Abstract
Objective
The purpose of this report is to describe a fifth metatarsal stress fracture that was not detectable using conventional radiographs and was identified with diagnostic ultrasonography (US), confirmed with computed tomography, and followed through symptom resolution with US.
Clinical features
A 68-year-old woman presented to a chiropractic teaching clinic for evaluation of right foot pain. Diagnostic US examination using an 8- to 15-MHz linear array transducer showed increased vascularity, periosteal elevation, and cortical disruption of the proximal diaphysis of the fifth metatarsal suggestive of a stress fracture. The patient was referred to an orthopedic specialist for comanagement.
Intervention and outcome
The patient was treated by an orthopedist who confirmed a stress fracture using computed tomography, and she was fit with a short-leg walking boot. Serial US images were obtained to document fracture healing and exclude complications. After 6 months, the patient was asymptomatic and had resumed all of her daily activities.
Conclusion
We report a case of a proximal fifth metatarsal stress fracture that was visualized with US and followed through symptom resolution by serial examinations.
Key indexing terms: Ultrasonography, Chiropractic, Fracture, Stress, Computed tomography
Introduction
Proximal fifth metatarsal fractures occur from a variety of mechanisms and are commonly classified into 3 types according to anatomical location1: tuberosity avulsion fractures (zone I), Jones fractures (zone II, located at the level of the fourth-fifth intermetatarsal articulation), and diaphyseal stress fractures (zone III, proximal diaphysis). The latter type is subclassified, using the Torg criteria, into acute (early), delayed, or nonunion.2 This classification helps to distinguish healing potential, with the acute form most likely to heal with immobilization therapy.2
Metatarsal fractures occur with an incidence of 67/100,000 per year, and up to 70% involve the fifth metatarsal.3 The entrance of the nutrient vessel at the junction of the proximal and middle one-third of the fifth metatarsal shaft corresponds to the area of diaphyseal stress fractures and may render the fracture site avascular.4 Fractures of the fifth metatarsal have been shown to be susceptible to the development of pseudoarthrosis during the healing phase.5 Furthermore, 56% of the reported 5521 fifth metatarsal osteoporotic fractures in an elderly white female population were of the proximal portion.6
Clinical findings of metatarsal stress fractures mimic osteoarthritis, tendonitis, or vascular disease; and as a result, imaging will be part of the diagnostic workup. Currently, because of its low cost and high specificity (94%), plain film radiography is initially used when there is clinical suspicion of a stress fracture.7 However, radiography lacks sufficient sensitivity in stress fracture detection (10%-20%). Magnetic resonance imaging (MRI) or skeletal scintigraphy, because of their high sensitivities (63%-100% for MRI and 74%-100% for skeletal scintigraphy), are therefore typically required for further diagnostic workup.7 More recently, ultrasonography (US) has been proposed as a reasonable follow-up to negative plain film radiographic results in the workup of a suspected stress fracture; and US criteria have been established that are consistent with and diagnostic of stress fractures.8
The purpose of this report is to present a case of a fifth metatarsal stress fracture that not only was visualized with US based on these criteria but also was periodically followed with US through symptom resolution.
Case report
A 68-year-old woman presented to a chiropractic teaching clinic with a chief concern of right foot pain of 10 days’ duration. The pain was described as generally dull with episodic sharp pain, localized to the lateral aspect of her right foot. She reported no specific mechanism of injury. Pain was reported to increase when the foot was inverted and plantar flexed. The initial onset of the pain was noted while she was bowling. Three days after the onset, the patient presented to urgent care and was examined; plain film radiography of the right ankle and foot was performed. Radiographic result was reported as negative for fracture, and the patient was informed that she had osteoarthritis. During her review of systems, she revealed a total of 4 previous surgical procedures involving her right foot. Two procedures were performed to repair the tibialis posterior tendon. The first surgery was performed with a flexor digitorum longus transfer; and the second, with a calcaneal osteotomy. Two other procedures, separate from and unrelated to the tibialis posterior tendon repair, were done for debridement of a large osteochondral defect in the medial talar dome. The first surgery on the defect consisted of arthroscopic debridement, whereas the second surgery consisted of both arthroscopic debridement and an osteoarticular transfer system procedure. The patient underwent the calcaneal osteotomy procedure approximately 12 years prior to presentation and underwent her last surgical procedure (osteoarticular transfer system procedure) approximately 10 years prior to her current presentation.
Ankle and foot examination revealed an abnormal gait due to reported right foot pain. Inspection revealed excessive pronation and calcaneal eversion of her right foot. Firm palpation around the fifth metatarsal base reproduced the patient’s symptoms. Soft tissue swelling was noted adjacent to the fifth metatarsal base. Active range of motion revealed a 30° decrease in plantar flexion relative to the contralateral side. Result of orthopedic and neurologic testing was unremarkable.
Because of the examination findings, a diagnostic US was performed of the right fifth metatarsal. The examination was performed by the radiology faculty at the chiropractic teaching clinic using a LOGIQ E9 ultrasonography system (GE Healthcare, Milwaukee, WI) operating with an 8- to 15-MHz linear array transducer. This frequency range is standard and provides high-resolution musculoskeletal US images.9 The US examination demonstrated cortical disruption, periosteal elevation with an adjacent hypoechoic region at the proximal diaphysis of the fifth metatarsal, and increased vascularity on color Doppler (Fig 1). Because the patient had minimal difficulty ambulating and reported no specific mechanism of injury, but did report engaging in repetitive bouts of bowling (in which the affected foot was subjected to routine supination forces), a stress fracture was suspected.
Fig 1.
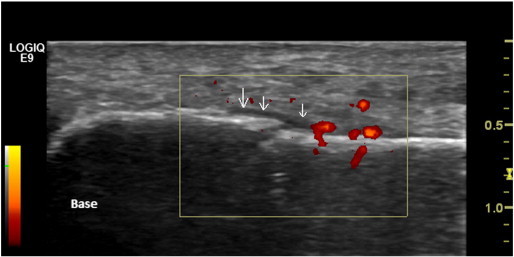
Initial ultrasound. Note the cortical break, periosteal elevation (arrows) with adjacent hypoechoic area, and hyperemia observed on color Doppler. There is an absence of callus formation and soft tissue swelling. Orientation with respect to the metatarsal base is also provided.
The patient was directed to an orthopedist for comanagement. A CT scan of the right foot was ordered by the orthopedist and confirmed the stress fracture of the proximal diaphysis of the fifth metatarsal. The patient was treated by the orthopedist with standard immobilization therapy consisting of a short leg walking boot. Four follow-up US scans were performed. On the first follow-up examination (11 days later and 21 days after symptom onset), the US was unchanged. A second follow-up examination was performed (day 27 in reference to the initial examination) revealing prominent callus formation and a hypoechoic area adjacent to the cortical break. Increased vascularity was persistent. The third follow-up examination (day 52) displayed only increased vascularity on color Doppler and callus formation, and the last examination (day 97) (Fig 2) displayed only callus formation. Soft tissue edema was not defined during any of the examinations likely because of the length of time between the actual injury and the US examinations. Approximately 6 months later, the patient was asymptomatic and had resumed all of her daily activities. The patient provided written consent to publish her deidentified health care information.
Fig 2.
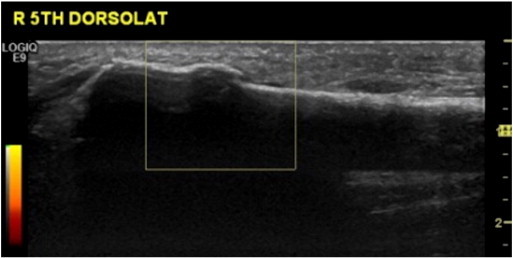
Final ultrasound. Observe the prominent callus that has formed and absence of hyperemia on color Doppler. There is persistence of the slight cortical break with no corresponding hypoechoic hematoma or periosteal elevation. Soft tissue swelling is still absent.
Discussion
The patient in this case was diagnosed and monitored with US through fracture healing and clinical resolution. Serial US observations were useful in monitoring interval changes and excluding complications in her metatarsal stress fracture.
Proximal fifth metatarsal stress fractures represent a clinical challenge, as they can be susceptible to delayed healing compared to other forms of metatarsal fractures.5 Most commonly, the mechanism of injury is a repetitive cyclical force applied to the foot.4 It is commonly seen in patients with cavus feet, genu varum, and chronic ankle instability.4 Gait alterations causing fatigue in the fifth metatarsal,10 total knee arthroplasty,11 Evans calcaneal osteotomy,12 and talipes equinovarus (club foot)13 have all been reported as rare causes of proximal fifth metatarsal stress fractures. Insufficiency fractures of the proximal fifth metatarsal in which there is underlying pathology can also occur.6
In this case, the patient had a history of acquired flat foot deformity that was treated with a calcaneal osteotomy procedure. It is unclear whether this was a specific Evans procedure. Regardless, a calcaneal osteotomy procedure designed to correct hindfoot valgus (done with this patient) will place the forefoot in relative supination and cause an overload of the lateral side of the foot and fifth metatarsal.12
With respect to early identification, it is important to note that physical examination of a metatarsal stress fracture may produce findings consistent with synovitis and neuritis.4 Combined with the inadequate sensitivity of plain film radiography in stress fracture identification, it is clear that multiple diagnostic tools will be required to adequately assess a suspected stress fracture. Ultrasonography may prove valuable in excluding a stress fracture in patients who initially present with symptoms consistent with synovitis or neuritis.
In this case, there was clear US evidence of stress fracture in the fifth metatarsal. Because of the etiology of stress injury in bone and the lack of knowledge with respect to staging stress fractures using US, it is unclear how long the evidence of fracture was present prior to visualization with US. However, this case is novel in that it not only provides a clear depiction of a fifth metatarsal stress fracture but also provides extensive follow-up imaging during the healing process. Larger clinical trials are warranted to better quantify and describe the US appearance of stress fracture development and healing, allowing for cost-effective clinical decisions. Given the superior sensitivity of US, earlier diagnosis could initiate conservative intervention before the evolution of unfortunate complications like nonunion and the development of pseudoarthrosis.
The first description of US in metatarsal stress fracture diagnosis was published in 1992.14 Since then, US has aided in diagnosing additional metatarsal stress fractures,8,15,16 detection of other occult fractures in the foot and ankle,17 stress fractures of the lower limb,18 and prediction of fracture callus formation with the use of color Doppler US.19 Furthermore, US has been recommended as a follow-up examination to negative radiography in the diagnostic workup of suspected stress fractures because it may circumvent the need for more costly tests such as MRI and skeletal scintigraphy.8,17
Currently, the following 5 US criteria are used to determine the presence of stress fractures: increased vascularity as demonstrated using color Doppler, periosteal elevation with a cortical break/loss of periosteal contiguity, periosteal reaction and early callus formation, hypoechoic area adjacent to the cortical break (corresponding to hematoma), and overlying soft tissue edema.8,16,18 In this case, the following US criteria were initially noted: increased vascularity demonstrated with color Doppler, periosteal elevation, and cortical disruption. During serial US scans, we observed resolution of the hematoma, a decrease in vascularity, and development of a bridging callus over the area of cortical break. Development of a bridging callus, hematoma resolution, and reduction of hypervascularity were all observed during serial US scans. No complications of the stress fracture were identified during follow-up examinations.
This case report enhances the breadth of clinical literature with respect to the utility of US for assessment of suspected metatarsal stress injury. The diagnosis of a proximal fifth metatarsal stress fracture using US may avoid the harms of ionizing radiation, and the use of time-consuming and more costly examinations. Ultrasonography is a cost-effective means to aid clinicians in early detection of metatarsal stress injury, essential to optimal nonsurgical outcomes and prognosis. Future research should evaluate the reliability of these US criteria in metatarsal stress fracture diagnosis.
Limitations
As with any case report, these findings cannot be applied to a larger set of patients, as more rigorous clinical trials need to be conducted to determine the efficacy of US in the workup of suspected metatarsal stress fracture. Furthermore, the temporal changes observed on US with respect to stress fracture healing cannot be extrapolated to other individuals. Future US work using sequential examinations on large patient populations will better characterize the US course and appearance of metatarsal stress fracture healing. Lastly, the patients’ complex history of foot and ankle injuries and surgical procedures must be considered when interpreting these findings.
Conclusion
Early detection of proximal fifth metatarsal diaphyseal stress fractures using diagnostic US may assist with optimal nonsurgical outcomes and prognosis. We have reported on the diagnosis and serial US changes in a case of a delayed proximal fifth metatarsal diaphyseal stress fracture.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Lawrence S.J., Botte M.J. Jones' fractures and related fractures of the proximal fifth metatarsal. Foot Ankle. 1993;14:358–365. doi: 10.1177/107110079301400610. [DOI] [PubMed] [Google Scholar]
- 2.Torg J.S. Fractures of the base of the fifth metatarsal distal to the tuberosity: a review. Orthopedics. 1990;13:731–737. doi: 10.3928/0147-7447-19900701-09. [DOI] [PubMed] [Google Scholar]
- 3.Petrisor B.A., Ekrol I., Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006;27:172–174. doi: 10.1177/107110070602700303. [DOI] [PubMed] [Google Scholar]
- 4.Weinfeld S.B., Haddad S.L., Myerson M.S. Metatarsal stress fractures. Clin Sports Med. 1997;16:319–338. doi: 10.1016/s0278-5919(05)70025-9. [DOI] [PubMed] [Google Scholar]
- 5.Peris P. Stress fractures. Best Pract Res Clin Rheumatol. 2003;17:1043–1061. doi: 10.1016/j.berh.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Hasselman C.T., Vogt M.T., Stone K.L., Cauley J.A., Conti S.F. Foot and ankle fractures in elderly white women. Incidence and risk factors. J Bone Joint Surg Am. 2003;85:820–824. doi: 10.2106/00004623-200305000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Dobrindt O., Hoffmeyer B., Ruf J. MRI versus bone scintigraphy. Evaluation for diagnosis and grading of stress injuries. Nuklearmedizin. 2012;51:88–94. doi: 10.3413/Nukmed-0448-11-12. [DOI] [PubMed] [Google Scholar]
- 8.Banal F., Gandjbakhch F., Foltz V. Sensitivity and specificity of ultrasonography in early diagnosis of metatarsal bone stress fractures: a pilot study of 37 patients. J Rheumatol. 2009;36:1715–1719. doi: 10.3899/jrheum.080657. [DOI] [PubMed] [Google Scholar]
- 9.Smith J., Finnoff J.T. Diagnostic and interventional muscuoloskeletal ultrasound: part 1. Fundamentals. PM R. 2009;1:64–75. doi: 10.1016/j.pmrj.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Roehrig G.J., McFarland E.G., Cosgarea A.J., Martire J.R., Farmer K.W. Unusual stress fracture of the fifth metatarsal in a basketball player. Clin J Sport Med. 2001;11:271–273. doi: 10.1097/00042752-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Fujioka H., Kokubu T., Makino T. Stress fracture of the fifth metatarsal bone as a late complication of total knee arthroplasty. Kobe J Med Sci. 2010;55:93–97. [PubMed] [Google Scholar]
- 12.Davitt J.S., Morgan J.M. Stress fracture of the fifth metatarsal after Evans' calcaneal osteotomy: a report of two cases. Foot Ankle Int. 1998;19:710–712. doi: 10.1177/107110079801901011. [DOI] [PubMed] [Google Scholar]
- 13.Craigen M.A., Clarke N.M. Bilateral Jones fractures of the fifth metatarsal following relapse of talipes equinovarus. Injury. 1996;27:599–601. doi: 10.1016/0020-1383(96)89023-1. [DOI] [PubMed] [Google Scholar]
- 14.Howard C.B., Lieberman N., Mozes G., Nyska M. Stress fracture detected sonographically. AJR Am J Roentgenol. 1992;159:1350–1351. doi: 10.2214/ajr.159.6.1442422. [DOI] [PubMed] [Google Scholar]
- 15.Banal F., Etchepare F., Rouhier B. Ultrasound ability in early diagnosis of stress fracture of metatarsal bone. Ann Rheum Dis. 2006;65:977–978. doi: 10.1136/ard.2005.046979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drakonaki E.E., Garbi A. Metatarsal stress fracture diagnosed with high-resolution sonography. J Ultrasound Med. 2010;29:473–476. doi: 10.7863/jum.2010.29.3.473. [DOI] [PubMed] [Google Scholar]
- 17.Wang C.L., Shieh J.Y., Wang T.G., Hsieh F.J. Sonographic detection of occult fractures in the foot and ankle. J Clin Ultrasound. 1999;27:421–425. doi: 10.1002/(sici)1097-0096(199910)27:8<421::aid-jcu2>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 18.Bodner G., Stockl B., Fierlinger A., Schocke M., Bernathova M. Sonographic findings in stress fractures of the lower limb: preliminary findings. Eur Radiol. 2005;15:356–359. doi: 10.1007/s00330-004-2525-8. [DOI] [PubMed] [Google Scholar]
- 19.Caruso G., Lagalla R., Derchi L., Iovane A., Sanfilippo A. Monitoring of fracture calluses with color Doppler sonography. J Clin Ultrasound. 2000;28:20–27. doi: 10.1002/(sici)1097-0096(200001)28:1<20::aid-jcu3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]


