Abstract
A detailed epidemiologic survey of spontaneous diseases of mice used in biomedical research has not been performed in more than 4 decades. The current study examined all mouse disease reports for a subset of the University of Pennsylvania vivaria from October 2010 through September 2011. Mortality logs were examined over the same period of time. After eliminating protocol-related cases, the incidence rates for more than 30 diseases were calculated in terms of number of cases per 1000 cages per month. The average daily census for the facilities analyzed exceeded 29,000 cages and included more than 180 research groups. No single research group accounted for more than 4% of the total number of cases reported, indicating that this study did not simply quantify the spontaneous disease incidence in a limited number of research groups. Spontaneous mortality with unknown cause in adult and neonatal mice without prior reported illness was the most commonly reported issue, followed by dermatitis, ocular disease, and nonspecific clinical signs including lethargy, poor hair coat, and muscle wasting. These results indicate that improving the ability to identify sick mice is important in refining the care and use of mice in biomedical research. The information provided in the current study can help to provide a baseline for comparison, guide the field in directing mouse welfare research toward areas of need, and identify optimal methods of care for mice in biomedical research.
Abbreviation: CPM, cases per 1000 cages per month
Epidemiology studies the distribution and determinants of disease in a population and commonly involves the calculation of the incidence of disease in an at-risk population. With this information, healthcare providers can focus their attention on the areas of greatest need. Most epidemiologic studies in mice used in biomedical research historically have focused on the prevalence of infectious agents.3,4,13,15,21,22,26,29,37 This attention was logical given the frequency of infectious agents and their effects on both the health of the mice and experimental outcomes. However, through a combination of improved diagnostics, rederivation of mice, and improved housing modalities, many of these infections have either been eradicated or greatly reduced in their incidence. In addition, epidemiologic studies in laboratory mice have revealed disease incidence rates within narrowly defined populations, such as specific strains of mice.2 However, many strains of mice in biomedical research are genetically manipulated, some genetic drift occurs within each strain, and there are differences in housing conditions and experimental protocols, so that information on a single strain does not provide the ability to determine the overall rate of spontaneous diseases in mice used in biomedical research.
There are myriad factors that make studying the epidemiology of spontaneous mouse diseases a difficult undertaking. Mice frequently present with protocol-related, experimentally induced lesions, which are specific to the model of disease. As mentioned earlier, hundreds of strains of inbred and outbred mice exist, each of which may have unique disease susceptibility. Further confounding this difficulty is the use of genetically manipulated mice, which may be predictably altered in phenotype but frequently present with other unexpected abnormalities, including direct and indirect consequences of altered immune function. These consequences, combined with intentional immunosuppression, either due to genetics, radiation, or pharmacology, are very common in mice used in biomedical research and will alter their susceptibility to normally benign opportunistic bacterial and viral infections.
The epidemiology of infections in pet and wild mice provides limited useful information related to mice used in biomedical research. Many of the infectious diseases that have been eliminated in laboratory rodents continue to be prevalent in pet and wild mouse populations.22,29 In addition, most mice in biomedical research are maintained under tightly regulated housing conditions, as recommended in the Guide for the Care and Use of Laboratory Animals,14 which can alter disease prevalence. Two studies from the 1950s and 1960s attempted to estimate disease prevalence in research mice by surveying institutions involved in biomedical research.18,31 These studies report disease rates according to the number of institutions reporting the disease. Because no in-depth attempt was made to report the incidence rate for each of the diseases, combined with the profoundly improved biosecurity approaches used now for animals in biomedical research, there is little value in extrapolating these results to the current rate of disease in research mice.
The practice of field epidemiology relies on admittedly imperfect databases, compared with data collected prospectively in controlled studies, to provide reasonable estimates of disease incidence.36 The mouse vivaria at the University of Pennsylvania provided an ideal location to undertake the current investigation for several reasons: mice are housed in both barrier and conventional facilities; as discussed below, no individual researcher accounts for a large percentage of mice included in any single facility (meaning that the study did not examine disease rates in a single research colony); each facility represents a heterogeneous mix of research projects and disease models (no facility was dedicated to a particular type of research); and a comprehensive sentinel monitoring system provides excellent surveillance of the mice for many of the common viruses, bacteria, and parasites of mouse colonies.
The current investigation was undertaken to document spontaneous disease rates in a large heterogeneous population of laboratory mice used in biomedical research. The benefits of this study are 2-fold: first, to provide a point of reference for institutions to evaluate the relevant prevalence of spontaneous diseases within their facilities; and second, to provide focus to the field of laboratory animal medicine in disease control efforts for mice.1,36,38 With a baseline for comparison, different husbandry and management techniques can be evaluated between institutions to optimize the care provided for mice in biomedical research.
Materials and Methods
We analyzed all ‘sick animal’ mouse cases reported from October 2010 through September 2011 to the University of Pennsylvania University Laboratory Animal Resources. The cases from 4 facilities were included in the study, in light of the size of the facility (Table 1) and the diversity of research being conducted within it. None of the facilities was designated for a specific type of research. Facilities included both barrier and conventional housing, used a variety of water treatments (for example, reverse-osmosis–purified, acidified, and hyperchlorinated), and included individually ventilated and static isolation cages.
Table 1.
Facilities included in the analysis
| Facility | Type | Water used | Watering system | Daily cage census (mean ± SE [range]) | Cage type | No. of mice per cage (mean ± SE) | No. of days on treatment (mean ± SE) |
| A | Barrier | Reverse-osmosis | Automatic | 10,345 ± 241 (8972–11,176) | Ventilated | 3.0 ± 0.1 | 6.4 ± 0.5 |
| B | Barrier and conventional | Acidified | Bottles | 6036 ± 152 (5457–7106) | Static | 2.6 ± 0.1 | 9.2 ± 0.9 |
| C | Barrier | Chlorinated | Bottles | 8669 ± 104 (8003–9143) | Static | 3.1 ± 0.1 | 6.1 ± 0.4 |
| D | Conventional | Chlorinated | Bottles | 4010 ± 85 (3480–4361) | Static | 3.1 ± 0.1 | 6.3 ± 0.4 |
| Total | 29,061 ± 346 (26,424–30,420) |
All supplies and food entering the barrier facilities are sterilized. Mice leaving barrier facilities may not return, although this is allowed in the conventional facilities.
All of the mice in the facilities were on active protocols approved by the University of Pennsylvania IACUC. The mice were housed in standard 7.5 in. × 11.5 in. × 5 in. polycarbonate cages (static isolation or ventilated; Ancare, Bellmore, NY) with 1/4-in. corncob bedding (Animal Specialties and Provisions, Quakertown, PA). IACUC guidelines allow as many as 5 adult mice per cage. All mice that were singly housed received either a Nestlet (Animal Specialties and Provisions) or some other form of enrichment, unless an exemption was granted by the IACUC. All husbandry materials in the barrier facilities were either autoclaved or irradiated. Cages were checked daily and typically were changed once weekly, with changes occurring more frequently if necessary (for example, mice with polyuria–polydipsia were changed 2 or 3 times weekly). Facility temperatures were maintained at 22.2 ± 1.1 °C (72 ± 2 °F); humidity was between 30% and 70% with 10 to 15 air changes hourly. Each facility had 24-h environmental monitoring, with notifications of deviations automatically sent to facility managers or onsite staff.
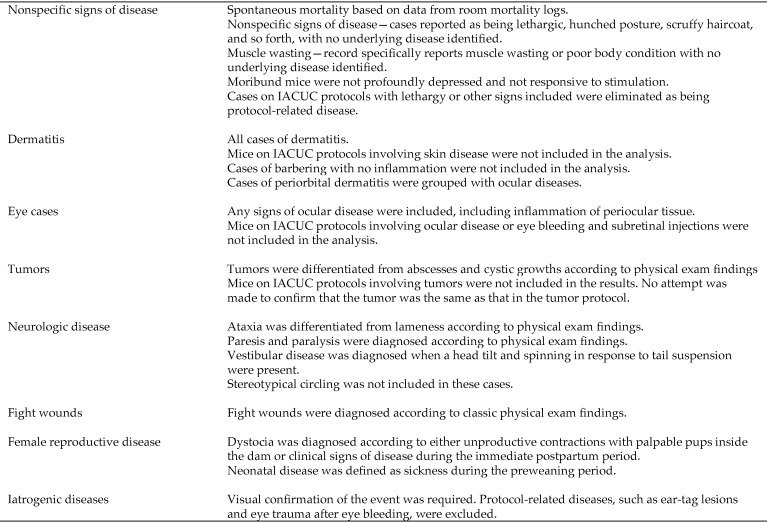
All cases were reported to University Laboratory Animal Resources by either an animal care technician or a member of the research staff. Cases were triaged by a certified veterinary technician within 48 h, unless the case was reported as an emergency and therefore was examined immediately. Mice then were examined by a veterinarian with training and expertise in laboratory animal medicine. The diagnosis or chief complaint was recorded as the main finding from either the veterinary exam or the veterinary technician's triage and was determined through examination of the medical records by one of the authors (JOM). Secondary observations and diagnoses were recorded for each case also. A description of the most common clinical diagnoses is included in Figure 1. An anatomic diagnosis was recorded for each case whenever possible (for example, tumor–abdomen, dermatitis–hindlimb, conjunctivitis). When an anatomic diagnosis could not be determined, the clinical signs were recorded (for example, lethargy, muscle wasting, eye closed). Other information recorded for each case included the date of the initial report, housing facility, room, principal investigator, approved IACUC protocol number, number of affected animals in the cage, and any other relevant comments. Any additional disease syndromes that developed during the course of treatment for the chief complaint were not included in the analysis. Room mortality logs, completed by the University Laboratory Animal Resources animal care staff, were used to calculate the number of cases of spontaneous mortality of unknown cause in the colonies.
Figure 1.
Descriptions of the diseases identified most frequently.
After all cases were recorded, protocol-related lesions were eliminated from the analysis. This elimination was done by a thorough review of all cases in comparison with the approved IACUC protocols and direct communication with research staff. For example, when a mass was reported on an animal maintained on a tumor-related protocol, we assumed that the mass or tumor was expected within the context of the study, and the case was removed as being protocol-related disease. Similar procedures were followed in experimental protocols relating to eye and skin diseases. Cases of lethargy, muscle wasting, or other nonspecific signs of illness were eliminated only when the symptom was described in the protocol as an expected outcome of the experimental study. Because spontaneous deaths in the mortality logs could not be assumed to be protocol-related, all reported deaths were included in the analysis. This inclusion consequently inflates the numbers of deaths because of our inability to exclude these cases. Barbering and alopecia, without inflammation, were not reported as clinical cases, and cases of infertility and decreased reproductive performance reported by laboratories were not reported as clinical disease but instead were addressed as nonclinical protocol-related issues by the veterinary staff. Cases of clinical disease associated with husbandry or animal handling were grouped as iatrogenic diseases.
Cases were grouped according to type of disease, that is, dermatitis, ocular disease, neurologic disease, tumors, and so forth. Incidence rates were calculated as the number of affected animals per 1000 cages per month (CPM), and the number of affected animals per 5000 mice per month. Many epidemiology studies report data in terms of cases per susceptible subjects in the population.36 However, reporting cases according to the total number of mice in the vivaria may not be particularly valuable to laboratory animal veterinary staff, because doing so requires knowledge of the exact number of mice in the facility, which is highly variable due to cages that can house 1 to 5 adult mice or various breeding schema that include litters of pups. Instead, many research facilities, including the University of Pennsylvania, maintain accurate counts of the total number of cages within facilities. We therefore determined the total cage census for each facility by scanning bar-coded cage cards on each cage once weekly. The average number of cages for each month was determined by averaging the scanning counts over the month. Once a cage was identified as being under treatment or observation, it was no longer included in the at-risk population. These cages were deleted from the at-risk population in the calculation of CPM by subtracting the number of new cases each month by the average time a cage was under treatment or observation. This average time was calculated as the average of the first 200 cases identified in each facility (Table 1). Incidence rate also was determined on the basis of the number of cases per 5000 mice per month.
The number of at-risk mice was determined by multiplying the total number of cages by the average number of mice in each cage, determined independently for each facility by averaging the number of mice in 200 cages from each facility. Cages with 2 mice affected by a disease therefore counted as 2 individual events. Cases of fight wounds were counted as a single event, independent of the number of mice with lesions within the cage, because frequently all of the mice in the cage except for the aggressor–dominant mouse presented with lesions, meaning that the total number of mice affected would simply be dependent on the total number of mice in the cage. Once treatments or observations ended on a case, it was eligible to be reported again as a new case. Diseases reported as more than 120 cases in the year (that is, 0.34 CPM or greater) were analyzed by facility and by month. Diseases reported between 40 times (0.11 CPM) and 120 cases in the year were analyzed by month but not by facility. Diseases occurring fewer than 40 times in the year were not subcategorized for further analysis.
The sentinel program was used to determine the effects of infectious diseases on the incidence rate of spontaneous diseases. The sentinel program uses female Swiss–Webster (Tac:SW) mice purchased at 5 to 6 wk of age from Taconic (Germantown, NY). A single sentinel cage housing 2 mice monitors each side of every rack on a quarterly schedule. Soiled bedding from each cage on a rack side is transferred weekly to its corresponding sentinel cage at cage change. During each of 3 quarters, the sentinel mice are examined onsite for fur mites and pinworms, and serology (ELISA) is performed by using antigens for mouse hepatitis virus, epizootic diarrhea of infant mice virus, Theiler virus, mouse minute virus, and mouse parvovirus. Antigen-coated plates are purchased from Charles River Laboratories (Wilmington, MA). Confirmatory testing, when required, is performed by indirect immunofluorescence using antigens prepared internally or provided by Dr Susan Compton (Yale University, New Haven, CT).
Live sentinel mice from each facility are shipped annually to Charles River Laboratories for more comprehensive monitoring. All sentinel mice are tested using the HM Plus profile (serology for 23 viral and bacterial agents; upper respiratory and gastrointestinal tract cultures; endo- and ectoparasites; and gross necropsy; http://www.criver.com/SiteCollectionDocuments/rm_ld_c_RADS_US_a.pdf), and lymph nodes from sentinel mice housed in barrier facilities are tested by PCR assay for mouse parvoviral DNA. The University of Pennsylvania does not exclude murine norovirus or Helicobacter spp. from its mouse housing facilities; in fact, both organisms are present enzootically. Over the surveyed year, excluded infectious or parasitic agents were identified in 7 rooms in sentinel animals (fur mites in 4 rooms in Facility C, mouse hepatitis virus in 2 rooms in Facility D, and mouse minute virus in one room in Facility D). In each case, the prevalence of the disease within the room was determined and an eradication plan enacted. The case reports within the affected rooms were examined for 4 mo before the diagnosis of the outbreak and for 3 mo after the diagnosis and treatment–eradication of the disease within the room.
For each disease occurring more than 120 times during the year, the incidence rates by season were estimated by using Poisson regression, with spring as the referent season (Stata 12.1, StataCorp, College Station, TX). After the Poisson regression and for each health outcome, we performed pairwise comparisons among the incidence rates for the other seasons. To ease the assumption of event independence, which is required with the Poisson regression approach, we corroborated the predictions of this approach with the use of negative binomial regression.8,12,27 When the results of the more conservative negative binomial regression approach indicated, we deferred to those. All statistical testing applied a 5% probability for statistical significance; when significant results were detected and to preserve this error rate, we adjusted the critical P value according to the method of Bonferroni when we performed the posthoc pairwise comparisons of incidence rates across seasons.
Results
A total of 4735 clinical cases fulfilled the criteria for inclusion in this study. The animal care staff reported 1670 other cases that were eliminated from the analysis because they fulfilled the criteria for protocol-related lesions. More than 180 research groups had mice included in the analysis. Within each facility, no principal investigator accounted for more than 16% of the total caseload for that facility or more than 4% of the total cases included in the analysis. This heterogeneity was important so that the data for each facility did not simply represent the spontaneous disease seen in a single research program or a small number of research groups. Spontaneous mortality occurred in 9527 adult and 6195 neonatal mice during the course of this study. These numbers are inevitably elevated relative to the incidence of the other diseases, because protocol-related deaths were not eliminated from these numbers.
Tables 2 and 3 report a breakdown of cases reported during the year. As the data show, spontaneous mortality with no previous signs of illness among both adults and neonates was the most commonly reported event in the colonies. As discussed earlier, these data include animals deaths associated with protocol-related procedures, potentially elevating these numbers compared with the other clinical diseases reported.
Table 2.
Incidence rate (CPM) and percentage of clinical cases for each disease
| Incidence rate (CPM) | ||||||||
| Facility A | Facility B | Facility C | Facility D | Overall | 95% confidence interval | % of clinical cases | ||
| Nonspecific systemic diseases | Spontaneous mortality with unknown cause—adults | 30.21 ± 0.48 (27.66–33.71) | 16.01 ± 1.14 (10.20–23.13) | 28.15 ± 1.01 (22.17–35.49) | 33.50 ± 1.37 (25.10–41.25) | 27.13 ± 0.54 (24.18–31.68) | 25.95–28.31 | |
| Spontaneous mortality with unknown cause—pups | 39.88 ± 2.82 (21.54–51.39) | 2.21 ± 0.56 (0.34–7.33) | 1.80 ± 0.28 (0.12–3.42) | 18.83 ± 2.95 (3.17–36.43) | 17.72 ± 1.08 (11.43–23.96) | 15.36–20.08 | ||
| Lethargy, poor haircoat, etc | 1.49 ± 0.24 (0.80–4.38) | 0.32 ± 0.10 (0.00–1.27) | 0.99 ± 0.15 (0.13–1.83) | 3.63 ± 0.33 (1.86–6.11) | 1.49 ± 0.13 (1.01–2.76) | 1.21–1.77 | 11.0 | |
| Muscle wasting | 0.73 ± 0.11 (0.22–1.46) | 0.16 ± 0.05 (0.00–0.65) | 0.78 ± 0.11 (0.13–1.60) | 1.94 ± 0.32 (0.58–4.69) | 0.79 ± 0.08 (0.36–1.28) | 0.61–0.97 | 5.6 | |
| Moribund | 0.24 ± 0.03 (0.10–0.44) | 0.18–0.30 | 1.8 | |||||
| Dermatitis | All anatomic locations | 2.51 ± 0.17 (1.43–3.33) | 1.75 ± 0.17 (0.51–2.98) | 1.97 ± 0.19 (0.57–3.20) | 9.08 ± 0.67 (5.66–12.97) | 3.11 ± 0.12 (2.57–4.02) | 2.85–3.37 | 21.7 |
| Ulcerative dermatitis and dermatitis of dorsal neck and pinnas | 1.42 ± 0.13 (0.55–2.12) | 1.14 ± 0.14 (0.51–2.10) | 0.85 ± 0.13 (0.23–1.59) | 4.69 ± 0.60 (1.62–8.83) | 1.65 ± 0.09 (1.17–2.30) | 1.46–1.84 | ||
| Face, muzzle, and nose | 0.51 ± 0.07 (0.18–0.84) | 0.20 ± 0.05 (0.00–0.67) | 0.29 ± 0.07 (0.00–0.68) | 1.57 ± 0.24 (0.58–3.42) | 0.52 ± 0.04 (0.30–0.84) | 0.44–0.60 | ||
| Back and flanks | 0.21 ± 0.07 (0.00–0.83) | 0.15 ± 0.06 (0.00–0.53) | 0.30 ± 0.06 (0.11–0.77) | 1.24 ± 020 (0.00–2.20) | 0.37 ± 0.03 (0.17–0.54) | 0.30–0.44 | ||
| Hindlimbs | 0.17 ± 0.02 (0.00–0.26) | 0.13–0.21 | ||||||
| Ventral neck | 0.12 ± 0.02 (0.00–0.20) | 0.08–0.16 | ||||||
| Base of tail and tail | 0.11 ± 0.02 (0.00–0.26) | 0.05–0.17 | ||||||
| Fight wounds | Fight wounds | 2.21 ± 0.06 (1.66–2.50) | 1.23 ± 0.14 (0.17–2.12) | 1.30 ± 0.16 (0.34–2.39) | 4.81 ± 0.54 (1.56–8.28) | 2.10 ± 0.06 (1.66–2.50) | 1.97–2.23 | 14.7 |
| Ocular lesions | Eye | 0.73 ± 0.13 (0.10–1.85) | 0.31 ± 0.07 (0.00–0.56) | 0.99 ± 0.27 (0.11–3.20) | 4.73 ± 0.13 (1.01–2.76) | 1.28 ± 0.13 (0.67–2.04) | 1.00–1.56 | 8.9 |
| Female reproductive and neonatal diseases | Dystocia | 0.81 ± 0.08 (0.30–1.50) | 0.04 ± 0.03 (0.00–0.57) | 0.19 ± 0.05 (0.00–0.57) | 0.57 ± 0.09 (0.00–1.39) | 0.43 ± 0.04 (0.24–0.68) | 0.35–0.51 | 3.0 |
| Neonates with clinical disease | 0.86 ± 0.08 (0.30–1.29) | 0.11 ± 0.04 (0.00–0.35) | 0.13 ± 0.03 (0.00–0.34) | 0.76 ± 0.12 (0.23–1.72) | 0.48 ± 0.02 (0.34–0.62) | 0.43–0.53 | 3.3 | |
| Prolapsed vagina or uterus | 0.14 ± 0.03 (0.03–0.40) | 0.08–0.20 | 1.0 | |||||
| Tumors | Tumors | 0.72 ± 0.10 (0.19–1.54) | 0.34 ± 0.07 (0.00–0.69) | 0.63 ± 0.14 (0.13–1.94) | 3.08 ± 0.48 (1.08–6.35) | 0.94 ± 0.08 (0.47–1.45) | 0.76–1.12 | 6.5 |
| Malocclusion | Malocclusion | 0.35 ± 0.05 (0.09–0.64) | 0.14 ± 0.04 (0.00–0.42) | 1.19 ± 0.19 (0.46–3.31) | 0.98 ± 0.17 (0.00–1.95) | 0.65 ± 0.06 (0.44–1.24) | 0.53–0.77 | 4.5 |
| Prolapsed rectum | Prolapsed rectum | 0.70 ± 0.06 (0.27–1.02) | 0.17 ± 0.06 (0.00–0.73) | 0.36 ± 0.06 (0.11–0.84) | 1.03 ± 0.15 (0.00–1.72) | 0.54 ± 0.04 (0.34–0.83) | 0.46–0.62 | 3.7 |
| Iatrogenic disease | Watering failures | 0.23 ± 0.03 (0.03–0.44) | 0.16–0.30 | 1.7 | ||||
| Iatrogenic lameness | 0.07 | 0.5 | ||||||
| Neurologic disease | Head tilt | 0.29 ± 0.04 (0.00–0.57) | 0.20–0.38 | 2.1 | ||||
| Paresis, paralysis | 0.18 ± 0.02 (0.03–0.27) | 0.14–0.22 | 1.3 | |||||
| Hydrocephalus | 0.17 ± 0.03 (0.03–0.40) | 0.11–0.23 | 1.2 | |||||
| Ataxia | 0.05 | <1 | ||||||
| Male urogenital diseases | Prolapsed penis | 0.20 ± 0.03 (0.03–0.36) | 0.13–0.27 | 1.5 | ||||
| Preputial gland disease | 0.12 ± 0.02 (0.00–0.30) | 0.07–0.17 | <1 | |||||
| Miscellaneous | Secondary Enterobacter infections in immunosuppressed mice | 0.28 ± 0.10 (0.00–1.11) | 0.07–0.49 | 2.0 | ||||
| Distended abdomen, ascites | 0.15 ± 0.02 (0.04–0.37) | 0.10–0.20 | 1.1 | |||||
| Lame | 0.14 ± 0.04 (0.00–0.27) | 0.05–0.23 | 1.1 | |||||
| Abscesses (not involving the preputial gland) | 0.07 | <1 | ||||||
| Perineal hernia or scrotal disease | 0.06 | <1 | ||||||
| Respiratory disease | 0.05 | <1 | ||||||
Data are presented as mean ± SE (range). Diseases reported more than 120 times were analyzed by both facility and month. Diseases reported between 40 and 120 times were analyzed by month, with all of the facilities pooled. Diseases reported fewer than 40 times were analyzed as cases during the year by total number of cages in all 4 facilities.
Table 3.
Incidence rate (no. of cases per 5000 mice per month; mean ± SE) for each disease
| Facility A | Facility B | Facility C | Facility D | Overall | 95% Confidence interval | ||
| Nonspecific systemic diseases | Spontaneous mortality with unknown cause adults | 50.35 ± 0.88 (46.11–56.18) | 30.78 ± 2.37 (19.62–44.48) | 45.10 ± 1.77 (35.76–57.23) | 54.06 ± 2.41 (40.48–66.52) | 45.82 ± 1.00 (40.81–53.47) | 43.62–48.02 |
| Spontaneous mortality with unknown cause pups | 66.46 ± 5.10 (35.90–85.64) | 4.25 ± 1.16 (0.65–14.10) | 2.91 ± 0.49 (0.19–5.52) | 30.41 ± 5.18 (5.11–58.76) | 29.93 ± 2.00 (19.30–40.69) | 25.53–34.33 | |
| Lethargy, poor haircoat, etc | 2.87 ± 0.43 (1.34–7.29) | 0.62 ± 0.21 (0.00–2.44) | 1.60 ± 0.27 (0.20–2.94) | 5.86 ± 0.59 (3.00–9.85) | 2.51 ± 0.23 (1.70–4.66) | 2.00–3.02 | |
| Muscle wasting | 1.21 ± 0.15 (0.37–2.44) | 0.31 ± 0.11 (0.00–1.25) | 1.26 ± 0.19 (0.20–2.58) | 3.13 ± 0.55 (0.93–7.57) | 1.34 ± 0.15 (0.61–2.16) | 1.01–1.67 | |
| Moribund | 0.41 ± 0.05 (0.17–0.74) | 0.29–0.53 | |||||
| Dermatitis | All anatomic locations | 4.19 ± 0.30 (2.39–5.54) | 3.37 ± 0.36 (0.97–5.73) | 3.18 ± 0.34 (0.92–5.15) | 14.65 ± 1.17 (9.13–20.92) | 5.24 ± 0.22 (4.34–6.78) | 4.76–5.72 |
| Ulcerative dermatitis and dermatitis of dorsal neck and pinnas | 2.36 ± 0.22 (0.92–3.54) | 2.19 ± 0.26 (0.97–4.05) | 1.36 ± 0.21 (0.37–2.56) | 7.57 ± 0.97 (2.61–14.24) | 2.78 ± 0.15 (1.98–3.90) | 2.46–3.10 | |
| Face, muzzle, and nose | 0.84 ± 0.12 (0.31–1.40) | 0.38 ± 0.10 (0.00–1.30) | 0.47 ± 0.12 (0.00–1.10) | 2.53 ± 0.39 (0.93–5.52) | 0.88 ± 0.06 (0.51–1.42) | 0.74–1.02 | |
| Back and flanks | 0.35 ± 0.11 (0.00–1.39) | 0.29–0.12 (0.00–1.01) | 0.49–0.10 (0.18–1.24) | 2.00 ± 0.32 (0.00–3.55) | 0.62 ± 0.06 (0.29–0.92) | 0.50–0.74 | |
| Hindlimbs | 0.28 ± 0.03 (0.11–0.43) | 0.21–0.35 | |||||
| Ventral neck | 0.20 ± 0.03 (0.00–0.34) | 0.13–0.27 | |||||
| Base of tail and tail | 0.19 ± 0.04 (0.00–0.43) | 0.09–0.29 | |||||
| Fight Wounds | Fight wounds | 3.68 ± 0.25 (2.33–5.65) | 2.35 ± 0.30 (0.33–4.07) | 2.10 ± 0.28 (0.55–3.85) | 7.76 ± 0.95 (2.52–13.36) | 3.54 ± 0.11 (2.80–4.24) | 3.29–3.79 |
| Ocular lesions | Eye | 1.22 ± 0.24 (0.17–3.08) | 0.60 ± 0.14 (0.00–2.44) | 1.59 ± 0.47 (0.18–5.15) | 7.64 ± 0.81 (3.79–12.51) | 2.16 ± 0.24 (1.24–3.45) | 1.64–2.68 |
| Female reproductive and neonatal diseases | Dystocia | 1.34 ± 0.15 (0.50–2.50) | 0.08 ± 0.06 (0.00–0.68) | 0.31 ± 0.09 (0.00–0.92) | 0.92 ± 0.16 (0.00–2.25) | 0.73 ± 0.06 (0.41–1.14) | 0.59–0.87 |
| Neonates with clinical disease | 1.43 ± 0.15 (0.50–2.15) | 0.22 ± 0.07 (0.00–0.68) | 0.22 ± 0.05 (0.00–0.55) | 1.22 ± 0.21 (0.38–2.77) | 0.80 ± 0.04 (0.34–0.62) | 0.71–0.89 | |
| Prolapsed vagina or uterus | 0.24 ± 0.05 (0.06–0.67) | 0.12–0.35 | |||||
| Tumors | Tumors | 1.19 ± 0.19 (0.31–2.56) | 0.66 ± 0.14 (0.00–1.33) | 1.01 ± 0.24 (0.20–3.13) | 4.98 ± 0.85 (1.74–10.24) | 1.59 ± 0.15 (0.80–2.44) | 1.25–1.93 |
| Malocclusion | Malocclusion | 0.58 ± 0.09 (0.15–1.06) | 0.26 ± 0.09 (0.00–1.41) | 1.92 ± 0.34 (0.74–5.34) | 1.57 ± 0.30 (0.00–3.15) | 1.10 ± 0.10 (0.74–2.10) | 0.88–1.32 |
| Prolapsed rectum | Prolapsed rectum | 1.17 ± 0.12 (0.45–1.69) | 0.33 ± 0.12 (0.00–1.41) | 0.58 ± 0.10 (0.18–1.35) | 1.66 ± 0.26 (0.00–2.77) | 0.91 ± 0.07 (0.57–1.40) | 0.76–1.06 |
| Iatrogenic disease | Watering failure | 0.38 ± 0.06 (0.06–0.74) | 0.25–0.41 | ||||
| Iatrogenic lameness | 0.07 | ||||||
| Neurologic disease | Head tilt | 0.49 ± 0.08 (0.00–0.96) | 0.32–0.66 | ||||
| Paresis, paralysis | 0.30 ± 0.03 (0.06–0.46) | 0.22–0.38 | |||||
| Hydrocephalus | 0.29 ± 0.05 (0.06–0.68) | 0.19–0.39 | |||||
| Ataxia | 0.11 | ||||||
| Male urogenital diseases | Prolapsed penis | 0.34 ± 0.06 (0.06–0.61) | 0.22–0.46 | ||||
| Preputial gland disease | 0.20 ± 0.04 (0.00–0.51) | 0.11–0.29 | |||||
| Miscellaneous | Secondary Enterobacter infections in immunosuppressed mice | 0.47 ± 0.18 (0.00–1.88) | 0.08–0.86 | ||||
| Distended abdomen, ascites | 0.25 ± 0.04 (0.06–0.63) | 0.15–0.35 | |||||
| Lame | 0.24 ± 0.04 (0.00–0.45) | 0.16–0.32 | |||||
| Abscesses (not involving the preputial gland) | 0.14 | ||||||
| Perineal hernia or scrotal disease | 0.13 | ||||||
| Respiratory disease | 0.11 |
Diseases reported more than 120 times were analyzed by both facility and month. Diseases reported between 40 and 120 times were analyzed by month, with all of the facilities pooled. Diseases reported fewer than 40 times were analyzed as cases during the year by total number of mice in all 4 facilities.
Mice with nonspecific signs of disease, including lethargy, hunched posture, muscle wasting, scruffy haircoat or moribundity, for which an underlying pathology could not be identified on physical exam were divided into 3 groups. Mice with signs of lethargy, hunched posture, and poor haircoat were analyzed separately from those with muscle wasting, because muscle wasting infers some degree of chronicity, whereas the other clinical presentations may occur more acutely. Moribund mice were treated as another separate presentation. The rate of mice presenting with nonspecific clinical signs was 1.49 CPM; the rate was 0.80 CPM for muscle wasting; and the rate was 0.24 CPM for moribund mice. We did note that many cases that presented with illness fell into more than one of our categories, for example, they had both muscle wasting and the other nonspecific signs of disease. Of the 514 cases with nonspecific signs, 214 presented with muscle wasting, whereas 252 of 277 cases of muscle wasting presented with other nonspecific clinical signs. Eighteen of the 539 mice reported with nonspecific signs were found spontaneously dead within 24 h, indicating that 521, or 97%, either were treated sufficiently to survive until the following day or were euthanized.
The most common clinical disease entity was dermatitis, occurring at a rate of 3.10 cases CPM. Tables 2 and 3 report the anatomic distribution of these lesions, with the classic locations of ulcerative dermatitis accounting for 53% of the dermatitis cases. The proportion of cages with multiple mice affected by dermatitis was 6.2%.
Eye cases occurred at a rate of 1.28 CPM. Because of the small size of mice, many of the eye lesions were not reported as an anatomic diagnosis but instead were reported as clinical signs, such as cloudy eye, squinting, closed eye, and so on. Histopathologic review of eye lesions demonstrated that conjunctivitis (primary or secondary) was nearly ubiquitous in mice with eye lesions, with corneal and lens lesions being less prevalent.
Female reproductive and urogenital disorders were grouped with reports of neonatal mice, because we inferred that instances of neonatal disease typically are linked to maternal factors. The majority of sick neonatal mice presented with signs of dehydration, lethargy, poor body condition, and so on. Clinical reproductive disease in male mice occurred relatively rarely.
Water-delivery problems and iatrogenic lameness were the most commonly reported iatrogenic diseases. The vast majority of water problems were cases of watering failures, predominantly flooded cages, occurring in facility A, which is the only facility predominantly using an automatic watering system.
During the year, a colony of immunosuppressed mice in facility C developed a series of bacterial infections that resulted in secondary Enterobacter spp. infections. Because of their repeated nature, these infections were considered a separate disease from other bacteria-related diseases.
Seven viral or parasitic outbreaks were identified during the year of analysis. Further analysis of each of these outbreaks indicated that fewer than 5% of cages within each affected room were positive for the infectious agent. Outbreak eradication efforts included testing and culling of mice with viral infections and medical treatment for parasite-affected mice. In view of this low rate of infection, it is unsurprising that examination of the disease rates indicated no changes in the noninfectious diseases present in the room either before or after treatment or resolution of the infectious agent.
The rate of animal deaths in adult mice was similar among all 4 facilities. The rate of neonatal mice found dead in facility A was twice as high as the average in the other facilities. The overall rate of mice reported as sick was highest in facility D, which had twice the incidence rate of nonspecific diseases, dermatitis, and fight wounds compared with the overall disease incidence and 3 times the overall incidence rate of eye lesions and tumors. Statistical analysis revealed no significant seasonal affects in any of the reported diseases (Table 4).
Table 4.
Incidence (CPM; mean ± SE) of clinical diseases by season for diseases occurring at rates higher than 0.50 CPM over the year
| Disease | Spring | Summer | Fall | Winter |
| Dermatitis | 2.70 ± 0.09 | 3.41 ± 0.34 | 3.04 ± 0.39 | 3.01 ± 0.16 |
| Eye cases | 0.99 ± 0.30 | 1.39 ± 0.32 | 1.55 ± 0.38 | 1.20 ± 0.09 |
| Fight wounds | 2.27 ± 0.04 | 1.82 ± 0.08 | 2.23 ± 0.13 | 2.04 ± 0.05 |
| Tumors | 0.82 ± 0.13 | 1.04 ± 0.16 | 0.97 ± 0.25 | 0.93 ± 0.26 |
| Malocclusion | 0.64 ± 0.08 | 0.79 ± 0.23 | 0.63 ± 0.04 | 0.53 ± 0.08 |
| Prolapsed rectum | 0.53 ± 0.01 | 0.59 ± 0.07 | 0.56 ± 0.15 | 0.47 ± 0.07 |
Seasons were defined as Spring: March, April, and May; Summer: June, July, and August; Fall: September, October, and November; Winter: December, January, and February.
No significant seasonal effects were detected.
Discussion
This investigation was undertaken to provide a current appraisal of spontaneous diseases of mice in a contemporary biomedical research setting and to provide a basis for comparison with similar large institutions to evaluate the incidence rate of mouse spontaneous disease at their institution. Our large heterogeneous population of mouse models provided an excellent opportunity to study the epidemiology of spontaneous disease in mice used in biomedical research. Despite significant improvements in animal husbandry and infectious disease control since the 1980s,19,34 the current investigation suggests that one of the most important areas for improvement in mice used in biomedical research is the identification of sick mice. Ultimately, the recognition of mice that are systemically ill at an early stage of the disease is an area to target for continued improvement in biomedical research involving mouse models.
Spontaneous mortality in adult and neonatal mice without prior reported illness was the most commonly reported issue. Despite being checked daily, we theorize that there are 3 main reasons why the recognition of sick mice is challenging in a research setting. First, mice as a species are nocturnal but routinely are checked by staff during the workday; typically, the mice are huddled together and sleeping, masking potential clinical signs of disease, such as muscle wasting, skin and eye lesions, and lethargy. Mice may only be readily identified as being ill if they are separated from their cage mates, which is usually a sign of advanced disease. Second, mice are a prey species and, as with other prey species, will remain alert and active to avoid predation despite being ill until the disease has progressed to an advanced state.16 Last, mice have a high metabolic rate; therefore, disease progression can be more rapid than that in other, larger species, perhaps further narrowing the window of detection for sick mice prior to their demise and death.30,33 In the current investigation, 78 mice were identified as moribund, which enabled euthanasia and alleviation of potential suffering, and helps to demonstrate how little time mice spend in this advanced diseased state. Potential solutions to aid in the recognition of sick mice, including activity monitoring and the examination of mice during the dark cycle of their circadian rhythm, are fraught with their own challenges of finances to incorporate equipment and personnel to check mice at night. In addition, checks during the dark cycle could have a high risk of negatively affecting experimental studies.
Mice that were reported with nonspecific lesions (dehydration, lethargy, muscle wasting, poor hair coat, and so on) were another common finding in this study. There are myriad common clinical diseases that are difficult to diagnose in mice until they have reached an advanced stage with overt adverse effects on the mice. These include renal disease (amyloidosis, glomerular disease, chronic progressive nephropathy), cardiac disease (atrial thrombosis), nonpalpable tumors (bone marrow, thoracic cavity tumors, hematopoietic neoplasia), and diseases of the oral cavity (foreign-body periodontitis).2,20,23,25,34 Even with the aid of a diagnostic necropsy, approximately 20% of mice found dead during toxicologic studies did not have a cause of death identifiable by necropsy, demonstrating the great difficulty in antemortem diagnosis of diseases in mice used in biomedical research.34 As the value of mice in biomedical research increases, these results demonstrate a need for improved diagnostics in mice.
Maternal reproductive disease, including both clinical disease, such as dystocia and vaginal prolapse, and subclinical disease, such as poor milk production, will result in compromised maternal care and an increased likelihood of illness or death of pups. Because we counted pups individually, the death of an entire litter due to maternal disease quickly inflated the number of deaths of neonatal mice. The identification of sick mouse pups was relatively rare compared with finding the mouse pups dead; as with adult mice, recognizing sick neonatal mouse pups is difficult. Early inspection and handling of mouse pups is very stressful for them and the dam, often leading to decreased reproductive performance, and perhaps cannibalism, and prompting recommendations discouraging close inspection of newborn mouse pups.24,28 In addition, as with adults, the window of time when pups can be identified as ill before they die may be very narrow, further minimizing our ability to aid these neonates. Another factor affecting the rate of neonatal deaths is the ‘expected’ mortality within a litter. In litter-bearing animals, it is accepted that a percentage of the litter will not survive to weaning. For example, preweaning mortality is reported to range between 10% and 30% in dogs and 7% and 20% in swine.9,35 In mice, this proportion varies by strain and genetic manipulation of the mice and usually is a factor in the fecundity data of mouse strains. Reasonable estimates of the rate of preweaning mortality in mice range between 5% and 20%.10 As with adults, the identification of sick neonatal animals to provide treatment or intervention by euthanasia is an important area for improvement in biomedical research.
Like that in other species,1 dermatitis was the clinical condition most often identified in the current investigation, with the main anatomic location being the dorsal neck and pinnae, consistent with C57Bl/6 ulcerative dermatitis.7,11,17,39 Interestingly, cases of ulcerative dermatitis accounted for only 53% of dermatitis cases in mice, indicating that there were many other cases of dermatitis that affected other body sites. The incidence of dermatitis within a cage was much higher when a first case was already present. The current investigation could not identify whether this correlation was due to genetic factors predisposing identical mice to dermatitis; environmental factors, which would be similar to all of the mice within a cage; opportunistic infectious agents not excluded from modern research facilities; or a combination of these factors. The high incidence and clinical significance of dermatitis continues to emphasize the important goal of identification of underlying pathology and efficacious treatments for laboratory mouse care.11,17,39
The presence of iatrogenic diseases in any facility can be particularly troublesome, because they potentially can be eliminated or greatly reduced through improved animal care procedures and training. The vast majority of watering failures occurred in facility A, which is the only facility using an automatic watering system. Although automatic watering has many long-term advantages to a facility in terms of husbandry costs and potentially diminished chance of ergonomic injuries to staff, there is also the risk of uncontrolled water flow into a cage, potentially completely flooding that cage and those below it. The use of bottled water sources greatly limits the potential injury to mice within a cage. Ultimately, a critical comparison between automatic watering and water bottles will reveal the optimal watering method for a facility.
Our current investigation found that neurologic disease and lameness in mice were rare. This finding contrasts with the results of a previous study,25 which reported that clinical evidence of osteoarthritis in elderly mice was common. This difference likely is due to the respective populations, with the disease being more prevalent in the aged population in the cited study.
Mice are predisposed to rectal prolapse due to the small amount of connective tissue providing support to the rectum.25 Diseases resulting in colitis and straining to defecate may lead to prolapse of the rectum. Infections with Citrobacter rodentium and Helicobacter spp. historically have been associated with rectal prolapse in mice. Although C. rodentium has essentially been eradicated from research facilities, Helicobacter spp. are still present in many facilities, including the institution in the current investigation, and may contribute to this condition.26 One interesting factor is that in the current investigation, diarrhea in mice was reported very rarely, leading to the finding that colitis and rectal prolapse may not be linked closely with diarrhea in this species.
Although none of the facilities were dedicated for a specific type of research, there are obvious differences between the disease incidence rates between the facilities. Facility D, the largest conventional facility in this study, had significantly more cases reported for several diseases, including dermatitis, ocular disease, tumors, and lethargy, than did the other 3 facilities. In comparison, facility A had the highest rate of neonatal mortality. We eliminated systematic differences in the environmental conditions between the facilities as possible causes of these differences, because all of the facilities were maintained according to the guidelines of the Guide for the Care and Use of Laboratory Animals14 and institutional policies. Other potential explanations for this increased reporting level include an aged population, phenotypic manifestations that were unexpected, immunosuppression inherent to the genetic background, and exposure to undesirable pathogenic agents due to differences in biosecurity between barrier and conventional facilities within each facility. Facility D was the largest conventional facility on campus, having fewer biosecurity practices than do the barrier facilities and allowing removal of mice from the vivarium followed by subsequent return. Barrier housing has been shown to be important in the maintenance of immunocompromised mice,5,6,32 but little work has examined its role in the prevention of spontaneous diseases in immunocompetent mice. Our data suggest this question warrants further investigation. The increased rate of neonatal death in facility A was due to the large population of breeding animals in the studies housed in this facility relative to the other facilities.
During the year, 7 outbreaks of viral or parasitic diseases were identified. Analysis of the reported diseases in these rooms did not reveal any trends in disease either before diagnosis of the outbreak or after the treatment or culling of affected animals. This result is not surprising, because many of the tested infectious agents only infrequently cause illness in immunocompetent mice.23 Although seasonal trends of disease are reported anecdotally by individual research groups, no significant seasonal trends were identified with any of the common diseases analyzed. Again, this outcome is not surprising, because laboratory animal professionals go to great lengths to maintain a stable environment with constant photoperiods that is optimal for the health of rodents in their vivaria.
Most sentinel monitoring programs are designed to detect only infectious diseases, intentionally exposing the animals to soiled bedding from colony cages and requiring that the sentinels are euthanized when younger than 1 y, while their immune systems are maximally active. The profound differences in infectious disease exposure and lifespan of sentinel animals (despite similar food, water, and caging) provide little information concerning the routine husbandry that the experimental animals receive. We have discussed the cost–benefit ratio of the possible use of ‘survival sentinels’ to look further into the incidence rate of spontaneous diseases in mice. If survival sentinels were to be used, we would house additional sentinel animals of a strain with extensive 24-mo survival and disease predilection data. Survival sentinels would be exposed to the same animal husbandry practices as those of the research mice. The disease incidence, survival rates, and causes of death among the sentinels could then be compared with published data for that particular mouse strain, thus providing information concerning the effects of husbandry and housing practices of the mice in the research facilities. Over time, the use of survival sentinels also could provide information regarding effects of barrier compared with conventional housing, ventilated racks compared with static filtered caging, water treatment systems, and food on mouse health. This option remains under discussion.
The disease rates from the current study can be compared with surveys of disease incidence at other similar institutions to determine husbandry and clinical treatment programs that optimize the care of mice in biomedical research. The data from this study suggest that the early recognition of mice with clinical disease is one of the most important challenges for our field. The early recognition of disease, both in adults and neonates, would provide increased opportunity for either early intervention and treatment or euthanasia of sick animals. It will be important in the future to periodically revisit this topic as the practices in the use, care, and husbandry of mice continues to evolve over time. The rates of common diseases can be affected by housing density, enrichment, and basic husbandry. As these factors change, along with the identification and eradication of as-yet unidentified viral and bacterial pathogens, it is reasonable to expect the prevalence of diseases in biomedical research to change as well.
Acknowledgments
We thank the leadership of the University of Pennsylvania Laboratory Animal Resources for their support throughout this project.
References
- 1.Bartlett PC, Van Buren JW, Neterer M, Zhou C. 2010. Disease surveillance and referral bias in the veterinary medical database. Prev Vet Med 94:264–271 [DOI] [PubMed] [Google Scholar]
- 2.Brayton C. 2006. Spontaneous diseases in commonly used mouse strains, p 623–719. In: Fox JG, Barthold SW, Davisson MT, Newcomer CE, Quimby FW, Smith AL. The mouse in biomedical research, 2nd ed. Amsterdam (the Netherlands): Academic Press. [Google Scholar]
- 3.Carty AJ. 2008. Opportunistic infections of mice and rats: Jacoby and Lindsey revisited. ILAR J 49:272–276 [DOI] [PubMed] [Google Scholar]
- 4.Clifford CB, Watson J. 2008. Old enemies, still with us after all these years. ILAR J 49:291–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Danneman P, Suckow MA, Brayton C, Suckow MA. 2013. The laboratory mouse. Boca Raton (FL): Taylor and Francis [Google Scholar]
- 6.Donovan J, Brown P. 2007. Managing immunocompromised animals. Curr Protoc Immunol Chapter 1:Unit 1.2. [Google Scholar]
- 7.Duarte-Vogel SM, Lawson GW. 2011. Association between hair-induced oronasal inflammation and ulcerative dermatitis in C57BL/6 mice. Comp Med 61:13–19 [PMC free article] [PubMed] [Google Scholar]
- 8.Dunn OJ. 1961. Multiple comparisons among means. J Am Stat Assoc 56:52–64 [Google Scholar]
- 9.Ettinger SA, Feldman EC. 2010. Textbook of veterinary internal medicine. Philadelphia (PA): Saunders [Google Scholar]
- 10.Fox RR, Witham BA. 1997. Handbook of genetically standardized JAX mice. Bar Harbor (ME): Jackson Laboratory [Google Scholar]
- 11.Hampton AL, Hish GA, Aslam MN, Rothman ED, Bergin IL, Patterson KA, Naik M, Paruchuri T, Varani J, Rush HG. 2012. Progression of ulcerative dermatitis lesions in C57BL/6Crl mice and the development of a scoring system for dermatitis lesions. J Am Assoc Lab Anim Sci 51:586–593 [PMC free article] [PubMed] [Google Scholar]
- 12.Hilbe JM. 2011. Negative binomial regression. Cambridge (UK): Cambridge University Press [Google Scholar]
- 13.Jacoby RO, Lindsey JR. 1997. Health care for research animals is essential and affordable. FASEB J 11: 609–614 [DOI] [PubMed] [Google Scholar]
- 14.Institute for Laboratory Animal Research 2011. Guide for the care and use of laboratory animals, 8th ed. Washington (DC): National Academies Press [Google Scholar]
- 15.Jacoby RO, Lindsey JR. 1998. Risks of infection among laboratory rats and mice at major biomedical research institutions. ILAR J 39:266–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kahn CM. 2005. Merck veterinary manual. Whitehouse Station (NJ): Merck.
- 17.Kastenmayer RJ, Fain MA, Perdue KA. 2006. A retrospective study of idiopathic ulcerative dermatitis in mice with a C57BL/6 background. J Am Assoc Lab Anim Sci 45:8–12 [PubMed] [Google Scholar]
- 18.Lane-Petter W, Barber AP, King HJ. 1955. Survey of laboratory animals in Great Britain. Brit Vet J 3:282–290 [Google Scholar]
- 19.Maita K, Hirano M, Harada T, Mitsumori K, Yoshida A, Takahashi K, Nakashima N, Kitazawa T, Enomoto A, Inui K, Shirasu Y. 1988. Mortality, major cause of moribundity, and spontaneous tumors in CD1 mice. Toxicol Pathol 16:340–349 [DOI] [PubMed] [Google Scholar]
- 20.Maronpot RR, Boorman GA, Gaul BW. 1999. Pathology of the mouse: reference and atlas. St Louis (MO): Cache River Press [Google Scholar]
- 21.McInnes EF, Rasmussen L, Fung P, Auld AM, Alvarez L, Lawrence DA, Quinn ME, del Fierro GM, Vassallo BA, Stevenson R. 2011. Prevalence of viral, bacterial, and parasitological diseases in rats and mice used in research environments in Australasia over a 5-y period. Lab Anim (NY) 40:341–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parker SE, Malone S, Bunte RM, Smith AL. 2009. Infectious diseases in wild mice (Mus musculus) collected on and around the University of Pennsylvania (Philadelphia) campus. Comp Med 59:424–430 [PMC free article] [PubMed] [Google Scholar]
- 23.Percy DH, Barthold SW. 2007. Pathology of laboratory rodents and rabbits. Ames (IA): Blackwell Publishing [Google Scholar]
- 24.Peters AG, Bywater PM, Festing MF. 2002. The effect of daily disturbance on the breeding performance of mice. Lab Anim 36:188–192 [DOI] [PubMed] [Google Scholar]
- 25. Pettan-Brewer C, Treuting PM. 2011. Practical pathology of aging mice. Pathobiol Aging Age Relat Dis 1. [DOI] [PMC free article] [PubMed]
- 26.Pritchett-Corning KR, Cosentino J, Clifford CB. 2009. Contemporary prevalence of infectious agents in laboratory mice and rats. Lab Anim 43:165–173 [DOI] [PubMed] [Google Scholar]
- 27.Rabe-Hesketh S, Everitt B. 2007. A handbook of statistical analyses using Stata. Boca Raton (FL): Chapman and Hall/CRC [Google Scholar]
- 28.Reeb-Whitaker CK, Paigen B, Beamer WG, Bronson RT, Churchill GA, Schweitzer IB, Myers DD. 2001. The impact of reduced frequency of cage changes on the health of mice housed in ventilated cages. Lab Anim 35:58–73 [DOI] [PubMed] [Google Scholar]
- 29.Roble GS, Gillespie V, Lipman NS. 2012. Infectious disease survey of Mus musculus from pet stores in New York City. J Am Assoc Lab Anim Sci 51:37–41 [PMC free article] [PubMed] [Google Scholar]
- 30.Savage VM, Gillooly JF, Woodruff WH, West GB, Allen AP, Enquist BJ, Brown JH. 2004. The predominance of quarter-power scaling in ecology. Funct Ecol 18:257–282 [Google Scholar]
- 31.Seamer J, Chesterman FC. 1967. A survey of disease in laboratory animals. Lab Anim 1:117–139 [Google Scholar]
- 32.Shek WR. 2008. Role of housing modalities on management and surveillance strategies for adventitious agents of rodents. ILAR J 49:316–325 [DOI] [PubMed] [Google Scholar]
- 33.Smith RJ. 1984. Allometric scaling in comparative biology: problems of concept and method. Am J Physiol 246:R152–R160 [DOI] [PubMed] [Google Scholar]
- 34.Son WC. 2003. Factors contributory to early death of young CD1 mice in carcinogenicity studies. Toxicol Lett 145:88–98 [DOI] [PubMed] [Google Scholar]
- 35. Straw BE, Zimmerman JJ, D'Allaire S, Taylor DJ. 2006. Diseases of swine. Ames (IA): Wiley-Blackwell.
- 36.Szklo M, Nieto F. 2014. Epidemiology: beyond the basics. Burlington (MA): Jones & Bartlett Learning [Google Scholar]
- 37.Treuting PM, Clifford CB, Sellers RS, Brayton CF. 2012. Of mice and microflora: considerations for genetically engineered mice. Vet Pathol 49:44–63 [DOI] [PubMed] [Google Scholar]
- 38.Weigler BJ. 2001. A primer in epidemiologic methodology. Comp Med 51:208–217 [PubMed] [Google Scholar]
- 39.Williams LK, Csaki LS, Cantor RM, Reue K, Lawson GW. 2012. Ulcerative dermatitis in C57BL/6 mice exhibits an oxidative stress response consistent with normal wound healing. Comp Med 62:166–171 [PMC free article] [PubMed] [Google Scholar]