Abstract
Objective
The purpose of this study was to examine work activities associated with work-related injury (WRI) in occupational and physical therapy.
Participants
1,158 occupational and physical therapists in Wisconsin responded to a mailed survey, from a total of 3,297 OTs and PTs randomly selected from the State licensure list.
Methods
The study used a cross-sectional, survey design. Participants reported information about WRI they sustained between 2004 and 2006, including the activities they were performing when injured. Investigators analyzed 248 injury incidents using qualitative and quantitative analysis.
Results
Data were examined across OT and PT practice in general, and also by practice area. Manual therapy and transfers/lifts were associated with 54% of all injuries. Other activities associated with injury were distinct to practice area, for example: floor work in pediatrics; functional activities in acute care; patient falls in skilled nursing facilities; and motor vehicle activities in home care.
Conclusions
Injury prevention activities must address transfers and manual therapy, but also must examine setting-specific activities influenced by environment and patient population.
Keywords: Occupational Injury, Therapy Activities, Pediatrics, Skilled Nursing Facilities, Rehabilitation, Home Health
1. Introduction
Occupational (OTs) and physical therapists (PTs) have substantial and similar rates of work-related injury (WRI), musculoskeletal pain and musculoskeletal disorders (WMSD) [1,3,5,7,9,14,29]. Among PTs, a prospective cohort study [3] found a one year incidence of 20.7% for moderate to major WMSDs in any body region among a randomly selected national sample of 882 PTs (case definition of WMSD: pain severity of 4/10 or higher and present at least once a month or lasting longer than a week). Darragh et al.[7] reported an annual WRI incidence rate among OTs and PTs of 16.5 and 16.9 per 100 full-time workers, respectively. Among those who did not report a WRI, Darragh et al. found an annual prevalence of WMSD of 18% and 16%, respectively, using the same case definition [7].
There are common therapeutic activities that appear to be associated with various WMSD and WRI. Patient handling (transfers, repositioning and patient lifting) and manual therapy (soft tissue work, joint mobilization, and orthpedic techniques) are the most consistently cited tasks associated with WMSDs among health care workers [3,12,24,30]. Campo et al.[3] reported that therapists who transferred patients 6 to 10 times per day had odds of moderate to severe low back WMSDs that were 2.4 times as high as those who did not transfer patients. Those who repositioned patients more than 10 times per day had odds of moderate to severe low back WMSDs that were 2.61 times as high as those who did not reposition patients. Hignett [11] reported that OTs in acute care identified patient handling as a risk factor for WRI. According to the Bureau of Labor Statistics in 2004, patient care activities (patient lifting in particular) were responsible for 100% of all OT WRI where the source was known and where time away from work was recorded. Patient lifting accounted for 71% of injuries to OTs [2].
Manual therapy (joint mobilization, passive range of motion/stretching and soft tissue work) also has been identified as a risk factor for musculoskeletal pain and WMSD. Campo et al. [3] reported that soft tissue work and joint mobilization techniques were associated with increased odds of WMSDs in the wrist and hand. Power & Flemming [24] found that manual and manipulative techniques were identified as associated with thumb pain in 56% of Irish PTs with symptoms. In a study of Australian PTs with thumb pain, 100% of participants attributed their pain to manual techniques, in particular, posterior to anterior spinal mobilization and soft tissue massage [25]. Wajon & Ada [28] identified spinal manipulative therapy, unilateral and central posteroanterior glides in particular, as responsible for thumb pain among Australian PTs.
Studies to date have focused on the major job tasks that are associated with WRI, WMSD, and pain in therapists. However, occupational and physical therapists perform a wide variety of work activities, and current research has reported primarily on transfers and manual therapy. OT and PT also practice in a wide range of settings, and the physical demands vary across those settings. For example, hospital-based practitioners attend to patients with complex medical conditions, requiring assistance with transfers, gait training, and activities of daily living (ADL) training. Outpatient therapists attend to patients with more mobility who may require manual therapy and splint fabrication, which carry a separate set of risks. Pediatric therapists may practice in school systems, interacting with an environment designed for typically developing children, not those with disabilities. Past research with construction workers has demonstrated the benefit of trade-specific analysis [15]. This approach would be useful for examining differences in characteristics of WMSD or WRI between the major practice areas. The present study examined work activities associated with self-reported WRI among OT and PT in all practice areas and in the five most common practice areas. The purpose of this study was: 1) to describe the range of work-related activities associated with WRI across all practice areas and 2) to describe the association between WRI, activity and practice area in occupational and physical therapists in the state of Wisconsin in 2004, 2005, and 2006.
2. Methods and Materials
2.1. Research Design
A cross-sectional, non-experimental design was used for this study. Associations between the following major variables were evaluated: work-related injury, practice area, and work-related activity. Injury data were obtained through self-report, in response to the following question: “Did you sustain or develop any injuries in any of the last three years that you believe are related to your work?” This terminology was chosen in order to capture as many different types of injury (as defined by the participant) as possible. Participants selected their primary practice area from a list on the questionnaire. They were able to write in a practice area if necessary. Study participants also provided a short statement on the survey questionnaire about the work-related activity they were performing when injured. These statements were coded by type of activity by the investigators.
2.2. Population and survey procedures
Researchers randomly selected and mailed surveys to 50% of all licensed occupational and physical therapists who resided in the state of Wisconsin (1,436 OTs and 1,861 PTs). Investigators mailed a pre-survey postcard to all potential participants. One week later, they sent a cover letter, demographic information page, questionnaire, and a stamped, self-addressed envelope. All responses were confidential and no personal identifiers were included in the survey. After a three-week waiting period, the mailing was repeated. No surveys were opened until the second mailing was completed. The Institutional Review Board at the University of Wisconsin-Milwaukee approved all study procedures.
2.3. Instrumentation
Researchers developed the survey questionnaire using two published instruments previously used with physical therapists [3,14]. The survey combined elements of a questionnaire designed by Holder et al. [14], designed to capture self-reports of injury in physical therapists, and Campo et al. [3], designed to identify and describe work-related musculoskeletal disorders in physical therapists [7,16]. The survey consisted of three parts: Section A, basic demographic and work history information; Section B, a self-report of WRI; and Section C, questions about musculoskeletal symptoms experienced in the past year, completed only by those who did not report an injury in Section B. The present paper is based only on Section A and Section B. It relied on self-report of WRI sustained in each of three years (2004, 2005, and 2006) and included questions regarding the characteristics of the injury that most interfered with job performance. Prior to dissemination, the survey was distributed to occupational and physical therapists for content and structural review, and revised based on their feedback.
To assess work-related injury, participants were asked, “Did you sustain or develop any injuries in any of the last three years that you believe are related to your work?” The term “injury” was presented generically, and the wording, “sustain or develop” was crafted in an attempt to capture those who experienced a sudden-onset WRI and those who experienced a condition that emerged over time. If “Yes”, they were directed to complete a table with the number of injuries sustained in each of the three years, the number of injuries causing at least a half day of lost work time, and whether they reported and sought treatment for their injuries. In addition, they answered a series of questions in regards to the one injury that most interfered with their primary clinical practice, including setting, body part injured, type of injury (e.g.: contusion, strain, sprain, with an option to write in more details or alternate type of injury), and contributing factors (e.g: awkward postures, bending, twisting, with an option to write in more details, or an alternate factor). The variables were based on self-report. Finally, they were asked about work-related activity; “Describe the activity that most closely describes what you were doing when you sustained your injury.” This was an open-ended question with responses that were entered verbatim into the database.
2.4. Data Analysis
A qualitative approach was used to analyze descriptions of activities in which therapists were engaged when the WRI occurred. The first two authors individually organized these descriptions into categories, such as ‘transfers’, ‘ADL’, or ‘stair training’. We then met to discuss the categories, review the descriptions, and collapse the categories into a master code list. For example, ‘ADL’ and ‘stair training’ were collapsed into ‘Functional Activities’. We individually recoded the descriptions a second time, using the master code list as a guide, then discussed our coding decisions in order to achieve consensus about the most appropriate code for each description. We then recoded all the descriptions based on this consensus, and we reviewed the descriptions for a final time to be sure they accurately reflected the meaning of each description. In the event a therapist identified more than one activity, e.g. ‘transfer training’ and ‘gait training’, we coded the activity as ‘Multiple Activities’ since the contribution of each activity could not be assessed. Examples of the codes and associated descriptions are included in the results to illustrate specific activities and variations in those activities between settings [Table 2].
Table 2.
Work-related activities associated with injuries to selected body parts, all practice areas between 2004 and 2006.
| Work-related activities and body part injured | Proportion of injuries (n=248) | Description |
|---|---|---|
| Manual Therapy | 27.4% (n=68) | Joint mobilization, soft tissue work, passive range of motion, massage, lymphedema massage and wrapping, and other hands-on patient activities. |
| Wrist/Hand | 69.1% (n=47) | |
| Elbow | 19.1% (n=13) | |
| Shoulder | 14.7% (n=10) | |
| Head/Neck | 10.3% (n=7) | |
| All Other | 17.6% (n=12) | |
| Transfer/Lift | 26.6% (n=66) | Transfer training, transfers occurring during other activities such as ADL |
| Low back | 53.0% (n=35) | |
| Shoulder | 19.7% (n=13) | |
| Head/Neck | 18.2% (n=12) | |
| Upper back | 10.6% (n=7) | |
| All Other | 16.7% (n=11) | |
| Environment/Equipment | 10.9% (n=27) | Carrying laptops, bags, bolsters; tripping over or moving equipment, like mats, bolsters, and weights; working with broken equipment (wheelchairs, oxygen tank), sitting in child-sized chairs |
| Low back | 22.2% (n=6) | |
| Shoulder | 22.2% (n=6) | |
| Wrist/Hand | 18.5% (n=5) | |
| Knee | 14.8% (n=4) | |
| All Other | 29.6% (n=8) | |
| Multiple Activities | 6.5% (n=16) | Injuries attributed to multiple types of activity, e.g. transfer and manual therapy; transfer and floor work |
| Low back | 56.3% (n=9) | |
| Wrist/Hand | 37.5% (n=6) | |
| Shoulder | 25.0% (n=4) | |
| Elbow | 25.0% (n=4) | |
| All Other | 50.0% (n=8) | |
| Patient Fall | 5.7% (n=14) | Therapist struck by falling patient; therapist lowering a patient to the floor during a fall |
| Low back | 64.3% (n=9) | |
| Upper back | 35.7% (n=5) | |
| Head/Neck | 21.4% (n=3) | |
| Elbow/Hand | 14.3% (n=2) | |
| Knee | 7.1% (n=1) | |
| Clerical | 4.4% (n=11) | Documentation, laptop use |
| Wrist/Hand | 63.6% (n=7) | |
| Head/Neck | 27.3% (n=3) | |
| Upper back | 18.2% (n=2) | |
| Shoulder | 9.1% (n=1) | |
| Elbow | 9.1% (n=1) | |
| Functional Activities | 4.0% (n=10) | ADL training, gait training, stair training |
| Low back | 60.0% (n=6) | |
| Head/Neck | 10% (n=1) | |
| Upper back | 10.0% (n=1) | |
| Shoulder | 10.0% (n=1) | |
| Elbow/Wrist/Hand | 10.0% (n=2) | |
| Floor Work | 2.8% (n=7) | Sitting on floor, providing treatment on floor |
| Low back | 42.9% (n=3) | |
| Head/Neck | 28.6% (n=2) | |
| Upper back | 14.3% (n=1) | |
| Knee | 28.6% (n=2) | |
| Patient Aggression or | 2.4% (n=6) | Therapist hit, bitten, kicked by patient, therapist restraining agitated patient |
| Restraint | 33.3% (n=2) | |
| Head/Neck | 16.7% (n=1) | |
| Shoulder | 16.7% (n=1) | |
| Wrist/Hand | 16.7% (n=1) | |
| Knee | 16.7% (n=1) | |
| Therapeutic Exercise | 1.6% (n=4) | Implementing exercise programs |
| Low back | 25.0% (n=1) | |
| Wrist/Hand | 25.0% (n=1) | |
| Hip/Thigh | 25.0% (n=1) | |
| Foot | 25.0% (n=1) | |
| Motor Vehicle | 1.2% (n=3) | Motor vehicle crash; extended time driving |
| Head/Neck | 33.3% (n=1) | |
| Shoulder | 33.3% (n=1) | |
| Elbow | 66.7% (n=2) | |
| Wrist/Hand | 33.3% (n=1) | |
| Knee | 66.7% (n=2) | |
| Ankle/Foot | 33.3% (n=1) | |
| Other/Unknown | 6.5% (n=16) | Debriding a wound; aquatic therapy; no activity provided |
Basic descriptive and inferential analyses, including one way analyses of variance with Tukey’s procedure for post hoc testing, Pearson’s chi-square, and Fisher’s exact test, were conducted to describe injuries to all therapists and compare therapists by practice setting. In particular, Pearson’s chi-square test was used to assess whether certain activities associated with injury were over-represented in any one practice area, as compared to all other practice areas (Fisher’s exact was used for comparisons with expected cell values <5), a strategy used by Hunting et al. [15] in their comparison of injuries among construction trades. An alpha level of 0.05 was used for all statistical tests.
3. Results
3.1. Participant Characteristics
The final sample of 1,158 therapists included 477 OT and 681 PT, yielding a final response rate of 35.5%.
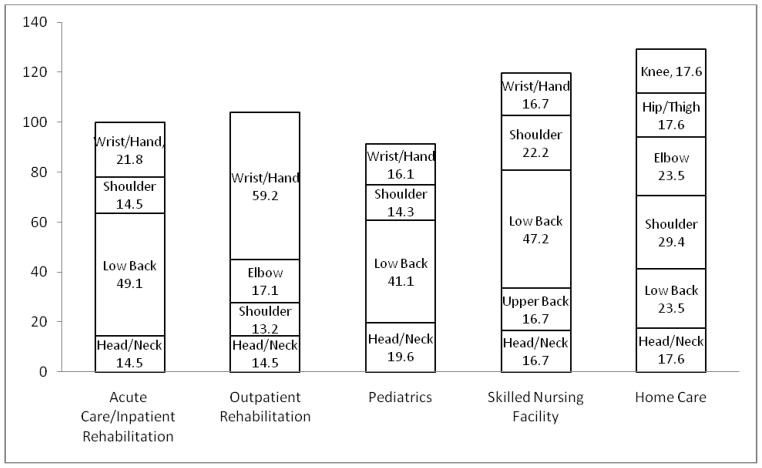
Therapists reported working in nine distinct practice areas [Fig. 1]. The proportions in each practice area changed slightly during each year, so for clarity, demographic information is presented for calendar year 2006 in Fig. 1 and Table 1. In 2006, about 93% were represented in five areas: outpatient rehabilitation, pediatrics, acute care/inpatient rehabilitation, skilled nursing facilities, and home care. Of note: in the present study, the majority of therapists selected both acute care and inpatient rehabilitation as their practice area, and these settings were combined into one category. The remaining worked in mental health, administration, industry, and academia. Participants in the five most represented areas varied on a number of factors (Table 1). Results of one-way ANOVA and post-hoc analyses revealed that therapists working in pediatrics and home care were older and had more years of experience than therapists working in acute care or outpatient rehabilitation. Therapists working in skilled nursing facilities were older than those working in outpatient rehabilitation, and therapists working in home care tended to have a higher body mass index (BMI) than those in outpatient rehabilitation and pediatrics. Finally, therapists working in acute care/inpatient rehabilitation spent more hours per day in direct patient care than those in skilled nursing facilities, pediatrics, and home care.
Fig. 1.
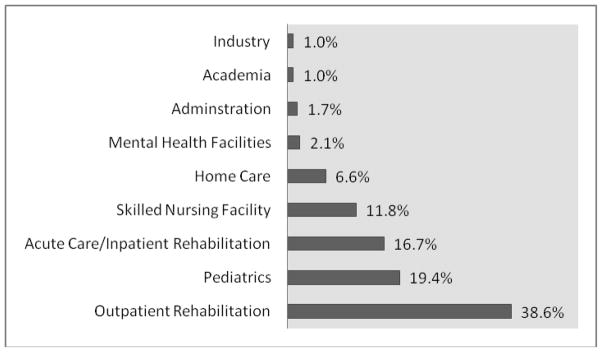
Distribution of OT and PT practice areas, 2006
Table 1.
Selected mean (SD) demographic and work characteristics of all therapists and therapists in five practice areas in 2006.
| Variable | All Areas (n =1158) | Outpatient Rehabilitation (n=444) | Pediatrics (n=223) | Acute Care (n=192) | Skilled Nursing Facility (n=136) | Home Care (n=76) | ANOVA F(10, 1158) |
|---|---|---|---|---|---|---|---|
| Age | 42.8 (9.81) | 40.5b,d,e (8.10) | 45.2a,b (9.81) | 41.1a,c (9.82) | 43.9e (10.19) | 45.9c,d (10.25) | 15.4** |
| BMI | 24.5 (4.36) | 24.2a (3.98) | 23.9b (3.91) | 24.7 (4.58) | 25.1 (5.07) | 25.8a,b (5.62) | 15.1** |
| Years of Experience | 17.7 (9.91) | 15.7b,d (9.16) | 20.3a,b (9.86) | 15.7a,c (9.34) | 18.3 (11.13) | 20.1c,d (9.64) | 3.4* |
| Hours worked weekly | 33.7 (11.60) | 35.0ab (11.04) | 33.1 (10.28) | 31.7a(11.50) | 34.9c (13.44) | 30.0b,c (9.24) | 5.5** |
| Hours patient care per day | 6.1 (2.29) | 6.8c,d,e (2.07) | 5.7a,c (2.30) | 6.5a,b (1.72) | 6.00d (1.97) | 5.3b,e (1.51) | 34.7** |
p≤0.05
p≤0.001
Note: Means in a row sharing subscripts are significantly different at p ≤ 0.05. Post-hoc analyses are the result of Tukey HSD
Injury prevalence was similar among the groups. Between 2004 and 2006, therapists reported 385 injuries, and provided detailed information on 248 (in response to a request to describe the injury that most affected their work). In 2006, 13.5% of therapists (all nine practice areas included) reported at least one injury (155/1151). Among pediatric therapists, 17.4% (39/223) reported at least one work-related injury in 2006, along with 15.7% of home care therapists (12/76), 15.1% of acute care/inpatient rehabilitation therapists (29/192), 12.2% of those in outpatient rehabilitation (54/444), and 11.0% of those in skilled nursing facilities (15/136).
3.2. Work activities associated with injuries, all practice areas
Injuries, body parts injured, and descriptions of treatment activity categories are detailed in Table 2. Manual therapy and transfers/lifts accounted for more than half of all injuries (54.0%), across all practice areas, with manual therapy associated with the greatest proportion of injury (27.4%) (Table 2). In addition to a description of the activity they were performing, the therapists provided their opinions on what aspects of the activity contributed to the injury. These aspects included force, awkward posture, repetitive motion, sustained posture, and fatigue.
Among therapists with injuries associated with manual therapy, the greatest proportion of injuries was to the wrist and hand (69.1%). Therapist-identified factors contributing to these injuries included repetitive motion (experienced during joint mobilizations and range of motion activities), force (experienced during range of motion, soft tissue work, and joint mobilizations), awkward posture and sustained posture. Repetitive motion was associated with 77.9% (53/68) of the manual therapy injuries. Force was associated with 47.1% (32/68), awkward posture with 42.6% (29/68), and sustained posture with 42.6% (29/68).
Transfer and lifting activities were associated with 26.6% of injuries (Table 2). Over half of these injuries were to the low back (53.0%), followed by the shoulder (19.7%) and the head/neck (18.2%). Therapists identified that these injuries occurred both gradually because of repeated performance of transfers over time and more suddenly when a patient behaved in an unexpected way (grabbed the therapist, stumbled, or moved in an unexpected direction). The majority of therapists identified force (72.7%; 48/66), including overexertion and lifting, and awkward posture (54.5%; 36/66) as the primary contributing factors to their transfer injuries.
Other activities associated with injury included environmental and equipment interactions (10.9%), multiple activities (6.5%) and patient falls (5.7%) (Table 2). Injuries attributed to environmental and equipment features typically affected the low back and shoulder (44.4%) and were associated with awkward postures (62.9%; 17/27) and force (51.9%; 14/27). Injuries attributed to multiple activities (6.5%) typically included the above three activities. Therapists commonly reported that transfers and manual therapy both contributed to their injury; they could not identify one or the other specifically. These injuries typically were associated with repetitive motion (63%, 10/16), sustained posture (50%; 8/16), force (43.8, 7/16), and awkward posture (44%; 7/16). Most injuries were to the low back (56.3%) and wrist/hand (37.5%). Patient falls were stated to result in an additional 5.7% of the injuries. Most patient falls injured the therapists’ low back (64.3%) and upper back (35.7%). Less frequently reported activities, such as patient falls, clerical, and functional activities, are described in Table 2.
3.3. Work activities associated with injury, practice area-specific
3.3.1. Outpatient Rehabilitation
Among therapists working in outpatient rehabilitation, manual therapy was overwhelmingly identified as the activity most often associated with injury [Table 3]. Manual therapy accounted for 71.1% of injuries to therapists in outpatient clinics, was overrepresented among therapists in outpatient settings (χ2=104.832; df = 1; p=<0.001), and outpatient therapists represented 89.4% (54/68) of all injuries attributed to manual therapy [Table 4].
Table 3.
Selected work-related activities associated with injury by practice area between 2004 and 2006.
| Activity | Outpatient % (n=76) | Pediatrics % (n=56) | Acute Care % (n=55) | Skilled Nursing % (n=36) | Home Care % (n=17) |
|---|---|---|---|---|---|
| Transfer/Lift | 2.6 (n=2) | 26.8 (n=15) | 52.7 (n=29) | 41.7 (n=15) | 29.4 (n=5) |
| Manual Therapy | 71.1 (n=54) | 10.7 (n= 6) | 7.3 (n=4) | 8.3 (n=3) | 0 |
| Environment/Equipment | 6.6 (n=5) | 12.5 (n=7) | 5.5 (n=3) | 16.7 (n=6) | 23.5 (n=4) |
| Functional Activities | 1.3 (n=1) | 3.6 (n=2) | 9.1 (n=5) | 2.8 (n=1) | 5.9 (n=1) |
| Patient Fall | 2.6 (n=2) | 5.4 (n=3) | 7.3 (n=4) | 13.9 (n=5) | 0 |
| Multiple Activities | 6.6 (n=5) | 14.3 (n= 8) | 3.6 (n=2) | 2.8 (n=1) | 0 |
| Floor Work | 0 | 8.9 (n=5) | 1.8 (n=1) | 2.8 (n=1) | 0 |
| Patient Aggression or Restraint | 0 | 7.1 (n=4) | 0 | 2.8 (n=1) | 0 |
| Therapeutic Exercise | 2.6 (n=2) | 0 | 3.6 (n=2) | 0 | 0 |
| Clerical | 1.3 (n=1) | 0 | 5.5 (n=3) | 2.8 (n=1) | 17.6 (n=3) |
| Motor Vehicle | 0 | 0 | 0 | 0 | 17.6 (n=3) |
| Other/Unknown | 5.6 (n=4) | 10.7 (n=6) | 3.6 (n=2) | 5.6 (n=2) | 5.9 (n=1) |
Table 4.
Work-related activities disproportionately represented among five primary practice areas, compared to all areas between 2004 and 2006.
| Setting -activity | Percent of cases | χ2 | p-value | |
|---|---|---|---|---|
| Selected Setting % (n) | All Settings % (n) | |||
| Outpatient | (n=76) | (n=172) | ||
| Manual Therapy | 71.1 (54/76) | 6.4 (14/172) | 104.83 | <0.001 |
| Pediatrics | (n=56) | (n=192) | ||
| Floor work | 8.9 (5/56) | 1.0 (2/192) | 9.83* | 0.007 |
| Multiple Activities | 14.3 (8/56) | 4.2 (8/192) | 7.36 | 0.012 |
| Patient Aggression | 7.1 (4/56) | 1.0 (2/192) | 6.84* | 0.025 |
| Acute/Inpatient | (n=55) | (n=193) | ||
| Transfer/Lift | 52.7 (29/55) | 19.2 (37/193) | 24.68 | <0.001 |
| Functional Activities | 9.1 (5/55) | 2.6 (5/188) | 4.67 | 0.046 |
| Skilled Nursing | (n=36) | (n=212) | ||
| Facility | 41.7 (15/36) | 24.1 (51/212) | 4.89 | 0.027 |
| Transfer/Lift | 13.9 (5/36) | 3.8 (9/212) | 5.37 | 0.037 |
| Patient Fall | ||||
| Home Care | (n=17) | (n=231) | ||
| Clerical | 17.6 (3/17) | 3.5 (8/231) | 7.52 | 0.031 |
Proportion comparison and p-values obtained through the Pearson chi-square test.
Fishers exact test was used for comparisons with expected cell values <5.
In therapists reporting injuries associated with manual therapy, most described injuries to the wrist and hand (59.2%) [Fig. 2].
Fig. 2.
Primary body parts injured (body part, %) among PT and OT in five primary practice areas between 2004 and 2006
*note: Figure 2 percentages do not sum to 100% because some therapists reported more than one body part injured
In most cases, the activity descriptions were general, “performing manual therapy”. Some specific examples that were identified were “deep tissue work”, “trigger point release”, and “joint mobilization”.
About seven percent of therapists reported that equipment and the environment contributed to their injuries. Two therapists experienced slips/trips: one over a cement block and one in the parking lot. Two others reported that their injuries were associated with lifting five and ten pound weights in and out of crates. A similar number attributed their injuries to multiple activities, including manual therapy and documentation; “performing manual therapy, performing documentation both computer and written”.
3.3.2. Pediatrics
Therapists working in pediatric settings experienced more variability in the types of factors associated with injury. Transfers and lifting were most commonly identified (26.8%), followed by multiple activities (14.3%), environmental and equipment factors (12.5%), manual therapy (10.7%), and floor work (8.9%) [Table 2]. Most pediatric therapists reported injuries to the low back (41.1%) and head/neck (19.6%) [Fig. 2].
In pediatrics, activities categorized as transfers/lifting were more commonly described as “lifting.” This physical therapist working in the school system reported that her low back injury occurred when lifting “a very large student after she collapsed to the floor.” Another physical therapist working in a pediatric outpatient facility reported “low back strain, “requiring time away from work, that occurred when she lifted “a young adult’s pelvis to shift it towards me.” Injuries associated with multiple activities were disproportionately represented in pediatric therapists (χ2=7.356; df=1; p = 0.012). They often included equipment/environmental factors and floor work, and were specific to working with children in a child-sized environment. One occupational therapist working in the school system ascribed her self-described “mid-back strain” to, “sitting on floor or in small (pre-k) sized chairs”. Another occupational therapist working in the school system attributed self-described “strain and disc injuries” in her low back, hip, thigh and lower leg to many different activities; “suspected on/off floor with students, lifting students from the floor, sitting in small student chairs, lifting/carrying heavy equipment.”
Equipment and environmental factors were distinct in pediatric settings. Three therapists described slips/trips. One physical therapist reported, “helping patient on playground equipment, movement awkwardly to assist and tripped backwards and fell.” Another occupational therapist reported, “tripped and fell on mat after exercising with a patient.” Equipment included sitting in child-sized chairs, playground equipment, and gym equipment such as bolsters, mats, and bolster swings. This occupational therapist working in the school system reported a “cartilage tear” in her shoulder when she had a “child on swing, had to stop abruptly.”
Floor work affected pediatric therapists to a greater extent than therapists in all other practice areas (χ2=9.832; df=1; p=0.007). One physical therapist working in an early intervention program (infants and children 0 – 3 years of age) reported that her neck and back WRI was due to “working with babies – sitting on the floor hunched over and then when working with 1 – 2 year olds with my arms raised above my shoulder height to hold child for balance.” Floor work injuries involved multiple body parts, including the neck, back, and knee. This physical therapist working in the school system reported “knee pain with squatting and floor play” and an occupational therapist also working in the schools identified “always on knees” as a risk factor for her “chronic bursitis”.
Pediatric therapists also were disproportionately affected by injuries associated with patient aggression or restraint when compared to all other practice settings (χ2=6.836; df=1; p= 0.025). Therapists were involved in restraining children or working with children who had behavioral disorders and experienced distinct injuries. One therapist was bitten on the hand when “restraining violent high school student with 3 other adults.” Another sustained a contusion to her head when “working with a student with a conduct disorder; became violent, punched, head butted me – he has a metal plate in his head secondary to head banging.”
Though manual therapy was the third most common injury, it was under-represented in pediatric therapists when compared to all other practice areas (χ2=10.143; df=1; p=0.002).
3.3.3. Acute Care/Inpatient Rehabilitation
Therapists in acute care/inpatient rehabilitation attributed the majority of their WRI to transfers and lifts (52.7%), followed by functional activities (9.1%), patient falls (7.3%) and manual therapy (7.3%) (Table 3). They were most likely to report injuries to the low back (49.1%) and wrist/hand (21.8%) [Fig. 2]. Therapists in acute care and inpatient rehabilitation accounted for 43.9% (29/66) of all transfer and lifting injuries reported and transfers/lift injuries were disproportionately represented among these therapists, compared to all others (χ2= 24.678; df=1; p = <0.001)(Table 4).
One physical therapist reported her low back injury resulted from transferring a patient into the bathtub. Another physical therapist reported that her WRI was a result of the physical demands of “transferring a heavy patient from sit to stand multiple times.” Transfer injuries also resulted from unexpected events during a transfer. In another case, a therapist reported “cervical radiculopathy” resulting from transferring a patient, when the patient “grabbed my neck and pulled.” Lifting was coded along with transfers, and lifting activities included lifting patients during transfers, from the floor, and from furniture (beds, commodes). One occupational therapist was injured while assisting nursing staff during an emergency; “called into patient’s room by nursing staff to assist with lifting patient off commode after he became unresponsive.. had to lift up and over to the bed.”
Acute care therapists also identified functional activities, such as gait training and ADL training, as associated with injury (9.1%). Functional activities, included ADL training and gait training, were disproportionately represented in this group (χ2=4.674; df = 1; p=0.046). One OT reported that her injury resulted from “leaning to the right and bending forward to wash [patient’s] back.” Another OT was injured while ambulating with a “patient up steps for a home eval: patient impulsive, increased speed of ambulation, loss of balance to right, therapist tensed up when holding gait belt …”
Patient falls resulted in 7.3% of all injuries. In two of the cases, the therapists sustained low back WRI while lowering the patient to the floor during the fall. Another therapist sustained a “torn flexor tendon” in her finger when it got caught in a gait belt as the patient fell during a transfer.
Manual therapy also was identified in 7.3% of injuries in acute care settings. Though not typically explained in detail, two therapists reported that sustained stretch and holding of patient extremities contributed to the development of “carpal tunnel syndrome, radial impingement, and adhesive capsulitis.”
3.3.4. Skilled Nursing Facilities
Like therapists working in acute care, most WRI in skilled nursing facilities were attributed to transfers and lifts (41.7%), and these were overrepresented among these therapists (χ2=4.886; df=1; p=0.027) [Table 4]. Most therapists in skilled nursing facilities characterized their WRI as strains and sprains, and most reported injuries to the low back (47.2%) and shoulder (22.2%) [Fig. 2]. Transfer/lift injuries were described in less detail than the acute care therapists, though patient weight was identified specifically in the activity descriptions. Two therapists specified that their low back and hip injuries occurred transferring an obese patient and another reported that there is “not enough help for the larger, bariatric population (equipment)”.
An important distinction is that patient falls accounted for disproportionately more injuries than those working in other settings (χ2=5.373; df=1; p=0.037). Weight was a contributing factor when a certified nursing assistant (CNA) and PT attempted to prevent a fall in a 375 lb patient who could not rise from a squat, resulting in a “low back strain” to the PT (CNA injury status unknown). In two other instances, as with acute care, therapists stated they were lowering the patient to the floor during a fall and this resulted in their WRI.
Equipment and environment accounted for 16.7% of WRI. Three therapists reported lifting equipment was associated with WRI to the back, shoulder, and knees. In another instance, the therapist was removing a sling from under a patient. The therapist sustained a low back injury when the sling became caught on the wheelchair while she was removing it.
3.3.5. Home Care
Home care therapists include therapists who worked both in group homes and individual’s homes. Most home care therapists reported strain/sprain injuries and injuries to the shoulder (29.4%), low back (23.5%), and elbow/forearm (23.5%). Most home care therapists reported that transfers and lifts (29.4%) and environment/equipment (23.5%) were associated with their WRI. As with therapists working in skilled nursing facilities, two therapists specifically identified patient weight as a contributing factor in their injury. Another was injured lifting a wheelchair over steps.
All injuries associated with equipment were described as carrying home care bag and laptop between the car and the patient’s home; two resulted in injuries to the low back, one to the hip/thigh, and one to the elbow. They experienced disproportionately more injuries associated with clerical duties, and all were associated with documentation using laptops (χ2=7.516; df=1; p=0.031).
Therapists working in home care were the only participants to report sustaining their injuries because of driving. Three therapists reported injuries associated with driving: two were involved in motor vehicle crashes and one developed tendonitis from “driving car 200+ miles daily.”
4. Discussion
The purpose of the present paper was to identify activities associated with injury in physical and occupational therapists, and to evaluate differences in activities associated with injury between five major practice areas.
4.1. Activities Associated with Injury
The results of this study support findings of prior research that identifies manual therapy and transfers/lifts as the activities most commonly associated with injury in OTs and PTs [3,5,14,24,25]. Interestingly, this body of research varies considerably in the way work-related discomfort or injury is defined. For example, Holder et al. [14] asked therapists to report work-related injury (as in the current study), Campo et al. [3] measured pain severity, duration and frequency and applied a case definition to identify work-related musculoskeletal disorders, and Snodgrass et al.[25] assessed pain using a 100 mm visual analogue scale and disability using the Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH). However, regardless of the outcome, pain, gradual onset of WMSDs, or acute WRI, transfers/lifts and manual therapy remain the primary activities identified by therapists as associated with their musculoskeletal symptoms or injury. Transfer/lifts and/or manual therapy were also the most commonly reported activities among therapists working in all five of the primary practice settings.
Transfers and lifts are activities also commonly associated with injuries in nurses and nursing personnel [11,29], and biomechanical evidence reveals that manual handling of even lightweight, compliant patients can exceed tissue tolerances in the lumbar spine [19]. There is now substantial evidence that patient handling increases the risk for injuries in both PTs and OTs, and that this is consistent across four of the five major practice settings identified in this study. Intervention programs designed specifically to address moving and handling patients safely have effectively reduced injury rates associated with patient handling among nursing personnel [4,17,21,22, 23, 26], but may be met with resistance by therapists [6]. In the aforementioned study, therapists working in a minimal lift environment expressed concerns regarding the effect of mechanical lift devices on patient outcomes and recovery. However, these therapists were also able to articulate specific uses of the equipment in the context of therapy, including standing tolerance, endurance training, and trunk control, and specific patient populations for whom it was useful, including low level and bariatric patients [6]. It is likely that therapists will need to embrace safe patient handling and movement (SPHM) programs, but a cultural shift may be needed before these programs can be implemented on a national basis. Evidence that these programs do not impede patient rehabilitation also will need to be conducted, and equipment will need further assessment for therapeutic use.
Manual therapy has also been identified as a consistent risk factor for both injuries as well as gradual onset of WSMDs [3, 5]. This was supported in the current study. Unlike patient handling where active efforts are underway to reduce related injuries, manual therapy has received very little attention as a substantial risk factor requiring injury prevention measures. Manual therapy should be considered, along with patient lifting as one of the most substantial risk factors for injury and methods and devices to improve manual therapy safety should be developed and tested. Hand held tools, such as thumb splints, mobilization wedges, and devices to aid soft tissue mobilization, are available but their efficacy in injury prevention is not known [3,10]. Other recommendations include adjustable tables, dynamic standing, anti-fatigue mats, and carts to transport equipment such as ultrasound devices [10].
4.2. Other Activities Associated with Injury in Specific Settings
Although transfers/lifts and manual therapy accounted for most injuries, analysis of injury data by practice area revealed several other factors that deserve closer attention. Each practice area had unique activities that therapists identified as associated with their injuries. Functional activities, such as gait training and ADL training, are common activities performed by therapists, and were a particular challenge for therapists working in acute care/inpatient rehabilitation. These activities are influenced by environmental as well as patient factors. Therapists often perform these tasks in awkward spaces, with complex and debilitated patients who may behave unpredictably [6]. Patient falls were of particular concern for those therapists in skilled nursing facilities, perhaps due to the frailty and medical complexity of the patients. It is possible that mechanical lift devices and other equipment associated with safe patient handling could be useful injury prevention strategies, given adequate space [6]. Pediatric therapists were vulnerable to environmental factors (such as working in a setting designed for children), person factors (working with small children and infants), and task factors (pediatric intervention that necessitates working while seated or kneeling on the floor). Pediatric therapists were also more likely to sustain an injury due to aggression. Home care therapists identified environmental and equipment-related activities, and also were more vulnerable to injuries related to documentation. They also were vulnerable to injuries related to driving. Like pediatric therapists, they work in less controlled environments, such as homes and schools, transport equipment between sites, and make use of equipment in these settings (home appliances, playground elements) to provide and document services. The nature of a poorly controlled and unpredictable environment makes prevention efforts more challenging than those in more medical environments. Such interventions must be highly individualized and specific activities targeted. In addition, efforts must be coordinated between therapists, administrators, and policy makers to ensure an integrated effort. This is an important area of research.
4.3. Study limitations
This study had several important limitations. Most notably, the response rate was only 36%. This leaves the study open to response bias, and possible inflation of injury prevalence. This limits external validity; however, the results are similar to other research [3]. Additionally, this study relied on self-report, which introduces substantial recall bias. [27]. Study participants described injuries, diagnoses, factors associated with injury, and activities associated with injury without the provision of medical confirmation, injury reports, or observations of activities. Since this was an anonymous survey, researchers had no way to follow up with participants for further detail or clarification. Self-report relies on the participant’s knowledge of the injury or perception of the factors associated with the injury. This information is useful, but needs to be further assessed. Future studies, including observational and quantitative assessments of such factors as awkward posture, repetitive motion, and force, are critical for the confirmation of these findings. Finally, many therapists change jobs and practice areas during their careers. Participants in this study were categorized according to the practice area they were working in when injured. However, if injuries can be attributed to cumulative effects over time, the causes of injury may be far more complex than this study implies.
4.4. Implications for future research
The effect of safe patient handling and movement (SPHM) zero-lift and minimal-lift programs on therapist and patient outcomes must be evaluated. To date, studies have shown that multifactor interventions using mechanical lift devices can reduce work-related pain and injury in nursing personnel [8,13,18]. However, no studies to date have examined the effects of using such equipment in a rehabilitation environment. Therapists are working with minimal lift and no-lift policies, and are using equipment in the context of therapeutic intervention, but the way in which they use the equipment could place them at risk. For example, therapists have reported pushing and pulling floor-based patient lifts and stand assist devices while facilitating patient activity [6]. Recent research demonstrates that moving a floor lift in this way can result in anterior/posterior shear forces in the lumbar spine that exceed acceptable levels [20]. Assessment of specific patient handling technologies (e.g. stand assist and ceiling lift) for use in therapy and for use in the facilitation of mobility and normal movement patterns is also critical. More specific observation of certain therapeutic activities, such as functional activity training, pediatric intervention and manual therapy, is crucial for the development of prevention strategies. Manual therapy is a primary activity associated with injury and pain, and yet little is known about how to make changes to reduce the risks associated with its performance.
4.5. Conclusion
In general, a significant portion of injuries experienced by PT and OT might be prevented through the use of safe patient handling and movement prevention programs, though the manner in which therapists use the equipment may impact its ability to protect them. However, given the practice setting-specific activities associated with injury, interventions must be designed based on the patient population and setting in order to most effectively address work-related risks.
Acknowledgments
This study was supported, in part, by a University of Wisconsin-Milwaukee, College of Health Sciences “Stimulus for Extramural Enhancement & Development” grant. Assistance with regulatory compliance was supported by award number UL1RR025755 from the National Center for Research Resources, funded by the Office of the Director, National Institutes of Health (OD) and supported by the NIH Roadmap for Medical Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Contributor Information
Amy R Darragh, School of Allied Medical Professions, The Ohio State University, 453 West 10th Avenue, 406 Atwell Hall, Columbus, OH 43210, 614 292 0370 (phone), 614 292 0210 (fax).
Marc Campo, School of Natural and Health Sciences, Mercy College, Dobbs Ferry, NY.
Phyllis King, Department of Occupational Therapy, College of Health Sciences, University of Wisconsin-Milwaukee, Milwaukee, WI.
References
- 1.Bork BE, Cook TM, Rosencrance JC, Englehardt KA, Thomason ME, Wuford IJ, Worley RK. Work-related musculoskeletal disorders among physical therapists. Phys Ther. 1996;76:827–835. doi: 10.1093/ptj/76.8.827. [DOI] [PubMed] [Google Scholar]
- 2.Bureau of Labor Statistics. 2004 Retrieved October 1, 2006 from: www.bls.gov.
- 3.Campo M, Weiser S, Koenig KL, Nordin M. Work-related musculoskeletal disorders in physical therapists: A prospective cohort study with 1 year follow-up. Phys Ther. 2008;88:608–619. doi: 10.2522/ptj.20070127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charney W, Simmons B, Lary M, Metz S. Zero lift programs in small rural hospitals in Washington state: reducing back injuries among health care workers. AAOHN J. 2006;54:355–358. doi: 10.1177/216507990605400803. [DOI] [PubMed] [Google Scholar]
- 5.Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders in physical therapists: Prevalence, severity, risks, and responses. Phys Ther. 2000;80:336–351. doi: 10.1093/ptj/80.4.336. [DOI] [PubMed] [Google Scholar]
- 6.Darragh AR, Campo M, Olson D. Therapy practice within a minimal lift environment: Perceptions of therapy staff. Work. 2009;33:241–253. doi: 10.3233/WOR-2009-0872. [DOI] [PubMed] [Google Scholar]
- 7.Darragh AR, Huddleston W, King P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. Am J Occup Ther. 2009;63:351–362. doi: 10.5014/ajot.63.3.351. [DOI] [PubMed] [Google Scholar]
- 8.Engkvist I. Evaluation of an intervention comprising a No Lifting Policy in Australian hospitals. Appl Ergon. 2006;37:141–148. doi: 10.1016/j.apergo.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Greene L, Goggins RW. Save Your Hands: The Complete Guide to Injury Prevention and Ergonomics for Manual Therapists. Body of Work Books; Coconut Creek, FL: 2008. pp. 45–73. [Google Scholar]
- 10.Glover W, McGregor A, Sullivan C, Hague J. Work-related musculoskeletal disorders affecting members of the chartered society of physiotherapy. Physiotherapy. 2005;91:138–147. [Google Scholar]
- 11.Hignett S. Work-related back pain in nurses. J Adv Nurs. 1996;23:1238–1246. doi: 10.1046/j.1365-2648.1996.13423.x. [DOI] [PubMed] [Google Scholar]
- 12.Hignett S. Manual handling risk assessments in occupational therapy. Brit J Occup Ther. 2001;64:81–86. [Google Scholar]
- 13.Hignett S, Crumpton E, Ruszala S, Alexander P, Fray M, Fletcher B. Evidence-based patient handling: A systematic review. Nurs Stand. 2003;17:33–36. doi: 10.7748/ns2003.04.17.33.33.c3383. [DOI] [PubMed] [Google Scholar]
- 14.Holder NL, Clark HA, DiBlasio JM, Hughes CL, Schepf JW, Harding L, Shepard KF. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists physical therapy assistants. Phys Ther. 1999;79:642–652. doi: 10.1093/ptj/79.7.642. [DOI] [PubMed] [Google Scholar]
- 15.Hunting KL, Welch LS, Nessel-Stephens L, Anderson J, Mawudeku A. Surveillance of construction worker injuries: The utility of trade specific analysis. Appl Occup Env Hyg. 1999;14:458–469. [PubMed] [Google Scholar]
- 16.King P, Huddleston W, Darragh AR. Work-related musculoskeletal disorders and injuries: Differences in older and younger occupational and physical therapists. J Occup Rehabil. 2009;19:274–283. doi: 10.1007/s10926-009-9184-1. [DOI] [PubMed] [Google Scholar]
- 17.Kutash M, Short M, Shea J, Martinez M. The lift team’s importance to a successful safe patient handling program. J Nurs Adm. 2009;39:170–175. doi: 10.1097/NNA.0b013e31819c9cfd. [DOI] [PubMed] [Google Scholar]
- 18.Li J, Wolf L, Evanoff B. Use of mechanical patient lifts decreased musculoskeletal symptoms and injuries among health care workers. Inj Prev. 2004;10:212–216. doi: 10.1136/ip.2003.004978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marras WS, Davis KG, Kirking BC, Bertsche PK. A comprehensive analysis of low-back disorder risk and spinal loading during the transferring and repositioning of patients using different techniques. Ergonomics. 1999;42:904–926. doi: 10.1080/001401399185207. [DOI] [PubMed] [Google Scholar]
- 20.Marras WS, Knapik GG, Ferguson S. Lumbar spine forces during maneuvering of ceiling-based and floor-cased patient transfer devices. Ergonomics. 2009;52:384–397. doi: 10.1080/00140130802376075. [DOI] [PubMed] [Google Scholar]
- 21.Miller A, Engst C, Tate RB, Yassi A. Evaluation of the effectiveness of portable ceiling lifts in a new long-term care facility. Appl Ergon. 2006;37:377–385. doi: 10.1016/j.apergo.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 22.Nelson A, Fragala G. Equipment for safe patient handling and movement. In: Charney W, Hudson A, editors. Back injury among health care workers: Causes, solutions, and impacts. Boca Raton, FL: Lewis Publishers; 2004. pp. 121–135. [Google Scholar]
- 23.Nelson A, Matz M, Chen F, Siddharthan K, Lloyd J, Fragala G. Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Int J Nurs Stud. 2006;43:717–733. doi: 10.1016/j.ijnurstu.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Power H, Flemming H. Work-related thumb pain in manipulative physiotherapists – an Irish survey. Physiother Ireland. 2007;28:51–57. [Google Scholar]
- 25.Snodgrass SJ, Rivett DA, Chiarelli P, Bates AM, Rowe LJ. Factors related to thumb pain in physiotherapists. Aust J Physiother. 2003;49:243–250. doi: 10.1016/s0004-9514(14)60140-9. [DOI] [PubMed] [Google Scholar]
- 26.Stenger K, Montgomery LA, Briesemeister E. Creating a culture of change through implementation of a safe patient handling program. Crit Care Nurs Clin North Am. 2007;19:213–222. doi: 10.1016/j.ccell.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Szklo M, Nieto FJ. Epidemiology: Beyond the Basics. Gaithersburg, MD: Aspen Publishers; 2000. pp. 125–176. [Google Scholar]
- 28.Wajon A, Ada L. Prevalence of pain in physical therapists practicing spinal manipulative therapy. J Hand Ther. 2003;16(2003):237–244. doi: 10.1016/s0894-1130(03)00039-5. [DOI] [PubMed] [Google Scholar]
- 29.West DJ, Gardner D. Occupational injuries of physiotherapists in North and Central Queensland. Aust J Physiother. 2001;47:179–186. doi: 10.1016/s0004-9514(14)60265-8. [DOI] [PubMed] [Google Scholar]
- 30.Yassi A, Khokher AJ, Tate R, Cooper JE, Snow C, Vallentyne S. The epidemiology of back injuries at a large Canadian tertiary care hospital: implications for prevention. Occ Med. 1995;45:215–220. doi: 10.1093/occmed/45.4.215. [DOI] [PubMed] [Google Scholar]