Abstract
Objective
The purpose of this preliminary study was to investigate the effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in women with menstrual low back pain (LBP).
Methods
Thirty women with menstrual LBP participated in the study. Subjects were assigned to a control group (n = 10, mean age = 25.1 ± 4.7 years) and an intervention group (n = 20, mean age = 21.7±2.4 years). Treatment for the intervention group consisted of functional lumbar stabilization exercises, 10 repetitions each, 3 times a day, for 3 consecutive months. The women in the control group received no exercise and performed their regular activity daily living. Pain intensity using a Numeric Pain Scale (NPS), Oswestry Disability Index (ODI), Roland-Morris Questionnaire (RMQ), and Tampa Scale of Kinesiophobia (TSK) was collected at baseline and at the end of 3 months in both groups.
Results
Statistical analysis (paired t test) revealed a significant decrease in NPS, ODI, RMQ, and TSK after treatment in the intervention group. No significant difference in NPS, ODI, RMQ, or TSK was found between pre- and postmeasurement scores in the control group. In the analysis of covariance, controlling for pretest scores, a significant difference was found between the 2 groups in the postmeasurement score of NPS (P = .01), ODI (P < .001), RMQ (P = .002), and TSK (P = .04).
Conclusion
Lumbar stabilization exercises were shown to improve pain, disability, and kinesiophobia during menstrual LBP for subjects who participated in this preliminary study compared to those who did not receive the intervention.
Key indexing terms: Low back pain, Menstruation, Exercise, Pain, Disability
Introduction
Menstrual low back pain (LBP) is one of the common complaints among women. Previous studies have indicated that more than 40% to 50% of the population experience LBP during the menstrual phase (days 1-6) of the menstrual cycle.1-3 Menstrual back pain can be a monthly occurrence for many women.1 For some women, this discomfort makes it difficult to perform normal household-, job-, or school-related activities for a few days during the menstrual cycle. Menstrual LBP may even be the leading cause of lost time from school and work among young women.1 Pain in the lower back has been also positively associated with menstruation and pregnancy in women.2-9 Despite its detrimental effects on individuals’ activities, the exact causes of menstrual LBP have not yet been fully understood. However, hormonal factors have been attributed as the cause of menstrual LBP in the literature.4
Investigators have long speculated that hormonal change in women is related to ligament laxity. They found that hormonal change may affect collagen synthesis, which, in turn, affects ligament laxity.10-12 Some studies showed that the chance of incidence of ligament injury in women and girls is different during different phases of the menstrual cycle because of hormonal changes during the menstrual cycle.13-15
Spinal instability is an important cause of LBP. There is substantial evidence indicating that LBP is related to insufficient spinal stability (instability) and dysfunction and loss of motor control characteristics of deep stabilizing muscles.13,14
The stabilizing system of the spine is divided into 3 subsystems: (1) passive, (2) active, and (3) the neural control unit. Considering the role of 3 subsystems (passive, active, and neural control system) for providing spinal stability according to the Panjabi model15-17 and with regard to the evidences indicating change in ligament tension following hormonal change, it is thought that ligament laxity due to hormonal changes in women can diminish the role of passive subsystems for providing sufficient spinal stability. Investigators attributed menstrual symptoms to hormonal change and stated that estrogen activity can affect menstrual symptoms.18 Menstrual LBP can be also attributed to the spinal instability resulting from ligament laxity (passive system impairment) due to hormonal change.
Exercise training protocols using active and neural system (functional lumbar stabilization exercise) can compensate the insufficient function of passive subsystem for providing trunk stability. Based on these findings, lumbar stabilization exercises have widely been used by physical therapists for subjects with LBP attending physical therapy.19,20 According to the existent evidence, functional lumbar stabilizing exercises (with emphasis on contraction of deep local stabilizing muscles) improve the pain and functional disability in subjects with LBP.19,20
It has been shown that deep abdominal muscles contraction considerably decreases the neutral zone or laxity of the sacroiliac joint.21 This decrease in laxity is larger than that caused by a bracing action using all the lateral abdominal muscles.
The evidence for the effectiveness of physical exercise in the management of menstrual symptoms revealed a sustained decrease in symptoms over the 3 menstrual cycles.22 However, to our knowledge, no study has directly investigated the effect of functional lumbar stabilization exercise (with emphasis on deep stability muscles) on menstrual LBP in women. Therefore, the purpose of this study was to investigate the effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in women with menstrual LBP.
Methods
Subjects
Thirty females from the Tehran region with menstrual LBP participated in this study. The subject population was a sample of convenience made up of subjects who were between the ages of 19 and 39 years. They were consecutive subjects who agreed to participate and fulfilled the inclusion criteria. Subjects were included if they had LBP during the menstrual phase (days 1-6) of the menstrual cycle. All subjects suffered from LBP during all menstrual cycles in the year before the study. The subjects experienced no back pain or LBP at times other than the menstrual phase. Pain intensity during menstrual LBP was greater than 5 in the Numeric Pain Scale (NPS). Subjects were excluded if they had history of spinal surgery, spinal or pelvic fracture and hospitalization for severe trauma or car accident, urinary tract infection, vaginal infection, and known neurological disorders. The subjects with pain intensity less than 5 in the NPS were excluded from the study. All the subjects signed an informed consent form approved by the human subjects ethics committee at the University of Social Welfare and Rehabilitation Sciences before participating in the study (reference no. 891025). This clinical trial has been reviewed and registered on the ClinicalTrials.gov registry (registration no. NCT01932723).
Physical characteristics of the subjects are shown in Table 1.
Table 1.
Demographic data of the subjects
| Variables | Control group (n = 10) |
Intervention group (n = 20) |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Age (y) | 25.1 ± 4.8 | 21.7 ± 2.5 |
| Weight (kg) | 60.7 ± 11.3 | 58.7 ± 7.7 |
| Height (cm) | 164.5 ± 7.9 | 163.0 ± 5.7 |
| BMI (kg/m2) | 22.4 ± 3.4 | 22.0 ± 2.7 |
BMI, body mass index.
Assignment
Subjects were assigned to a control group (n = 10, mean age = 26.1 ± 4.8 years) and an intervention group (n = 20, mean age = 21.7 ± 2.5 years). Physical characteristics of the subjects in each group are shown in Table 1.
Twenty women with menstrual LBP were selected based on the selection criteria, and they were instructed to perform the lumbar stabilization exercises for 3 months. Following the initial 20 subjects’ inclusion in the study, 10 subjects with menstrual LBP were selected and received no exercise and performed their activity daily living as before. Although the subjects were not randomly assigned to the groups, the subjects did not choose the group.
Procedure
The treatment regimen for intervention group consisted of the functional lumbar stabilization exercises for 3 months consecutively. The women in the control group received no exercise and performed their activity daily living as before.
The procedure for exercise program was as follows:
Subjects were instructed to perform abdominal hollowing (drawing-in) exercises in supine positions, progressing to more functional positions and activities as described by others.13,14 The first stage was the cognitive stage, where, in the early training period of stabilizing exercises, a high level of awareness was needed in order to isolate the contraction of the local muscle system without global muscle substitution. The aim of the first stage is to train the specific isometric co-contraction of deep abdominals with lumbar multifidus at low levels of maximal voluntary contraction and with controlled respiration. They were then instructed to perform transversus abdominis and multifidus contraction during single limb and alternating opposite arm and leg movements followed by cross limb movements. Finally, the subjects were trained to contract the muscles during walking and functional activities.
All subjects in intervention group were instructed to perform the lumbar stabilization exercises daily, 10 repetitions each (3 times a day), for 3 months consecutively. All exercises were performed to a count of 7 seconds.
Main outcome measures
Pain intensity using NPS, Oswestry Disability Index (ODI), Roland-Morris Questionnaire (RMQ), and Tampa Scale of Kinesiophobia (TSK) was collected at baseline and at the end of treatment (after 3 months) in both groups to investigate the efficacy of stabilization exercise on pain and disability of the women with LBP during menstruation.
The Persian versions of the ODI, RMQ, and TSK are reliable and valid questionnaires to measure functional status in Persian-speaking patients with LBP.23,24 They are simple and fast scales, and the use of them has been recommended in a clinical setting and outcome studies in Iran.
The NPS is a simple, sensitive, and reproducible instrument frequently used for the assessment of variations in intensity of pain during the menstrual phase. In clinical practice, the amount of pain relief, assessed by NPS, is often considered as a measure of the efficacy of treatment. In this study, the level of pain was recorded on a 10-cm line with “no pain” at one end and marked at the other end with “the worst pain that you can imagine,” with numbers along the line. Subjects were asked to state their pain level by placing a mark along this horizontal line intersecting a number.25,26
The revised ODI, commonly used to assess pain-related disability in persons with LBP, consists of 10 sections related to the effect of pain on usual daily activities including pain intensity, personal care (washing, dressing, etc), lifting, walking, sitting, standing, sleeping, social life, traveling, and homemaking/employment. Each section contains 6 items relating to different levels of limitation in the same activity (0 = no limitation, 5 = maximal limitation). The answers to each of the combined section add up a maximum score of 50.26-28
The RMQ is a validated self-administered scale for measuring disability related to LBP.21 It is a 24-point scale that reflects limitation in different functional activities of daily living. The questionnaire is filled out by the subjects who have to indicate which items reflect their current status. Thus, results range from 0 (no disability) to 24 (maximum disability). The RMQ has been shown to be reliable and to be sensitive to change over time for patients with LBP.
The TSK is a 17-item questionnaire designed to assess kinesiophobia. Subjects were asked to indicate their level of agreement to each of the 17 statements on a 4-point response scale, with scoring alternatives from “strongly disagree” to “strongly agree.” Results range from 17 to 68, with scores greater than 37 indicating a high degree of kinesiophobia. The TSK has been has been considered to have face and content validity as well as stability over time and internal consistency.29,30
The main outcome measures (NPS, ODI, RMQ, and TSK) were taken as pre-post testing for all subjects at the same time (day 4) during their cycle.
Statistical analysis
Statistical analysis was performed using SPSS version 17.0. Kolmogorov-Smirnov test was utilized to assess the normality of distribution for tested variables before and after treatment. Normal distribution was observed for variables in both groups.
Paired t test was used to determine any significant change in tested variables (NPS, ODI, RMQ, and TSK) at the end of treatment compared with pretreatment scores in the control and intervention groups. Analysis of covariance (ANCOVA) was calculated to determine the significance of differences between the control and intervention groups in posttest measurements, with pretreatment scores used as covariates in the analysis. The test for homogeneity of regression coefficient was conducted because it is a necessary condition for valid application of the ANCOVA. Statistical significant was attributed to P value less than .05.
Results
The subject flow diagram provided in Fig 1 reports the number of subjects who were registered and those who received allocated intervention, assignment, and measurements for each group.
Fig 1.
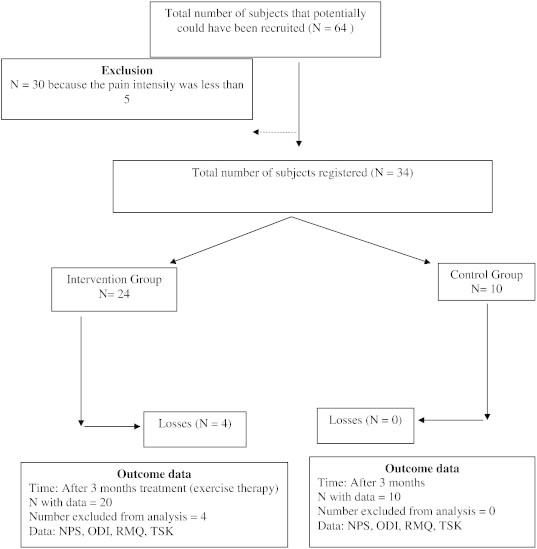
Flow diagram for study. NPS, numeric pain scale; ODI, Oswestry Disability Index; RMQ, Roland-Morris Questionnaire; TSK, Tampa Scale of Kinesiophobia.
Demographic data (mean ± SD) for the subjects in both groups are presented in Table 1.
Pre- and postmeasurement scores for NPS, ODI, RMQ, and TSK in the control and intervention groups and the results of paired t test are provided in Table 2. The result of paired t test showed a significant decrease in NPS, ODI, RMQ, and TSK after treatment in intervention group compared with before treatment. No significant difference in NPS, ODI, RMQ, and TSK was found between pre- and postmeasurement scores in the control group (Table 2, Fig 2). The findings of ANCOVA revealed significant difference between the control and intervention groups on the postmeasurement score of NPS (P = .01), ODI (P < .001), RMQ (P = .002), and TSK (P = .04), with pretreatment scores as the covariate.
Table 2.
Pre- and postmeasurement scores for NPS, ODI, RMQ, and TSK in the subjects
| Variables | Group | Before treatment |
After treatment |
P value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| NPS | Intervention | 7.1 ± 1.4 | 4.1 ± 1.8 | < .001 |
| Control | 6.5 ± 0.5 | 5.6 ± 1. 2 | .19 | |
| ODI | Intervention | 17.6 ± 7.5 | 7.65 ± 3.5 | < .001 |
| Control | 15.9 ± 7.5 | 14.3 ± 3.6 | .33 | |
| RMQ | Intervention | 10.0 ± 5.7 | 3.9 ± 3.0 | < .001 |
| Control | 9.1 ± 4.4 | 8.2 ± 3.9 | .18 | |
| TSK | Intervention | 36.7 ± 7.1 | 33.4 ± 5.4 | .01 |
| Control | 35.5 ± 4.6 | 36.2 ± 3.8 | .56 |
NPS, numeric pain scale; ODI, Oswestry Disability Index; RMQ, Roland-Morris Questionnaire; TSK, Tampa Scale of Kinesiophobia.
Fig 2.
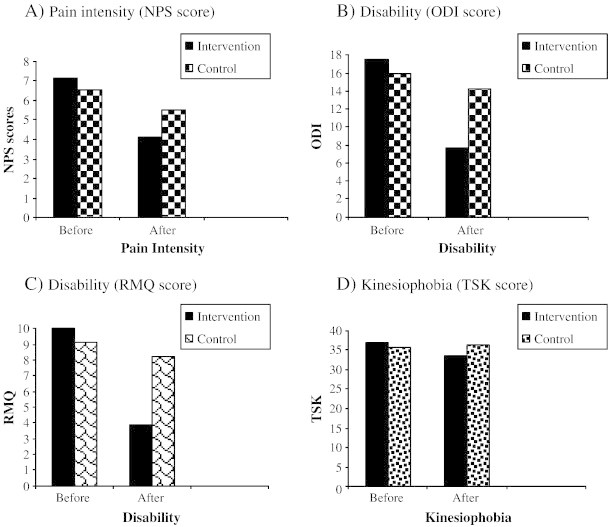
NPS, ODI, RMQ, and TSK after treatment compared with before treatment. A, Pain intensity (NPS score). B, Disability (ODI score). C, Disability (RMQ score). D, Kinesiophobia (TSK score). NPS, numeric pain scale; ODI, Oswestry Disability Index; RMQ, Roland-Morris Questionnaire; TSK, Tampa Scale of Kinesiophobia.
Discussion
The result of this study showed a significant decrease in NPS, ODI, RMQ, and TSK scores after functional lumbar stabilization exercises for 3 months compared with before treatment. These findings revealed a significant improvement in pain intensity, disability, and kinesiophobia during menstrual LBP after 3 months of functional lumbar stabilization exercises.
The change in pain intensity and disability after trunk stability exercise found in our study complements the results of previous studies that indicated improvement of pain and disability following exercise in subjects LBP.19,20 However, the subjects in previous studies were mainly subjects with chronic nonspecific LBP. To our knowledge, this is the first study to directly investigate the effect of stabilization exercise on LBP during the menstrual phase (days 1-6) of the menstrual cycle.
Investigators hypothesize that menstrual LBP may be due to a decrease in spinal stability resulting from ligament laxity (passive system impairment) due to hormonal changes.10-12 Hormonal change may affect collagen synthesis, which, in turn, affects ligament laxity. Previous studies showed that change in laxity of the knee joint ligaments (eg, anterior circulate ligament) is strongly related to the hormonal changes and hormone surge during the cycle.10-12 Some others showed that the chance of incidence of ligament injury in women and girls is different during different phases of the menstrual cycle because of hormonal changes during the menstrual cycle.31-33
According to the Panjabi model, the spinal stabilizing system consists of 3 interrelated subsystems including passive, active, and neural control system.15-17 It is thought that reduced function of one subsystem may place increased demands on the other subsystems to maintain stability.
Spinal ligaments along with joint capsules are important passive structures to provide segmental spinal stability. The ligaments may play an important role in controlling the movement occurring in different frontal planes.34 Evidence for the role of ligaments in trunk stability has been shown by anatomical observations.35-37 Injury to the passive subsystem (ligaments) may have important implications for spinal stability. It may increase the size of the neutral zone and enhance the demands on the active and neural control subsystems to avoid the development of segmental instability.15,16 The active subsystem of the spinal stabilizing system consists of the spinal muscles and tendons. The relative importance of different muscle groups in providing lumbar stability is a topic of much research and study.38-41 Deep abdominal muscles including transversus abdominis and oblique abdominal muscles are reported to be a part of a deep muscle cylinder that contributes to the stability of the lumbar spine during functions.13,42 Automatic activation of these muscles is considered as a protective mechanism for the lumbar spine.43 This theory is supported by studies demonstrating continuous and feed-forward activity of these muscles throughout movements of the lumbar spine. The neural control system may play an important role in stabilizing the spine in anticipation of an applied load41,44 found that the transversus abdominis and multifidus muscle activity consistently precedes lower or upper extremity movement in healthy subjects without LBP. Previous studies have shown delayed activity of the deep abdominal muscles in subjects with LBP, indicating deficient neural control.
Although ligament laxity may increase the size of the neutral zone, contraction of deep stabilizing muscles is thought to decrease the neutral zone in the spine.15,16 We think that exercise training protocols using active and neural system (functional lumbar stabilization exercise with emphasis on contraction of deep local stabilizing muscles) can compensate the diminished function of passive subsystem for providing trunk stability as a result of ligament laxity due to hormonal change. Thus, improvement in pain, functional disability, and kinesiophobia after 3 months of treatment may be due to increase in the spinal stability following stabilizing exercise. These findings are in accordance with other studies showing a decrease in menstrual symptoms in women following general exercise therapy.22
Limitations
One of the limitations of this study was that we did not measure for ligament laxity. Thus, the women were not assessed and categorized as being with or without sacroiliac joint laxity. It is suggested that future investigations include the effect of exercise in patients with and without laxity of sacroiliac joint.
Limitations of this study also included the small number of subjects, and there was lack of randomization for the allocation of the subjects into the control and intervention groups.
Conclusion
This preliminary study assessed the effect of functional lumbar stabilization exercise (with emphasis on deep stability muscles) on pain, disability, and kinesiophobia in women with menstrual LBP. It seems that lumbar stabilization exercise has potential to decrease LBP and disability for women who have LBP during their menses.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgment
The authors thank the Iran National Science Foundation.
References
- 1.Lentz G.M. Primary and secondary dysmenorrhea, premenstrual syndrome, and premenstrual dysphoric disorder: etiology, diagnosis, management. In: Katz V.L., Lentz G.M., Lobo R.A., Gershenson D.M., editors. Comprehensive gynecology. 5th ed. Mosby Elsevier; Philadelphia, Pa: 2007. chap 36. [Google Scholar]
- 2.Svensson H.O., Andersson G.B., Hagstad A., Jansson P.O. The relationship of low-back pain to pregnancy and gynecologic factors. Spine. 1990;15:371–375. doi: 10.1097/00007632-199005000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Smith D.R., Mihashi M., Adachi Y. Menstrual disorders and their influence on low back pain among Japanese nurses. Ind Health. 2009;47:301–312. doi: 10.2486/indhealth.47.301. [DOI] [PubMed] [Google Scholar]
- 4.Wijnhoven H.A., de Vet H.C., Smit H.A., Picavet H.S. Hormonal and reproductive factors are associated with chronic low back pain and chronic upper extremity pain in women—the MORGEN study. Spine. 2006;31:1496–1502. doi: 10.1097/01.brs.0000220706.96724.76. [DOI] [PubMed] [Google Scholar]
- 5.Malmqvist S., Kjaermann I., Andersen K., Økland I., Brønnick K., Larsen J.P. Prevalence of low back and pelvic pain during pregnancy in a Norwegian population. J Manipulative Physiol Ther. 2012;35(4):272–278. doi: 10.1016/j.jmpt.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Sipko T., Grygier D., Barczyk K., Eliasz G. The occurrence of strain symptoms in the lumbosacral region and pelvis during pregnancy and after childbirth. J Manipulative Physiol Ther. 2010;33(5):370–377. doi: 10.1016/j.jmpt.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Skaggs C.D., Prather H., Gross G., George J.W., Thompson P.A., Nelson D.M. Back and pelvic pain in an underserved United States pregnant population: a preliminary descriptive survey. J Manipulative Physiol Ther. 2007;30(2):130–134. doi: 10.1016/j.jmpt.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Murphy D.R., Hurwitz E.L., McGovern E.E. Outcome of pregnancy-related lumbopelvic pain treated according to a diagnosis-based decision rule: a prospective observational cohort study. J Manipulative Physiol Ther. 2009;32(8):616–624. doi: 10.1016/j.jmpt.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 9.Stuber K.J., Smith D.L. Chiropractic treatment of pregnancy-related low back pain: a systematic review of the evidence. J Manipulative Physiol Ther. 2008;31(6):447–454. doi: 10.1016/j.jmpt.2008.06.009. [Review] [DOI] [PubMed] [Google Scholar]
- 10.Heitz N.A., Eisenman P.A., Beck C.L., Walker J.A. Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athletic Train. 1999;34:144–149. [PMC free article] [PubMed] [Google Scholar]
- 11.Park S.K., Stefanyshyn D.J., Ramage B., Hart D.A., Ronsky J.L. Alterations in knee joint laxity during the menstrual cycle in healthy women leads to increases in joint loads during selected athletic movements. Am J Sports Med. 2009;37:1169–1177. doi: 10.1177/0363546508330146. [DOI] [PubMed] [Google Scholar]
- 12.Karageanes S.J., Blackburn K., Vangelos Z.A. The association of the menstrual cycle with the laxity of the anterior cruciate ligament in adolescent female athletes. Clin J Sport Med. 2000;10:162–168. doi: 10.1097/00042752-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Richardson C.A., Jull G.A., Hodges P.W., Hides J.A. Therapeutic exercise for spinal segmental stabilization in low back pain. Scientific basis and clinical approach. 1999. Churchill Livingstone, Edinburgh. [Google Scholar]
- 14.Jull G.A., Richardson C.A. Motor control problems in patients with spinal pain: a new direction for therapeutic exercises. J Manipulative Physiol Ther. 2000;23:115–117. [PubMed] [Google Scholar]
- 15.Panjabi M.M. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5:383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Panjabi M.M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5:390–396. doi: 10.1097/00002517-199212000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Panjabi M.M. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003;13:371–379. doi: 10.1016/s1050-6411(03)00044-0. [DOI] [PubMed] [Google Scholar]
- 18.Barnard N.D., Scialli A.R., Hurlock D., Bertron P. Diet and sex-hormone binding globulin, dysmenorrhea, and premenstrual symptoms. Obstet Gynecol. 2000;95:245–250. doi: 10.1016/s0029-7844(99)00525-6. [DOI] [PubMed] [Google Scholar]
- 19.O’Sullivan P.B., Twomey L.T., Allison G.T. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22:2959–2967. doi: 10.1097/00007632-199712150-00020. [DOI] [PubMed] [Google Scholar]
- 20.Standaert C.J., Weinstein S.M., Rumpeltes J. Evidence-informed management of chronic low back pain with lumbar stabilization exercises. Spine J. 2008;8:114–120. doi: 10.1016/j.spinee.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 21.Richardson C.A., Snijders C.J., Hides J.A., Damen L., Pas M.S., Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine. 2002;15(27):399–405. doi: 10.1097/00007632-200202150-00015. [DOI] [PubMed] [Google Scholar]
- 22.Brown J., Brown S. Exercise for dysmenorrhoea. Cochrane Database Syst Rev. 2010;2 doi: 10.1002/14651858.CD004142.pub2. CD004142. [DOI] [PubMed] [Google Scholar]
- 23.Mousavi S.J., Parnianpour M., Mehdian H., Montazeri A., Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine. 2006;31:E454–E459. doi: 10.1097/01.brs.0000222141.61424.f7. [DOI] [PubMed] [Google Scholar]
- 24.Jafari H., Ebrahimi E., Salavati M., Kamali M., Fata L. Psychometric properties of Iranian version of tampa scale for kinesiophobia in low back pain patients (press in farsi) J Rehabil. 2010;11:15–22. [Google Scholar]
- 25.Huskisson E.C., Jones J., Scott P.J. Application of visual analogue scales to the measurement of functional capacity. Rheumatology. 1976;15:185–187. doi: 10.1093/rheumatology/15.3.185. [DOI] [PubMed] [Google Scholar]
- 26.Murtezani A., Hundozi H., Orovcanec N., Sllamniku S., Osmani T. A comparison of high intensity aerobic exercise and passive modalities for the treatment of workers with chronic low back pain: a randomized, controlled trial. Eur J Phys Rehabil Med. 2011;47:1–8. [PubMed] [Google Scholar]
- 27.Fairbank J.C., Couper J., Davies J.B., O’Brien J.P. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 28.Roland M., Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 29.Lundberg M.K.E., Styf J., Carlsson S.G. A psychometric evaluation of the Tampa Scale for Kinesiophobia—from a physiotherapeutic perspective. Physiother Theory Pract. 2004;20:121–130. [Google Scholar]
- 30.Bränström H., Fahlström M. Kinesiophobia in patients with chronic musculoskeletal pain: differences between men and women. J Rehabil Med. 2008;40:375–380. doi: 10.2340/16501977-0186. [DOI] [PubMed] [Google Scholar]
- 31.Wojtys E.M., Huston L.J., Lindenfeld T.N., Hewett T.E., Greenfield M.L. Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. Am J Sports Med. 1998;26:614–619. doi: 10.1177/03635465980260050301. [DOI] [PubMed] [Google Scholar]
- 32.Hewett T.E., Zazulak B.T., Myer G.D. Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. Am J Sports Med. 2007;35:659–668. doi: 10.1177/0363546506295699. [DOI] [PubMed] [Google Scholar]
- 33.Shultz S.J., Kirk S.E., Johnson M.L., Sander T.C., Perrin D.H. Relationship between sex hormones and anterior knee laxity across the menstrual cycle. Med Sci Sports Exerc. 2004;36:1165–1174. doi: 10.1249/01.MSS.0000132270.43579.1A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Panjabi M.M., Goel V.K., Takata K. Physiologic strains in the lumbar spinal ligaments: an in vitro biomechanical study. Spine. 1982;7:192–203. doi: 10.1097/00007632-198205000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Jiang H., Russell G., Raso J. The nature and distribution of human supraspinal and interspinal ligaments. Spine. 1995;20:869–876. doi: 10.1097/00007632-199504150-00001. [DOI] [PubMed] [Google Scholar]
- 36.Indahl A., Kaigle A.M., Reikeras O., Holm S.H. Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine. 1997;22:2834–2840. doi: 10.1097/00007632-199712150-00006. [DOI] [PubMed] [Google Scholar]
- 37.Sharma M., Langrana N.A., Rodriguez J. Role of ligaments and facets in lumbar spinal stability. Spine. 1995;20:887–900. doi: 10.1097/00007632-199504150-00003. [DOI] [PubMed] [Google Scholar]
- 38.Crisco J.J., III, Panjabi M.M. The intersegmental and multisegmental muscles of the lumbar spine: a biomechanical model comparing lateral stabilizing potential. Spine. 1991;16:793–799. doi: 10.1097/00007632-199107000-00018. [DOI] [PubMed] [Google Scholar]
- 39.Gracovetsky S., Farfan H.F., Helleur C. The abdominal mechanism. Spine. 1985;10:317–324. doi: 10.1097/00007632-198505000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Tesh K.M., Dunn J.S., Evans J.H. The abdominal muscles and vertebral stability. Spine. 1987;12:501–508. doi: 10.1097/00007632-198706000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Hodges P.W., Richardson A. Inefficient muscular stabilization of the lumbar spine associated with low back pain. Spine. 1996;21:2640–2650. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- 42.Bergmark A. Stability of the lumbar spine: a study in mechanical engineering. Acta Orthop Scand Suppl. 1989;230:1–54. doi: 10.3109/17453678909154177. [DOI] [PubMed] [Google Scholar]
- 43.Hodges P.W., Moseley G.L. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13:361–370. doi: 10.1016/s1050-6411(03)00042-7. [DOI] [PubMed] [Google Scholar]
- 44.Hodges P.W., Richardson C.A. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77:132–142. doi: 10.1093/ptj/77.2.132. [DOI] [PubMed] [Google Scholar]


