blair-Greiner A, Strachowski D. Weight concerns influence the development of eating disorders: A four-year prospective study. J Consult Clin Psychol. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- 20.Jacobi C, Abascal L, Taylor CB. Screening for eating disorders and high risk behavior: Caution. Int J Eat Disorders. 2004;36:273–288. doi: 10.1002/eat.20048. [DOI] [PubMed] [Google Scholar]
- 21.Fairburn CG, Cooper Z. The Eating Disorder Examination (12th edition) In: Fairburn CF, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. New York: The Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 22.Cooper Z, Fairburn C. The Eating Disorder Examination: a semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disorders. 1987;6:1–8. [Google Scholar]
- 23.Rosen JC, Vara L, Wendt S, Leitenberg H. Validity studies of the Eating Disorder Examination. Int J Eat Disorders. 1990;9:519–528. [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 25.Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154(11):1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- 26.Hayward C, Wilson KA, Lagel K, Killen JD, Taylor CB. Parent-reported risk factors for panic attacks. J Am Acad Child Adolescent Dis. 2004;43:613–620. doi: 10.1097/00004583-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 27.McKnight Investigators. Risk factors for the onset of eating disorders in adolescent girls: results of the McKnight Longitudinal Risk Factor Study. Am J Psychiatry. 2003;160:248–254. doi: 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- 28.Garner DM, Olmsted MP. Eating Disorder Inventory Manual. New York: Psychological Assessment Resources; 1984. [Google Scholar]
- 29.Luce KH, Crowther JH. The reliability of the Eating Disorder Examination-Self-Report Questionnaire Version (EDE-Q) Int J Eat Disorders. 1999;25:349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 30.Orme JG, Reis J, Herz EJ. Factorial and discriminant validity of the Center for Epidemiological Studies Depression (CES-D) scale. J Clin Psychol. 1986:28–33. doi: 10.1002/1097-4679(198601)42:1<28::aid-jclp2270420104>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 31.Plutchik R, van Praag HM. Interconvertability of five self-report measures of depression. Psychiatry Res. 1987;22(3):243–256. doi: 10.1016/0165-1781(87)90039-4. [DOI] [PubMed] [Google Scholar]
- 32.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 33.Clara IP, Cox BJ, Enns MW, Murray LT, Torgrudc LJ. Confirmatory factor analysis of the multidimensional scale of perceived social support in clinically distressed and student samples. J Pers Assess. 2003;81(3):265–270. doi: 10.1207/S15327752JPA8103_09. [DOI] [PubMed] [Google Scholar]
- 34.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 35.Cash TF. Body image therapy: A program for self-directed change. New York: Guilford Press; 1991. [Google Scholar]
- 36.Celio CI, Luce KH, Bryson SW, Cunning D, Rockwell R, Wilfley D, Taylor CB. Use of diet pills and other dieting aids in a college population with high weight and shape concerns. Int J Eat Dis. doi: 10.1002/eat.20254. In press. [DOI] [PubMed] [Google Scholar]
- 37.Stice E, Killen JD, Hayward C, Taylor CB. Support for the continuity hypothesis of bulimic pathology. JCCP. 1998;66:784–790. [PubMed] [Google Scholar]
- 38.Fitzgibbon ML, Sanchez-Johnsen LA, Martinovich Z, et al. A test of the continuity perspective across bulimic and binge eating pathology. Int J Eat Disord. 2003;34:83–97. doi: 10.1002/eat.10160. [DOI] [PubMed] [Google Scholar]
- 39.Sobell MB, Sobell LC, Klainer F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students' recent drinking history: utility for alcohol research. Add Beh. 1986;11(2):149–161. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- 40.Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. JCCP. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 41.Ravaldi C, Vannacci A, Truglia E, Zucchi T, Mannucci E, Rotella CM, Faravelli C, Ricca V. The Eating Disorder Examination as a retrospective interview. Eat Weight Disord. 2004;9(3):228–231. doi: 10.1007/BF03325072. [DOI] [PubMed] [Google Scholar]
- 42.Taylor CB, Cameron R, Newman M, Junge J. Issues related to combining risk factor reduction and clinical treatment for eating disorders in defined populations. J Beh Health Services Res. 2002;29:81–90. doi: 10.1007/BF02287835. [DOI] [PubMed] [Google Scholar]