Hepatic resection is the gold-standard treatment for hepatocellular carcinoma (HCC). In East Asia, however, only 20 % of patients with HCC are eligible for hepatectomy [1]. In a small subset of patients, surgical resection using conventional techniques is extremely challenging. In these marginal cases, the tumor size, extension of the lesion, and proximity of the tumor to critical structures are important factors determining how to proceed. For tumors considered unresectable by conventional means, extracorporeal hepatic resection with autotransplantation (ECHRA) has been proposed to be an alternative [2].
ECHRA has been used to treat hepatic pathologies including giant hemangioma [3], liver metastases [4], and sarcomas [2]. However, few studies have reported on its application as a treatment for HCC [5]. Herein we report a case series involving three consecutive patients with HCC who were successfully treated with ECHRA as curative therapy for otherwise unresectable HCCs.
Patient Selection and Pre-operative Evaluation
In 2011, ECHRA was performed in three patients with liver tumors at anatomically critical locations that were deemed technically impossible to resect (Fig. 1). Patient characteristics and indications for this technique are outlined in Table 1. To ensure sufficient liver function after liver resection, we estimated pre- and post-operative liver volumes using 3-D computed tomography volumetry. Indocyanine green (ICG) test was performed in selected patients. None of the patients showed evidence of portal hypertension.
Fig. 1.
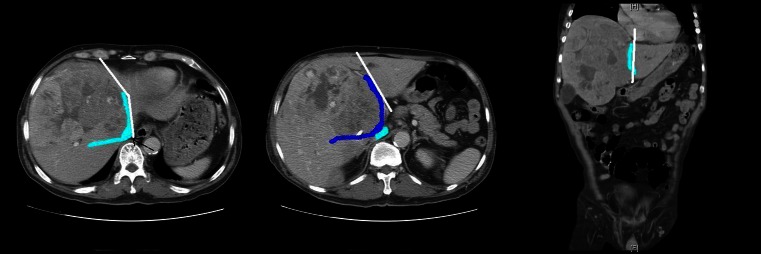
CT images of case series. a Large liver tumor with compression of the IVC (arrow), left hepatic vein and right hepatic vein. The middle hepatic vein has been obscured. The resection line (white line) follows the left hepatic vein. b Both the portal vein (navy blue) and IVC (dark blue) are compressed by the tumor. The resection line in this view follows the left portal vein. c Coronal illustration of the resection line (white line)
Table 1.
Patient characteristics
| Patient characteristics | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Age | 67 | 71 | 60 |
| Sex | M | M | M |
| ECOG | 0 | 0 | 0 |
| Pre-operative data | |||
| Hepatitis history | Non-B/C, alcoholism | Hepatitis B | Hepatitis C |
| AFP (ng/ml) | 357.59 | >270,000 | 24.25 |
| Platelet count (/μl) | 227 × 103 | 335 × 103 | 380 × 103 |
| INR | 1.22 | 1.28 | 0.93 |
| Evidence of PH | No | No | No |
| Tumor characteristics | |||
| Maximum diameter (cm) | 18 × 12 | 18 × 13 | 5.8 × 6.8 |
| Tumor location | S 1, 4, 5, 7, 8 | S 2, 3, 4, 5, 8 |
S 4, 5, 8; Satellite S7 |
| Indication for ECHRA (vascular involvement/tumor location) | At confluence of LHV, MHV, IVC | At confluence of V7/RHV into IVC | Centrally located, involve RHV, PV |
| Remnant liver volume (%)a | 44.26 | 34.46 | 51.00 |
ECOG Eastern Cooperative Oncology Group performance status, PH portal hypertension, S liver segment, LHV left hepatic vein, MHV middle hepatic vein, IVC inferior vena cava, V7 hepatic vein to segment 7, RHV right hepatic vein, PV portal vein
aRatio of remnant liver volume and standard liver volume
Surgery
ECHRA was performed as described previously with minor modifications [6]. Unlike previous reports, we employed temporary portocaval shunt during the anhepatic period (Fig. 2). In patients with tumor-invaded major vasculature, the vessel wall was pared and reconstruction with a venous patch harvested from the explanted liver (Fig. 3). Details of the surgery are given in Table 2. The affected segments of liver were resected after total hepatectomy and the autograft was re-implanted orthotopically. Pathology evaluation confirmed all three tumors to be HCC.
Fig. 2.
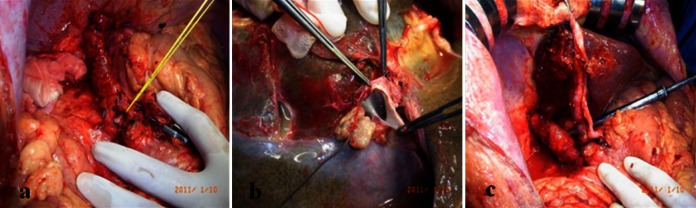
a Temporary portocaval shunt used during the anhepatic period. b Tumor thrombus found in the confluence of the hepatic veins. c Re-implantation of the graft
Fig. 3.
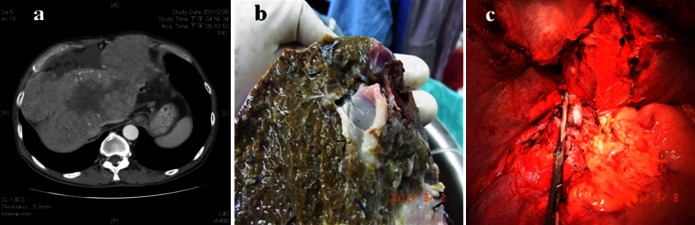
a Large HCC compressing the juncture of left hepatic vein and IVC. b Part of the IVC wall was excised and repaired with a venous patch (arrow). c Unification of V7 and right hepatic vein, which was later widened with a venous patch
Table 2.
Operation characteristics
| Operation (OP) details | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Replanted graft segments | S 2, 3, and partial S 4 | S 5–8 | S 2, 3, and S 6, 7 |
| Graft weight (g) | 440 | 696 | 961 |
| Blood loss (ml) | 1,500 | 5,300 | 7,000 |
| Cold ischemic time (min) | 120 | 202 | 162 |
| Warm ischemic time (min) | 40 | 14 | 43 |
Results and Outcome
The outcomes are outlined in Table 3. Patient 3 had major complications included postoperative biliary leakage and intra-abdominal abscess, which were treated with endoscopic retrograde cholangiopancreatography and surgical drainage of the abscess, respectively. There was no hospital mortality.
Table 3.
Postoperative data
| Post-op data | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| ICU days (days) | 8 | 7 | 8 |
| Length of stay (days) | 30 | 22 | 39 |
| Ishak score | 3 | 3 | 4 |
| Metavir fibrosis score | F2 | F2 | F3 |
| Post-op complication |
1. Sepsis 2. Transient hepatic insufficiency |
1. Sepsis 2. Transient hepatic insufficiency |
1. Sepsis 2. Transient hepatic insufficiency 3. Biliary leakage 4. Intra-abdominal abscess |
| Intervention | None | None | ERCP for biliary leakage |
| Reoperation | None | None | Laparotomy for drainage of abscess |
| Long-term follow-up | |||
| Recurrence | None | In post-op 8 month | In post-op 8 month |
| Management for recurrence | None | RFA | TACE |
| Current status | Alive (28 months) | Alive (26 months) | Alive (23 months)a |
RFA radiofrequency ablation, TACE transarterial chemoembolization
aAlive until May, 2013
Two of the three patients experienced tumor recurrence 8 months after the operation. Patient 2 was treated with radiofrequency ablation while the other was treated by transarterial chemoembolization. All patients are currently alive with stable disease at the most recent follow-up.
To date, the only large series involving ECHRA was reported by Oldhafer et al. [7]. The difficulty of the surgical technique and the high perioperative and postoperative morbidity impede surgeons from using this procedure. We are the first institution to use preoperative liver volumetry to prevent postoperative hepatic failure, the most serious complication. The preoperative evidence of preserved liver function and without liver cirrhosis or portal hypertension were other determinants for a good outcome. The three patients did well after the operation. In the literature reporting patients with HCC receiving ECRHA, our first patient had the longest survival [5, 7].
Unlike other studies, we used a temporary portocaval shunt instead of venovenous bypass to facilitate hemodynamic stability during the anhepatic period. Temporary portocaval shunts have been shown to improve hemodynamic status, reduce requirement of intraoperative blood transfusion, and preserve renal function during orthotopic liver transplantation [8]; however, it has not been reported to be used in ECHRA. We believed that the relatively short cold ischemic time and preservation of the inferior vena cava enhanced the functionality of the temporary portocaval shunt during the anhepatic period.
Conclusions
ECHRA represents an additional surgical option in the treatment of unresectable hepatic tumors, including HCC. In addition, the use of a temporary portocaval shunt is a feasible alternative to venovenous bypass during the anhepatic period.
References
- 1.Morris-Stiff G, Gomez D, de Liguori Carino N, Prasad KR. Surgical management of hepatocellular carcinoma: is the jury still out? Surg Oncol. 2009;18:298–321. doi: 10.1016/j.suronc.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Gruttadauria S, Marsh JW, Bartlett DL, Gridelli B, Marcos A. Ex situ resection techniques and liver autotransplantation: last resource for otherwise unresectable malignancy. Dig Dis Sci. 2005;50:1829–1835. doi: 10.1007/s10620-005-2946-5. [DOI] [PubMed] [Google Scholar]
- 3.Ikegami T, Soejima Y, Taketomi A, et al. Extracorporeal hepatic resection for unresectable giant hepatic hemangiomas. Liver Transpl. 2008;14:115–117. doi: 10.1002/lt.21272. [DOI] [PubMed] [Google Scholar]
- 4.Hemming AW, Cattral MS. Ex vivo liver resection with replacement of the inferior vena cava and hepatic vein replacement by transposition of the portal vein. J Am Coll Surg. 1999;189:523–526. doi: 10.1016/S1072-7515(99)00192-1. [DOI] [PubMed] [Google Scholar]
- 5.Sugimachi K, Shirabe K, Taketomi A, et al. Successful curative extracorporeal hepatic resection for far-advanced hepatocellular carcinoma in an adolescent patient. Liver Transpl. 2010;16:685–687. doi: 10.1002/lt.22051. [DOI] [PubMed] [Google Scholar]
- 6.Pichlmayr R, Grosse H, Hauss J, Gubernatis G, Lamesch P, Bretschneider HJ. Technique and preliminary results of extracorporeal liver surgery (bench procedure) and of surgery on the in situ perfused liver. Br J Surg. 1990;77:21–26. doi: 10.1002/bjs.1800770107. [DOI] [PubMed] [Google Scholar]
- 7.Oldhafer KJ, Lang H, Schlitt HJ, et al. Long-term experience after ex situ liver surgery. Surgery. 2000;127:520–527. doi: 10.1067/msy.2000.105500. [DOI] [PubMed] [Google Scholar]
- 8.Figueras J, Llado L, Ramos E, et al. Temporary portocaval shunt during liver transplantation with vena cava preservation. Results of a prospective randomized study. Liver Transpl. 2001;7:904–911. doi: 10.1053/jlts.2001.27870. [DOI] [PubMed] [Google Scholar]


