Abstract
Background
Patients with high grade chronic pulmonary obstructive disease (COPD) account for much of the COPD-related mortality and incur excessive financial burdens and medical care utilization. We aimed to determine the characteristics and medical care use of such patients using nationwide data from the Korean Health Insurance Review and Assessment Service in 2009.
Materials and methods
Patients with COPD were identified by searching with the International Classification of Diseases–10th Revision for those using medication. Patients with high grade COPD were selected based on their patterns of tertiary institute visits and medication use.
Results
The numbers of patients with high grade COPD increased rapidly in Korea during the study period, and they showed a high prevalence of comorbid disease. The total medical costs were over three times higher in patients with high grade COPD compared with those without it ($3,744 versus $1,183; P < 0.001). Medication costs comprised the largest portion of medical cost, but most impact came from hospitalization and exacerbation in both groups of patients. COPD grade and hospitalization in the previous year were the major factors affecting medical costs and days of utilizing health care resources.
Conclusion
Patients with high grade COPD impose a high economic burden on the health care system in Korea. Prevention of progression to high grade COPD is important, both clinically and economically.
Keywords: COPD, population characteristics, health care utilization, medical cost
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality, with a substantial and increasing societal burden.1 COPD is a serious public health problem in many countries throughout the world. According to World Health Organization estimates, 80 million people have moderate to severe COPD, and three million people died of COPD in 2005. The organization also predicted that COPD will become the fourth leading cause of death worldwide by 2030 (http://www.who.int/respiratory/copd/burden/en/).
Mortality from COPD increases as the severity of COPD aggravates,2 and socioeconomic burdens are mostly observed in severe COPD patients.3 Furthermore, the severity of COPD is directly correlated with medical care costs, and the medical expenses of patients with severe COPD are reportedly more than two times greater than for those with mild COPD.4 Acute exacerbation and hospital admission account for most expenses incurred by patients with severe COPD.5 Most studies have assessed severity of disease with the degree of airflow limitation; however, there has been growing evidence which demonstrates that the degree of airflow limitation does not correlate well with patients’ severity of symptoms and health status,6 and a history of frequent exacerbations (>2 exacerbations in the previous year) is itself a strong predictor of future risk.7 In light of these changes in thinking about COPD as being more than a disease of airflow limitation, the 2011 Global Initiative for Chronic Obstructive Lung Disease guidelines recommend a new system of assessment which combines the symptomatic assessment with the spirometric classification and/or risk of exacerbations.8 According to the 2011 guidelines, patients with more symptomatic and higher COPD risk are most highly impacted by COPD and can be regarded as high grade COPD patients.
Identifying the characteristics of such patients and financial influences may be crucial for their effective and economical treatment. Until recently, there were few studies that focused on the characteristics and utilization of medical resources in patients with high grade COPD.
Korea has a unique health care security system that is managed and supervised by the government. It is based on a health insurance plan that includes almost all the population and medical facilities. The Korean National Health Insurance (KNHI), where almost the entire Korean population is mandatorily registered, covers nearly all medical expenses, and the Korean Health Insurance Review and Assessment Service (KHIRA) database has details of all medications, medical services, and diagnoses for claims made. Thus, the KHIRA database provides a useful and reliable source of epidemiologic data and allows nationwide studies.9
The present study aimed to define the characteristics and use of medical resources in patients with high grade COPD selected according to treatment setting and drug use by analyzing the nationwide KHIRA database. This could provide insight into the medical and economic problems faced by such patients.
Materials and methods
Dataset
We used the 2009 KHIRA database to define the clinical characteristics and utilization of medical resources in cases of high grade COPD. The databases for 2006 to 2010 were employed to study any changes in the incidence of patients with COPD. The KHIRA is responsible for reviewing medical fees, assessing the quality of health care institutions, evaluating whether health care services are necessary medically, and assuring services are delivered to beneficiaries at an appropriate level and cost. The Korean health security system is based on the obligatory KNHI scheme. Almost all citizens are obliged to join this. In 2008, there were 50,001,027 beneficiaries, and medical aid was provided through a social welfare fund for 1,841,339 persons: 3.7% of the population was unable to pay the insurance premium.10 Almost all hospitals, private clinics, public health centers, and pharmacies were registered in KNHI. Medical facilities claim costs from the KNHI, then KHIRA assesses the claims based on diagnostic codes and medical records. All medical costs associated with COPD treatment, including laboratory examinations, medications, surgeries, and hospitalizations, are covered by the health security system, and all related records are stored in the KHIRA databases.
Criteria for patient selection
We identified patients with COPD as a principal or secondary diagnosis by searching for codes of the International Classification of Diseases-10th Revision (ICD-10) and medication use.
The definition of a patient with COPD was based on the following criteria: (1) age more than 40 years, (2) ICD-10 codes of COPD or emphysema, namely J43.x–J44.x (except for J43.0), (3) use of more than one drug for COPD such as a long-acting muscarinic antagonist (LAMA), a long-acting beta-2 agonist (LABA), inhaled corticosteroids (ICS), ICS plus LABA (ICS + LABA), short-acting muscarinic antagonist, short-acting beta-2 agonist, or methylxanthine at least twice per year.
The arbitrary definition of having high grade COPD was a patient who met all the following criteria: (1) tertiary hospital care patient who met the definition of COPD described above, (2) use of triple inhaler therapy regularly (ICS + LABA + LAMA) or systemic steroid therapy at least two times per year with COPD inhaler therapy (LAMA or ICS + LABA).
Patients with more than one reimbursement per year because of cancer (ICD-10 codes C00.x–C97.x), renal failure (N17.x–N19.x), and/or cerebrovascular disease (I60.x–I69.x) were excluded from this study because the enormous expenses reimbursed for treatment of these diseases were difficult to distinguish from COPD-related medical services.
Outcome
For patients who were defined as having COPD, medical utilization and costs were analyzed during 2009. Analysis was confined to COPD-related utilization and costs. Medical utilization and costs were excluded for analysis if they were not considered as COPD-related. For outpatient service, analysis was confined to visits when the principal or secondary diagnosis was COPD (ICD-10 codes J43.x–J44.x, except for J43.0) and when COPD-related medications were received. For inpatient service, analysis was confined to admissions when the principal or secondary diagnosis was COPD (J43.x–J44.x, except for J43.0) or COPD-related diseases such as pneumonia (J12.x–J17.x), pulmonary thromboembolism (I26, I26.0 and I26.9), dyspnea (R06.0), or acute respiratory distress syndrome (J80) with prescriptions of COPD-related medication.
Data regarding age, sex, comorbidity, hospitalization, emergency room visits, intensive care unit admission, medical costs, and medication use were collected. For comorbidity, the prevalence of ten diseases (ischemic heart disease, osteoporosis, depressive disorder, arthritis, diabetes mellitus, pneumothorax, congestive heart failure, hypertension, anemia, and metabolic syndrome) were analyzed using ICD-10 codes.
Days of health care use were analyzed separately according to outpatient and inpatient services. Days of outpatient service utilization were analyzed only for patients who used such service. Days of inpatient service utilization were analyzed only for patients who used an inpatient service including an emergency room or intensive care. Total health care utilization days were analyzed for all patients who used outpatient or inpatient service.
All costs are presented in US dollars, with an exchange rate of 1 dollar equal to 1,152 Korean won (exchange rate on July 20, 2012). The National Evidence-Based Healthcare Collaborating Agency ethics committee approved the present study (PIRB11-022). The requirement for informed consent from the patients included in the study was waived by the ethical review board.
Statistical analysis
Differences between groups were assessed using the chi-squared test for categorical variables and Student’s t-test for continuous variables. Multiple linear regression analysis was performed to identify factors affecting medical cost and days of health care use. Dependent variables were log-transformed in linear regression analysis, as health care utilization variables are usually not normally distributed, with a long and heavy right tail. All tests were two sided, and P-values < 0.05 were considered statistically significant. Data are expressed as the mean ± standard deviation. All statistical analyses were performed using SAS version 9.2 (SAS Institute, Inc, Cary, NC, USA).
Results
Baseline characteristics and changes in the incidence of patients with high grade COPD
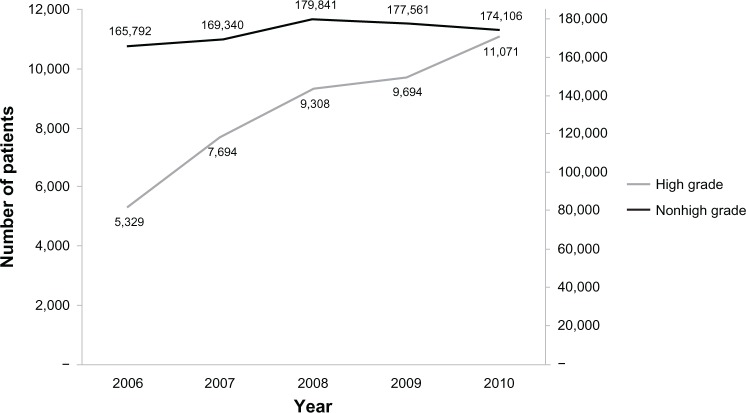
The number of patients with nonhigh grade COPD increased from 165,792 in 2006 to 174,106 in 2010: a 5% (8,314 patients) increase over 5 years. However, patients with high grade COPD more than doubled from 5,329 to 11,071 in the same period, showing a 119.6% (6,372 patients) increase. Patients with high grade COPD accounted for 3.1% of all patients with COPD in 2006, increasing to 6.0% in 2010 (Figure 1).
Figure 1.
Changes in number of high grade and nonhigh grade COPD patients during the years 2006–2010.
We explored the 2009 database to analyze the clinical characteristics of patients with high grade COPD. A total of 187,255 patients with COPD were identified. Among them, 9,694 (5.2%) were compatible with the criteria of high grade COPD and 177,561 (94.8%) were classed as having nonhigh grade COPD. A comparison was made between the two groups: high grade versus nonhigh grade COPD (Table 1). High grade COPD was more common in men (severe versus nonsevere; 78.7% versus 61.8%, P < 0.001). Although the difference was negligible, mean age was significantly higher in the nonhigh grade COPD group (69.4 ± 9.6 years versus 69.9 ± 10.7 years, P < 0.001). The percentage of elderly patients over 80 years-old was also slightly higher in patients with nonhigh grade COPD. High grade COPD was more prevalent among medical aid patients than medical insurance patients. The prevalence of COPD-associated comorbid diseases such as ischemic heart disease, congestive heart failure, hypertension osteoporosis, depressive disorder, diabetes, metabolic syndrome, and anemia were significantly higher in patients with high grade COPD (P < 0.001), except for arthritis.
Table 1.
Sociodemographic and clinical characteristics of patients studied
| High grade COPD (n = 9,694) | Nonhigh grade COPD (n = 177,561) | P-value | |
|---|---|---|---|
| Male, n (%) | 7,627 (78.7%) | 109,821 (61.8%) | <0.001 |
| Age, years | |||
| Mean ± SD | 69.4 ± 9.6 | 69.9 ±10.7 | <0.001 |
| Age, n (%) | |||
| 40–49 years | 333 (3.4%) | 7,978 (4.5%) | |
| 50–59 years | 1,167 (12.0%) | 21,116 (11.9%) | |
| 60–69 years | 2,976 (30.7%) | 48,418 (27.3%) | |
| 70–79 years | 3,904 (40.3%) | 68,830 (38.8%) | |
| ≥80 years | 1,314 (13.6%) | 31,219 (17.6%) | |
| Insurance type | <0.001 | ||
| Health insurance | 7,865 (81.1%) | 148,373 (83.6%) | |
| Medical aid | 1,829 (18.9%) | 29,188 (16.4%) | |
| Comorbidity | |||
| Ischemic heart disease | 1,207 (12.5%) | 14,682 (8.3%) | <0.001 |
| Congestive heart failure | 721 (7.4%) | 9,755 (5.5%) | <0.001 |
| Hypertension | 3,418 (35.3%) | 50,435 (28.4%) | <0.001 |
| Osteoporosis | 736 (7.6%) | 8,434 (4.7%) | <0.001 |
| Depressive disorder | 342 (2.1%) | 3,022 (1.7%) | <0.001 |
| Arthritis | 298 (3.1%) | 6,600 (3.7%) | 0.001 |
| Diabetes mellitus | 1,740 (13.4%) | 22,260 (12.5%) | <0.001 |
| Anemia | 208 (2.1%) | 2,721 (1.5%) | <0.001 |
| Metabolic syndrome | 732 (7.6%) | 10,902 (6.1%) | <0.001 |
Note: Data are expressed as mean ± standard error or number of patients with percentage in parentheses.
Abbreviations: COPD, chronic pulmonary obstructive disease; SD, standard deviation.
Health care utilization and costs of patients with high grade COPD
The health care utilization of cases with COPD by grade is shown in Table 2. The proportion of patients who had a history of emergency room visits, hospital admissions, or intensive care unit admissions was significantly higher in patients with high grade COPD than patients with nonhigh grade COPD (P < 0.001). In patients with high grade COPD, more than half of them had an experience of hospitalization, and 34.7% of them had a history of emergency room visits. In particular, patients who had a history of more than three emergency room visits were almost nine times more prevalent in the high grade COPD group than among patients with nonhigh grade COPD (severe versus nonsevere; 5.3% versus 0.6%, P < 0.001). Moreover, 30.6% of patients with high grade COPD had a history of admission to hospital in the previous year, significantly higher than the 11.4% of patients with nonhigh grade COPD (P < 0.001). In particular, patient visits to emergency rooms in the previous year were more than three times more frequent among patients with high grade COPD (high grade versus nonhigh grade; 18.1% versus 4.9%, P < 0.001). One out of five patients with high grade COPD had visited the emergency department more than once a year. Moreover, the number of outpatient clinic visits, admission days, and total days of health care use were significantly higher in patients with high grade COPD (P < 0.001).
Table 2.
Health care resource utilization of COPD patients according to grade of disease
| High grade COPD (n = 9,694) | Nonhigh grade COPD (n = 177,561) | P-value | |
|---|---|---|---|
| History of hospitalization (yes)† | 5,331 (55.0%) | 37,564 (21.2%) | <0.001 |
| History of ICU admission (yes)† | 74 (0.8%) | 587 (0.3%) | <0.001 |
| History of ER visit (yes) | 3,363 (34.7%) | 15,399 (8.7%) | <0.001 |
| Number of visits (%) | <0.001 | ||
| 0 visit | 6,331 (65.3%) | 162,162 (91.3%) | |
| 1–2 visits | 2,855 (29.5%) | 14,379 (8.1%) | |
| 3≥ visits | 508 (5.3%) | 1,020 (0.6%) | |
| Last year hospitalization (yes)* | 2,969 (30.6%) | 20,654 (11.6%) | <0.001 |
| Last year ER visit (yes) | 1,751 (18.1%) | 8,658 (4.9%) | <0.001 |
| Used days | |||
| Outpatient services | 9.6 ± 9.8 | 7.4 ± 8.6 | <0.001 |
| Inpatient services | 30.0 ± 38.1 | 24.6 ± 35.8 | <0.001 |
| Total used days | 26.0 ± 33.8 | 12.5 ± 21.0 | <0.001 |
Notes: Data are expressed as mean ± standard error or number of patients with percentage in parentheses.
Represents number of patients who were hospitalized, cared for in ICU, and visited ER in the year 2009
represents number of patients who were hospitalized in the year 2008.
Abbreviations: COPD, chronic pulmonary obstructive disease; ER, emergency room; ICU, intensive care unit.
The medical costs per patient during 2009 according to the grade of COPD are shown in Table 3. The total costs of all medical utilization by patients with COPD and the proportion of medical utilization were analyzed. The total cost of outpatient service and inpatient services per person were significantly higher in patients with high grade COPD compared with those with nonhigh grade COPD (P < 0.001). The total medical costs were over three times higher in patients with high grade COPD compared with the nonhigh grade COPD group ($3,744 versus $1,183). Hospital costs accounted for 55% of all medical costs in the nonhigh grade COPD group and 69% in the high grade COPD group. Cost for medication, regardless of whether COPD-related or nonrelated drugs such as antibiotics, was the most important factor determining medical expenses for outpatient services. However, costs other than for medication and examination (including personnel expenditure, administrative charge, and food expense) had the largest portion in the expense for inpatient services. Taken together, the largest proportion of cost in both groups of patients was for medication; however, patients with high grade COPD spent almost three times more for medication than patients with nonhigh grade COPD ($1,691 versus $577).
Table 3.
Comparison of different components of medical cost between high grade and nonhigh grade COPD patients (per patient)
| High grade COPD
|
Nonhigh grade COPD
|
P-value | |||
|---|---|---|---|---|---|
| Cost (US$) | % | Cost (US$) | % | ||
| Outpatient services | |||||
| Laboratory examination | 53.2 | 4.6% | 23.1 | 4.5% | |
| Radiologic examination | 16.5 | 1.4% | 7.0 | 1.4% | |
| Medication | 979.0 | 83.9% | 401.5 | 78.9% | |
| Others | 116.9 | 10.1% | 77.1 | 15.2% | |
| Total | 1,166.2 | 100% | 508.7 | 100% | <0.001 |
| Inpatient services | |||||
| Medical examination | 522.9 | 20.3% | 113.0 | 16.7% | |
| Radiologic examination | 93.5 | 3.6% | 25.7 | 3.8% | |
| Medication | 712.0 | 27.6% | 176.2 | 26.1% | |
| Others | 1,250.3 | 48.5% | 355.1 | 53.4% | |
| Total | 2,578.6 | 100% | 647.7 | 100% | <0.001 |
| Total | |||||
| Medical examination | 576.1 | 15.4% | 136.1 | 11.5% | |
| Radiologic examination | 111.0 | 2.9% | 32.7 | 2.8% | |
| Medication | 1,691.0 | 45.2% | 577.7 | 48.8% | |
| Others | 1,367.7 | 36.5% | 436.9 | 36.9% | |
| Total | 3,744.8 | 100% | 1,183.4 | 100% | <0.001 |
Note: Medical examination includes laboratory examinations, pulmonary function tests, and echocardiography but not radiologic examination.
Abbreviation: COPD, chronic pulmonary obstructive disease.
We analyzed the pattern of COPD-related drug use and cost per patient (Table 4). Oral corticosteroids and LAMA were prescribed for over 99% of patients with high grade COPD. Methylxanthine was used universally in both groups. The total costs of COPD-related medication per person were significantly higher in patients with high grade COPD compared with patients with nonhigh grade COPD ($671.00 versus $188.04, P < 0.001). Costs for inhaled drugs accounted for the largest difference between groups. The mean cost of each medication per patient was also significantly higher in patients with high grade COPD compared with the nonhigh grade group (P < 0.001).
Table 4.
Pattern of COPD related drug use and costs by grade
| Drug | High grade COPD
|
Nonhigh grade COPD
|
P-value† | ||
|---|---|---|---|---|---|
| n (%) | Cost (US$)a | n (%) | Cost (US$)a | ||
| ICS | 2,552 (26.3) | 14.0 ± 23.1 | 16,232 (9.1) | 3.6 ± 6.7 | <0.001 |
| ICS + LABA | 7,205 (74.3) | 206.2 ± 142.0 | 48,933 (27.6) | 57.5 ± 46.1 | <0.001 |
| LAMA | 9,691 (99.9) | 259.3 ± 344.3 | 44,054 (24.8) | 59.5 ± 80.0 | <0.001 |
| LABA | 16 (0.2) | 0.1 ± 0.1 | 122 (0.1) | 0.1 ± 0.0 | 0.284 |
| LTRA | 3,684 (38.0) | 81.0 ± 61.8 | 29,260 (16.5) | 24.7 ± 24.6 | <0.001 |
| OCS | 9,690 (99.9) | 8.7 ± 22.6 | 38,810 (21.9) | 1.0 ± 2.8 | <0.001 |
| SAMA | 4,209 (43.4) | 13.6 ± 41.4 | 24,523 (13.8) | 3.0 ± 5.8 | <0.001 |
| SABA | 6,241 (64.4) | 15.4 ± 28.2 | 45,866 (25.8) | 3.6 ± 20.2 | <0.001 |
| SABA + SAMA | 422 (4.35) | 2.1 ± 2.6 | 4,036 (2.3) | 1.0 ± 1.3 | <0.001 |
| Oral beta-2 agonist | 4,655 (48.0) | 22.9 ± 29.9 | 80,709 (45.5) | 12.2 ± 21.3 | <0.001 |
| Methylxanthine | 8,360 (86.2) | 47.5 ± 39.6 | 137,937 (77.7) | 22.4 ± 28.6 | <0.001 |
| Total cost | 671.0 | 188.4 | |||
Notes:
P-value is for the comparison of cost per patient
represents cost per patient.
Abbreviations: ICS, inhaled corticosteroids; COPD, chronic pulmonary obstructive disease; LABA, long-acting beta-2 agonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene antagonist; OCS, oral corticosteroids; SABA, short-acting beta-2 agonist; SAMA, short-acting muscarinic antagonist.
Multiple linear regression was performed to search for factors affecting days of health care use (Table 5). Age, sex, COPD severity, hospitalization in the previous year, and previous emergency room visit were used for the analysis. All these variables were significant factors affecting days of health care use (P < 0.001). Among four categorical variables (male sex, COPD grade, previous year’s hospitalization, and previous year’s emergency room attendance), a history of hospitalization in the previous year was the most powerful factor affecting days of health care use, followed by COPD grade.
Table 5.
Multiple linear regression for factors affecting days of health care use
| Variable | Unadjusted
|
Adjusted
|
||||
|---|---|---|---|---|---|---|
| β | exp(β) | P-value | β | exp(β) | P-value | |
| Last year hospitalization | 0.834 | 2.302 | <0.0001 | 0.669 | 1.935 | <0.001 |
| COPD grade | 0.781 | 2.184 | <0.0001 | 0.622 | 1.862 | <0.001 |
| Age (year) | 0.138 | 1.148 | <0.0001 | 0.125 | 1.133 | <0.001 |
| Last year | 0.799 | 2.224 | <0.0001 | 0.061 | 1.063 | <0.001 |
| ER visit | ||||||
| Male | 0.013 | 1.013 | <0.0001 | 0.011 | 1.011 | <0.001 |
Abbreviations: COPD, chronic pulmonary obstructive disease; ER, emergency room; exp, exponentiated regression coefficients.
Discussion
This study was designed to investigate the characteristics, health care utilization, and medical expenses of patients with high grade COPD by utilizing data from the KNHI and KHIRA systems, where almost the entire Korean population is currently registered.
In our analysis, patients presenting with high grade COPD have more than doubled in presentation (119.3%) compared with patients with nonhigh grade COPD, with a 5% increase between 2006 and 2010. This outcome might be attributable to natural aging of the population, use of more therapeutic options by physicians such as ICS, LAMA, or ICS + LABA, and continuous exposure to risk factors, but these are insufficient to explain this amazing increase. An additional reason may be that as the recognition of COPD has increased, more patients with high grade COPD are being diagnosed, resulting in a trend toward more frequent visits to tertiary institutions by patients with high grade COPD. This trend is expected to continue.
In this study, patients with high grade COPD were more common in younger age groups (<80 years) than in older groups. This finding is likely to be due to the impact of a “healthy survivor” effect. The relatively higher number of patients with high grade COPD in their 60s and 70s is thought to be attributable to the higher mortality of patients with high grade COPD before they reach their 80s.
Because people with a low income, who cannot afford medical insurance premiums, are supported by medical aid funded by the national welfare fund in KNHI, medical aid patients can be considered a low-income group. Such patients were more common in the high grade COPD group. These results are consistent with other data suggesting that low socioeconomic status is an important risk factor for COPD.11
COPD is characterized by the more frequent contraction of comorbid diseases compared to the general population.12,13 Comorbidity is a critical factor determining the severity of COPD and has a significant impact on the mortality of patients with COPD.12,13 These associations might be explained by exposure to cigarette smoke, but some data show a significant interaction of reduced lung function and cigarette smoking on systemic inflammation.14 Although the relationship between the severity of COPD and associated diseases has not yet been completely clarified, some studies have reported that no significant relationship could be found between them.15
This analysis showed that, except for arthritis, almost all diseases that were comorbid with COPD tended to prevail in patients with high grade COPD including cardiovascular diseases, osteoporosis, and type 2 diabetes. In particular, severe heart diseases such as ischemic heart disease, congestive heart failure, which can affect mortality directly, were more commonly observed in patients with high grade COPD. Therefore, comorbid diseases appear to be profoundly linked with the mortality of patients with high grade COPD. Because a previous study demonstrated that the prevalence of cardiovascular disease was one of the major determinants of the overall cost of the disease,16 a high prevalence of comorbidity can be speculated as a major contributor to medical costs in patients with high grade COPD.
In our study, patients with a history of hospitalization or visits to the intensive care or emergency rooms were significantly more prevalent among patients with high grade COPD than in patients with nonsevere COPD. Thus, patients with high grade COPD showed statistically significant increases by more than 2.5- and 3-fold in terms of hospitalization in the previous year and a history of emergency department use, respectively. The number of days using medical institutions was more than two times higher in patients with high grade COPD than in the nonhigh grade group, incurring a heavy burden of health care costs.
In conclusion, the grade of COPD was profoundly associated with the use of medical institutions, and acute diseases were found to occur very frequently to the degree of needing to visit emergency rooms. These findings agree with previous studies showing that there was a positive relationship between the degree of COPD severity and health care utilization.17,18
Costs for patients with high grade COPD almost doubled compared with the nonhigh grade COPD group for outpatient treatments, and most medical expenses were for drug therapy. Moreover, greater medical care costs were incurred by hospital admission. The total medical care cost per patient with high grade COPD was more than three times greater than that of patients with nonhigh grade COPD. This is consistent with findings by Masa et al,19 that the cost of severe COPD was more than three times that of moderate COPD.
In-patient treatment was the major cause for the more than three times higher medical expenses among patients with high grade COPD. This finding implies that to decrease the economic burden of COPD, proactive countermeasures must be introduced to reduce the hospital admission of severely affected patients. In this study, we could not delineate the hospitalization and emergency room use caused by the acute exacerbation of COPD, as we only included COPD-related hospital admission in our study. However, it is well known that acute exacerbation is the major cause of hospitalization in patients with COPD. Additionally, the severity of COPD is strongly associated with its degree of exacerbation,20 and exacerbations become more frequent and severe as the severity of COPD increases. Therefore, treatment for preventing the exacerbation of patients with COPD is thought to be essential to reduce the number of admitted patients.
In this study, patients with high grade COPD accrued three times higher medical costs than did patients with nonhigh grade COPD. This is consistent with the results of Menn et al,21 who showed that patients with COPD graded stage 2 or more entailed only 54% more medical costs than did stage 1 patients. This can be explained by the different criteria for patient classification. Our study showed that oral steroids were given to almost all patients with high grade COPD at least once a year. This means that clinically relevant exacerbation occurred very frequently in such patients. This study showed that ICS + LABA and ICS were widely used for treatment of COPD. In Korea, use of ICS + LABA has been approved for COPD patients who have severe degree airflow obstruction (<50% of predicted) since 2004. Although, ICS monotherapy is not approved in the treatment of COPD, it is frequently used in overlap syndrome and prescribed combined with LAMA in case of LABA intolerance. Another interesting finding in our study was the prevalent use of methylxanthine, regardless of the severity of COPD. This reflects the underutilization of inhalers in primary care and low adherence to COPD treatment guidelines in real practice.
Although hospitalization in the previous year had the largest influence on days of health care use, COPD grade can be considered as a more important factor determining the days of health care use because such previous hospitalization occurred very frequently in patients with high grade COPD. Our study suggests that management strategies for COPD should put greater emphasis on reducing the incidence of patients with high grade COPD by early intervention to prevent disease progression.
There were some limitations to our study; we could not adopt pulmonary function data as a parameter for the grade of COPD. However, recent studies demonstrated that the degree of airflow limitation has a poor correlation with symptoms and impairment of health-related quality of life.6,22 The present study used information derived from a database covering an entire nation and classified patients according to their treatment pattern. Thus, our study might reflect the “real world” more closely.
Conclusion
In conclusion, this study has provided new insight regarding the characteristics and health care burden of high grade COPD in Korea. The incidence of patients with high grade COPD has increased rapidly in recent years. COPD grade was an important determinant of medical cost and health care resource utilization. The results of this study suggest that preventing patients with COPD from progression to a high grade disease is essential from both clinical and socioeconomic perspectives.
Acknowledgments
This study was supported by a grant from the Korea Health-care Technology R&D Project (A102065).
Author contributions
JinHee Kim contributed in study design, data collection and analysis, discussions regarding the significance of results, and in writing a draft of the manuscript. Chin Kook Rhee contributed in study design and in discussions regarding the significance of the results. Kwang Ha Yoo contributed in research study design, data collection, collating results, and in discussions regarding the significance of study results. Young Sam Kim, Sei Won Lee, Yong Bum Park, YeonMok Oh, and Sang Do Lee contributed in the study design and in discussions of the significance of results.
Jin Hwa Lee, Yuri Kim and KyungJoo Kim contributed in data collection and analysis. HyoungKyu Yoon contributed in providing study design, data collection, discussing the significance of analyzed data and results, and in reviewing the manuscript. All authors contributed in the interpretation of data, revising the paper and approving the final version.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Halpin DM, Miravitlles M. Chronic obstructive pulmonary disease: the disease and its burden to society. Proc Am Thorac Soc. 2006;3(7):619–623. doi: 10.1513/pats.200603-093SS. [DOI] [PubMed] [Google Scholar]
- 2.Jensen HH, Godtfredsen NS, Lange P, Vestbo J. Potential misclassification of causes of death from COPD. Eur Respir J. 2006;28(4):781–785. doi: 10.1183/09031936.06.00152205. [DOI] [PubMed] [Google Scholar]
- 3.Jensen MB, Fenger-Grøn M, Fonager K, Omland Ø, Vinding AL, Hansen JG. Chronic obstructive pulmonary disease involves substantial health-care service and social benefit costs. Dan Med J. 2013;60(1):A4557. [PubMed] [Google Scholar]
- 4.Miravitlles M, Murio C, Guerrero T, Gisbert R. Costs of chronic bronchitis and COPD: a 1-year follow-up study. Chest. 2003;123(3):784–791. doi: 10.1378/chest.123.3.784. [DOI] [PubMed] [Google Scholar]
- 5.Detournay B, Pribil C, Fournier M, et al. SCOPE Group The SCOPE study: health-care consumption related to patients with chronic obstructive pulmonary disease in France. Value Health. 2004;7(2):168–174. doi: 10.1111/j.1524-4733.2004.72329.x. [DOI] [PubMed] [Google Scholar]
- 6.Jones PW. Health status and the spiral of decline. COPD. 2009;6(1):59–63. doi: 10.1080/15412550802587943. [DOI] [PubMed] [Google Scholar]
- 7.Hurst JR, Vestbo J, Anzueto A, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. doi: 10.1056/NEJMoa0909883. [DOI] [PubMed] [Google Scholar]
- 8.Global Initiative for Chronic Obstructive Lung Disease [homepage on the Internet] Global strategy for the diagnosis, management and prevention of COPD. 2011. [updated Feb 2013]. Available from: http://www.goldcopd.org/Guidelines/guidelines-resources.html.
- 9.Lee SY, Jung KY, Lee IK, et al. Korean Epilepsy Society Prevalence of treated epilepsy in Korea based on national health insurance data. J Korean Med Sci. 2012;27(3):285–290. doi: 10.3346/jkms.2012.27.3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korean National Health Insurance Cooperation Seoul Annual Report of National Health Insurance Statistics, 2008 Seoul: Division of statistical analysis, Korean National Health Insurance Cooperation; 2008Available from: http://www.nhis.or.kr/portal/site/main/MENU_WBDDG02/Accessed August 2013 [Google Scholar]
- 11.Prescott E, Lange P, Vestbo J. Socioeconomic status, lung function and admission to hospital for COPD: results from the Copenhagen City Heart Study. Eur Respir J. 1999;13(5):1109–1114. doi: 10.1034/j.1399-3003.1999.13e28.x. [DOI] [PubMed] [Google Scholar]
- 12.Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–1257. doi: 10.1183/09031936.00133805. [DOI] [PubMed] [Google Scholar]
- 13.Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962–969. doi: 10.1183/09031936.00012408. [DOI] [PubMed] [Google Scholar]
- 14.Gan WQ, Man SF, Sin DD. The interactions between cigarette smoking and reduced lung function on systemic inflammation. Chest. 2005;127(2):558–564. doi: 10.1378/chest.127.2.558. [DOI] [PubMed] [Google Scholar]
- 15.Burgel PR, Paillasseur JL, Caillaud D, et al. Initiatives BPCO Scientific Committee Clinical COPD phenotypes: a novel approach using principal component and cluster analyses. Eur Respir J. 2010;36(3):531–539. doi: 10.1183/09031936.00175109. [DOI] [PubMed] [Google Scholar]
- 16.de Miguel Diez J, Carrasco Garrido P, García Carballo M, et al. Determinants and predictors of the cost of COPD in primary care: a Spanish perspective. Int J Chron Obstruct Pulmon Dis. 2008;3(4):701–712. doi: 10.2147/copd.s2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jansson SA, Andersson F, Borg S, Ericsson A, Jönsson E, Lundbäck B. Costs of COPD in Sweden according to disease severity. Chest. 2002;122(6):1994–2002. doi: 10.1378/chest.122.6.1994. [DOI] [PubMed] [Google Scholar]
- 18.Faganello MM, Tanni SE, Sanchez FF, Pelegrino NR, Lucheta PA, Godoy I. BODE index and GOLD staging as predictors of 1-year exacerbation risk in chronic obstructive pulmonary disease. Am J Med Sci. 2010;339(1):10–14. doi: 10.1097/MAJ.0b013e3181bb8111. [DOI] [PubMed] [Google Scholar]
- 19.Masa JF, Sobradillo V, Villasante C, et al. Costes de la EPOC en España. Estimación a partir de un estudio epidemiológico poblacional. [Costs of chronic obstructive pulmonary disease in Spain. Estimation from a population-based study.] Arch Bronconeumol. 2004;40(2):72–79. doi: 10.1016/s1579-2129(06)60198-5. Spanish. [DOI] [PubMed] [Google Scholar]
- 20.Hoogendoorn M, Feenstra TL, Hoogenveen RT, Al M, Mölken MR. Association between lung function and exacerbation frequency in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:435–444. doi: 10.2147/COPD.S13826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menn P, Heinrich J, Huber RM, et al. KORA Study Group Direct medical costs of COPD – an excess cost approach based on two population-based studies. Respir Med. 2012;106(4):540–548. doi: 10.1016/j.rmed.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000;320(7245):1297–1303. doi: 10.1136/bmj.320.7245.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]