Abstract
Approximately 3.0% of young Americans have used anabolic-androgenic steroids (AAS). A traditional model of adolescent substance use, the gateway hypothesis, suggests that drug use follows a chronological, causal sequence, whereby initial use of a specific drug leads to an increased likelihood of future drug use. Therefore, the use of illicit appearance and performance enhancing drugs (APED), such as AASs, also follows an analogous progression, whereby legal APEDs, (e.g., nutritional supplements) precedes illicit APED use. We examined the relationship between nutritional supplement use, beliefs about APEDs, and APED use in 201 male (n = 100) and female (n = 101) undergraduates. Participants completed measures of muscle dysmorphia (MDDI), body checking (BCQ, MBCQ), eating disorder symptoms (EDE–Q), perfectionism (FMPS), positive beliefs about the efficacy–safety of AAS use and APED use patterns. A series of covariance structure models (CSM) showed body image disturbance, compulsive exercise, illicit drug use, and perfectionism, independent of gender, were significant predictors of positive beliefs about AAS. Those who used both fat burning and muscle building supplements reported the strongest beliefs in AAS efficacy–safety, which was associated with higher likelihood of current illicit APED use. There was evidence of significant indirect relationships between supplement use and illicit APED use through contact with other AAS users and beliefs about AAS. The potential role for nutritional supplement use in the initiation of illegal APED use is discussed. Future prevention efforts may benefit from targeting legal APED users in youth.
Keywords: anabolic-androgenic steroids, gateway hypothesis, nutritional supplements, body image disturbance, risk factor
Appearance and performance enhancing drugs (APEDs) include a range of substances used to promote physical changes to muscle or body fat to improve athletic performance, physical appearance, and perceived social opportunity or self-esteem (Evans, 2004; Hildebrandt, Langenbucher, Carr, & SanJuan, 2007). The legal use of APEDs takes the form of nutritional supplements and occurs in approximately 49% of the U.S. population (Bailey, Gahche, Lentino, Dwyer, Engel, & Thomas, 2011). Purposes for supplement use include general health, weight loss, and muscle building. The most commonly used class of illicit APEDs is the anabolicandrogenic steroids (AASs). Approximately 3.3% of high school students use AASs in the United States (Centers for Disease Control, 2009), and they have reported increased rates of aggression, hostility (Beaver, Vaughn, Delisi, & Wright, 2008), and affective distress (Denham, 2009).
There are a number of psychological–behavioral risk factors that may increase the likelihood of illicit APED use. Eating and weight concerns, substance abuse, negative affect (Irving, Wall, Neumark-Sztainer, & Story, 2002; Vertalino, Eisenberg, Story, & Neumark-Sztainer, 2007), and body image disturbance (Hildebrandt, Alfano, & Langenbucher, 2010) are associated with illicit APED use in adolescents and adults. The developmental course that results in illicit APED use is not well understood, although it has been suggested that illicit AAS use may result in a syndrome of dependence (Kanayama, Brower, Wood, Hudson, & Pope, 2009). However, these traditional definitions have been challenged in favor of a unique substance use disorder that includes (a) polypharmacy, (b) dietary rigidity and compulsive exercise, and (c) body image disturbance (Hildebrandt et al., 2011). Consequently, theories characterizing the developmental trajectories of APED use are necessary to better understand AAS attainment and inform the nosology of APED use disorders.
An established model of adolescent substance use, the “gateway hypothesis,” postulates that drug use follows a chronological, causal sequence, whereby initial use of a specific drug leads to an increased likelihood of future drug use (Kandel, 1975). The gateway hypothesis posits that adolescent–young adult drug use progresses through several clear temporal developmental stages whereby the use of licit substances precedes and increases the risk for use of serious illicit substances (Kandel, 1975; Yamaguchi & Kandel, 1984). Although the causal mechanisms are still debated (Vanyukov et al., 2012), the gateway model offers a framework for characterizing the process of drug initiation and use.
We propose that the use of illicit APED may follow an analogous progression, whereby legal APEDs act as a gateway to AAS use. This gateway occurs by allowing nonusers access to the APED culture where they may garner access to illicit APEDs and develop attitudes and beliefs consistent with such use. The APED culture involves a hierarchy of knowledge and expertise communicated by experienced users (Evans, 1997; Monaghan, 2002) and may serve as a social mechanism of APED progression. Furthermore, we predict that this progression is correlated with psychological and social features, including body image disturbance, rigid dietary and exercise practices, and perfectionism.
Method
Participants
Two hundred and one (women = 101; men = 100) participants were recruited from the North Eastern Public University through campus flyers and electronic postings. All participants were currently using a nutritional supplement with 16% (n = 32) using an illicit APED. Participants were 19.17 (SD = 1.99) years old and had used supplements for an average of 4.24 (SD = 2.34) years. The majority self-identified as heterosexual 97.5% (n = 197), White non-Hispanic 55.7% (n = 112), African American–Black 19.9% (n = 40), Asian–East Indian 15.9% (n = 32), or other 8.0% (n = 17) with 10.0% (n = 20) identified as Black Hispanic. A total of 27 participants who completed questionnaires were excluded from the analysis because they could not recall the APED or could not describe its primary ingredients or intended. Participants received course credit for their participation, and procedures were approved by the university IRB.
Materials and Procedures
Muscle Dysmorphic Disorder Inventory (MDDI; Hildebrandt, Langenbucher, & Schlundt, 2004)
The MDDI is dimensional measure of muscle dysmorphia symptoms (α= .89) with established test–retest reliability and construct validity of these scales.
Eating Disorder Examination—Questionnaire (EDE–Q; Fairburn & Beglin, 1994)
The EDE–Q measures core eating disorder symptoms. It has four subscales (Eating Concern, Dietary Restraint, Shape Concern, and Weight Concern) and a global score (α= .83–.88) and 28 day totals for compulsive exercise and purging methods (fasting, vomiting, laxative, and diet pill use).
Male/Body Checking Questionnaire—Short Form (M/BCQ–SF; Alfano, Hildebrandt, Bannon, Walker, & Walton, 2010)
The M/BCQ–SF measures global aspects of male and female body checking–evaluation and has limited gender bias (BCQ–M α = .75 and BCQ–F α = .82).
Frost-Multidimensional Perfectionism Scale (FMPS; Frost et al., 1990)
The FMPS measures the construct of perfectionism and generates six subscales, three of which were used in this study [Concern Over Mistakes (CM), Doubts About Actions (DA), and Personal Standards (PS)]. The CM subscale reflects a tendency to be overly self-critical and self-evaluative, the DA subscale reflects uncertainty about one’s decisions, and the PS subscale reflects the setting of high performance standards (α= 78, α = .89, and α= .82, respectively).
Attitudes About Appearance and Performance Enhancing Drugs (A–APED)
The A–AED was designed for this study and consists of 15 items divided into two subscales (Safety of Illicit APEDs α = .81; Efficacy of Illicit APEDs α = .89) scored on a 5-point ordinal scale, ranging from −2 (I believe this to be absolutely false) to 2 (I believe this to be absolutely true). Participants were provided with a brief description of APEDs and asked to rate the degree to which they believe the following statements to be true. The safety items assess the degree to which one believes certain physical and psychological consequences will happen as a result of illicit APEDs (see Langenbucher, Hildebrandt, & Carr, 2008). The efficacy scale included items about APED’s efficacy to help in achieving the typical types of desired physical and psychological changes associated with illicit APEDs.
Appearance and Performance Enhancing Drug Use Checklist (APED–C)
The APED–C was also designed for this study and involved collecting information about supplement use in three broad categories (health–well-being, muscle building, & weight–fat loss). Participants wrote the name or major ingredients of all of the current and past nutritional supplements within each category. Additional questions asked the “age of first use of the [health, muscle building, weight–fat loss, illegal APED].” Follow-up questions included asking participants about how each supplement was used (as directed by packaging; under direction of a nonmedical expert; under direction of a medical professional; self-directed). In addition, they were asked, “How many people do you know well (e.g., well enough to call or spend time with) that use illegal substances to improve their appearance or physical performance?”
Demographics and Background Questionnaire
Information about age, race–ethnicity, height, weight, and gender were gathered from participants. Participants also self-reported 28-day drug and alcohol use, including nonprescription pain or psychiatric medicine. In addition, participants were asked,
Do you currently participate in an organized sport including club sports such as track, basketball, volleyball, wrestling, and so forth)? If so, on how many of the past 28 days have you been involved in training for or competing in these sports? Do not count exercise done for leisure or reasons other than organized sports.
Statistical Analysis
Descriptive statistics and between-group t tests or chi-square tests were used to characterize the sample and their APED use. To examine relationships between predictors and both types of APED use, we used covariance structure models to estimate unique effects of predictors on both supplement and illicit APED use. Models were evaluated based on overall goodness-of-fit statistics, comparative fit index (CFI), chi-square test, sample-size adjusted Bayesian Information Criterion (aBIC), and root-mean-square error of approximation (RMSEA). Higher CFI scores and low aBIC and RMSEA are considered evidence of better fit with RMSEA below .05 being considered evidence of acceptable model fit (Bentler & Dudgeon, 1996). For tests of indirect effects within the covariance structure models, we used the bias corrected bootstrap methods described by MacKinnon, Lockwood, and Williams (2004).
Results
Participants
Participants reported being engaged in organized sports (n = 80, 39.8%) of some kind, with the majority (n = 68, 85%) of these individuals being involved in club sports or recreational sports. Illegal drug use was reported by n = 74 (36.8%) of this sample. When including only those with nonalcohol based illicit drug use, n = 31 (15.4%) reported some illicit drug use in the past 28 days. The most commonly used drug was marijuana (n = 26, 12.9%). All individuals reported exercising in the past 28 days, on average 17.22 (SD = 6.11) days for an average of 70.87 min (SD = 63.22 min).
Description of APED Use
Participants reported currently using primarily health–well-being supplements (HW–S; n = 145–201, 72.1%) with individual or multivitamins (n = 120–201, 59.7%), sleep aids (n = 40–201, 19.9%; e.g., melatonin), immune-system enhancers (n = 37–201; 18.4%; e.g., echinacea), and mood enhancers (n = 18–201, 9.0%; e.g., St. John’s wort) being the most common. Current weight–fat-loss supplements (WFL–S) were reported by n = 110 participants (54.7%; e.g., ephedra, caffeine, and/or mau huang-based products) and included 33 different substances. Muscle building supplements (MB–S) were reported by n = 106 participants (52.7%; e.g., protein powder) with protein powder (n = 92; 45.8%), creatine (n = 88; 43.8%), and prohormones (n = 44; 21.9%; e.g., androstenedione) as the most common. The average number of current supplements was 2.96 (SD = 4.6; range = 1–18) cost students $84.96 (SD = 86.41) per month.
Men were more likely to use MB–S than women (86 vs. 20; odds ratio [OR] = 24.89, 95% confidence interval [CI] = 11.11–56.80, p < .001) and women were more likely to use WFL–S (75 vs. 35; OR = 4.19, 95% CI = 2.23–7.92, p < .001). There was no significant difference in the current use of HW-S use (men = 72; women = 73; OR = 0.99, 95% CI = .51–1.91, p = 1.0). Men endorsed using all three supplements more often than women (30 vs. 7; OR = 5.78, 95% CI = 2.25–15.34, p < .001). Those using just the combination of both MB–S and WLF–S were also higher among men (40 vs. 4; OR = 16.17, 95% CI 5.17–56.22, p < .001). Men reported a greater total number (4.1 vs. 1.8; t = 7.61, p < .001, Cohen’s d = 0.92) and greater amount of money spent per month on supplements (t = 10.69, p < .001, Cohen’s d = 1.60).
A total of 32 participants reported current illicit APED use with all 32 reporting some form of AAS use as part of their APED use. Men were more likely to be using illicit APEDs (28 vs. 4; OR = 9.431, 95% CI = 2.97–33.29, p < .001). Those who reported using illicit APEDs reported using more supplements (6.21 vs. 2.35, t = 4.32, p < .001, Cohen’s d = 0.77) and spent more money on their APEDs ($310.55 vs. $42.25/month, t = 15.31, p < .001, Cohen’s d = 2.32). Among the 32 illicit APED users, all of them reported using supplements prior to their use of illicit APEDs (16.31 years old vs. 19.59 years old; t = 5.57, p < .001, Cohen’s d = −1.53).
Global Gateway Model
Table 1 reports the means, standard deviations and partial correlations (controlling for gender) of the psychosocial measures. Body image disturbance had the highest single partial correlation with illicit APED use. There were are also similar significant positive relationships between specific aspects of perfectionism, eating disorder symptoms, male-oriented body checking, compulsive exercise and both types of APED use (legal and illegal).
Table 1.
Means, Standard Deviations, and Intercorrelations of Predictors APED Use
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Personal standards | — | ||||||||||||||||||
| 2. Concern over mistakes | 0.48 | — | |||||||||||||||||
| 3. Doubts about actions | 0.24 | 0.45 | — | ||||||||||||||||
| 4. MDDI total | 0.35 | 0.35 | 0.09 | — | |||||||||||||||
| 5. Non APED drag use | 0.04 | 0.05 | 0.02 | 0.25 | — | ||||||||||||||
| 6. Sport participation | 0.39 | 0.3 | 0.18 | 0.28 | 0.17 | — | |||||||||||||
| 7. Licit APEDs | 0.48 | 0.11 | −0.02 | 0.55 | 0.34 | 0.54 | — | ||||||||||||
| 8. Illicit APEDs | 0.39 | 0.14 | −0.07 | 0.6 | 0.39 | 0.49 | 0.69 | — | |||||||||||
| 9. Purging | 0.30 | 0.30 | 0.35 | 0.09 | 0.11 | 0.02 | 0.08 | 0.02 | — | ||||||||||
| 10. Compulsive exercise | 0.34 | 0.32 | 0.04 | 0.27 | 0.08 | 0.34 | 0.32 | 0.37 | 0.20 | — | |||||||||
| 11. BCQ-male | 0.68 | 0.62 | 0.44 | 0.69 | 0.35 | 0.21 | 0.30 | 0.40 | 0.26 | 0.5 | — | ||||||||
| 12. BCQ-female | 0.66 | 0.49 | 0.42 | −0.05 | 0.11 | 0.22 | 0.25 | 0.31 | 0.68 | 0.56 | 0.4 | — | |||||||
| 13. APED-safety | 0.4 | 0.54 | 0.2 | 0.56 | 0.77 | 0.69 | 0.84 | 0.89 | 0.31 | 0.40 | 0.37 | 0.24 | — | ||||||
| 14. APED-efficacy | 0.45 | 0.26 | 0.01 | 0.53 | 0.75 | 0.45 | 0.80 | 0.92 | 0.20 | 0.53 | 0.45 | 0.34 | 0.57 | — | |||||
| 15. Eating concern | 0.43 | 0.6 | 0.5 | 0.14 | 0.05 | 0.14 | 0.25 | 0.21 | 0.38 | 0.33 | 0.26 | 0.50 | −0.04 | 0.07 | — | ||||
| 16. Restraint | 0.19 | 0.23 | 0.25 | 0.25 | 0.02 | 0.31 | 0.27 | 0.22 | 0.40 | 0.41 | 0.37 | 0.46 | 0.07 | −0.03 | 0.60 | — | |||
| 17. Shape concern | 0.44 | 0.39 | 0.43 | 0.51 | 0.26 | 0.25 | 0.30 | 0.31 | 0.36 | 0.33 | 0.52 | 0.65 | 0.13 | 0.15 | 0.49 | 0.51 | — | ||
| 18. Weight concern | 0.36 | 0.41 | 0.32 | 0.31 | 0.12 | 0.3 | 0.32 | 0.33 | 0.39 | 0.35 | 0.29 | 0.39 | 0.16 | 0.12 | 0.45 | 0.69 | 0.70 | — | |
| 19. EDE-Q total | 0.34 | 0.5 | 0.35 | 0.18 | 0.10 | 0.18 | 0.33 | 0.32 | 0.37 | 0.36 | 0.35 | 0.50 | 0.07 | 0.09 | 0.52 | 0.45 | 0.47 | 0.48 | — |
| M | 22.3 | 21.1 | 9.7 | 23.4 | 8.4 | 7.3 | 3.0 | 2.2 | 8.9 | 13.2 | 15.1 | 27.3 | 21.4 | 2.3 | 1.9 | 2.2 | 3.1 | 2.7 | |
| SD | 7.8 | 9.4 | 3.6 | 7.3 | 13.2 | 14.2 | 4.2 | 1.5 | 7.9 | 4.6 | 5.5 | 7.5 | 8.2 | 1.5 | 2.3 | 1.9 | 2.0 | 1.9 |
Note. APED = appearance and performance enhancing drag use; MDDI = measures of muscle dysmorphia; BCQ = Body Checking Questionnaire; EDE–Q = Eating Disorder Examination—Questionnaire. All correlations are controlled for the effects of gender. Correlations in boldface type are not significant at p < .05.
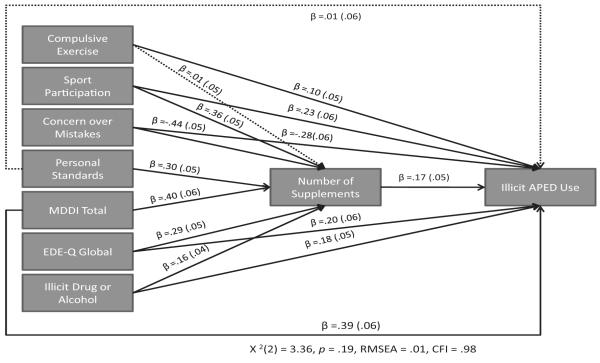
To test an initial gateway model, we estimated a covariance structure model (CSM) of APED use. To model the gateway effect, we placed supplement use upstream of the illicit APED use to demonstrate the time ordered relationship indicated by age of onset data (see Figure 1). We compared this model to the same set of predictors, but with illicit and legal supplements reversed and the predictors of Model 1 being downstream of Model 2. The goodness of fit indicators for Model 2 were considerably worse than Model 1: Model 1, CFI = 0.98, RMSEA = 0.02, aBIC = 4470.62; versus Model 2, CFI = 0.93, RMSEA = 0.08, aBIC = 4527.91.
Figure 1.
The model above was estimated using gender as a control variable and controlling for the covariance between independent variables, which were not depicted to ease in interpretation. It summarizes the general gateway model designed to identify nonspecific risk factors of illicit appearance and performance enhancing drugs (APED) use. The dotted lines represent paths that were deleted in the final model. Illicit APED use is a dichotomous variable and the coefficient reported predicting this dependent variable are logit parameters, and all parameters are unstandardized.
Gateway Mechanism Model
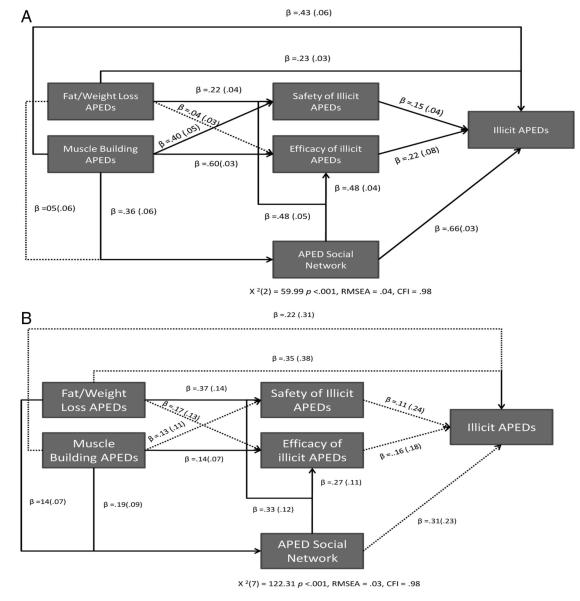
To investigate the possible mechanisms by which supplement use brings about illicit APED use, we constructed a separate CSM to examine the relationship between supplement use and illicit APED use through attitudes about the safety and efficacy of illicit APEDs and size of APED social network. Figure 2A depicts the best-fitting model for the complete sample. We compared this model to a model with paths reversed and found evidence of superior goodness of fit for Model 1: Model 1, CFI = 0.98, RMSEA = 0.04, aBIC = 2380.56; versus Model 2, CFI = 0.77, RMSEA = 0.64, aBIC = 2612.17. HW–S use was unrelated to mediating variables and was subsequently dropped from the model. There was a differential relationship between MB–S and FWL–S and beliefs about illicit APEDs with FWL–S use being unrelated to illicit APED efficacy. We also estimated a female specific model (see Figure 2b) but dropped illicit APED use due to low power. FWL–S use was correlated with safety beliefs about APEDs and APED social network, suggesting gender specificity in these relationships.
Figure 2.
A: The specific gateway model above reports unstandardized regression coefficients. The dotted lines represent paths that were deleted in the final model. Each nutritional supplement and illicit appearance and performance enhancing drugs (APED) use were included as dichotomous variables. The coefficient reported for paths between predictors and illicit APED use is in logit scale. RMSEA = root-mean-square error of approximation; CFI = comparative fit index. B: The model was also tested only with women to examine for potential gender differences in the relationship between supplement us and potential mediators of APED use. Unique to women were the contribution of both fat–weight loss and muscle-building supplements to APED use and a lack of a significant relationship between muscle building APED use and safety of illicit APEDs.
Table 2 displays estimated indirect effects of both types of supplements on APED use. There was evidence of several single and multiple indirect effects of supplement use on illicit APED use. The results suggest MB–S carry their relationship with APED use through the number of APED users in their social network and through greater certainty in their beliefs that illicit APEDs are both safe and efficacious. Similarly, FWL–S carried their indirect effects through the size of individual’s APED network and their beliefs about the safety, but not efficacy, of illicit APEDs.
Table 2.
Summary of Indirect Effects With Bootstrap Bias Corrected Standard Errors for Supplements on Illicit APED Use
| Predictor | Via | Partial indirect effect | Total indirect effect |
|---|---|---|---|
| Muscle building supplements | APED efficacy APED network |
.129 (.114–.133) .042 (.038–.048) |
|
| .170 (.161–.177) | |||
| Muscle building supplements | APED safety APED network |
.061 (.049–.075) .029 (.018–.034) |
|
| .090 (.083–.091) | |||
| Muscle building supplements | APED network | .267 (.263–.275) | |
| Fat–Weight Loss supplements | APED safety APED network |
.034 (.019–.045) .004 (−.001–.012) |
|
| .038 (.018–.050) |
Note. APED = appearance and performance enhancing drug use. 95% confidence intervals in parentheses.
Discussion
Our preliminary study indicated that regular supplement use may be an important factor in the development and risk for illicit APED use among college students, independent of sports participation, body image disturbance, or other illicit drug use. These latter factors have previously been linked with AAS use among adolescents (Bahrke, Yesalis, Kopstein, & Stephens, 2000; Irving et al., 2002) and adults (Pope, Kanayama, & Hudson, 2011). A more detailed analysis of the gateway process revealed that risk for illicit APED use is partially explained by contact with illicit APED users and the positive beliefs about the safety and efficacy of APEDs. This process is consistent with other models of illicit drug use, which suggest that social groups facilitate initiation of drug use (Branstetter, Low, & Furman, 2011). This relationship between peers, family, and larger social context is complex; and it is likely to involve some social norm development around the substance in question (Scull, Kupersmidt, Parker, Elmore, & Benson, 2011). Our study supports the possibility that these social norms develop in the form of attitudes that promote the safety and efficacy of illicit APED use. Such views–beliefs may be communicated to supplement users through the information and experience associated with supplements themselves or through social contact with those using AASs. Although our cross-sectional models are preliminary, these results do raise the possibility that supplement use increases access to an APED culture, where illicit forms of APED use are modeled and norms reinforce the safety and efficacy of the substances.
There was evidence of gender differences in the types of supplements used and the relative effect of these substances on attitudes about APEDs and the social network of APED users. To be specific, use of FWL–S was associated with more favorable attitudes toward APEDs and a larger network of current illicit APED users. The same effect was not found for men. Female AAS use in the general population is rare (Kanayama, Boynes, Hudson, Field, & Pope, 2007), and our sample suggests this is true for supplement using female individuals as well. There are likely to be general and gender-specific risk factors for illicit APED use as assumed in existing APED prevention programs (Elliot et al., 2004; Goldberg et al., 1996, 2000).
In addition to identifying a unique role for nutritional substance use, eating disorder pathology and specific aspects of perfectionism were also positively associated with both supplement and illicit APED use. The majority of risk-based studies have focused on either body image disturbance or impulsive behavior (e.g., drug use, impulsive aggression, etc.), therefore, this finding is novel. For women, eating disorders symptoms have been associated with appearance-altering drug use (Elliot et al., 2004) although perfectionism and APED use in women has not been explored. Thus, there appears a larger cluster of symptoms including exercise, dietary control, body image disturbance, and substance use that uniquely contribute to APED use.
In an effort to endorse a gateway model for illicit APED use, further evidence is still required. Although cross-sectional relationships are robust in this study, they may be weaker when examined in a longitudinal context. Thus, we cannot conclude that the evidence of indirect effects of supplement use through social contact or beliefs about illicit APEDs are also evidence of a causal mechanism. We encourage caution in interpreting these findings and suggest that longitudinal research is needed to further test this theory. The potential for a gateway risk appears to be specific to substances marketed to increase lean muscle mass or reduce weight and may be due to a multitude of factors including availability, relative safety, and legality.
In addition to the potential for examining this gateway model in longitudinal samples, at least four other questions need to be considered. First, the proposed model does not consider biological mechanisms for the changes in risk associated with supplemental use. It is possible that either the pharmacological properties of some supplements or contaminants of existing supplements may inadvertently expose individuals to the types of biological effects found among illicit APEDs (Geyer et al., 2008; Kicman, 2008). Second, the age range was restricted to college students from a single university, therefore, testing this model in other populations will be essential to generalizability. Third, there is ample evidence to support the presence of unique subtypes of APED users (e.g., Hildebrandt et al., 2010), and the potential for these subtypes to predate initiation of APED use may be an important goal in identifying APED risk. Finally, future studies should include a nonsupplement-using control group. Although AAS is rare among nonsupplement users (Evans, 1997; Parkinson & Evans, 2006), the nonsupplement-using APED user may represent an important subtype with a unique set of risk factors and outcomes.
Acknowledgments
Research conducted was supported by Grants DA 024043-04 and L30 DA0237709-01 awarded to Tom Hildebrandt by the National Institutes on Drug Abuse.
Contributor Information
Tom Hildebrandt, Eating and Weight Disorders Program, Mount Sinai School of Medicine, New York, New York.
Seth Harty, Eating and Weight Disorders Program, Mount Sinai School of Medicine, New York, New York.
James W. Langenbucher, Department of Psychology, Rutgers, The State University of New Jersey
References
- Alfano L, Hildebrandt T, Bannon K, Walker C, Walton KE. The impact of gender on the assessment of body checking behavior. Body Image. 2011;8:20–25. doi: 10.1016/j.bodyim.2010.09.005. doi:10.1016/j.bodyim.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahrke MS, Yesalis CE, Kopstein AN, Stephens JA. Risk factors associated with anabolic-androgenic steroid use among adolescents. Sports Medicine. 2000;29:397–405. doi: 10.2165/00007256-200029060-00003. doi:10.2165/00007256-200029060-00003. [DOI] [PubMed] [Google Scholar]
- Bailey RL, Gahche JJ, Lentino CV, Dwyer JT, Engel JS, Thomas PR. Dietary supplement use in the United States, 2003–2006. Journal of Nutrition. 2011;141:261–266. doi: 10.3945/jn.110.133025. doi:10.3945/jn.110.133025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaver KM, Vaughn MG, Delisi M, Wright JP. Anabolic-androgenic steroid use and involvement in violent behavior in a nationally representative sample of young adult males in the United States. American Journal of Public Health. 2008;98:2185–2187. doi: 10.2105/AJPH.2008.137018. doi:10.2105/AJPH.2008.137018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM, Dudgeon P. Covariance structure analysis: Statistical practice, theory, and directions. Annual Review of Psychology. 1996;47:563–592. doi: 10.1146/annurev.psych.47.1.563. doi:10.1146/annurev.psych.47.1.563. [DOI] [PubMed] [Google Scholar]
- Branstetter SA, Low S, Furman W. The influence of parents and friends on adolescent substance use: A multidimensional approach. Journal of Substance Use. 2011;16:150–160. doi: 10.3109/14659891.2010.519421. doi:10.3109/14659891.2010.519421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Youth Risk Behavior Surveillance. Surveillance Summaries. 2009 Jun;59:SS–5. MMWR 2010. [Google Scholar]
- Denham BE. Determinants of anabolic-androgenic steroid risk perceptions in youth populations: A multivariate analysis. Journal of Health and Social Behavior. 2009;50:277–292. doi: 10.1177/002214650905000303. doi:10.1177/002214650905000303. [DOI] [PubMed] [Google Scholar]
- Elliot DL, Goldberg L, Moe EL, Defrancesco CA, Durham MB, Hix-Small H. Preventing substance use and disordered eating: Initial outcomes of the ATHENA (athletes targeting healthy exercise and nutrition alternatives) program. Archives of Pediatrics & Adolescent Medicine. 2004;158:1043–1049. doi: 10.1001/archpedi.158.11.1043. doi:10.1001/archpedi.158.11.1043. [DOI] [PubMed] [Google Scholar]
- Evans NA. Gym and tonic: A profile of 100 male steroid users. British Journal of Sport Medicine. 1997;31:54–58. doi: 10.1136/bjsm.31.1.54. doi:10.1136/bjsm.31.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans NA. Current concepts in anabolic-androgenic steroids. American Journal of Sports Medicine. 2004;32:534–542. doi: 10.1177/0363546503262202. doi:10.1177/0363546503262202. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Frost R, Marten P, Lahart C, Rosenblate R. The dimensions of perfectionism. Cognitive Therapy and Research. 1990;14:449–468. [Google Scholar]
- Geyer H, Parr MK, Koehler K, Mareck U, Schanzer W, Thevis M. Nutritional supplements cross-contaminated and faked with doping substances. Journal of Mass Spectrometry. 2008;43:892–902. doi: 10.1002/jms.1452. doi:10.1002/jms.1452. [DOI] [PubMed] [Google Scholar]
- Goldberg L, Elliot D, Clarke GN, MacKinnon DP, Moe E, Zoref L, Lapin A. Effects of a multidimensional anabolic steroid prevention intervention. The Adolescents Training and Learning to Avoid Steroids (ATLAS) Program. JAMA: Journal of the American Medical Association. 1996;276:1555–1562. doi:10.1001/jama.1996.03540190027025. [PubMed] [Google Scholar]
- Goldberg L, MacKinnon DP, Elliot DL, Moe EL, Clarke G, Cheong J. The adolescents training and learning to avoid steroids program: Preventing drug use and promoting health behaviors. Archives of Pediatrics & Adolescent Medicine. 2000;154:332–338. doi: 10.1001/archpedi.154.4.332. [DOI] [PubMed] [Google Scholar]
- Hildebrandt T, Alfano L, Langenbucher J. Body image disturbance among 1000 appearance and performance enhancing drug users. Journal of Psychiatric Research. 2010;44:841–846. doi: 10.1016/j.jpsychires.2010.01.001. doi:10.1016/j.jpsychires.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt T, Lai JK, Langenbucher JW, Schneider M, Yehuda R, Pfaff DW. The diagnostic dilemma of pathological appearance and performance enhancing drug use. Drug and Alcohol Dependence. 2011;114:1–11. doi: 10.1016/j.drugalcdep.2010.09.018. doi:10.1016/j.drugalcdep.2010.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt T, Langenbucher JW, Carr SJ, Sanjuan P. Modeling population heterogeneity in appearance- and performance-enhancing drug (APED) use: Applications of mixture modeling in 400 regular APED users. Journal of Abnormal Psychology. 2007;116:717–733. doi: 10.1037/0021-843X.116.4.717. doi:10.1037/0021-843X.116.4.717. [DOI] [PubMed] [Google Scholar]
- Hildebrandt T, Langenbucher J, Schlundt DG. Muscularity concerns among men: Development of attitudinal and perceptual measures. Body Image. 2004;1:169–181. doi: 10.1016/j.bodyim.2004.01.001. doi:10.1016/j.bodyim.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Irving LM, Wall M, Neumark-Sztainer D, Story M. Steroid use among adolescents: Findings from Project EAT. Journal of Adolescent Health. 2002;30:243–252. doi: 10.1016/s1054-139x(01)00414-1. doi:10.1016/S1054-139X(01)00414-1. [DOI] [PubMed] [Google Scholar]
- Kanayama G, Boynes M, Hudson JI, Field AE, Pope HG., Jr. Anabolic steroid abuse among teenage girls: An illusory problem? Drug and Alcohol Dependence. 2007;88:156–162. doi: 10.1016/j.drugalcdep.2006.10.013. doi:10.1016/j.drugalcdep.2006.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanayama G, Brower KJ, Wood RI, Hudson JI, Pope HG. Anabolic-androgenic steroid dependence: An emerging disorder. Addiction. 2009;104:1966–1978. doi: 10.1111/j.1360-0443.2009.02734.x. doi:10.1111/j.1360-0443.2009.02734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel D. Stages in adolescent involvement in drug-use. Science. 1975 Nov 28;190:912–914. doi: 10.1126/science.1188374. doi:10.1126/science.1188374. [DOI] [PubMed] [Google Scholar]
- Kicman AT. Pharmacology of anabolic steroids. British Journal of Pharmacology. 2008;154:502–521. doi: 10.1038/bjp.2008.165. doi:10.1038/bjp.2008.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langenbucher J, Hildebrandt T, Carr S, editors. Medical consequences of performance enhancing drug use. 2nd ed Hawthorne Medical Press; New York, NY: 2008. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. doi:10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan LF. Vocabularies of motive for illicit steroid use among bodybuilders. Social Science & Medicine. 2002;55:695–708. doi: 10.1016/s0277-9536(01)00195-2. doi:10.1016/S0277-9536(01)00195-2. [DOI] [PubMed] [Google Scholar]
- Parkinson AB, Evans NA. Anabolic androgenic steroids: A survey of 500 users. Medicine and Science in Sports and Exercise. 2006;38:644–651. doi: 10.1249/01.mss.0000210194.56834.5d. doi:10.1249/01.mss.0000210194.56834.5d. [DOI] [PubMed] [Google Scholar]
- Pope HG, Jr., Kanayama G, Hudson JI. Risk factors for illicit anabolic-androgenic steroid use in male weightlifters: A cross-sectional cohort study. Biological Psychiatry. 2012;71:254–261. doi: 10.1016/j.biopsych.2011.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope HG, Kean J, Nash A, Kanayama G, Samuel DB, Bickel WK. A diagnostic interview module for anabolic-androgenic steroid dependence: Preliminary evidence of reliability and validity. Experimental and Clinical Psychopharmacology. 2010;18:203–213. doi: 10.1037/a0019370. doi:10.1037/a0019370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scull TM, Kupersmidt JB, Parker AE, Elmore KC, Benson JW. Adolescents’ media-related cognitions and substance use in the context of parental and peer influences. Journal of Youth and Adolescence. 2010;39:981–998. doi: 10.1007/s10964-009-9455-3. doi:10.1007/s10964-009-9455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ, Ridenour TA. Common liability to addiction and “gateway hypothesis”: Theoretical, empirical and evolutionary perspective. Drug and Alcohol Dependence. 2012 doi: 10.1016/j.drugalcdep.2011.12.018. [Epub ahead of print, January 18, 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vertalino M, Eisenberg ME, Story M, Neumark-Sztainer D. Participation in weight-related sports is associated with higher use of unhealthful weight-control behaviors and steroid use. Journal of the American Dietetic Association. 2007;107:434–440. doi: 10.1016/j.jada.2006.12.010. doi:10.1016/j.jada.2006.12.010. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K, Kandel DB. Patterns of drug-use from adolescence to young adulthood: II sequences of progression. American Journal of Public Health. 1984;74:668–672. doi: 10.2105/ajph.74.7.668. doi:10.2105/AJPH.74.7.668. [DOI] [PMC free article] [PubMed] [Google Scholar]