Abstract
In vitro activity of ozenoxacin, a novel nonfluorinated topical (L. D. Saravolatz and J. Leggett, Clin. Infect. Dis. 37:1210–1215, 2003) quinolone, was compared with the activities of other quinolones against well-characterized quinolone-susceptible and quinolone-resistant Gram-positive bacteria. Ozenoxacin was 3-fold to 321-fold more active than other quinolones. Ozenoxacin could represent a first-in-class nonfluorinated quinolone for the topical treatment of a broad range of dermatological infections.
TEXT
Antibiotic resistance remains a major public health threat worldwide (1, 2). Gram-positive bacteria, particularly Gram-positive cocci, are important pathogens in both hospital and community environments. They are associated mainly with bacteremia, pneumonia, and skin and soft tissue infections (SSTIs) (3). Nowadays, the incidence of both hospital- and community-acquired methicillin-resistant Staphylococcus aureus (MRSA) presents therapeutic problems in many countries (4, 5).
Fluoroquinolones, an alternative therapeutic option, have shown good activity against Gram-positive bacteria, including methicillin-susceptible S. aureus (MSSA) and MRSA. However, the emergence of resistant strains has compromised the clinical usefulness of quinolones currently available for the treatment of staphylococcal infections (3, 5, 6). The emergence of resistance has made it necessary to design new drugs for the treatment of infections caused by resistant strains.
Ozenoxacin (Fig. 1), 1-cyclopropyl-8-methyl-7-[5-methyl-6-(methylamino)-3-pyridinyl]-4-oxo-1,4-dihydro-3-quinolinecarboxylic acid (Ferrer Laboratories), belongs to a new generation of nonfluorinated quinolone antibacterials, having a pyridinyl group at C-7. Developed for topical use, it has recently successfully completed a phase III clinical trial with adult and pediatric patients with impetigo. Ozenoxacin has demonstrated excellent in vitro activity against MRSA and methicillin-resistant Staphylococcus epidermidis (MRSE), including quinolone-resistant strains (7, 8).
Fig 1.
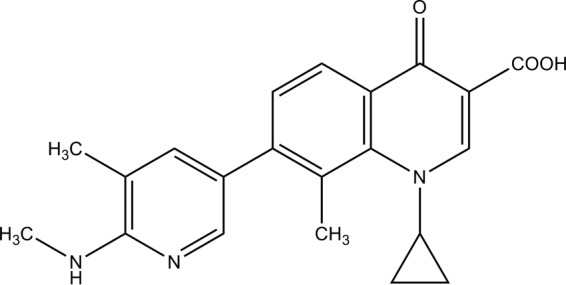
Structure of ozenoxacin.
In this study, the in vitro activity of ozenoxacin was compared to those of moxifloxacin, levofloxacin, and ciprofloxacin against both quinolone-susceptible and quinolone-resistant Gram-positive bacteria with well-characterized resistance mechanisms.
(Part of this work was presented at the 52nd Interscience Conference on Antimicrobial Agents and Chemotherapy, San Francisco, CA, 9 to 12 September 2012.)
A total of 50 quinolone-susceptible (QS) and quinolone-resistant (QR) Gram-positive cocci strains collected between 2009 and 2010 were studied. The clinical isolates were obtained from the Clinical Microbiology Laboratory at the Hospital Clínic in Barcelona, Spain. The strains included methicillin-susceptible S. aureus (n = 9), methicillin-resistant S. aureus (n = 5), methicillin-susceptible S. epidermidis (n = 8), methicillin-resistant S. epidermidis (n = 5), Streptococcus pyogenes (n = 8), Streptococcus agalactiae (n = 8), and Enterococcus faecium (n = 6). S. aureus ATCC 25923 was used as a control microorganism. All strains were grown aerobically at 37°C in brain heart infusion broth (BHI) (Becton, Dickinson Co., Sparks, MD).
Susceptibilities to ozenoxacin (OZN) (Ferrer Laboratories), moxifloxacin (MXF), levofloxacin (LVX), and ciprofloxacin (CIP) (Sigma-Aldrich, St. Louis, MO) were determined using broth microdilution according to the CLSI standard method (9). The MIC of each antimicrobial agent was determined in the presence and absence of 25 mg/liter of the efflux pump inhibitor reserpine (Sigma, St. Louis, MO). CLSI breakpoints were used to classify strains as QS or QR. If one of the strains was found to be resistant to LVX and MXF, it was allocated to the QR group, although they were susceptible to the remaining fluoroquinolones. The quinolone resistance-determining regions (QRDRs) of the gyrA, gyrB, parC, and parE genes were amplified by PCR using a set of previously described primers (10–14).
An analysis of the relationship between the MICs of the different quinolones tested and mutations in the QRDRs found in all of the strains studied is shown in Tables 1 and 2.
Table 1.
Distribution of different fluoroquinolone MICs in staphylococcus strains and QDRD amino acid substitutions responsible for elevated fluoroquinolone MICsa
| Organism and isolate no. | MIC (mg/liter) |
Amino acid substitution(s) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OZN |
MXF |
LVX |
CIP |
|||||||
| −R | +R | −R | +R | −R | +R | −R | +R | GyrA | ParC | |
| MSSA-QS | ||||||||||
| 361 | 0.008 | 0.002 | 0.25 | 0.25 | 2 | 2 | 0.25 | 0.25 | Ser84Leu | NM |
| 172 | 0.008 | 0.002 | 0.25 | 0.06 | 0.25 | 0.25 | 0.25 | 0.25 | Ser84Leu | NM |
| 89.01 | 0.008 | 0.002 | 0.06 | 0.06 | 0.5 | 0.5 | 2 | 2 | NM | Ser87Leu |
| MSSA-QR | ||||||||||
| 330 | 0.12 | 0.002 | 8 | 8 | 16 | 16 | 64 | 64 | Ser84Leu | NM |
| 144 | 0.12 | 0.12 | 4 | 4 | 32 | 32 | 16 | 16 | Ser84Leu | NM |
| 440 | 0.12 | 0.12 | 32 | 32 | 64 | 64 | 64 | 64 | Ser84Leu | NM |
| 847 | 0.5 | 0.5 | 8 | 4 | 32 | 32 | 128 | 128 | Ser84Leu | NM |
| 176 | 0.5 | 0.5 | 16 | 2 | 64 | 64 | 256 | 256 | Ser84Leu/Ser85Pro | NM |
| 51 | 2 | 2 | 64 | 32 | 64 | 64 | 256 | 128 | Ser84Leu/Ser85Pro | Ser80Tyr/Glu84Gly |
| MRSA-QR | ||||||||||
| 108 | 0.06 | 0.002 | 2 | 2 | 16 | 16 | 16 | 16 | Ser84Leu | NM |
| 50 | 0.06 | 0.002 | 32 | 32 | 128 | 64 | 16 | 16 | Ser84Leu | NM |
| 908 | 0.12 | 0.12 | 4 | 4 | 16 | 16 | 64 | 64 | Ser84Leu | NM |
| 823 | 0.12 | 0.12 | 32 | 32 | 64 | 64 | 256 | 256 | Ser84Leu | NM |
| 126 | 2 | 2 | 32 | 32 | 512 | 256 | 256 | 256 | Ser84Leu/Glu88Lys | Ser80Phe/Glu84Val |
| MSSE-QR | ||||||||||
| 67 | 0.5 | 0.5 | 32 | 16 | 32 | 32 | 16 | 16 | Ser84Phe | Ser80Phe |
| 58 | 1 | 1 | 32 | 16 | 64 | 64 | 64 | 64 | Ser84Phe | Ser80Phe |
| 30 | 1 | 1 | 32 | 16 | 64 | 64 | 64 | 64 | Ser84Tyr/Glu88Lys | Ser80Phe/Asp84Tyr |
| 56 | 2 | 2 | 64 | 32 | 512 | 512 | 128 | 128 | Ser84Phe/Glu88Lys | Ser80Phe |
| MRSE-QS | ||||||||||
| FG015 | 0.004 | 0.002 | 0.12 | 0.06 | 0.25 | 0.12 | 0.25 | 0.25 | NM | NM |
| 7602 | 0.03 | 0.008 | 0.06 | 0.06 | 0.5 | 0.25 | 1 | 0.5 | NM | NM |
| 12 | 0.06 | 0.06 | 0.5 | 0.12 | 0.5 | 0.5 | 1 | 0.5 | NM | NM |
| 69.02 | 0.03 | 0.015 | 1 | 1 | 2 | 2 | 2 | 2 | Ser84Phe | NM |
| MRSE-QR | ||||||||||
| FG012 | 0.12 | 0.12 | 2 | 2 | 32 | 32 | 128 | 128 | Ser84Phe | Ser80Phe |
| FG014 | 1 | 0.5 | 16 | 16 | 128 | 128 | 64 | 64 | Ser84Tyr/Glu88Gly | Ser80Phe/Asp84Tyr |
| FG013 | 2 | 1 | 32 | 32 | 512 | 512 | 128 | 128 | Ser84Tyr/Glu88Lys | Ser80Phe/Asp84Tyr |
| FG011 | 2 | 2 | 32 | 32 | 256 | 128 | 32 | 4 | Ser84Tyr/Glu88Lys | Ser80Phe/Asp84Tyr |
| 31 | 2 | 2 | 64 | 16 | 128 | 128 | 64 | 32 | Ser84Tyr/Glu88Lys | Ser80Phe/Asp84Tyr |
R, reserpine; QS, quinolone susceptible; QR, quinolone resistant; NM, no mutations in the gyrA and parC genes.
Table 2.
Distribution of different fluoroquinolone MICs in streptococcus and enterococcus strains and amino acid substitutions responsible for elevated fluoroquinolone MICsa
| Organism and isolate no. | MIC (mg/liter) |
Amino acid substitution(s) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OZN |
MXF |
LVX |
CIP |
|||||||
| −R | +R | −R | +R | −R | +R | −R | +R | GyrA | ParC | |
| S. pyogenes (QS) | ||||||||||
| 017 | 0.03 | 0.015 | 0.25 | 0.25 | 0.5 | 0.5 | 0.5 | 0.12 | NM | NM |
| 117 | 0.03 | 0.015 | 0.12 | 0.12 | 0.5 | 0.5 | 0.5 | 0.12 | NM | NM |
| 39 | 0.03 | 0.015 | 0.12 | 0.12 | 0.5 | 0.12 | 0.5 | 0.12 | NM | NM |
| 016 | 0.12 | 0.12 | 0.12 | 0.06 | 0.5 | 0.12 | 2 | 1 | NM | NM |
| S. pyogenes (QR) | ||||||||||
| 165 | 0.12 | 0.12 | 1 | 0.06 | 16 | 0.06 | 4 | 2 | NM | NM1 |
| 170 | 0.12 | 0.12 | 1 | 1 | 8 | 8 | 8 | 8 | NM | NM |
| 168 | 0.25 | 0.12 | 2 | 0.06 | 8 | 0.015 | 4 | 2 | Ser81Phe | NM |
| 166 | 0.25 | 0.25 | 4 | 4 | 16 | 8 | 16 | 16 | Ser81Phe | Ser79Phe |
| S. agalactiae (QS) | ||||||||||
| 283 | 0.03 | 0.03 | 0.25 | 0.25 | 1 | 1 | 0.5 | 0.25 | NM | NM |
| 536 | 0.03 | 0.03 | 0.25 | 0.25 | 1 | 1 | 1 | 0.25 | NM | NM |
| 420 | 0.03 | 0.03 | 0.25 | 0.25 | 1 | 1 | 0.5 | 0.25 | NM | NM |
| 146 | 0.06 | 0.03 | 0.25 | 0.25 | 2 | 1 | 0.25 | 0.25 | NM | NM |
| S. agalactiae (QR) | ||||||||||
| 159 | 0.5 | 0.5 | 4 | 4 | 32 | 32 | 64 | 32 | NM | Ser79Phe |
| 155 | 0.5 | 0.5 | 4 | 4 | 32 | 32 | 64 | 32 | Ser81Leu | Ser79Phe |
| 156 | 1 | 1 | 8 | 8 | 64 | 64 | 64 | 32 | Ser81Leu | Ser79Phe |
| 157 | 1 | 1 | 8 | 8 | 64 | 64 | 128 | 32 | Ser81Leu | Ser79Phe |
| E. faecium (QS) | ||||||||||
| 29.01 | 0.06 | 0.06 | 0.5 | 0.5 | 2 | 2 | 1 | 1 | NM | Ser80Ile |
| 897 | 0.25 | 0.25 | 0.5 | 0.5 | 2 | 2 | 1 | 1 | NM | Ser80Ile |
| E. faecium (QR) | ||||||||||
| 531 | 0.5 | 0.5 | 2 | 2 | 4 | 2 | 8 | 8 | NM | Ser80Ile |
| 454 | 2 | 2 | 32 | 32 | 128 | 64 | 512 | 512 | Ser83Ile | Ser80Ile |
| 075 | 4 | 4 | 64 | 32 | 128 | 32 | 512 | 512 | Ser83Ile | Ser80Ile |
| 59.02 | 4 | 4 | 64 | 32 | 128 | 64 | 256 | 256 | Ser83Ile | Ser80Ile |
R, reserpine; QS, quinolone susceptible; QR, quinolone resistant; NM, no mutations in the gyrA and parC genes.
Overall, OZN showed the highest antibacterial activities against clinical isolates of Gram-positive microorganisms, with MICs ranging from 0.008 to 4 mg/liter. The good activities of OZN against strains of MRSA, MSSA, MSSE, and MRSE with 2, 3, or 4 mutations in the gyrA and grlA (parC) genes is worthy of note.
Two groups of MSSA strains were established: (i) MSSA strains with a mutation in the amino acid codon Ser84 of the gyrA gene and MICs of CIP, MXF, and LVX of between 0.25 and 2 mg/liter (the MIC of OZN was 0.008 mg/liter) and (ii) MSSA strains with the same gyrA mutation but MICs of CIP, MXF, and LVX ranging from 4 to 128 mg/liter. The MICs of the above-mentioned fluoroquinolones against strains with MICs of >4 mg/liter remained the same in the presence of reserpine. This may be due to the overexpression of an unknown reserpine-inhibited efflux pump. The MIC of OZN for MRSA strains with a mutation at the amino acid codon Ser84 was between 0.06 and 0.12 mg/liter, whereas the range of MICs of the other fluoroquinolones was between 2 and 256 mg/liter. It should be noted that the MIC of OZN of a MRSA strain with four mutations, two in the gyrA gene and two in the parC genes (Ser84 → Tyr/Glu88 → Lys and Ser80 → Phe/Glu84 → Val), was 2 mg/liter. The MICs of MXF, CIP, and LVX were 32 mg/liter, 256 mg/liter, and 512 mg/liter, respectively.
Our results are similar to those described by Yamakawa et al. (15), who showed that the MIC of T-3912 (now OZN) against quinolone-resistant MSSA with 2 or 3 mutations in these genes was 0.06 or 0.25 mg/liter, respectively, compared with the MICs of between 0.12 and 2 mg/liter found in the present study. The effects of the different mutations in the gyrA and grlA genes on the MIC of OZN were similar for MRSA and MRSE.
In vitro activities of nemonoxacin, another nonfluorinated quinolone, was tested against clinical isolates of S. aureus, enterococci, and Streptococcus pneumoniae by Chen et al. (16). These authors found that nemonoxacin had a potent activity against MSSA and CIP-susceptible MRSA (MIC90 of ≤0.03 mg/liter), whereas activity was limited against CIP-resistant MRSA (MIC90 of 1 mg/liter). No reference was made, however, to mutations in the gyrA and/or grlA genes in these last strains.
Fluoroquinolone-resistant MSSE strains with a double mutation in gyrA (Ser84 → Phe) and parC (Ser80 → Phe) showed a MIC of OZN of 0.5 to 1 mg/liter. This was 16-fold to 64-fold lower than those of MXF, LVX, and CIP. Four groups were established when studying MRSE strains. (i) Three QS-MRSE strains had no mutation in the gyrA or parC genes; the MICs of OZN for these strains ranged from 0.004 to 0.06 mg/liter, whereas the MICs of the remaining quinolones ranged between 0.06 and 1 mg/liter. (ii) One QS-MRSE strain had a mutation in gyrA (Ser84 → Phe), which showed a MIC of OZN of 0.03 mg/liter. (iii) One QS-MRSE strain had a double mutation (Ser84 → Phe in gyrA and Ser80 → Phe in parC) and a MIC of OZN of 0.03 mg/liter. The MIC of OZN of the strain in group ii, however, was reduced to 0.015 mg/liter in the presence of reserpine, suggesting that this strain possesses two concomitant mechanisms of resistance, an amino acid substitution in gyrA plus an overexpression of a reserpine-inhibited efflux pump. (iv) Four QR-MRSE strains that had double mutations in gyrA (Ser80 → Tyr/Glu88 → Gly or Glu88 → Lys) and parC (Ser80 → Phe/Asp84 → Tyr) showed a MIC of OZN of 1 to 2 mg/liter. This was at least 8-, 16-, and 64-fold higher than MICs of MXF, CIP, and LVX, which were 16 to 64 mg/liter, 32 to 128 mg/liter, and 128 to 256 mg/liter, respectively.
Although the prevalence of fluoroquinolone-resistant S. pyogenes and S. agalactiae is still low, it has been steadily increasing (13, 17). Two S. pyogenes strains (165 and 168) showed reduced MICs of MXF, LVX, and CIP in the presence of reserpine, whereas the MIC of OZN was not affected, thus suggesting the overexpression of a reserpine-inhibited efflux pump which does not affect OZN. As regards the S. pyogenes and S. agalactiae strains with mutations in both gyrA and parC, the effect of these mutations on the MIC of OZN seems greater in S. agalactiae than in S. pyogenes, with MICs of 1 and 0.25 mg/liter, respectively. The effect on the fluoroquinolones tested was similar to that reported in other studies (18). Finally, the MIC values of OZN for E. faecium were greater than those for other microorganisms due to the high level of resistance present in Enterococcus spp., which has been associated with many antibiotics with their intrinsic resistance and/or other resistance mechanisms (18). In the study described by Chen et al. (16), the MIC90s of nemonoxacin for vancomycin-susceptible and vancomycin-resistant E. faecium were 4 and 16 mg/liter, respectively, with the MICs ranging from 0.06 to 8 mg/liter and 0.06 to 16 mg/liter. However, those authors did not describe mutations in the strains studied. In our study, strains with double mutations presented a MIC of OZN from 2 to 4 mg/liter.
In conclusion, OZN shows excellent in vitro activity against the most important microorganisms isolated as etiological agents in SSTIs, even against methicillin-resistant strains and those with 2, 3, or 4 mutations in the gyrA and/or parC genes.
ACKNOWLEDGMENTS
The study was carried out with a research grant from Ferrer International S.A. (Barcelona, Spain). This study was supported by grant 2009-SGR1256 from the Departament de Universitats, Recerca I Societat de la Informació de la Generalitat d'Catalunya, and by the Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III, Spanish Network for Research in Infectious Diseases (REIPI RD12/0015) and FIS 11/02024.
Fernando Garcia-Alonso and Domingo Gargallo-Viola are staff members of Ferrer Laboratories. The remaining authors declare no conflicts of interest.
Footnotes
Published ahead of print 30 September 2013
REFERENCES
- 1. Almer LS, Hoffrage JB, Keller EL, Flamm RK, Shortridge VD. 2004. In vitro and bactericidal activities of ABT-492, a novel fluoroquinolone, against Gram-positive and Gram-negative organisms. Antimicrob. Agents Chemother. 48:2771–2777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhang R, Eggleston K, Rotimi V, Zeckhauser RJ. 2006. Antibiotic resistance as a global threat: evidence from China, Kuwait and the United States. Global Health 2:6. 10.1186/1744-8603-2-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Maina EK, Kiiyukia C, Wamae CN, Waiyaki PG, Kariuki S. 2013. Characterization of methicillin-resistant Staphylococcus aureus from skin and soft tissue infections in patients in Nairobi, Kenya. Int. J. Infect. Dis. 17:e115–9. 10.1016/j.ijid.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 4. Rice LB. 2006. Antimicrobial resistance in gram-positive bacteria. Am. J. Med. 119(6 Suppl 1):S11–S19 [DOI] [PubMed] [Google Scholar]
- 5. Bhagwat SS, McGhee P, Kosowska-Shick K, Patel MV, Appelbaum PC. 2009. In vitro activity of the quinolone WCK 771 against recent U.S. hospital and community-acquired Staphylococcus aureus pathogens with various resistance types. Antimicrob. Agents Chemother. 53:811–813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saravolatz LD, Leggett J. 2003. Gatifloxacin, gemifloxacin, and moxifloxacin: the role of 3 newer fluoroquinolones. Clin. Infect. Dis. 37:1210–1215 [DOI] [PubMed] [Google Scholar]
- 7. Wiles JA, Bradbury BJ, Pucci MJ. 2010. New quinolone antibiotics: a survey of the literature from 2005 to 2010. Expert Opin. Ther. Pat. 20:1295–1319 [DOI] [PubMed] [Google Scholar]
- 8. López Y, Tato M, Cantón R, Vila J. 2012. Abstr. 52nd Intersci. Conf. Antimicrob. Agents Chemother., abstr C1-682. [Google Scholar]
- 9. Clinical and Laboratory Standards Institute 2012. Performance standards for antimicrobial susceptibility testing: 21st international supplement. M100-S21 Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 10. Sierra JM, Marco F, Ruiz J, Jiménez de Anta MT, Vila J. 2002. Correlation between the activity of different fluoroquinolones and the presence of mechanisms of quinolone resistance in epidemiologically related and unrelated strains of methicillin-susceptible and -resistant Staphylococcus aureus. Clin. Microbiol. Infect. 8:781–790 [DOI] [PubMed] [Google Scholar]
- 11. Yamada M, Yoshida J, Hatou S, Yoshida T, Minagawa Y. 2008. Mutations in the quinolone resistance determining region in Staphylococcus epidermidis recovered from conjunctiva and their association with susceptibility to various fluoroquinolones. Br. J. Ophthalmol. 92:848–851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Billal DS, Fedorko DP, Yan SS, Hotomi M, Fujihara K, Nelson N, Yamanaka N. 2007. In vitro induction and selection of fluoroquinolone-resistant mutants of Streptococcus pyogenes strains with multiple emm types. J. Antimicrob. Chemother. 59:28–34 [DOI] [PubMed] [Google Scholar]
- 13. Biedenbach DJ, Toleman MA, Walsh TR, Jones RN. 2006. Characterization of fluoroquinolone-resistant beta-hemolytic Streptococcus spp. isolated in North America and Europe including the first report of fluoroquinolone-resistant Streptococcus dysgalactiae subspecies equisimilis: report from the SENTRY Antimicrobial Surveillance Program (1997–2004). Diagn. Microbiol. Infect. Dis. 55:119–127 [DOI] [PubMed] [Google Scholar]
- 14. Oyamada Y, Ito H, Fujimoto K, Asada R, Niga T, Okamoto R, Inoue M, Yamagishi J. 2006. Combination of known and unknown mechanisms confers high-level resistance to fluoroquinolones in Enterococcus faecium. J. Med. Microbiol. 55(Part 6):729–736 [DOI] [PubMed] [Google Scholar]
- 15. Yamakawa T, Mitsuyama J, Hayashi K. 2002. In vitro and in vivo antibacterial activity of T-3912, a novel non-fluorinated topical quinolone. J. Antimicrob. Chemother. 49:455–465 [DOI] [PubMed] [Google Scholar]
- 16. Chen YH, Liu CY, Lu JJ, King CHR, Hsueh PR. 2009. In vitro activity of nemonoxacin (TG-873870), a novel non-fluorinated quinolone, against clinical isolates of Staphylococcus aureus, enterococci and Streptococcus pneumoniae with various resistance phenotypes in Taiwan. J. Antimicrob. Chemother. 64:1226–1229 [DOI] [PubMed] [Google Scholar]
- 17. Ki M, Srinivasan U, Oh KY, Kim MY, Shin JH, Hong HL, Dang T, Britt Z, Foxman B. 2012. Emerging fluoroquinolone resistance in Streptococcus agalactiae in South Korea. Eur. J. Clin. Microbiol. Infect. Dis. 31:3199–3205 [DOI] [PubMed] [Google Scholar]
- 18. Arai K, Hirakata Y, Yano H, Kanamori H, Endo S, Hirotani A, Abe Y, Nagasawa M, Kitagawa M, Aoyagi T, Hatta M, Yamada M, Nishimaki K, Takayama Y, Yamamoto N, Kunishima H, Kaku M. 2011. Emergence of fluoroquinolone-resistant Streptococcus pyogenes in Japan by a point mutation leading to a new amino acid substitution. J. Antimicrob. Chemother. 66:494–498 [DOI] [PubMed] [Google Scholar]


