Abstract
Purpose
Increased intima-media thickness (IMT) is an early marker of atherosclerotic disease and several prospective studies have demonstrated that IMT is a strong predictor of cerebrovascular complications. In this paper we propose a novel method to assess IMT, called “intima media thickness variability” (IMTV) and evaluate its relationship with the development of cerebrovascular events.
Material and Methods
The study was approved by the local IRB. Twenty consecutive patients underwent ultrasound analysis of the carotid arteries (mean age 68 years; age range 59-81 years). The IMT and IMTV of the 40 carotid vessels was assessed. Bland–Altman statistics were employed to measure the inter-observer variability, and ROC analysis was used to assess the association with cerebrovascular events.
Results
In all cases the ROC area under the curve was higher for IMTV than IMT. There was a statistical significant association between IMTV and cerebrovascular events (P=0.018), but no relationship between IMT and events. The results for inter-observer variability showed a systematic error between 0.04 and 0.08 mm. In the Person Rho correlation analysis in no case a statistical association between IMT and symptoms was detected whereas in 2 cases (observer 1 and observer 2), a statistically significant association between IMTV and symptoms was found.
Conclusions
Data of this preliminary study suggest that IMTV may represent a powerful method to assess carotid atherosclerotic disease with a significant association to cerebrovascular events.
Key Words: Increased intima-media thickness, intima media thickness variability, carotid atherosclerotic disease, cerebrovascular events
Introduction
Atherosclerosis of the carotid artery represents one the major causes cerebrovascular disease in developed countries. The identification of a reliable marker of increased atherosclerotic risk would allow to initiate specific therapeutical interventions reduce the risk of future cerebrovascular events (1).
Increased carotid artery wall thickness is an established marker of early stages in the atherosclerotic process and is associated with the development of future cerebrovascular events (2-4). Iit has been suggested that an increased Intima-Media-Thickness (IMT) can be considered as a measure of atherosclerosis in general (5,6).
High resolution B-mode ultrasound of the carotid arteries allows the identification of the distinct layers in the arterial wall. Typically, longitudinal images of the arterial wall show two parallel echogenic lines separated by a relatively hypoechoic central region referred to as the Intima-Media layer (7). The distance between these two lines is the IMT. However, measurement of the IMT, suffers several limitations. In particular relatively poor inter-observer and intra-observer agreement that can be ascribed to several parameters including the sonographer experience and type of sonographic equipment used for the analysis (8-10).
In this study we propose a new technique for the analysis of the carotid artery wall, called Intima-Media-Thickness Variability (IMTV), which is based on the variance of the standard deviation of the IMT.
Material and Methods
Patient population
Twenty consecutive patients (13 males, 7 females; mean age 65 years; range 59-79 years) who were examined with carotid ultrasound between October and December 2010, were prospectively included in this study. The study was conducted in accordance with the guidelines of our Institution's research committee.
Classification of cerebrovascular symptoms
We classified patients as symptomatic or asymptomatic based on the history of cerebrovascular events in the 6 months prior to the ultrasound examination, as documented in the clinical chart. A patient was considered as symptomatic when a transitory ischemic attack (TIA) or stroke occurred. TIA was considered as an episode of neurological dysfunction (hemiparesis, hemiparesthesia, dysarthria, dysphasia or monocular blindness), not exceeding 24 hours. If the episode of neurological dysfunction exceeded 24 hours it was considered as a stroke. Patient with events >6 months prior to the ultrasound examination were included in the asymptomatic group. In our Institution carotid ultrasound is routinely performed in asymptomatic patients undergoing cardiac interventions for coronary artery disease, aortic interventions, lower leg artery surgery and in diabetics who were >50 years old.
CD-US technique
Colour duplex ultrasound scanning was performed with a US machine (MyLab™ 70, Esaote, Genova, Italy) with a 10 MHz linear-array transducer. The bilateral carotid arteries were scanned, and the images stored on video tape. The sonographer adjusted optimal gain settings according to their experience. The subject's head was tilted to obtain images of the CCA just proximal to the bulb placed horizontally across the screen.
Measure of IMT
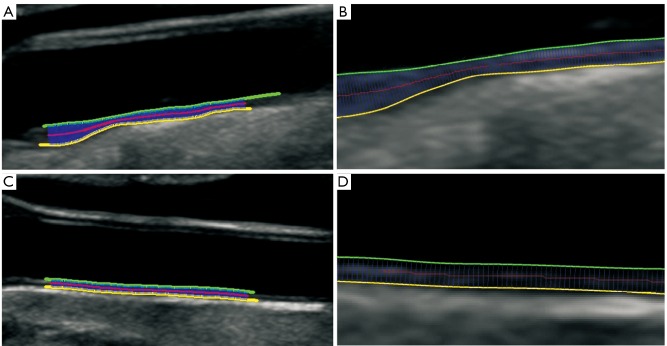
Three observers with 10 years, 4 years and 3 years experience in vascular imaging measured the IMT by using dedicated software (ImgTracer™, Biomedical Technologies, Inc., Denver, CO) that has the ability to compute the IMT (Figure 1). The distance computation method as first described by Suri et al. (11) was used. This algorithm has been standardized in vascular IMT measurement and has been well adapted by several groups around the world (12,13).
Figure 1.
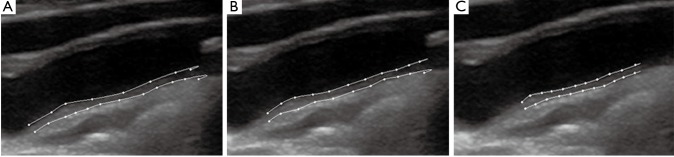
IMT analysis for Observer A, B and C
IMTV measurement
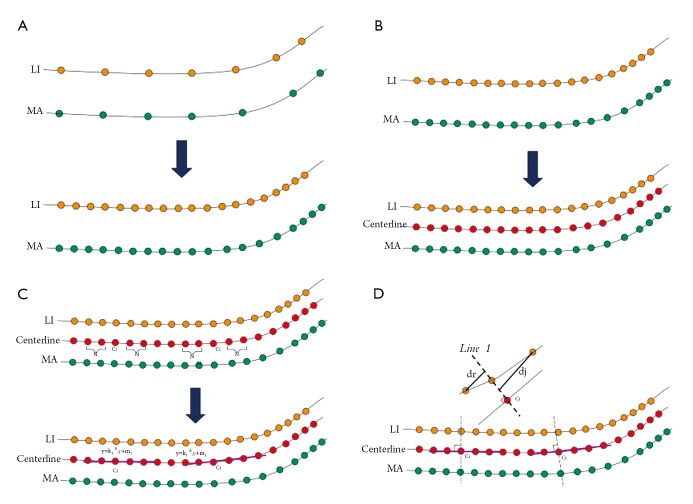
The IMTV is computed by finding the variability of the lumen-intima (LI) and media-adventita (MA) borders along the carotid artery. The algorithm consists of the following stages: (I) interpolating the LI and MA borders to a fixed number of points; (II) finding the centreline points between the LI and MA borders along the carotid artery; (III) finding the chords and their lengths, which are perpendicular to the LI and MA segments passing through the centreline points; (IV) estimating the mean and standard deviations of the chord lengths corresponding to each centreline points along the carotid artery; and (V) IMTV is defined as the standard deviation of the far carotid LI and MA walls. Figure 2 summarizes the computation steps. Examples showing the chords along the carotid artery are shown in Figure 3.
Figure 2.
A. Interpolation of the LIMA boundaries to the standard value of 100 points; B. Centerline (red) is computed as the average distance between LI and MA; C. 2N+1 points along the centerline are used to fit a line; D. The perpendicular to the fitted line is computed (upper figure) and the LIMA points of intersection from this perpendicular are used to compute IMT (bottom figure). LI=lumen-intima; MA=media-adventitia
Figure 3.
A. Figure showing the LI and MA borders along with the red centerline with corresponding chords perpendicular to LI and MA borders; B. Zoomed version showing the chords perpendicular to the red centerline of the LI and MA borders; C. Figure showing the LI and MA borders along with the red centerline with corresponding chords perpendicular to LI and MA borders; D. Zoomed version showing the chords perpendicular to the red centerline of the LI and MA borders
Statistical analysis
Kolmogorov-Smirnov Z test for the distribution the normality of each continuous variable group was calculated. Continuous data were described as the mean value ± standard deviation (SD). Inter-observers agreement was evaluated by using the Bland–Altman analysis (14). Receiver Operating Characteristics (ROC) curve analysis was performed in order to evaluate the association between cerebrovascular symptoms, IMT and IMTV and the area under the ROC (Az) was calculated [Az values between 0.5 (no significant) to 1 (perfect association)]. The correlation coefficients are also provided. A P value less than 0.05 were considered significant. R software (www.r-project.org) was employed for statistical analyses.
Results
No exams were excluded for poor quality. We observed 9 subjects with ischemic symptoms (2 strokes, 6 transitory ischemic attacks, 1 amaurosis fugax). We considered the symptomatic artery as the artery ipsilateral to the neurological symptoms. Therefore we included 9 symptomatic arteries and 31 asymptomatic arteries. The IMT and IMTV values are summarized in Table 1.
Table 1. Summary table.
| Mean | 95% CI | Variance | SD | RSD | Median | 95% CI | Minimum | Maximum | 2.5-97.5 P | Normal Distr. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| IMT Observer 1 | 1.386 | 1.224-1.548 | 0.2705 | 0.5201 | 0.3752 | 1.35 | 1.050-1.515 | 0.662 | 2.638 | 0.691-2.524 | 0.155 |
| IMT Observer 2 | 1.427 | 1.253-1.602 | 0.3131 | 0.5596 | 0.3921 | 1.351 | 1.133-1.581 | 0.612 | 3.161 | 0.673-3.024 | 0.003 |
| IMT Observer 3 | 1.389 | 1.215-1.563 | 0.313 | 0.5595 | 0.4028 | 1.237 | 1.091-1.494 | 0.703 | 3.086 | 0.714-3.026 | 0.001 |
| IMTV Observer 1 | 0.192 | 0.153-0.231 | 0.0159 | 0.126 | 0.6558 | 0.148 | 0.121-0.231 | 0.05 | 0.558 | 0.051-0.545 | 0.003 |
| IMTV Observer 2 | 0.146 | 0.117-0.176 | 0.0089 | 0.0945 | 0.6457 | 0.14 | 0.082-0.172 | 0.028 | 0.395 | 0.030-0.387 | 0.037 |
| IMTV Observer 3 | 0.109 | 0.083-0.136 | 0.0072 | 0.0848 | 0.7751 | 0.079 | 0.058-0.124 | 0.023 | 0.406 | 0.026-0.359 | 0.001 |
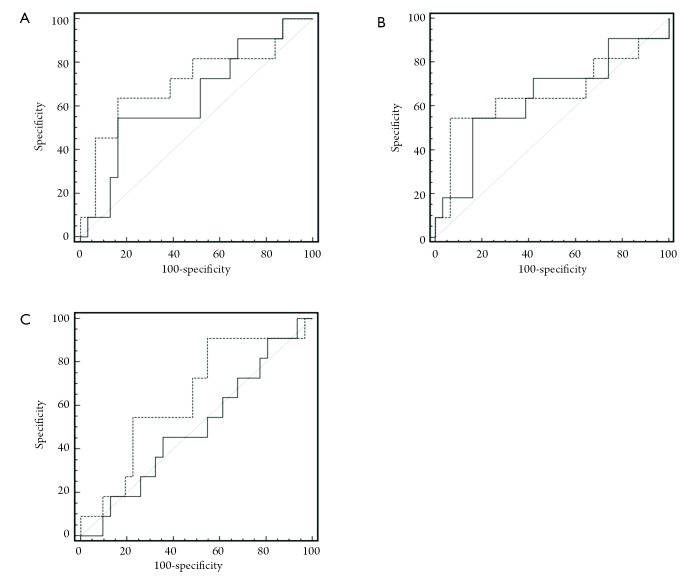
ROC curve analysis
The ROC curve analysis is summarized in Table 2 and the graphs are shown in Figure 4. In all cases the Az of IMTV was higher of the Az of IMT. In no case a statistical significant association was detected by IMT and cerebrovascular symptoms whereas with the IMTV a statistically significant association was detected (P=0.018) for observer 1.
Table 2. ROC curve analysis statistic.
| AUC | SE | 95% CI | P value | |
|---|---|---|---|---|
| IMT Observer 1 | 0.636 | 0.102 | 0.474 to 0.779 | 0.178 |
| IMTV Observer 1 | 0.713 | 0.097 | 0.552 to 0.841 | 0.018 |
| IMT Observer 2 | 0.639 | 0.102 | 0.477 to 0.781 | 0.173 |
| IMTV Observer 2 | 0.657 | 0.101 | 0.495 to 0.796 | 0.082 |
| IMT Observer 3 | 0.501 | 0.103 | 0.341 to 0.657 | 0.932 |
| IMTV Observer 3 | 0.636 | 0.102 | 0.474 to 0.779 | 0.177 |
Figure 4.
An A,B,C. ROC curve analysis for Observer 1, 2 and 3. The dashed line represent IMTV whereas the normal lien represent the IMT
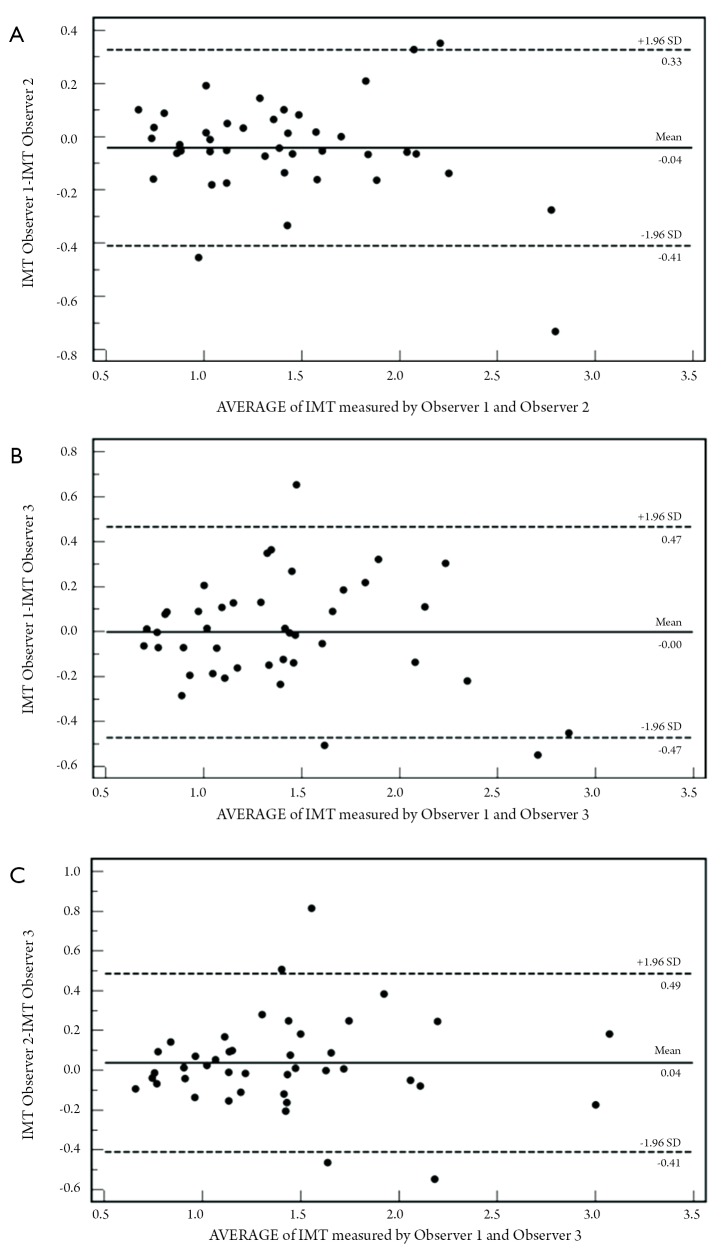
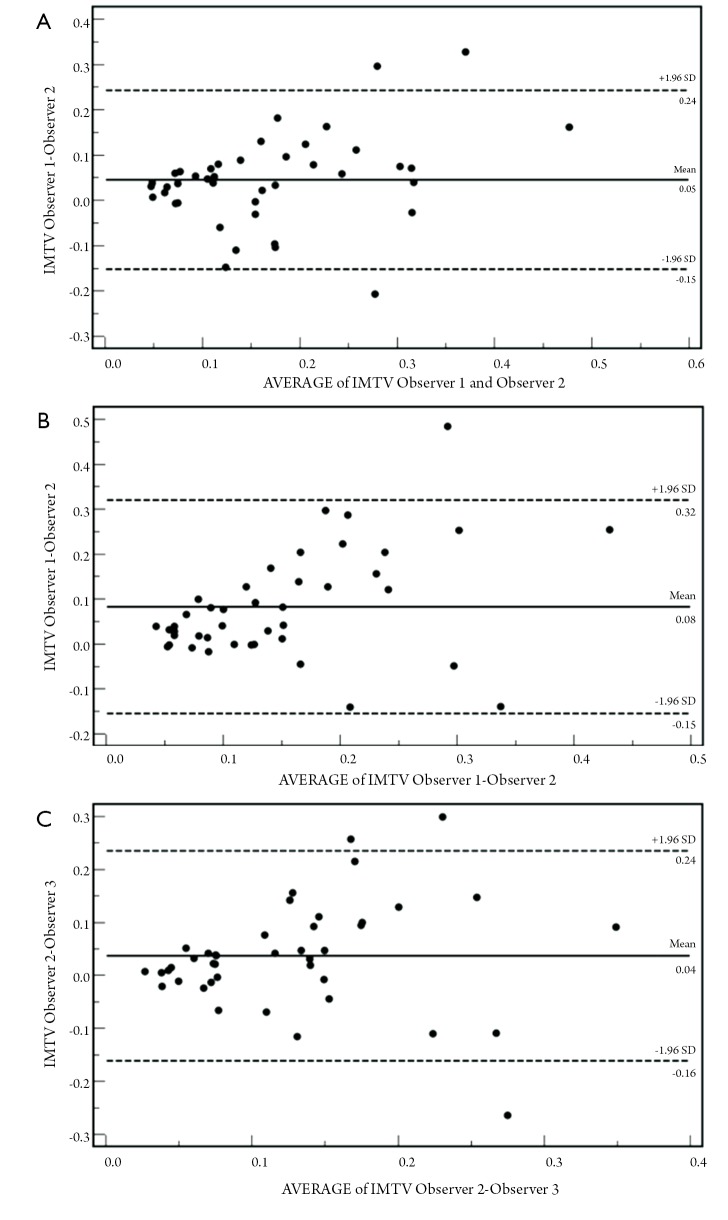
Bland-Altman analysis
The Bland Altman plot for IMT and IMTV are shown in Figures 5,6. The results for the IMTV were very good with a systematic error between 0.04 and 0.08 mm.
Figure 5.
A. Bland-Altman analysis for IMT between observer 1 and 2; B. observer 1 and 2; C. observer 2 and 3
Figure 6.
A. Bland-Altman analysis for IMTV between observer 1 and 2; B. Observer 1 and 2; C. Observer 2 and 3
Pearson Rho correlation
The Correlation results analysis is summarized in the Table 3. In no case a statistical association between IMT and symptoms was detected whereas in 2 cases (observer 1 and observer 2) a statistical significant correlation was observed.
Table 3. Correlation analysis summary statistics.
| IMT Analysis | IMT Observer 1 | IMT Observer 2 | IMT Observer 3 |
|---|---|---|---|
| Correlation coefficient r | 0.2499 | 0.1993 | 0.0255 |
| Significance level | P=0.1105 | P=0.2058 | P=0.8726 |
| 95% Confidence interval for r | -0.0585 to 0.5147 | -0.1114 to 0.4745 | -0.3269 to 0.2806 |
| IMTV Analysis | IMTV Observer 1 | IMTV Observer 2 | IMTV Observer 3 |
| Correlation coefficient r | 0.3399 | 0.292 | 0.1757 |
| Significance level | P=0.0277 | P=0.031 | P=0.2657 |
| 95% Confidence interval for r | 0.0401 to 0.5835 | -0.0131 to 0.5474 | -0.1355 to 0.4553 |
Discussion
The purpose of this study was to analyze a novel method to assess carotid atherosclerosis, based on the difference in the variability of the IMT. Increased carotid artery wall thickness is an established earlier marker of the atherosclerotic process and is associated with the development of cerebrovascular events (2-4). IMT has been suggested as a measure of atherosclerosis in general (5,6).
The standard IMT measure is based on the distance between Intima-Media (7). However this measurement suffers from low reproducibility that is only partially solved by the development of automated measurement tools.
Our data explores the hypothesis that the variance of the standard deviation of the IMT (IMTV) represent a better predictor of the atherosclerosis compared to IMT. The basic concept of IMTV is to explore the variation of the IMT along the length of the examined carotid wall segment. It is logical that a carotid artery wall with a completely smooth surface will show a very low variance of standard deviation because the IMT lines are parrallel, whereas a carotid artery wall with an irregular profile will show a significant variation of the IMT standard deviation.
The results of this preliminary study indicate that the IMTV is associated with the presence of cerebrovascular events. Both the ROC curve analysis and correlation analysis showed the presence of a statistically significant association between the IMTV and cerebrovascular symptoms for Observer 1 and Observer 2. In contrast, the IMTV of observer 3 did not showed a statistically significant association in Az and Pearson Rho analysis, which may be explained by the fact that observer 3 had only 2 years of experience in vascular imaging study and his ability in define the IMT lumen-intima and media-adventitia layers were sub-optimal. This variability could be solved in the future with the development of software to automated analysis of IMTV.
There was no statistically significant association between IMT and cerebrovascular symptoms in the correlation analysis (P value=0.1105, 0.2058, 0.8726 for Observer 1, 2 and 3 respectively). This result is concordant with previous works that suggest that IMT is a poor marker for the identification of patients with a risk of cerebrovascular events.
This study has several limitations. First of all, a statistical bias can be ascribed because of the small number of carotid arteries examined (n=40). Therefore, our results should be considered as preliminary and future studies with larger patient cohort will be useful to reduce statistical bias. Second the prevalence of patients with cerebrovascular symptoms is high (45%), more that the common general population. It is important to test this parameter in cohort of patient with a lower prevalence similarly to the general population.
In conclusion, the data of this preliminary study suggest that IMTV may represent a powerful method to study carotid atherosclerosis, and that this parameter has a statistically significant association with cerebrovascular events. In the future it will be important to test IMTV performance in larger population and to analyze its association with the classic cardiovascular risk factors like smoking, diabetes, hypertension, and dyslipidemia.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.von Sarnowski B, Lüdemann J, Völzke H, et al. Common carotid intima-media thickness and framingham risk score predict incident carotid atherosclerotic plaque formation: longitudinal results from the study of health in Pomerania. Stroke 2010;41:2375-7 [DOI] [PubMed] [Google Scholar]
- 2.Davis PH, Dawson JD, Riley WA, et al. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation 2001;104:2815-9 [DOI] [PubMed] [Google Scholar]
- 3.Silvestrini M, Cagnetti C, Pasqualetti P, et al. Carotid wall thickness and stroke risk in patients with asymptomatic internal carotid stenosis. Atherosclerosis 2010;210:452-7 [DOI] [PubMed] [Google Scholar]
- 4.Johnsen SH, Mathiesen EB, et al. Carotid plaque compared with intima-media thickness as a predictor of coronary and cerebrovascular disease. Curr Cardiol Rep 2009;11:21-7 [DOI] [PubMed] [Google Scholar]
- 5.Simon A, Gariepy J, Chironi G, et al. Intima-media thickness: a new tool for diagnosis and treatment of cardiovascular risk. J Hypertens 2002;20:159-69 [DOI] [PubMed] [Google Scholar]
- 6.Zureik M, Ducimetière P, Touboul PJ, et al. Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: longitudinal results from the Aging Vascular Study (EVA) study. Arterioscler Thromb Vasc Biol 2000;20:1622-9 [DOI] [PubMed] [Google Scholar]
- 7.Burke GL, Evans GW, Riley WA, et al. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study. Stroke 1995;26:386-91 [DOI] [PubMed] [Google Scholar]
- 8.Veller MG, Fisher CM, Nicolaides AN, et al. Measurement of the ultrasonic intima-media complex thickness in normal subjects. J Vasc Surg 1993;17:719-25 [DOI] [PubMed] [Google Scholar]
- 9.Riley WA, Barnes RW, Applegate WB, et al. Reproducibility of noninvasive ultrasonic measurement of carotid atherosclerosis. The Asymptomatic Carotid Artery Plaque Study. Stroke 1992;23:1062-8 [DOI] [PubMed] [Google Scholar]
- 10.Wendelhag I, Wiklund O, Wikstrand J.Atherosclerotic changes in the femoral and carotid arteries in familial hypercholesterolemia. Ultrasonographic assessment of intima-media thickness and plaque occurrence. Arterioscler Thromb 1993;13:1404-11 [DOI] [PubMed] [Google Scholar]
- 11.Suri JS, Haralick RM, Sheehan FH. Greedy algorithm for error correction in automatically produced boundaries from low contrast ventriculgrams. Pattern Analysis and Applications 2000;3:39-60 [Google Scholar]
- 12.Molinari F, Zeng G, Suri JS. Greedy Technique and Its Validation for Fusion of Two Segmentation Paradigms Leads to an Accurate Intima–Media Thickness Measure in Plaque Carotid Arterial Ultrasound. The Journal for Vascular Ultrasound 2010;34:63–73 [Google Scholar]
- 13.Molinari F, Zeng G, Suri JS. A state of the art review on intima-media thickness (IMT) measurement and wall segmentation techniques for carotid ultrasound. Comput Methods Programs Biomed 2010;100:201-21 [DOI] [PubMed] [Google Scholar]
- 14.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307-10 [PubMed] [Google Scholar]