Abstract
An increasing number of adolescents born with HIV in South Africa are on antiretroviral treatment and have to confront complex issues related to coping with a chronic, stigmatizing and transmittable illness. Very few evidence-based mental health and health promotion programs for this population exist in South Africa. This study builds on a previous collaboratively designed and developmentally-timed family-based intervention for early adolescents (CHAMP). The study uses community-based participatory approach as part of formative research to evaluate a pilot randomized control trial at two hospitals. The paper reports on the development, feasibility and acceptability of the VUKA family-based program and its short-term impact on a range of psychosocial variables for HIV+ pre-adolescents and their caregivers. A ten session intervention of approximately 3 months duration was delivered to 65 pre-adolescents aged 10-13 years and their families. VUKA participants were noted to improve on all dimensions, including mental health, youth behaviour, HIV treatment knowledge, stigma, communication and adherence to medication. VUKA shows promise as a family-based mental and HIV prevention program for HIV+ pre-adolescents and which could be delivered by trained lay staff.
Keywords: Family-based, Psychosocial intervention, Mental health, HIV+ adolescents
Introduction
In 2009, an estimated 334,000 children living with HIV in South Africa were primarily infected perinatally (Republic of South Africa, 2010). With significantly greater access to antiretroviral treatment (ART), children previously not expected to survive childhood will reach adolescence in significant numbers, with improved clinical and nutritional status (Sutcliff, van Dijk, Bolton, Persaud, & Moss, 2008).
Nonetheless, adolescents born with HIV/AIDS continue to face a stigmatizing and chronic illness (Havens & Mellins, 2008) and have to learn to cope with the effect of HIV on normative developmental challenges, including pubertal delays (Buchacz et al., 2003), neurodevelopmental and cognitive problems (Brackis-Cott, Kang, Dolezal, Abrams, & Mellins, 2009; Nozyce et al., 2006), and a tendency for greater social and emotional immaturity relative to same age peers (Donenberg & Pao, 2005). In addition, they experience multiple family disruptions due to caregiver illness, death, or substance use (Domek, 2010; Havens & Mellins, 2008). These factors may result in poor impulse control or judgment and increased possibility of negative peer relations and early or riskier sexual experimentation (Havens & Mellins, 2008).
Evidence from high-resource settings indicates that as children with HIV enter adolescence they are also at significant risk for mental health problems and substance use (Havens & Mellins, 2008; Mellins et al., 2009; Mellins et al., 2012; Mellins et al., 2011). Although limited, research in African countries, including South Africa, suggests that youth living with perinatal HIV-infection (YLWPHIV) may be equally, if not more, vulnerable to behavioral and emotional problems than comparison controls (Cluver, Orkin, Gardner, & Boyes, 2012; Domek, 2010). South Africa is at the forefront of providing ART but is challenged to meet the complex needs of increasing numbers of adolescents who must now cope with HIV as a chronic, highly stigmatized, and transmittable illness (Domek, 2010; Ledlie, 2001). The challenges adolescents face with non-adherence to medical treatment are compounded for YLWPHIV by HIV stigma, ART side effects, life-long need for medication (Haberer et al., 2010; Mills et al., 2006), sexual development and behavior compromised by early and lifetime exposure to HIV and treatment (Bauermeister, Elkington, Robbins, Kang, & Mellins, 2011), and widespread poverty in sub-Saharan Africa (Reisner et al., 2009).
While families remain the mainstay of providing protection and care for children in sub-Saharan Africa, the loss of many adult caregivers to HIV/AIDS and widespread poverty may compromise the family’s ability to meet the needs of children living with HIV/AIDS (Heymann & Kidman, 2009). Parents may experience feelings of chronic sorrow, fears that HIV/AIDS, stigma, and discrimination will negatively impact their child’s health, mortality, and future, and concern about when to disclose HIV to the child (Antle, Wells, Goldie, DeMatteo, & King, 2001).
Psychosocial Programs for Youth Living with Perinatal HIV
While there are programs that have been developed for YLWPHIV, including family social support (Abramowitz et al., 2009), psycho-educational intervention (Bacha, Pomeroy, & Gilbert, 1999), multi-systemic therapy for children living with HIV (Ellis, Naar-King, Cunningham, & Secord, 2006), and more general clinical interventions (Rogers, Miller, Murphy, Tanney, & Fortune, 2001), there are few evidence-based interventions to support families in promoting the health and psychosocial well-being of children and adolescents born with HIV, and even fewer that are not resource intensive and have been tailored to the particular cultural context and needs of adolescents in low-and-middle-income countries (Domek, 2010; Petersen et al., 2010).
The Collaborative HIV prevention and Adolescent Mental Health Family Program (CHAMP) is a developmentally-timed, multi-session, family-based intervention that has been adapted and implemented with HIV- youth in South Africa (CHAMPSA) and with YLWPHIV in the US (CHAMP+US) (Bhana, McKay, Mellins, Petersen, & Bell, 2010; Domek, 2010; McKay & Paikoff, 2007). Multiple randomized controlled trials (RCTs) of CHAMP and a pilot RCT of CHAMP+US have shown that the intervention results in significant improvements in family process variables (e.g., communication, supervision, monitoring, and support) and youth mental health and risk behaviors (e.g., improved externalizing behaviors; less time spent in risky situations), and family and child medication adherence support, with high acceptability by caregivers and youth (Bell et al., 2008; Bhana et al., 2010; McKay & Paikoff, 2007; McKay et al., 2004; Mellins, Brackis-Cott, Dolezal, & Abrams, 2004).
The VUKA Family Intervention
A multi-disciplinary team of physicians, nurses, psychologists, lay counselors, and researchers, together with patients, South African artists, and educators/curriculum developers, reviewed existing CHAMP, CHAMP+, and CHAMPSA materials and conducted formative qualitative interviews with adolescent youth and caregivers to adapt the CHAMP model for YLWPHIV in South Africa (Petersen et al., 2010). In addition to issues related to negative peer influences and poor financial, family and social support, specific psychosocial problems and challenges particular to YLWPHIV and their caregivers emerged in interviews (Petersen et al., 2010). These included unfulfilled bereaving at the loss of biological parents, difficulty accepting and dealing with identity and status issues related to living with HIV, high external stigma, discrimination and disclosure, and difficulties in understanding ART and adherence (Mellins et al., 2012; Petersen et al., 2010). Participant feedback also suggested caregiver-youth difficulty discussing topics such as sexual behavior and loss and bereavement. The revised intervention retained the overall CHAMP structure (multiple child-caregiver pairs) and the use of a cartoon-based storyline (Petersen, Mason, Bhana, Bell, & McKay, 2006) from CHAMPSA, with an altered curriculum to accommodate the unique needs of YLWPHIV. Patient and provider community advisors renamed the intervention “VUKA” (“Let’s wake up” in isiZulu).
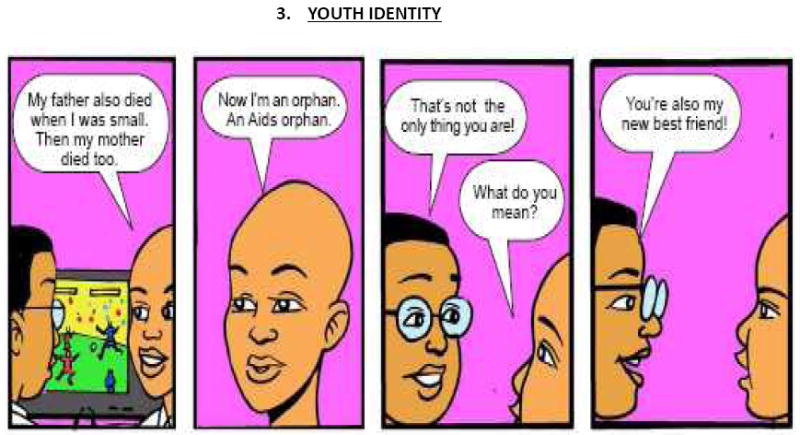
A new culturally-tailored cartoon storyline and curriculum enabled lay counselors supervised by a psychologist to deliver the intervention in an engaging and structured way. The cartoon storyline tells the story of a 12-year-old boy, orphaned by AIDS, who moves in with relatives and learns about his own HIV diagnosis and treatment needs, while coping with family loss, stigma, peer relationships, identity, and family functioning (see Figure 1 for examples). The curriculum provides step-by-step guidance for counselors to deliver critical information to facilitate discussions and problem-solving within and between families in multi-family groups. Session topics include: (1) AIDS-related loss and bereavement; (2) HIV transmission and treatment knowledge; (3) Disclosure of HIV status to others; (4) Youth identity, acceptance and coping with HIV; (5) Adherence to medical treatment; (6) Stigma and discrimination; (7) Caregiver-child communication, particularly on sensitive topics such as puberty and HIV; (8) Puberty; (9) Identifying and developing strategies to keep children safe in high-risk situations where sexual behavior and drug use are possible; and (10) Social support. As with the original CHAMP intervention program, HIV-infected youth and their primary caregiver come together with other affected families for sessions, which include both multiple family group activities and separate parent and child group activities.
Figure 1.


A pilot RCT of VUKA was conducted to examine the 1) development, feasibility and acceptability of VUKA for health care settings in South Africa and 2) short-term impact of the VUKA family program on a range of psychosocial variables for YLWPHIV and their caregivers.
Methods
Participants and Procedure
The VUKA Family Program was developed and piloted at two clinical sites in KwaZulu-Natal, South Africa: a) a subsidized not-for-profit hospital in Durban with a dedicated clinic serving adults and children with HIV/AIDS and b) a Department of Health regional- and district-level public hospital located in Pietermaritzburg, approximately 100km from Durban, that primarily serves low-income patients and is a primary treatment site for the rollout of ART in KwaZulu-Natal. Both sites afford subsidized or free treatment and represent typical treatment scenarios for YLWPHIV in South Africa.
Caregivers approached in clinic waiting rooms were referred to the study project director (fluent in both English and isiZulu) if they expressed interest and had a child who met study criteria. Inclusion criteria included: a) Child 10-14 years old; b) Child enrolled in HIV care at the hospital; and c) Child aware of his/her HIV status. Families were enrolled only if both the caregiver and child provided written consent and assent. Among the 74 families enrolled, 65 families completed a baseline assessment and were then randomly assigned to receive VUKA immediately (n=33) or approximately three months later, after both groups had completed a post-evaluation (comparison group; n=32). The comparison group data presented here was collected prior to their receiving VUKA.
The intervention was administered in 6 sessions over a 3-month period (2 Saturdays a month) based on participant and provider feedback concerning feasibility and space. Intervention facilitators were primarily lay counselors and one masters-level psychologist, who also provided supervision after initial training by the study team. All participants were assessed at two time points, at baseline and approximately two weeks after the last intervention session (approximately 3 months after baseline); 59 families (91% of participants) completed the post-test assessment. South African and US institutional review boards, including the hospitals involved in the project, approved the study. Self-administered questionnaires were translated into isiZulu using standard procedures for translation and back-translation (Preciago & Henry, 1997; Tanzer & Sim, 1999). Participants completed research questionnaires (1 hour sessions) in small groups (youth and caregivers separately), with questionnaires read-aloud by trained research staff. These procedures have been used successfully with children as young as nine years old (Bell et al., 2008; Mellins et al., 2004).
During the evaluation sessions, participants were encouraged to express their level of comfort with the topic under discussion to ensure that children were not experiencing high levels of distress in relation to the questions asked. Training explicitly included sensitivity to such issues with the involvement of a supervising psychologist. However, no such instances were reported. Using a cartoon-based story-line assisted in lending distance to sensitive issues and negative life events. In addition, a referral system was put into place to ensure that any participants in need of further counselling could access such services.
Measures
A summary table of the measures used is presented below.
| Descriptor | Inter-item reliability (pre- and post-test) | Measures | Construct |
| Youth Adherence to ART | Single items | Derived from Pediatric AIDS Clinical Trials Group (Mellins et al., 2006; Usitalo et al., 2010) | How often medications missed over past 6 months |
| Youth Mental Health | .42 to .54 | Strengths and Difficulties Questionnaire (Goodman, 1997; Youth in Mind, 2012) | Emotional symptoms, conduct, peer relations. Hyperactivity/inattentiveness, prosocial behavior |
| Child Depression | .54 | Child Depression Inventory (Kovacs, 1981) | Depression symptoms |
| Self-Concept | .70 to .58 | Tennessee Self-Concept Scale-Short Form (Fitts & Warren, 1996) | Self-identity, self-satisfaction, self-esteem |
| Youth HIV Treatment Knowledge | .65 to .74 | HIV Treatment Knowledge (Levy, Lampman, Handler, Flay, & Weeks, 1993) | HIV causality, transmission, treatment |
| Youth and Caregiver Communication and Comfort | .88 to .73 | Family Environment Scale/Family Assessment Measure (FES/FAM) (Bell et al., 2008) | Comfort and communication around hard to talk about issues |
| HIV/AIDS Illness Stigma | .82 to .67 | Stigma (Westbrook, Bauman, & Shinnar, 1992) | Perceived stigma, disclosure and self-esteem |
Analysis
Quantitative Analysis
Generalized linear model (GLM) was used to compare VUKA families to control families on change in key outcomes over time. Generalized estimating equation (GEE) was employed to account for within-subject correlations due to the effect of repeated measures. We report the group difference (VUKA vs. control) in change over time on outcomes (i.e., the regression coefficient (beta) obtained from each of the GLM models) as well as its corresponding p-values.
Process evaluation
Process evaluation involved two focus group interviews with intervention caregiver participants from both sites (n=20) and six in-depth follow-up individual interviews, conducted after the last session. Interviews focused on participants’ experience and perceptions of how participation affected themselves and their children. Following informed consent procedures, interviews were recorded in isiZulu and translated and transcribed into English, with back-translation checks by an independent, bilingual English-isiZulu speaker. The data were analyzed using thematic analysis; data across focus groups and individual interviews were read twice to identify common issues or constructs that were grouped into common themes and used to form a coding framework. The data were then coded according to these common themes by two independent coders using NVivo 8 software (QSR International) to verify and ensure reliability of the emergent themes.
Results
Demographics Characteristics
All participants were Black South Africans of Zulu ethnicity with most speaking both English and Zulu. Ninety one percent of accompanying caregivers were the children’s mothers, and 52% of children lived with the mother and 40% with grandparents. Chi-square analysis of the demographic characteristics of the two study sites did not reveal any significant differences except the proportion of families receiving child support grants (100% in site 2 compared to less than 75% for site 1).
Attendance and Feasibility
Among the 33 families randomized to the VUKA arm, 32 attended at least one session, 100% of whom completed it, with 94% attending at least 5 of the 6 days and 55% attending all six days. The most common reasons for not attending were illness and family time conflicts. There were no differences in rates of attendance by sites.
Quantitative Analysis
Despite the small sample size, comparisons between VUKA and the comparison group arms revealed some significant differences and trends on key domains including reported ART adherence, HIV treatment knowledge, and caregiver-child communication, with participants in the VUKA arm improving in all key outcomes (Table II). Youth in the VUKA condition evidenced significantly greater improvements in reported ART adherence than youth in the comparison group post-intervention (reported as change scores), (VUKA = 1.10; Control=-.43 at baseline and follow up, p < .05) (Table III). Caregivers in VUKA reported significantly greater change in comfort communicating with their children about sensitive topics (VUKA =.26; Control =-.54, p < .002) and a trend for experiencing less stigma (-.21) than caregivers in the control group (.28, p <.09) (Table III). There was also a trend for youth in VUKA to show more improvements in treatment knowledge (VUKA =.27; Control =-.74, p <.08), and caregiver-child communication than non-intervention group youth (.41 vs-.07, p <.09) (Table III).
Table II. Descriptive Data.
Descriptive characteristics of Intervention Group (VUKA) and Comparison participants
| Measure | N | Mean | SD | Range |
|---|---|---|---|---|
| Children Depression Inventory | ||||
| VUKA | 64 | 3.25 | 2.67 | 0-12 |
| Control | 58 | 2.34 | 2.35 | 0-11 |
| Strengths and Difficulties | ||||
| VUKA | 54 | 18.80 | 3.56 | 11-26 |
| Control | 47 | 17.68 | 4.34 | 11-32 |
| External Stigma | ||||
| VUKA | 62 | 2.47 | .82 | 1-4 |
| Control | 56 | 2.30 | .72 | 1-4 |
| Caregiver Communication | ||||
| VUKA | 65 | 2.43 | .77 | 1-4 |
| Control | 55 | 2.55 | .71 | 1-4 |
| Caregiver Communication Comfort | ||||
| VUKA | 65 | 3.26 | .65 | 2-4 |
| Control | 55 | 3.14 | .73 | 1-4 |
Table III.
Multivariate Analysis - VUKA Intervention Outcomes
| Comparison (mean scores) | VUKA (mean scores) | |||||
|---|---|---|---|---|---|---|
| Item/Scale | Baseline | Follow-up | Baseline | Follow-up | Beta | p-value |
| Youth Adherence Last Time Missed Meds | 4.79 | 4.36 | 3.71 | 4.81 | 1.527 | .05** |
| Youth mental health (CDI; higher worse) | 3.19 | 2.64 | 3.31 | 2.03 | -.736 | .417 |
| Youth behavior (SDQ; higher worse) | 18.80 | 18.38 | 18.79 | 16.96 | -1.412 | .371 |
| Youth HIV treatment knowledge (higher is better) | 4.88 | 4.14 | 4.18 | 4.45 | 1.002 | .079** |
| Caregiver HIV treatment knowledge (Higher is better) | 5.74 | 6.36 | 6.36 | 6.58 | -.402 | .227 |
| Caregiver external stigma | 2.34 | 2.62 | 2.71 | 2.50 | -.484 | .09** |
| Caregiver communication frequency | 2.49 | 2.42 | 2.32 | 2.73 | .478 | .09** |
| Caregiver communication comfort | 3.35 | 2.81 | 3.16 | 3.42 | .796 | .002*** |
significant at α=.05
significant at α =.10
Beta coefficient: Regression Coefficient obtained from GLM model (with GEE method to adjust for within subject correlation) which presents the group differences (VUKA vs. Control) in change in key outcomes over time.
Process evaluation
A number of common themes emerged in the focus groups and individual interviews post VUKA implementation as presented below.
Adherence to medication
Caregivers indicated that VUKA helped improve adherence as children realized that they were not the only ones on medication and became hopeful about their future:
I’m very happy because he didn’t want to take his medication and now [after coming here] he takes it on time, with no difficulties. I think it’s also because he can see other children, he can see that he’s not the only one, there are many others … he now goes out, plays soccer…until seven in the evening and he comes and take his medication and then leaves again.
Improved Self-concept and Future Orientation
Caregivers reported that VUKA helped promote healthy HIV-positive self-identities and future orientation, particularly through the Themba character in the storybook:
…his self-esteem has improved because … [in the] storybook that we use, there it says that Themba is not sick. He even says that “ma, now I know that I’m suffering from something that anyone could suffer from. Just because I’m HIV+ does not mean I’m sick.”
Improved Social Support
Caregivers reported strengthened social support for both themselves and their children through new friendships with other HIV+ children and their caregivers:
“In the beginning he [the child] was scared but now he has realized that he’s not the only one who has [HIV]… he has made new friends…This program has really helped him.”
“…it enabled us to talk to other caregivers…And from that you’d see that problems that one experiences like having an HIV+ child, you’re not the only one.”
Talking About Sensitive Topics
Caregivers also reported that VUKA helped them discuss sensitive topics with their children:
No, I did not talk to her before we came here; I got help from this program. We were given storybooks that had information on adolescence and on how we as caregivers should sit down with our kids and talk to them about such things.
Diffusion of the Program to Other Family Members
The storybooks were reported to assist in garnering support from other family members who read them at home and then assisted in caring for the HIV+ child:
My older son would tell L (the child) to bring the book and they would read it and talk about it, so it has really helped me a lot… now they understand that even if I’m not home they have to look after the child, and check if she has taken her medication, not to wait for me like before when they would leave everything to me…
Discussion
The pilot study results indicate high levels of feasibility and acceptability of VUKA at both hospitals with high levels of attendance. Although a small sample, the results are promising as VUKA participants improved in all the key intervention outcomes with some statistically significant differences in the RCT. This is particularly encouraging in light of the fact that VUKA was delivered by lay counselors, indicating that with appropriate training and support, a family-based intervention for YLWPHIV is feasible in settings with limited professional staff.
Given the importance of ART adherence (Domek, 2010), several significant related changes were found in this pilot. Among those who received VUKA, ART adherence as a function of the last time they missed taking medication was significantly better than that reported in the comparison group. This variable has been strongly associated with HIV viral load (Usitalo et al., 2010). Also, HIV treatment knowledge scores and the frequency and comfort of communication about HIV and other sensitive topics increased and perceptions of external stigma were reduced in the VUKA participants. These findings are important given that previous studies have linked caregiver-child communication to reduced adolescent risk behavior and improved adherence (McKay et al., 2004) and studies have also linked reduced stigma to improved mental health and adherence outcomes (Reisner et al., 2009).
There are several limitations to this study, including the use of self-reported adherence measures and the small sample size. Moreover, it is possible that there was selection bias in participants who agreed to be in the study.
Nevertheless, with the increasing roll-out of ART in South Africa, VUKA was deliberately piloted in one public health facility, reflective of facilities available for the majority of South African HIV+ patients, using lay counselors. VUKA shows promise as a family-based prevention program for YLWPHIV to improve behavioral health outcomes such as adherence that can be effectively delivered by lay staff in public health clinics. In South Africa, where there is a dearth of specialists compared to the number of patients, task-sharing has been central to the re-engineered primary health care system (Pillay & Baron, November 2011). Within the context of South Africa’s resource constraints, use of lay staff under the supervision of a mental health specialist, enhances the possibility of the program being scaled up in South African care settings and thus warrants further study and potential use. It is noteworthy that VUKA was retained in one of the hospitals as part of standard care after the pilot study was completed, based on participant and provider response.
Table I.
Summary Demographics (Youth and Caregivers)
| HIV+ Adolescents (N=66) | n | Percent | ||||
|---|---|---|---|---|---|---|
| Durban Site | 47 | 71 | ||||
| Pietermaritzburg Site | 19 | 29 | ||||
|
| ||||||
| Combined | Site 1 | Percent | Site 2 | Percent | ||
| Gender | ||||||
| Male | 32 | 49 | 24 | 52 | 9 | 47 |
| Female | 33 | 51 | 22 | 48 | 10 | 53 |
| Age Distribution | ||||||
| 10 years | 15 | 23 | 9 | 20 | 6 | 32 |
| 11 years | 18 | 28 | 13 | 28 | 5 | 26 |
| 12 years | 12 | 18 | 8 | 17 | 4 | 21 |
| 13 years | 20 | 31 | 16 | 35 | 4 | 21 |
| Grade | ||||||
| 2 – 3 | 3 | 5 | 1 | 2 | 2 | 10 |
| 4 | 10 | 15 | 7 | 15 | 3 | 16 |
| 5 | 18 | 28 | 13 | 28 | 5 | 26 |
| 6 | 21 | 32 | 16 | 35 | 5 | 26 |
| 7 - 8 | 13 | 20 | 9 | 19 | 4 | 21 |
| Living Arrangements – Yes Responses (non-exclusive) | ||||||
| Mother only | 34 | 52 | 23 | 50 | 11 | 58 |
| Father only | 12 | 18 | 11 | 24 | 1 | 5* |
| Mother and Father | 8 | 12 | 7 | 100 | 1 | 100 |
| Stepmother only | 2 | 3 | 2 | 4 | 0 | 0 |
| Aunt/Uncle | 13 | 20 | 9 | 20 | 4 | 21 |
| Grandparents | 26 | 40 | 16 | 35 | 10 | 53 |
| Older Sibling | 10 | 15 | 7 | 15 | 3 | 16 |
|
| ||||||
| Caregiver Characteristics (N=66) | n | Percent | ||||
| Durban Site | 47 | 71 | ||||
| Pietermaritzburg Site | 19 | 29 | ||||
|
| ||||||
| Combined | Site 1 | Percent | Site 2 | Percent | ||
| Gender | ||||||
| Male | 6 | 9 | 5 | 11 | 1 | 5 |
| Female | 59 | 91 | 41 | 89 | 18 | 95 |
| Age Distribution | ||||||
| 21-30 | 5 | 9 | 2 | 5 | 3 | 16 |
| 31-40 | 23 | 40 | 14 | 36 | 9 | 47 |
| 41-50 | 17 | 29 | 15 | 39 | 2 | 10 |
| 51-60 | 4 | 7 | 2 | 5 | 2 | 10 |
| 61-70 | 6 | 10 | 3 | 8 | 3 | 16 |
| 71+ | 3 | 5 | ||||
| Level of Formal Education | ||||||
| 8th grade or less | 22 | 35 | 18 | 40 | 4 | 22 |
| Some high school | 19 | 30 | 9 | 20 | 10 | 56 |
| Completed high school | 13 | 21 | 10 | 22 | 3 | 17 |
| Post School | 9 | 14 | 9 | 13 | 1 | 6 |
| Employment Status | ||||||
| Employed | 19 | 29 | 14 | 31 | 5 | 26 |
| Intermittent employment | 6 | 9 | 3 | 7 | 3 | 7 |
| Unemployed | 39 | 61 | 28 | 62 | 11 | 58 |
| Relationship Status | ||||||
| Married | 21 | 34 | 14 | 32 | 7 | 37 |
| Single (never married) | 29 | 47 | 20 | 46 | 9 | 47 |
| Separated | 3 | 5 | 2 | 4 | 1 | 5 |
| Divorced | 2 | 3 | 2 | 4 | 0 | 0 |
| Widowed | 7 | 11 | 5 | 11 | 2 | 11 |
| Live in Own Place | ||||||
| Yes | 38 | 58 | 26 | 56 | 12 | 63 |
| Receiving a grant for the child | ||||||
| Yes | 45 | 82 | 33 | 73 | 19 | 100* |
| Household Income | ||||||
| At least one person has job | 20 | 32 | 16 | 36 | 4 | 22 |
| At least one person has pension | 19 | 30 | 12 | 27 | 7 | 39 |
| At least 1 person has job + 1 person has pension | 21 | 33 | 14 | 31 | 7 | 39 |
| No one has a job or a pension | 3 | 5 | 3 | 7 | 0 | 0 |
| Gone without Food in Past Month | ||||||
| More than 6 times | 11 | 17 | 7 | 17 | 0 | 0 |
| 4-6 times | 10 | 16 | 5 | 12 | 2 | 13 |
| 2-3 times | 12 | 19 | 7 | 17 | 2 | 13 |
| 1 time | 5 | 8 | 1 | 2 | 1 | 7 |
| Never | 25 | 40 | 20 | 50 | 10 | 67 |
| Caregiver HIV Status | ||||||
| Positive | 34 | 69 | 25 | 73 | 9 | 60 |
| Negative | 11 | 22 | 8 | 23 | 3 | 20 |
| Mother Aware of Child’s HIV Status | ||||||
| Less than 5 years ago | 38 | 60 | 27 | 61 | 11 | 58 |
| More than 5 years ago | 25 | 40 | 17 | 39 | 8 | 42 |
Contributor Information
Prof. Arvin Bhana, Human Sciences Research Council, Human & Social Development, Durban, South Africa.
Dr. Claude Ann Mellins, Columbia University, Psychiatry, 1051 Riverside Drive, Box 15, NYC, 10032 United States New York State Psychiatric Institute, HIV Center for Clinical and Behavioral Studies, 1051 Riverside Drive, Box 15, NYC, 10032 United States.
Dr. Inge Petersen, University of KwaZulu-Natal, Psychology, Howard College, Durban, 4000 South Africa
Ms. Stacey Alicea, New York University, Department of Applied Psychology, 246 Greene Street, New York, 10003 United States
Ms. Nonhlahla Myeza, McCord Hospital, Psychology, Durban, South Africa
Dr. Helga Holst, McCord Hospital, Durban, South Africa
Dr. Elaine Abrams, Columbia University’s Mailman School of Public Health, ICAP, New York, United States
Ms. Sally John, McCord Hospital, Psychology, McCord Road, Overport, Durban, Durban, 4001 South Africa
Dr. Meera Chhagan, University of KwaZulu-Natal, Maternal and Child Health, Durban, South Africa
Ms. Danielle F Nestadt, New York State Psychiatric Institute, HIV Center for Clinical and Behavioral Studies, 1051 Riverside Drive, Box 15, NYC, 10032 United States
Dr. Cheng-Shiun Leu, HIV Center for Clinical and Behavioral Studies, Biostatistics, New York, United States
Dr. Mary McKay, New York University, Silver School of Social Work, New York, United States
References
- Abramowitz S, Koenig LJ, Chandwani S, Orban L, Stein R, Lagrange R, Barnes W. Characterizing social support: global and specific social support experiences of HIV-infected youth. AIDS Patient Care and STDs. 2009;23(5):323–330. doi: 10.1089/apc.2008.0194. [DOI] [PubMed] [Google Scholar]
- Antle BJ, Wells LM, Goldie RS, DeMatteo D, King SM. Challenges of parenting for families living with HIV/AIDS. Social Work. 2001;46(2):159–169. doi: 10.1093/sw/46.2.159. [DOI] [PubMed] [Google Scholar]
- Bacha T, Pomeroy EC, Gilbert D. A psychoeducational group intervention for HIV-positive children: a pilot study. Health & Social Work. 1999;24(4):303–306. doi: 10.1093/hsw/24.4.303. [DOI] [PubMed] [Google Scholar]
- Bauermeister JA, Elkington KS, Robbins RN, Kang E, Mellins CA. A prospective study of the onset of sexual behavior and sexual risk in youth perinatally infected with HIV. Journal of Sex Research. 2011;49(5):413–422. doi: 10.1080/00224499.2011.598248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CC, Bhana A, Petersen I, McKay MM, Gibbons R, Bannon W, Amatya A. Building protective factors to offset sexually risky behaviors among black youths: A randomized control trial. Journal of the National Medical Association. 2008;100(8):1–9. doi: 10.1016/s0027-9684(15)31408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhana A, McKay MM, Mellins C, Petersen I, Bell CC. Family-based HIV prevention and intervention services for youth living in poverty-affected contexts: The CHAMP model of collaborative, evidence-informed programme development. Journal of the International AIDS Society. 2010;13(Supp 2):S8. doi: 10.1186/1758-2652-13-S2-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brackis-Cott E, Kang E, Dolezal C, Abrams EJ, Mellins CA. Brief report: Language ability and school functioning of youth perinatally infected with HIV. Journal of Pediatric Health Care. 2009;23(3):158–164. doi: 10.1016/j.pedhc.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchacz K, Rogol AD, Lindsey JC, Wilson CM, Hughes MD, Seage GR, 3rd, Rogers AS, et al. Delayed onset of pubertal development in children and adolescents with perinatally acquired HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2003;33(1):56–65. doi: 10.1097/00126334-200305010-00009. [DOI] [PubMed] [Google Scholar]
- Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2012;53(4):363–370. doi: 10.1111/j.1469-7610.2011.02459.x. [DOI] [PubMed] [Google Scholar]
- Domek GJ. Debunking common barriers to pediatric HIV disclosure. Journal of Tropical Pediatrics. 2010;56(6):440–442. doi: 10.1093/tropej/fmq013. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Pao M. Youths and HIV/AIDS: Psychiatry’s role in a changing epidemic. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(8):728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis DA, Naar-King S, Cunningham PB, Secord E. Use of multisystemic therapy to improve antiretroviral adherence and health outcomes in HIV-infected pediatric patients: evaluation of a pilot program. AIDS Patient Care and STDs. 2006;20(2):112–121. doi: 10.1089/apc.2006.20.112. [DOI] [PubMed] [Google Scholar]
- Fitts WH, Warren WL. Tennessee self-concept scale. 2. Torrance, CA: Western Psychological Services; 1996. [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Haberer JE, Kahane J, Kigozi I, Emenyonu N, Hunt P, Martin J, Bangsberg DR. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS and Behavior. 2010;14(6):1340–1346. doi: 10.1007/s10461-010-9799-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens JF, Mellins CA. Psychiatric aspects of HIV/AIDS in childhood and adolescence. In: Rutter M, Taylor E, editors. Child and adolescent psychiatry: Modern approaches. 5. Oxford: Blackwell; 2008. pp. 945–955. [Google Scholar]
- Heymann J, Kidman R. HIV/AIDS, declining family resources and the community safety net. AIDS Care. 2009;21(sup1):34–42. doi: 10.1080/09540120902927593. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta paedopsychiatrica. 1981;46(5-6):305–315. [PubMed] [Google Scholar]
- Ledlie SW. The psychosocial issues of children with perinatally acquired HIV disease becoming adolescents: A growing challenge for providers. AIDS Patient Care and STDs. 2001;15(5):231–236. doi: 10.1089/10872910152050748. [DOI] [PubMed] [Google Scholar]
- Levy SR, Lampman C, Handler A, Flay BR, Weeks K. Young adolescent attitudes toward sex and substance use: Implications for AIDS prevention. AIDS Education and Prevention. 1993;5(4):340–351. [PubMed] [Google Scholar]
- McKay M, Paikoff R, editors. Community collaborative partnerships: The foundation for HIV prevention research efforts in the United States and internationally. PA: Haworth Press; 2007. [Google Scholar]
- McKay MM, Chasse KT, Paikoff R, McKinney L, Baptiste D, Coleman D, Bell CC, et al. Family-level impact of the CHAMP Family Program: A community collaborative effort to support urban families and reduce youth HIV risk exposure. Family Process. 2004;43:79–93. doi: 10.1111/j.1545-5300.2004.04301007.x. [DOI] [PubMed] [Google Scholar]
- Mellins C, Brackis-Cott E, Dolezal C, Abrams E, Wiznia A, Bamji M, Mckay M, et al. Predictors of non-adherence in perinatally HIV-infected youths; Paper presented at the NIMH/IAPAC International Conference on HIV Treatment and Adherence; Jersey City, NJ. 2006. [Google Scholar]
- Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. The role of psychosocial and family factors in adherence to antiretroviral treatment in human immunodeficiency virus-infected children. The Pediatric infectious disease journal. 2004;23(11):1035–1041. doi: 10.1097/01.inf.0000143646.15240.ac. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Elkington KS, Bauermeister JA, Brackis-Cott E, Dolezal C, McKay M, Abrams EJ, et al. Sexual and drug use behavior in perinatally HIV-infected youth: Mental health and family influences. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(8):810–819. doi: 10.1097/CHI.0b013e3181a81346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins CA, Elkington KS, Leu CS, Santamaria EK, Dolezal C, Wiznia A, Abrams EJ, et al. Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care. 2012;24(8):953–962. doi: 10.1080/09540121.2012.668174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins CA, Tassiopoulos K, Malee K, Moscicki AB, Patton D, Smith R, Seage GR, et al. Behavioral health risks in perinatally HIV-exposed youth: Co-occurrence of sexual and drug use behavior, mental health problems, and nonadherence to antiretroviral treatment. AIDS Patient Care and STDs. 2011;25(7):413–422. doi: 10.1089/apc.2011.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, Cooper C, et al. Adherence to HAART: A systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Medicine. 2006;3(11):e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nozyce ML, Lee SS, Wiznia A, Nachman S, Mofenson LM, Smith ME, Pelton S, et al. A behavioral and cognitive profile of clinically stable HIV-infected children. Pediatrics. 2006;117(3):763–770. doi: 10.1542/peds.2005-0451. [DOI] [PubMed] [Google Scholar]
- Petersen I, Bhana A, Myeza N, Alicea S, John S, Holst H, Mellins C, et al. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: A qualitative investigation. AIDS Care. 2010;22(8):970–978. doi: 10.1080/09540121003623693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen I, Mason A, Bhana A, Bell CC, McKay M. Mediating social representations using a cartoon narrative in the context of HIV/AIDS: The AmaQhawe Family Project in South Africa. Journal of Health Psychology. 2006;11(2):197–208. doi: 10.1177/1359105306061180. [DOI] [PubMed] [Google Scholar]
- Pillay Y, Baron P. The implementation of PHC re-engineering in South Africa. 2011 Nov; Retrieved from http://www.phasa.org.za/articles/the-implementation-of-phc-re-engineering-in-southafrica.html.
- Preciago J, Henry M. Linguistic Barriers in health education and services. In: Garcia JG, Zea MC, editors. Psychological interventions and research with Latino populations. Boston: Allyn and Bacon; 1997. pp. 235–254. [Google Scholar]
- Reisner SL, Mimiaga MJ, Skeer M, Perkovich B, Johnson CV, Safren SA. A review of HIV antiretroviral adherence and intervention studies among HIV–infected youth. Adherence and Intervention in Youth. 2009;17(1):14–25. [PMC free article] [PubMed] [Google Scholar]
- Republic of South Africa. Country Progress Report on the Declaration of Commitment on HIV/AIDS. 2010 Retrieved from http://data.unaids.org/pub/Report/2010/southafrica_2010_country_progress_report_en.pdf.
- Rogers AS, Miller S, Murphy DA, Tanney M, Fortune T. The TREAT (Therapeutic Regimens Enhancing Adherence in Teens) program: Theory and preliminary results. The Journal of Adolescent Health. 2001;29(3 Suppl):30–38. doi: 10.1016/s1054-139x(01)00289-0. [DOI] [PubMed] [Google Scholar]
- Sutcliff CG, van Dijk JH, Bolton C, Persaud D, Moss WJ. Effectiveness of antiretroviral therapy among HIV-infected children in sub-Saharan Africa. Lancet Infectious Diseases. 2008;8:477–489. doi: 10.1016/S1473-3099(08)70180-4. [DOI] [PubMed] [Google Scholar]
- Tanzer NK, Sim CQE. Adapting instruments for use in multiple languages and cultures: A review of the ITC Guidelines for Test Adaptations. European Journal of Psychological Assessment. 1999;15(3):258–269. doi: 10.1027//1015-5759.15.3.258. [DOI] [Google Scholar]
- Usitalo A, Leister E, Tassiopoulos K, Allison S, Malee K, Mellins C, Seage G, et al. Relationship between viral load and behavioral measures of medication adherence among youth with HIV; Paper presented at the Pediatric Academic Society; Vancouver, BC. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook LE, Bauman LJ, Shinnar S. Applying stigma theory to epilepsy: A test of a conceptual model. Journal of Pediatric Psychology. 1992;17(5):633–649. doi: 10.1093/jpepsy/17.5.633. [DOI] [PubMed] [Google Scholar]
- Youth in Mind. The CORC-YouthinMind outcomes measures database. 2012 Retrieved from http://www.corc.uk.net/resources/implementation-support/databases-templates-and-info-to-send-to-corc/youth-in-mind/


