Abstract
Skeletal structures act as lever arms during walking. Muscle activity and the ground reaction against gravity exert forces on the skeleton, which generate torque (moments) around joints. These lead to the sequence of movements which form normal human gait. Skeletal deformities in cerebral palsy (CP) affect the function of bones as lever arms and compromise gait. Lever arm dysfunction should be carefully considered when contemplating treatment to improve gait in children with CP.
Keywords: Gait, Cerebral palsy, Lever arm
Introduction
Normal gait relies on the integrity of the musculo-skeletal system and its neurological control. Appropriate and timely muscle activity, controlled by the central nervous system, generates forces across the skeleton. These forces lead to the generation of the sequence of movements necessary in walking. Gravity and its counterpart, the reaction force from the ground, are used in an optimal way to stabilise joints and minimise energy expenditure. During this sequence of events, the bones act as rigid lever arms, facilitating the application of torque on the joints.
The primary neurological impairment caused by the brain injury in cerebral palsy (CP) affects muscle tone, selective control, co-ordination and balance. Although the neurological impairment is static, its musculo-skeletal manifestations are progressive, particularly during growth. Muscle contractures may develop over time, due to increased tone and reduced mobility, and these can lead to joint contractures and reduced joint range of movement. Secondary bone deformities can develop in the lower limbs. Foot deformities are commonly caused by muscle imbalance and abnormal loading. These secondary musculo-skeletal deformities add significantly to the motor impairment of children with CP. The motor control of the body, which is already impaired by the neurological deficit, is further compromised by these deformities. This leads to additional challenges in the child’s ability to ambulate.
The detrimental effect of secondary musculo-skeletal deformity on motor function is mainly due to the compromised function of the normal lever arm. Deformed bones, stiff joints and foot deformities all affect the ability of the skeleton to adequately respond to forces generated by muscle activity. Furthermore, the compromised lever arm prevents adequate transfer of forces and torques arising from the ground reaction force (GRF).
When considering gait management options in children with CP, it is important to distinguish between problems arising from the primary neurological compromise and those caused by the secondary musculo-skeletal deformities. When considering the management of musculo-skeletal deformity, optimal treatment of the lever arm dysfunction can lead to significant improvements in gait. Therefore, adequate understanding of lever arm dysfunction in CP gait is of paramount importance when considering management options.
Basic principles of gait biomechanics
A force acting upon a lever arm attached to a fulcrum will generate torque, which is quantifiable as a moment. The amount of torque generated is proportional to the force applied and to the length of the lever arm. This is expressed by the formula M = F × D, where M is the moment and F the force. D is the distance between the point where the force is applied and the fulcrum, i.e. the length of the lever arm. In the human body, forces are generated by muscles and are applied at the point of muscle attachment on the bone. In a simplified example, the bone will act as a lever arm and the adjacent joint as a fulcrum. Considering the function of the hip abductor muscles, the force is applied on their attachment to the greater trochanter. The lever arm is represented by the distance between the force vector and the fulcrum, i.e. the centre of rotation of the hip joint. Any muscle weakness or lever arm problem (short femoral neck, coxa breva) will compromise the abductor moment and will lead to a gait deviation, such as a Trendelenburg gait.
Gravity plays an important role during gait, as it also affects the forces and moments generated around joints. According to Newton’s third law, for every force, there is an equal and opposite reaction. Gravity is applied on the ground, through the point of contact of the foot (or feet). This generates an opposite force, defined as the GRF. There are additional forces to consider, including those generated by friction and inertia. For simplicity, however, the GRF is represented as a single vector from the point of contact with the ground to the centre of gravity of the body. As the body moves forward during gait, the size and orientation of the GRF changes continuously. The GRF can be measured using force plates placed on the ground. The graphic representation of the evolution of the GRF vector in the sagittal plane during a gait cycle produces a characteristic “butterfly” shaped curve (Fig. 1).
Fig. 1.
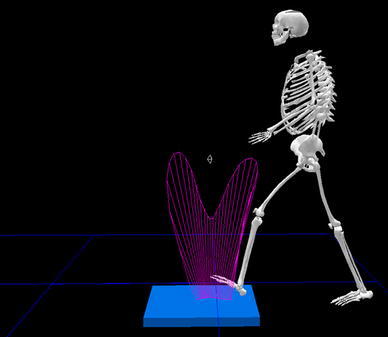
Picture of a Pedotti diagram
During walking, the GRF generates moments around the lower limb joints. The direction of such a moment around a joint depends on the position of the GRF vector in relation to the joint. For example, if the GRF vector is anterior to the knee joint, it will generate an extensor moment. This is often the case in plantarflexor tightness causing forefoot loading (toe-walking). This causes the GRF to displace forward, generating an excessive knee extensor moment and to cause knee hyperextension (Fig. 2). The magnitude of the moment generated around a joint by the GRF depends on the magnitude of the force vector and its distance from the joint. This follows the formula M = F × D discussed above. An example of this concept can be seen in patients with severe crouch gait. As a result of the increased knee flexion, the GRF vector is posterior to the knee joint by a significant distance, causing an increased flexor moment at the knee. Patients often lean their trunk forward to displace the centre of gravity and the GRF anteriorly, thus reducing the flexor moment.
Fig. 2.
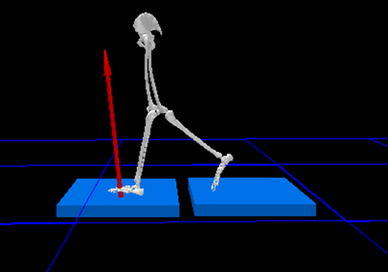
Picture showing knee hyperextension with vector
During normal gait, the GRF is used to optimise moments around the joints and to reduce, as much as possible, the muscle activity required to maintain upright posture and forward propulsion. This minimises the energy expenditure during gait. Muscle activity counter-balances the moments generated by the GRF and facilitates the sequence of joint movements necessary during walking. The three ankle rockers represent a characteristic example of how the GRF and the muscle activity work together in producing an optimal effect. During the first rocker, the eccentric activity of the dorsiflexors allows the smooth plantarflexion of the foot from the initial contact of the heel to the full placement of the whole of the plantar surface of the foot to the ground, whilst the GRF moves from the heel to the centre of the foot. During the second rocker, the plantar surface of the foot stays in full contact with the ground whilst the body progresses forward over it. The forward progress of the tibia is allowed by dorsiflexion of the ankle. The smooth progression of the tibia is controlled by the eccentric activity of the plantarflexors, whilst the GRF progresses further forward. During the third rocker, the plantarflexors act concentrically, leading to plantarflexion of the ankle. The loading is transferred fully to the forefoot as the heel leaves the ground. The rigid foot acts as a lever arm of the plantarflexors. The transfer of the loading to the forefoot generates a strong moment as the lever arm (the length of the foot) is longer and this facilitates the “push-off” or forward propulsion in this phase of gait. The gradual anterior advancement of the GRF from the heel to the forefoot during the three ankle rockers has beneficial effects at the knee and hip, facilitating flexion during load acceptance and extension during the late stance (Fig. 3).
Fig. 3.
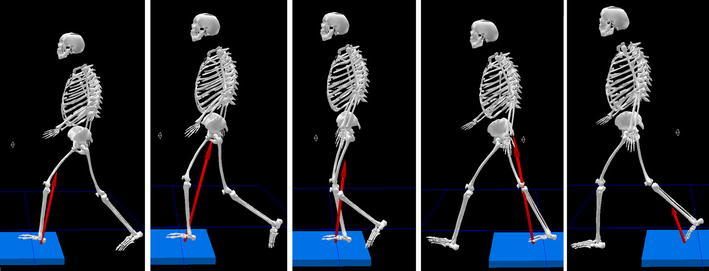
Picture showing progression of the ground reaction force (GRF) during stance
Lever arm deformities in cerebral palsy
The most usual skeletal deformities causing lever arm dysfunction in CP include increased femoral anteversion, external tibial torsion and deformities of the foot. Joint contractures also cause lever arm dysfunction, as they prevent the adequate torque generation of muscles across joints and the optimal use of the GRF in controlling joint movements.
Increased femoral anteversion in CP may represent a failure of remodelling of the foetal anteversion. It is believed that upright posture and full hip extension contribute to the remodelling of foetal anteversion in able-bodied young children. The anterior hip capsule and ligaments probably exert forces on the proximal femur during upright standing, which lead to the reduction of femoral anteversion during the first few years of life. As children with CP are usually late to walk and often do not achieve a fully upright posture with full extension at the hip, it is probable that they fail to remodel the proximal femur. Abnormal loading of the hip and proximal femur caused by abnormal posture and gait may also contribute to this problem.
Increased femoral anteversion is associated with internal hip rotation during gait in children with CP. It is probable that femoral anteversion is not the only cause of internal hip rotation, as distal rotational deviations and abnormal muscle activity are also known to contribute to this problem. From the biomechanical point of view, however, it is evident that increased femoral anteversion compromises the lever arm of the hip abductors as the projection of the femoral neck length in the frontal (coronal) plane is shortened. Internal hip rotation may, therefore, represent a compensation to bring the full femoral neck length to the frontal plane and increase the lever arm of the abductors. Multiple clinical studies have shown that surgical correction of the femoral anteversion through derotation osteotomy can correct the internal hip rotation during gait in the short- to mid-term. However, there is a risk of recurrence in the long-term, which indicates that factors other than increased femoral anteversion play a role in this problem.
Internal hip rotation during gait also affects the loading of the knee and the foot. As the whole limb is internally rotated, the projection of the lever arm of forces acting in the sagittal plane is shortened. For example, the internally rotated foot will represent a poor lever arm during push-off, as its projected length in the sagittal plane is shortened.
External tibial torsion is also common in ambulant children with CP, particularly in those with bilateral involvement. This deformity probably develops over time and is associated with equino-valgus foot deformity. Loading of the valgus foot in combination with flexion and internal rotation of the knee would generate torsional forces on the tibia, leading to remodelling towards external torsion. This compromises the alignment between the knee and the foot in the transverse plane. The plantarflexors’ moment is, therefore, compromised as the projected length of the foot in the sagittal plane is shortened and the lever arm is inadequate. This further affects any pre-existing weakness of the plantarflexors. The inadequate plantarflexor moment has a detrimental effect on knee extension. The ineffective plantarflexors allow the tibia to progress forward during stance and cause excessive ankle dorsiflexion. This, in turn, allows the knee to flex excessively, leading to a crouched gait. Derotation osteotomy of the tibia, together with the correction of any foot deformity, can restore the plantarflexor moment and form a crucial part of surgical correction of the lever arm deficiency. Adequate correction of any knee contracture in this situation will also restore adequate knee extension during the stance phase of gait.
Increased femoral anteversion and external tibial torsion often co-exist. This gives the appearance of valgus collapse at the knee. This appearance is usually due to the torsional effect of these deformities in combination with increased flexion at the knee, although true knee valgus can co-exist. Adequate correction of the torsional deformities together with the correction of any joint contractures and foot deformities can restore the lever arm and improve gait.
The most common foot deformity in young ambulant children with CP is dynamic equinus. This often progresses to fixed equinus and a secondary coronal plane foot deformity follows as the calcaneum is driven into varus or valgus by the tight plantarflexors. The coronal plane deformity can take the form of equino-varus, which is more common in unilateral CP, or equino-(plano)-valgus, which is more common in bilateral CP. Muscle imbalance, abnormal loading patterns, rotational gait deviations and intrinsic anatomical characteristics probably play a role in the development of these deformities. Internal rotation of the whole limb, weakness of the peronei and spasticity of the tibialis posterior are often associated with the equino-varus pattern. In equino-valgus deformity, the calcaneum is primarily driven into valgus by the tight plantarflexors. The everted position of the subtalar joint allows flexibility in the midfoot joints, which collapse and drive the forefoot in abduction. This is often described as a midfoot break.
The equinus foot deformity causes shortening of the plantarflexors’ lever arm, as the effective length of the foot is shortened. It is often compensated by flexion at the hip and knee or by knee hyperextension. These alterations in joint position affect the lever arm of both the GRF and the muscle forces, and compromise the efficiency of gait control.
Further compromise occurs with coronal plane foot deformity as the abnormal loading of the foot changes the direction of the GRF in the coronal plane. This affects the stability of the foot in stance and produces deleterious effects on proximal joints. Abnormal moments in the coronal and transverse planes occur as a result, leading to deviations in joint loading and motion. The equino-valgus foot alignment, for example, is often associated with increased knee flexion, a valgus knee thrust and internal hip rotation. The midfoot break, in particular, further affects the lever arm function as it compromises the rigidity of the foot, which is necessary for it to act as a lever. The effective length of the lever arm in this situation extends only between the heel and the midfoot. Adequate correction of foot deformity and/or the use of appropriately tuned orthoses can improve the foot function as a lever arm and restore stability and adequate loading patterns.
The role of gait analysis
The understanding of gait biomechanics and lever arm dysfunction in patients with CP is based on the background knowledge of normal gait mechanics, thorough clinical examination, gait observation and appropriate medical imaging. Instrumented three-dimensional analysis of gait can offer objective and quantifiable further information, which can substantiate the clinical assessment of gait. Kinematics demonstrate the three-dimensional motion of joints and body segments. Kinetics display the loading of joints and the moments acting on them based on their position in relation to the GRF at any given time during walking. Most gait analysis systems also offer the ability to observe the GRF vector on the patient’s video or on a skeletal model. This can help in the understanding of pathological patterns and the lever arm dysfunction. The additional information offered by dynamic electromyography can clarify abnormal muscle activity responsible for some gait deviations.
Conclusions
Skeletal structures act as lever arms during walking. Muscle activity and the ground reaction against gravity exert forces on the skeleton, which generate torque (moments) around joints. These lead to the sequence of movements which form normal human gait. Skeletal deformities in cerebral palsy (CP) affect the function of bones as lever arms and compromise gait. Lever arm dysfunction should be carefully considered when contemplating treatment to improve gait in children with CP.


