Abstract
Many common genetic variants identified by genome-wide association studies for complex traits map to genes previously linked to rare inherited Mendelian disorders. A systematic analysis of common single-nucleotide polymorphisms (SNPs) in genes responsible for Mendelian diseases with kidney phenotypes has not been performed. We thus developed a comprehensive database of genes for Mendelian kidney conditions and evaluated the association between common genetic variants within these genes and kidney function in the general population. Using the Online Mendelian Inheritance in Man database, we identified 731 unique disease entries related to specific renal search terms and confirmed a kidney phenotype in 218 of these entries, corresponding to mutations in 258 genes. We interrogated common SNPs (minor allele frequency >5%) within these genes for association with the estimated GFR in 74,354 European-ancestry participants from the CKDGen Consortium. However, the top four candidate SNPs (rs6433115 at LRP2, rs1050700 at TSC1, rs249942 at PALB2, and rs9827843 at ROBO2) did not achieve significance in a stage 2 meta-analysis performed in 56,246 additional independent individuals, indicating that these common SNPs are not associated with estimated GFR. The effect of less common or rare variants in these genes on kidney function in the general population and disease-specific cohorts requires further research.
CKD affects approximately 10% of the general population in industrialized nations, and is significantly associated with cardiovascular morbidity and mortality.1–4 Traditional risk factors for CKD, including diabetes and hypertension, fail to fully explain the increased risk of CKD,5–9 suggesting other factors including a genetic component. Family studies indicate familial aggregation of CKD and ESRD risk.10 For example, family studies have shown that genetic factors account for 36%–75% of the variability in kidney function, with similar estimates for disease susceptibility and CKD progression.10–14 Therefore, unraveling the genetic underpinnings of CKD bears the potential of discovering novel disease mechanisms as a basis for research into much needed therapeutic targets and strategies.
Genome-wide association studies (GWAS) recently identified several genomic loci associated with kidney traits.15–21 The strongest of these associations is at the UMOD locus,15,17,18,20,22,23 a gene in which rare variants are known to cause autosomal-dominant kidney diseases with high risk for ESRD: MCKD2 (Online Mendelian Inheritance in Man [OMIM] database #603860), HNFJ1 (OMIM #162000), or GCKD (OMIM #609886). In addition, other kidney disease genes in which mutations follow Mendelian inheritance patterns were uncovered in GWAS of kidney function (SLC7A9, SLC34A1)17 and albuminuria (CUBN)21 in the general population. Similar examples exist for traits such as hypertension and dyslipidemia, in which common variants in genes causing inherited Mendelian diseases are identified in population-based GWAS.24,25
These findings lead us to hypothesize that additional common variants in monogenic kidney disease genes26,27 are associated with kidney function in the general population but have not yet been identified by GWAS efforts due to power limitations related to multiple testing for nearly 2.5 million SNPs. Thus, we aimed to (1) create a comprehensive, curated database of monogenic kidney disease genes, (2) analyze the association of common genetic variants in these candidate genes with serum creatinine-based estimated GFR (eGFR) and secondarily with CKD in the general population, and (3) examine SNPs beneath the genome-wide threshold that would have been overlooked in prior GWAS of eGFR and CKD.15,17–19
Results
Query of Online OMIM
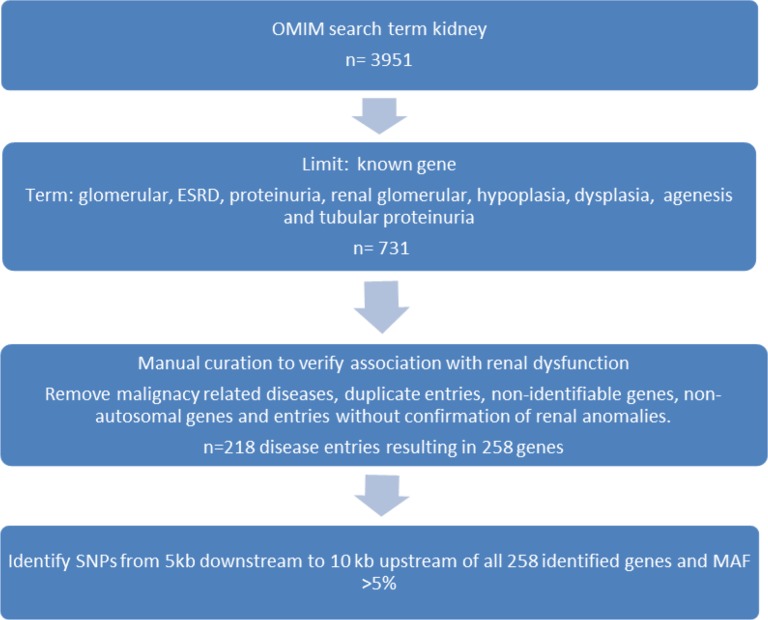
The OMIM database query yielded 731 entries after excluding entries of kidney expressed genes without kidney phenotype: 77 for the term glomerular, 114 for renal tubular, 147 for renal hypoplasia, 128 for renal dysplasia, 84 for renal agenesis, 89 for ESRD, and 92 for proteinuria (Figure 1). Of these, we excluded a total of 513 entries that were not unique, described genes causing renal malignancy, were without an identified gene or were with a nonautosomal gene, or if we could not confirm kidney anomaly or dysfunction on our manual search, leaving a total of 218 OMIM-based disease entries corresponding to a total of 258 unique genes (some syndromes had more than one associated gene). We assigned each OMIM entry to one of three broad categories that corresponded best to their underlying pathology: (1) glomerular/developmental (n=128), (2) tubular function (n=45), or (3) secondary kidney disease (n=45) (see Supplemental Tables 1–3 or Fox28).
Figure 1.
Flow chart showing the process of the three-step OMIM database search.
Interrogation of CKDGen Stage 1 Data Set
We interrogated SNPs with a minor allele frequency (MAF) >5% within these genes in the stage 1 meta-analysis eGFR and CKD data sets of the CKDGen Consortium encompassing 74,354 individuals from 26 cohorts (Supplemental Table 4). A complete listing of all tested SNPs and results is also available online (see Pattaro et al.15 and Fox28). Supplemental Table 5 shows the eGFR stage 1 meta-analysis results for the index SNPs of the 258 genes identified in the three-step OMIM search. Supplemental Tables 6 and 7 show P values for the association of these SNPs with CKD and serum cystatin C–based eGFR (eGFRcys), respectively. Of the 49 loci showing a significant association with eGFR and/or CKD using a gene-specific Bonferroni correction (Table 1), 8 independent SNPs had a P value <10−4 for the association with eGFR. Of these, four SNPs, rs12922822 in UMOD (P=1.20×10−25) and rs12460876 in SLC7A9 (P=9.50×10−12), were previously identified in GWAS meta-analyses of eGFR or CKD,17–19 and rs4073745 in NSD1 and rs894250 in SCARB2 showed linkage disequilibrium (LD; D’>0.2) with the GFR-associated SNPs at the UMOD and SHROOM3 loci. These SNPs were not further considered. The rs11789185 SNP in the ENG gene did not show a direction consistent association with cystatin C and was dropped from our replication pool. Thus, this resulted in a total of three eGFR-associated SNPs (rs6433115 in LRP2, rs9827843 in ROBO2, and rs1050700 in TSC1) and one CKD-associated SNP (rs249942 in PALB2) that moved forward to stage 2 meta-analysis (Table 2). Of these four SNPs, only rs6433115 at LRP2 met the more stringent experiment-wide significance criteria after adjustment for multiple correlated association tests in meta-analysis using the Conneely and Boehnke method (stage 1 meta-analysis P=3.49×10−6, PACTexperiment-wide = 0.05 [P value adjusted for correlated tests for each gene with additional adjustment for the number of genes tested in the experiment]) (Table 2).29,30
Table 1.
SNPs significantly associated with eGFR or CKD in stage 1 meta analysis in the CKDGen Consortium
| Gene Name | Syndrome | SNP ID | Coded Allele Frequency | Trait | P | Phenotype |
|---|---|---|---|---|---|---|
| ACTN4 | FSGS 1, FSGS1 | rs755690 | 0.44 | eGFR | 0.004 | Nephrotic syndrome, ESRD |
| AGXT | Primary hyperoxaluria type I | rs4538195 | 0.06 | CKD | 0.01 | Calcium oxalate accumulation and renal failure |
| AQP2 | Nephrogenic diabetes insipidus, autosomal | rs296736 | 0.52 | eGFR | 0.004 | Diabetes insipidus |
| BBS1 | Bardet-Biedl syndrome (BBS) | rs1671062 | 0.40 | eGFR | 0.001 | Developmental abnormalities with common renal failure |
| BMP4 | Syndromic microphthalmia 6 (MCOPS6) | rs11623717 | 0.58 | eGFR | 0.001 | Hypoplastic kidneys, renal failure possible |
| CA2 | Autosomal recessive osteopetrosis 3, (OPTB3) | rs3758078 | 0.36 | eGFR, CKD | 0.01, 0.04 | Isozymes of carbonic anhydrase, associated with RTA |
| CACNA1S | Hypokalemic periodic paralysis (HOKPP) | rs3850625 | 0.12 | eGFR | 0.0004 | Renal phosphate wasting, associated with hypokalemia and episodic weakness |
| CASR | Familial hypocalciuric hypercalcemia type I, HHC1 acquired hypocalciuric hypercalcemia | rs7638770 | 0.25 | eGFR, CKD | 0.001, 0.0003 | PTH-independent renal tubular defect in calcium reabsorption, associated with hypercalcemia and hypermagnesemia |
| CFI | Complement factor I deficiency GN with isolated C3 deposits and factor I deficiency | rs6815517 | 0.72 | CKD | 0.01 | Deficiency of the C3 inactivator associated with GN and renal failure |
| ENG | Hereditary hemorrhagic telangiectasia Rendu-Osler-Weber (HHT) | rs11789185 | 0.10 | eGFR | 0.001 | Vascular dysplasia, associated with rare hematuria |
| ERCC8 | Cockayne syndrome type A (CSA) | rs158938 | 0.65 | eGFR | 0.002 | Immune complex-mediated GN |
| FGF23 | Hyperphosphatemic familial tumoral calcinosis (HFTC) | rs720333 | 0.85 | eGFR, CKD | 0.003, 0.003 | Increase renal absorption of phosphate, associated with deposition of basic calcium phosphate crystals |
| G6PC | Glycogen storage disease I | rs2593595 | 0.82 | CKD | 0.01 | Glycogen storage with renal failure |
| GIF | Intrinsic factor deficiency (IFD) | rs558660 | 0.18 | eGFR | 0.01 | Cobalamin transport, associated with tubular proteinuria |
| GSS | Glutathione synthetase deficiency | rs2236270 | 0.39 | eGFR | 0.0002 | Urinary excretion of 5-oxoproline, associated with metabolic acidosis, RTA |
| HOXD13 | VACTERL association | rs847148 | 0.69 | eGFR | 0.001 | Dysplasia, hydronephrosis with likely failure |
| ICK | Endocrine-cerebroosteodysplasia (ECO) | rs316144 | 0.43 | eGFR | 0.001 | Cystically dilated renal tubules |
| INF2 | FSGS 5 (FSGS5) | rs7140154 | 0.18 | eGFR | 0.01 | FSGS, may lead to ESRD |
| JAG1 | Alagille syndrome 1 (ALGS1) | rs6040050 | 0.29 | eGFR | 0.0004 | Renal dysplasia, renal mesangiolipidosis, medullary cystic disease |
| KCNJ1 | Bartter syndrome, antenatal type 2 | rs2238009 | 0.14 | eGFR | 0.01 | Potassium channel, associated with salt wasting, hypokalemic alkalosis, hypercalciuria, low BP, and nephrocalcinosis Potassium channel, associated with salt wasting, hypokalemic alkalosis, hypercalciuria, low BP, and nephrocalcinosis |
| KRAS | Cardiofaciocutaneous syndrome | rs7960917 | 0.78 | eGFR | 0.001 | Prenatal hydronephrosis, reflux |
| LAMB2 | Pierson syndrome | rs9880088 | 0.10 | eGFR, CKD | 0.0002, 0.02 | Congenital nephrotic syndrome; early onset ESRD |
| LCAT | Lecithin: cholesterol acyltransferase deficiency (LCAT) | rs2292318 | 0.13 | eGFR, CKD | 0.01, 0.01 | Proteinuria and renal failure |
| LRP2 | Donnai-Barrow syndrome | rs6433115 | 0.79 | eGFR | 3.5×10−6 | Proteinuria |
| MKKS | McKusick-Kaufman syndrome (MKKS) | rs6032878 | 0.89 | eGFR | 0.01 | Reproductive system developmental abnormalities, with possible renal failure |
| MMACHC | Methylmalonic aciduria and homocystinuria, type cblC | rs12029322 | 0.22 | eGFR | 0.004 | Thrombotic microangiopathic nephropathy, hematuria, proteinuria, and renal failure |
| NEU1 | Neuramidase deficiency sialidosis type I | rs13118 | 0.93 | eGFR | 0.003 | Lysosomal storage, sialyloligosacchariduria |
| NSD1 | Sotos syndrome | rs4073745 | 0.69 | eGFR, CKD | 3.7×10−6, 0.002 | Rare vesicoureteric reflux |
| PALB2 | Fanconi anemia | rs249942 | 0.10 | eGFR, CKD | 0.002, 0.0002 | CAKUT, renal malformations |
| PKD2 | Autosomal dominant polycystic kidney disease (ADPKD) | rs2728111 | 0.77 | eGFR, CKD | 0.01, 0.01 | Renal cysts, ESRD |
| PLCE1 | Early onset nephrotic syndrome (NPHS3) | rs12258052 | 0.31 | eGFR | 0.001 | FSGS, nephrotic proteinuria, and ESRD |
| PROKR2 | Kallmann syndrome 3 (KAL3) | rs6053283 | 0.25 | eGFR | 0.01 | Reproductive dysfunction, angiogenesis, renal agenesis |
| PSTPIP1 | Pyogenic sterile arthritis, pyoderma gangrenosum, and acne | rs3936040 | 0.17 | eGFR | 0.01 | Proteinuria, possibly immune mediated |
| PVRL1 | Cleft palate ectodermal dysplasia syndrome (CLPED1); orofacial cleft 7 (OFC7) | rs7122134 | 0.60 | eGFR | 0.01 | Renal dysplasia |
| RECQL4 | Baller-Gerold syndrome (BGS) | rs10111332 | 0.52 | eGFR | 0.003 | Renal dysplasia |
| RET | Ret protooncogene | rs1864405 | 0.25 | eGFR | 0.002 | Renal agenesis, vesicoureteric reflux |
| ROBO2 | Vesicoureteral reflux 2 (VUR2) | rs9827843 | 0.58 | eGFR | 0.001 | CAKUT, reflux nephropathy |
| SCARB2 | Action myoclonus-renal failure syndrome (AMRF) | rs894250 | 0.50 | eGFR | 0.001 | FSGS, nephrotic syndrome, renal failure |
| SCNN1B | Liddle syndrome | rs2106374 | 0.81 | eGFR | 0.001 | Hypertension, renal failure rare |
| SLC7A9 | Cystinuria type A | rs12460876 | 0.61 | eGFR, CKD | 9.5×10−12, 0.004 | Cystine precipitation, obstruction, and renal failure |
| SOX17 | Vesicoureteral reflux 1 (VUR1) | rs16920355 | 0.16 | CKD | 0.004 | CAKUT and ESRD |
| STRA6 | Syndromic microphthalmia 9 (MCOPS9) | rs974456 | 0.23 | eGFR | 0.002 | Horseshoe kidney, hydronephrosis, hypoplasia, can lead to ESRD |
| SUCLA2 | Autosomal recessive mitochondrial DNA depletion syndrome, encephalopathic form with methylmalonic aciduria | rs6561429 | 0.91 | CKD | 0.003 | Possibly mitochondrial DNA depletion, rare renal tubular dysfunction |
| TBX1 | Di George syndrome (DGS) | rs4819843 | 0.19 | CKD | 0.01 | Renal hypoplasia, renal insufficiency |
| TSC1 | Tuberous sclerosis 1 (TSC1) | rs1050700 | 0.71 | eGFR | 0.00004 | Renal cysts and tumors, without kidney failure |
| TTC8 | Bardet-Biedl syndrome (BBS) | rs17700521 | 0.73 | eGFR, CKD | 0.001, 0.01 | Developmental abnormalities with common renal failure |
| UMOD | Medullary cystic kidney disease 2 (MCKD2) | rs12922822 | 0.18 | eGFR, CKD | 1.2×10−25, 5.5×10−17 | Medullary cysts with gouty arthritis |
| USF2 | Upstream stimulatory factor 2 | rs1882694 | 0.65 | eGFR | 0.002 | Cystic renal dysplasia and hypodysplasia |
| WDPCP | Bardet-Biedl syndrome (BBS 1–15) | rs1850983 | 0.97 | eGFR, CKD | 0.001, 0.002 | Developmental abnormalities with common renal failure |
Results are from meta-analysis of 74,354 participants. Gene-specific significance thresholds were defined according to the Bonferroni method, as 0.05/ number of independent LD blocks within each gene. If a locus was significantly associated with both eGFR (<60 ml/min per 1.73 m2) and CKD, both P values are provided, respectively. RTA, renal tubular acidosis; PTH, parathyroid hormone; CAKUT, congenital anomalies of the kidney and urinary tract.
Table 2.
Results of stage 1 and stage 2 association meta-analysis
| Trait | SNP ID | Locus | Effect Allele | Stage 1 Discovery Meta-Analysis | Stage 2 Replication Meta-Analysis | Stage 1 and 2 Combined Meta-Analysis | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | P | PACT experiment-wide | β | P | β | P | ||||
| eGFR | rs6433115 | LRP2 | T | −0.007 | 3.5×10−6 | 0.05 | 0.0005 | 0.42a | 0.003 | 0.02a |
| eGFR | rs1050700 | TSC1 | T | −0.006 | 4.3×10−5 | 0.06 | −0.002 | 0.14 | −0.004 | 3×10−4 |
| CKD | rs249942 | PALB2 | A | 0.15 | 2.1×10−4 | 0.10 | −0.007 | 0.66 | 0.017 | 0.30 |
| eGFR | rs9827843 | ROBO2 | C | 0.005 | 4.8×10−5 | 0.10 | 0.0005 | 0.36 | 0.003 | 1.4×10−3 |
Results are from stage 1 meta-analysis of 74,354 participants and stage 2 meta-analysis of 56,246 participants using a fixed-effects model except where indicated otherwise. Stage 1 and stage 1 and 2 combined meta-analysis P values were two sided and one-sided for stage 2 meta-analysis. GFR was estimated by serum creatinine.
Effect estimates and P values from a random-effects model due to significant heterogeneity in stage 2 meta-analysis.
Stage 2 Meta-Analyses
Stage 2 meta-analysis of the stage 1 meta-analysis significant locus (LRP2) and our three other top loci was performed in a total of 19 independent cohorts totaling 56,246 individuals (Supplemental Table 4). In stage 2 meta-analysis, rs6433115 in LRP2 showed evidence of heterogeneity (I2=54.6%, P=0.002). We thus tested for stage 2 meta-analysis significance using a random-effects model that is more robust in the setting of between-study heterogeneity, under which rs6433115 was not significantly associated with eGFR (one-sided P=0.42). Using a distinct pathway-based approach, a different SNP in LRP2, rs10490130, was recently found to be associated with eGFR.31 However, this locus was not in strong LD with the SNP identified in this project (rs6433115; R2=0.11, D’=0.75). The other three SNPs analyzed in stage 2 were also not significantly associated with eGFR (Table 2).
Discussion
We have curated a comprehensive list of Mendelian genes that were previously linked to kidney pathology, followed by the exploration of common SNPs in these genes for association with eGFR or CKD in the CKDGen meta-analysis of population-based genetic association studies. Overall, our results show that common genetic variants are not typically associated with eGFR in Mendelian kidney disease genes.
The SNP associations we present for our stage 1 meta-analysis are obtained from the results of the same GWAS meta-analysis data sets as those used in our previously published GWAS.15 The intent of our study was to focus systematically on SNPs in the curated list of candidate Mendelian genes, most of which were not previously reported in our prior work.15 Indeed, it is well established that current GWAS approaches miss many true associations due to limited power and the high penalty to be paid for an unbiased approach. We thus identified 45 additional SNPs showing a nominally significant association with eGFR or CKD in the stage 1 meta-analysis that did not meet our criteria for being considered for stage 2 meta-analysis. These SNPs and the curated list of Mendelian kidney disease genes and their measures of association with eGFR and CKD may represent a valuable resource for further research (Supplemental Tables 1–3, 5–7, and Fox28).
Our findings suggest that targeting common variants within Mendelian kidney disease genes for associations with more subtle phenotype variation such as cross-sectional measures of eGFR in the general population may not easily identify new gene loci that have not already been identified by current large-scale GWAS.15,17 However, we feel that further exploration of these candidate genes should be extended beyond this first step. Examples include conducting future analysis of less common variants (e.g., with MAF 1%–5%) in these gene regions using SNP data sets imputed to the 1000 Genomes reference panel,32 or using targeted sequencing or whole exome chip data as well as further replication efforts in disease-specific and prospective cohorts.
The strengths of this study include the manual curation of a kidney gene database followed by a systematic search, identification of potential candidate loci, and the large sample size used for variant discovery. Our study has some limitations. First, because we analyzed population-based cohorts, our findings are not generalizable to cohorts enriched for kidney disease. Second, despite significant effort to curate a comprehensive and extensive list of Mendelian genes affecting renal function, our query may not capture all discovered genes; moreover, not all of the genes are completely confirmed as causative for the noted phenotypes. Third, of all of the numerous loci with a gene-based significant association with kidney function in stage 1, we only followed up the four most significantly associated SNPs. Thus, we cannot exclude that true positive associations are among the SNPs not further pursued. Finally, because this was a cross-sectional study, we were not able to explore the association of our candidate SNPs with kidney disease progression.
In summary, we have manually curated the largest published list of Mendelian kidney disease genes. In these genes, we did not identify novel common gene variants that are robustly associated with renal function in the general population. Further research is needed to determine the role of less common variants in these genes in disease and population-based studies.
Concise Methods
Query of OMIM
Using the unspecific search term kidney yielded 3951 entries in an OMIM query (http://www.ncbi.nlm.nih.gov/omim) (Figure 1). To focus our search on inherited kidney disease leading to kidney malformations, dysfunction, and ESRD, we utilized the following three-step search procedure: (1) recording of all listings using the search terms glomerular, renal tubular, renal hypoplasia, renal dysplasia, renal agenesis, ESRD, and proteinuria, each entered separately; (2) exclusion of duplicate entries, genes causing renal malignancy, genes expressed in kidney without a clear kidney phenotype, nonautosomal genes, and entries without clearly identified genes; and (3) manual OMIM and PubMed searches of the remaining loci to confirm an identifiable kidney phenotype (defined as documented kidney anomalies and any evidence of glomerular or tubular dysfunction). These conditions were then classified into three categories: (1) developmental and/or glomerular origin, (2) tubular function related, and (3) secondary kidney disease (e.g., amyloid deposition).
Stage 1 Analysis—Interrogation of the CKDGen GWAS Meta-Analysis Data Set
For each gene in the curated gene list, we examined the stage 1 meta-analysis results for the association between eGFR and all common SNPs in the gene region. We restricted our analyses to SNPs with a MAF >5% due to power considerations and imputation quality consideration for SNPs with low MAF. We defined each gene region as 10 kb upstream and 5 kb downstream of the known transcription start and end sites of the gene, using build 36 of the reference genome as the reference.
Each of the participating cohorts of the CKDGen Consortium (Supplemental Table 1) performed GWAS of eGFR and CKD or eGFRcys using linear and logistic regression for continuous and dichotomous traits, respectively. An additive genetic effect model for the genotype dosages was used, adjusting for age and sex in all studies and for the study site and relatedness where applicable. Study-specific genotyping and HapMap-based imputation platforms were previously described.15 Study-specific GWAS data were subjected to inverse-variance weighted fixed-effects meta-analysis using METAL software (http://www.sph.umich.edu/csg/abecasis/Metal/).32 Genomic control was applied as previously described.15
Within each gene, the SNP with the lowest eGFR-associated P value was chosen as the index SNP representing that gene. Once these index SNPs were identified, we secondarily tested for the association between these SNPs and CKD (eGFR <60 ml/min per 1.73 m2) from the CKDGen meta-analysis.
Gene-specific significance thresholds were defined, according to the Bonferroni method, as 0.05/ (the number of independent tests within the gene). The denominator is given by the number of independent LD blocks, whereby independent blocks were identified by grouping SNPs in LD (r2>0.20, based on HapMap Phase 2 release 21) together. To reduce the likelihood of a false positive result, we used the Conneely and Boehnke method for adjustment of multiple correlated association tests in meta-analysis.28,29 This is an alternative method to other multiple testing adjustment methods that do not properly account for correlation between SNPs. This method computes the PACTexperiment-wide for each gene locus. Because individual-level genotypes were not available, we used genotypes from HapMap Phase 2 CEU samples to estimate correlation matrices for SNPs. A PACTexperiment-wide <0.05 was defined as being significant experiment wide.
Stage 2 Analyses
SNPs were selected for stage 2 meta-analysis of their association with eGFR in independent cohorts if they met the following criteria: (1) they had an association P value <10−4 in the CKDGen discovery result for either eGFR or CKD; (2) the associations with eGFR, CKD, and eGFRcys were all direction consistent; and (3) they mapped into regions not previously associated with eGFR in GWAS. If no SNPs reached the defined P value threshold of <10−4 for eGFR or CKD, we selected the SNP with the lowest P value for the association.
SNPs thus identified were analyzed in stage 2 analysis in 19 independent cohorts (Supplemental Table 4) using inverse-variance weighted meta-analysis in METAL software.15,33 Significance in stage 2 meta-analysis was defined as one-sided P<0.05. Information regarding de novo and in silico genotyping and imputation platforms for the stage 2 cohorts was previously described.15
Disclosures
None.
Acknowledgments
AGES. The Age, Gene/Environment Susceptibility (AGES) study was funded by the National Institutes of Health (NIH) (contract N01AG12100), the National Institute on Aging (NIA) Intramural Research Program, Hjartavernd (the Icelandic Heart Association), and the Althingi (the Icelandic Parliament).
Amish Study. The Amish study was supported by NIH grants and contracts (R01AG18728, Amish Longevity Study; R01HL088119, Amish Calcification Study; U01GM07451804, Pharmacogenomics of Anti-Platelet Intervention [PAPI] Study; U01HL072515-06, Heredity and Phenotype Interaction [HAPI] Study; and U01-HL084756 and K12RR023250), as well as grants from the University of Maryland (MCRDP grant), University of Maryland General Clinical Research Center (M01RR16500), Baltimore Veterans Affairs Medical Center Geriatrics Research and Education Clinical Center, and the Paul Beeson Physician Faculty Scholars in Aging Program.
ASPS. The Austrian Stroke Prevention Study (ASPS) research reported in this article was funded by grants from the Austrian Science Fund (P20545P05 and P13180). The Medical University of Graz supported the databank of the ASPS.
ARIC. The Atherosclerosis Risk in Communities (ARIC) study is carried out as a collaborative study supported by the National Heart, Lung, and Blood Institute (NHLBI) (contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, HHSN268201100012C, R01HL087641, R01HL59367, and R01HL086694), the National Human Genome Research Institute (NHGRI) (U01HG004402), and the NIH (HHSN268200625226C). Infrastructure was partly supported by a component of the NIH and NIH Roadmap for Medical Research (Grant UL1RR025005). A.K. and C.H. were supported by the Emmy Noether programme of the German Research Foundation (KO3598/2-1). The authors thank the staff and participants of the ARIC study for their important contributions.
BLSA. The Baltimore Longitudinal Study of Aging (BLSA) was supported in part by the Intramural Research Program of the NIH NIA.
CHS. The Cardiovascular Health Study (CHS) research reported in this article was supported by the NHLBI (contracts N01HC85079 through N01HC85086, N01HC35129, N01HC15103, N01HC55222, N01HC75150, and N01HC45133; grants U01HL080295 and R01HL087652), with additional contributions from the National Institute of Neurological Disorders and Stroke. A full list of principal CHS investigators and institutions is available at http://www.chs-nhlbi.org/pi.htm. DNA handling and genotyping was supported in part by a National Center for Research Resources grant (M01RR00425) to the Cedars-Sinai General Clinical Research Center genotyping core and a National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant (DK063491) to the Southern California Diabetes Endocrinology Research Center.
ERF. The Erasmus Rucphen Family (ERF) study was supported by grants from the Netherlands Organization for Scientific Research (Pioneer grant), Erasmus Medical Center, Centre for Medical Systems Biology, and Netherlands Kidney Foundation.
FHS. The Family Heart Study (FHS) work was supported in part by the NHLBI (grants 5R01HL08770003 and 5R01HL08821502 to M.P.) and the NIDDK (5R01DK07568102 and 5R01DK06833603 to I.B.).
Framingham Heart Study. The Framingham Heart Study research reported in this paper was conducted in part using data and resources from the Framingham Heart Study of the NIH NHLBI and the Boston University School of Medicine. The analyses reflect intellectual input and resource development from the Framingham Heart Study investigators participating in the SNP Health Association Resource (SHARe) project. This work was partially supported by NHLBI Framingham Heart Study contracts (N01HC25195) as well as an Affymetrix contract for genotyping services (N02HL64278). A portion of this research utilized the Linux Cluster for Genetic Analysis funded by the Robert Dawson Evans Endowment of the Department of Medicine at Boston University School of Medicine and Boston Medical Center.
GENOA. The Genetic Epidemiology Network of Arteriopathy (GENOA) research was partially supported by the NHLBI (R01HL87660).
Health ABC. The Health Aging and Body Composition Study (Health ABC) was funded by the NIA. This research was supported by the NIA (contracts N01AG62101, N01AG62103, and N01AG62106). The GWAS was funded by a NIA grant (1R01AG032098-01A1) to Wake Forest University Health Sciences. Genotyping services were provided by the Center for Inherited Disease Research (CIDR). CIDR is fully funded through a federal contract from the NIH to Johns Hopkins University (HHSN268200782096C). This research was supported in part by the Intramural Research Program of the NIH NIA.
KORA. For the Kooperative Gesundheitsforschung in der Region Augsburg (KORA) F3 and F4 studies, the genetic epidemiological work was funded by an NIH subcontract from the Children’s Hospital Boston (prime grant 1 R01DK07578701A1 to H.E.W. and I.M.H.), the German National Genome Research Net NGFN2 and NGFNplus (01GS0823 to H.E.W.; WK project A3, 01GS0834), the Munich Center of Health Sciences as part of LMUinnovativ, and by Else Kröner-Fresenius-Stiftung (P48/08//A11/08 to C.A.B. and B.K.K. and 2012_A147 to C.A.B. and I.M.H.). The F3 kidney parameter measurements were funded by Else Kröner-Fresenius-Stiftung (to C.A.B. and B.K.K.) and the Regensburg University Medical Center, Germany, and the F4 measurements were funded by the University of Ulm, Germany (to W.K.). Genome-wide genotyping costs in F3 and F4 were funded in part by Else Kröner-Fresenius-Stiftung (to C.A.B. and B.K.K.). De novo genotyping in F3 and F4 was funded by the Else Kröner-Fresenius-Stiftung (C.A.B. and B.K.K.). C.A.B. has received research funding from Else Kröner-Fresenius-Stiftung, KfH Stiftung Präventivmedizin, and Doktor Robert Pfleger-Stiftung. The KORA research platform and the Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) Augsburg studies were initiated and financed by the German Research Center for Environmental Health, the German Research Center for Environmental Health, the German Federal Ministry of Education and Research, and the State of Bavaria. Genotyping was performed in the Genome Analysis Center of the German Research Center for Environmental Health. The LINUX platform for computation was funded by the University of Regensburg for the Department of Epidemiology and Preventive Medicine at the Regensburg University Medical Center.
NHS/HPFS. The Nurses' Health Study (NHS)/Health Professionals' Follow-Up Study (HPFS) type 2 diabetes GWAS (U01HG004399) is a component of a collaborative project that includes 13 other GWAS (U01HG004738, U01HG004422, U01HG004402, U01HG004729, U01HG004726, U01HG004735, U01HG004415, U01HG004436, U01HG004423, U01HG004728, RFAHG006033; U01DE018993, all funded by the NHGRI; U01DE018903 from the National Institute of Dental and Craniofacial Research). The study is also funded as part of the Gene Environment-Association Studies (GENEVA) under the NIH Genes, Environment, and Health Initiative (GEI). Assistance with phenotype harmonization and genotype cleaning, as well as with general study coordination, was provided by the GENEVA Coordinating Center (U01HG004446). Assistance with data cleaning was provided by the National Center for Biotechnology Information. Genotyping was performed at the Broad Institute of the Massachusetts Institute of Technology and Harvard University, with funding support from the NIH GEI (U01HG04424), as well as the Johns Hopkins University Center for Inherited Disease Research, with support from the NIH GEI (U01HG004438) and the NIH (contract HHSN268200782096C). Additional funding for the current research was provided by the National Cancer Institute (NCI) (P01CA087969 and P01CA055075) and the NIDDK (R01DK058845). The authors thank the staff and participants of the NHS and HPFS for their dedication and commitment.
Korcula. The Korcula study was supported through grants from the Medical Research Council UK (to H.C., A.F.W., and I. R.) and by the Ministry of Science, Education, and Sport of the Republic of Croatia (108-1080315-0302 to I.R.).
MICROS. The MICROS study was supported by the Ministry of Health and Department of Educational Assistance, the Universities and Research of the Autonomous Province of Bolzano, the South Tyrolean Sparkasse Foundation, and the European Union framework program 6 EUROSPAN project (contract LSHG-CT-2006018947).
Northern Swedish Population Health Study. The Northern Swedish Population Health Study was supported by grants from the Swedish Natural Sciences Research Council, the European Union through the EUROSPAN project (contract LSHG-CT-2006018947), the Foundation for Strategic Research (SSF), and the Linneaus Centre for Bioinformatics.
NHS. The Nurses’ Health Study (NHS) renal function and albuminuria work was supported by a NIDDK grant (DK66574). Additional funding for the current research was provided by the NCI (P01CA087969 and P01CA055075) and the NIDDK (R01DK058845).
ORCADES. The Orkney Complex Disease Study (ORCADES) was supported by the Chief Scientist Office of the Scottish Government, the Royal Society, and the European Union framework program 6 EUROSPAN project (contract LSHG-CT-2006018947). DNA extractions were performed at the Wellcome Trust Clinical Research Facility in Edinburgh.
PopGen. The PopGen study was supported by the German Ministry of Education and Research through the National Genome Research Network, and the Ministry of Science, Commerce, and Transportation of the State of Schleswig-Holstein. The project has also received infrastructure support through the DFG “Inflammation at Interfaces” excellence cluster.
SORBS. The SORBS study was funded by grants from the German Research Council (KFO152 to M.S.) and the Adiposity Diseases Integrated Research and Treatment Center (K7-37 to M.S. and A.T.). The authors also thank Dr. Knut Krohn (Microarray Core Facility of the Interdisciplinary Centre for Clinical Research, University of Leipzig, Germany) for providing the genotyping platform. I.P. is funded in part through the European Community’s Seventh Framework Programme (FP7/2007-2013), ENGAGE project (grant agreement HEALTH-F4-2007- 201413). R.M. acknowledges financial support from the European Commission under a Marie Curie Intra-European Fellowship.
Rotterdam Study-I and Rotterdam Study-II. For the Rotterdam Study-I and Rotterdam Study-II, the GWAS was funded by the Netherlands Organization of Scientific Research (NWO) (175-010-2005-011 and 911-03-012), the Research Institute for Diseases in the Elderly (RIDE2; 014-93-015,), and the Netherlands Genomics Initiative (NGI)/Netherlands Consortium for Healthy Aging (NCHA) project (050-060-810). The Rotterdam Study is funded by Erasmus Medical Center, Erasmus University, Netherlands Organization for Health Research and Development, Research Institute for Diseases in the Elderly (RIDE), the Ministry of Education, Culture, and Science, the Ministry for Health, Welfare, and Sports, the European Commission (DG XI), and the Municipality of Rotterdam. The Erasmus Computing Grid (Rotterdam, The Netherlands) and the national German MediGRID and Services@MediGRID part of the German D-Grid were both funded by grants from the German Bundesministerium fuer Forschung und Technology (01-AK803A-H and 01-IG07015G) for access to their grid resources. A.D. is supported by an NWO grant (vici, 918-76-619).
SHIP. The Study of Health in Pomerania (SHIP) is part of the Community Medicine Research net of the University of Greifswald, Germany, funded by grants from the Federal Ministry of Education and Research (01ZZ9603, 01ZZ0103, and 01ZZ0403), the Ministry of Cultural Affairs, as well as the Social Ministry of the Federal State of Mecklenburg-West Pomerania. Genome-wide data have been supported by a grant from the Federal Ministry of Education and Research (03ZIK012) as well as a joint grant from Siemens Healthcare (Erlangen, Germany) and the Federal State of Mecklenburg-West Pomerania. The University of Greifswald is a member of the Center of Knowledge Interchange program of Siemens AG.
Vis. The Vis study was supported through grants from the Medical Research Council UK (to H.C., A.F.W., and I.R.), the Ministry of Science, Education, and Sport of the Republic of Croatia (108-1080315-0302 to I.R.), and the European Union framework program 6 EUROSPAN project (contract LSHG-CT-2006-018947).
WGHS. The Women's Genome Health Study (WGHS) is supported by the NHLBI (HL043851 and HL69757) and the NCI (CA047988), the Donald W. Reynolds Foundation, and the Fondation Leducq, with collaborative scientific support and funding for genotyping provided by Amgen.
3 City Study. The 3 City Study was supported by the National Foundation for Alzheimer’s Disease and Related Disorders, the Institut Pasteur de Lille, and the Centre National de Génotypage. The 3 City Study was performed as part of a collaboration between the Institut National de la Santé et de la Recherche Médicale (INSERM), the Victor Segalen Bordeaux II University, and Sanofi-Synthélabo. The Fondation pour la Recherche Médicale funded the preparation and initiation of the study. The 3 City Study was also funded by the Caisse Nationale Maladie des Travailleurs Salariés, Direction Générale de la Santé, MGEN, Institut de la Longévité, Agence Française de Sécurité Sanitaire des Produits de Santé, the Aquitaine and Bourgogne Regional Councils, Fondation de France and the joint French Ministry of Research/INSERM “Cohortes et collections de données biologiques” programme. L.G. received an unconditional grant from Eisai.
BMES. The Blue Mountains Eye Study (BMES) has been supported by grants from the Australian Research and Development Grants Advisory Committee (1992-94) and the Australian National Health and Medical Research Council, Canberra Australia (974159, 211069, 991407, and 457349). The GWAS studies of he BMES population are supported by grants from the Australian National Health and Medical Research Council (512423, 475604, 529912) and the Wellcome Trust UK (2008), as part of Wellcome Trust Case Control Consortium 2 (085475/B/08/Z and 085475/08/Z to A.V., P.Mc., P.Mi., F.T., P.F.). E.G.H. and J.J.W. are funded by the Australian National Health and Medical Research Council Fellowship Schemes.
CoLaus. The CoLaus study received financial contributions from GlaxoSmithKline, the Faculty of Biology and Medicine of Lausanne, and the Swiss National Science Foundation (33CSCO-122661). M.Bo. is supported by the Swiss School of Public Health Plus.
YFS. The Cardiovascular Risk in Young Finns study (YFS) is supported by grants from the Academy of Finland (117797, 121584, and 126925), the Social Insurance Institution of Finland, University Hospital Medical funds to Tampere and Turku University Hospitals, the Finnish Foundation of Cardiovascular Research, and the Emil Aaaltonen Foundation (to T.L.).
University of Tartu Estonian Gene Project. The Estonian Genome Center of the University of Tartu (EGCUT) received support from FP7 grants (201413 ENGAGE, 212111 BBMRI, 205419 ECOGENE, 245536 OPENGENE) and also received targeted financing from Estonian Government (SF0180142s08) and from the European Union through the European Regional Development Fund, in the frame of the Centre of Excellence in Genomics.
FamHS-II. The research of the FamHS-II was conducted in part using data and resources from the NHLBI Family Heart Study supported in part by an NIH grant (5R01HL08770002).
GoDARTS. For the Genetics of Diabetes Audit and Research Tayside (GoDARTS) study, the Wellcome Trust provides support for the Wellcome Trust United Kingdom Type 2 Diabetes Case Control Collection and the informatics support is provided by the Chief Scientist Office, and the Wellcome Trust funded Scottish Health Informatics Programme.
INGI-Carlantino and INGI-FVG. The INGI-Carlantino and INGI-FVG studies were supported by grants from Telethon, FVG region, and Fondo Trieste. The INGI-Cilento study was supported by grants from the European Union (Vasoplus-037254), the Italian Ministry of Universities (FIRB -RBIN064YAT), the Assessorato Ricerca Regione Campania, the Ente Parco Nazionale del Cilento e Vallo di Diano, and the Fondazione Banco di Napoli to M Ciullo. The INGI–Val Borbera Study was supported from Compagnia di San Paolo (Torino, Italy), Cariplo Fundation (Milano, Italy), and Italian Ministry of Health Progetto Finalizzato 2007 and 2009.
JUPITER. The Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) trial and the genotyping were supported by AstraZeneca. The Ogliastra Genetic Park (OGP) Replication Study and the OGP Talana study were supported by grants from the Italian Ministry of Education, University (5571/DSPAR/2002), and Research (718/Ric/2005).
PROSPER. The Prospective Study of Pravastatin in the Elderly at Risk (PROSPER) trial was supported by an investigator-initiated grant from Bristol-Myers Squibb. The study was conducted, analyzed, and reported independently of the company. The research leading to these results has received funding from the European Union's Seventh Framework Programme (FP7/2007-2013, under Grant Agreement HEALTH-F2-2009-223004). For a part of the genotyping, we received funding from the Netherlands Consortium of Healthy Aging (NGI 05060810).
SAPALDIA. The Swiss Study on Air Pollution and Lung Disease in Adults (SAPALDIA) was supported by grants from the Swiss National Science Foundation (33CSCO-108796, 3247BO-104283, 3247BO-104288, 3247BO-104284, 3247-065896, 3100-059302, 3200-052720, 3200-042532, and 4026-028099), the Federal Office for Forest, Environment, and Landscape, the Federal Office of Public Health, the Federal Office of Roads and Transport, the canton's government of Aargau, Basel-Stadt, Basel-Land, Geneva, Luzern, Ticino, Zurich, the Swiss Lung League and the canton's Lung League government of Basel Stadt/Basel Landschaft, Geneva, Ticino, and Zurich.
SAPHIR. The Salzburg Atherosclerosis Prevention program in subjects at High Individual Risk (SAPHIR) study was partially supported by a grant from the Kamillo Eisner Stiftung (to B.P.) and by grants from the Genomics of Lipid-Associated Disorders of the Austrian Genome Research Programme GEN-AU (to F.K.). For eQTL analysis, H.J.G received support from a Ellison Medical Foundation/American Federation for Aging Research postdoctoral fellowship and a Stanford Dean’s postdoctoral fellowship. H.E.W. and S.K.K. were supported by grants from the NIA, NHGRI, and NIGMS.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2012100983/-/DCSupplemental.
References
- 1.Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, Nahas ME, Jaber BL, Jadoul M, Levin A, Powe NR, Rossert J, Wheeler DC, Lameire N, Eknoyan G: Chronic kidney disease as a global public health problem: Approaches and initiatives - a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 72: 247–259, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT, Chronic Kidney Disease Prognosis Consortium : Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet 375: 2073–2081, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumeister SE, Böger CA, Krämer BK, Döring A, Eheberg D, Fischer B, John J, Koenig W, Meisinger C: Effect of chronic kidney disease and comorbid conditions on health care costs: A 10-year observational study in a general population. Am J Nephrol 31: 222–229, 2010 [DOI] [PubMed] [Google Scholar]
- 4.Meguid El Nahas A, Bello AK: Chronic kidney disease: The global challenge. Lancet 365: 331–340, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR, UKPDS GROUP : Development and progression of nephropathy in type 2 diabetes: The United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int 63: 225–232, 2003 [DOI] [PubMed] [Google Scholar]
- 6.Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C: Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med 165: 923–928, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Hunsicker LG, Adler S, Caggiula A, England BK, Greene T, Kusek JW, Rogers NL, Teschan PE: Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int 51: 1908–1919, 1997 [DOI] [PubMed] [Google Scholar]
- 8.Kastarinen M, Juutilainen A, Kastarinen H, Salomaa V, Karhapää P, Tuomilehto J, Grönhagen-Riska C, Jousilahti P, Finne P: Risk factors for end-stage renal disease in a community-based population: 26-year follow-up of 25,821 men and women in eastern Finland. J Intern Med 267: 612–620, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Ritz E, Stefanski A: Diabetic nephropathy in type II diabetes. Am J Kidney Dis 27: 167–194, 1996 [DOI] [PubMed] [Google Scholar]
- 10.Satko SG, Sedor JR, Iyengar SK, Freedman BI: Familial clustering of chronic kidney disease. Semin Dial 20: 229–236, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Placha G, Canani LH, Warram JH, Krolewski AS: Evidence for different susceptibility genes for proteinuria and ESRD in type 2 diabetes. Adv Chronic Kidney Dis 12: 155–169, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Fox CS, Muntner P: Trends in diabetes, high cholesterol, and hypertension in chronic kidney disease among U.S. adults: 1988-1994 to 1999-2004. Diabetes Care 31: 1337–1342, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D: Predictors of new-onset kidney disease in a community-based population. JAMA 291: 844–850, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Pattaro C, Köttgen A, Teumer A, Garnaas M, Böger CA, Fuchsberger C, Olden M, Chen MH, Tin A, Taliun D, Li M, Gao X, Gorski M, Yang Q, Hundertmark C, Foster MC, O’Seaghdha CM, Glazer N, Isaacs A, Liu CT, Smith AV, O’Connell JR, Struchalin M, Tanaka T, Li G, Johnson AD, Gierman HJ, Feitosa M, Hwang SJ, Atkinson EJ, Lohman K, Cornelis MC, Johansson A, Tönjes A, Dehghan A, Chouraki V, Holliday EG, Sorice R, Kutalik Z, Lehtimäki T, Esko T, Deshmukh H, Ulivi S, Chu AY, Murgia F, Trompet S, Imboden M, Kollerits B, Pistis G, Harris TB, Launer LJ, Aspelund T, Eiriksdottir G, Mitchell BD, Boerwinkle E, Schmidt H, Cavalieri M, Rao M, Hu FB, Demirkan A, Oostra BA, de Andrade M, Turner ST, Ding J, Andrews JS, Freedman BI, Koenig W, Illig T, Döring A, Wichmann HE, Kolcic I, Zemunik T, Boban M, Minelli C, Wheeler HE, Igl W, Zaboli G, Wild SH, Wright AF, Campbell H, Ellinghaus D, Nöthlings U, Jacobs G, Biffar R, Endlich K, Ernst F, Homuth G, Kroemer HK, Nauck M, Stracke S, Völker U, Völzke H, Kovacs P, Stumvoll M, Mägi R, Hofman A, Uitterlinden AG, Rivadeneira F, Aulchenko YS, Polasek O, Hastie N, Vitart V, Helmer C, Wang JJ, Ruggiero D, Bergmann S, Kähönen M, Viikari J, Nikopensius T, Province M, Ketkar S, Colhoun H, Doney A, Robino A, Giulianini F, Krämer BK, Portas L, Ford I, Buckley BM, Adam M, Thun GA, Paulweber B, Haun M, Sala C, Metzger M, Mitchell P, Ciullo M, Kim SK, Vollenweider P, Raitakari O, Metspalu A, Palmer C, Gasparini P, Pirastu M, Jukema JW, Probst-Hensch NM, Kronenberg F, Toniolo D, Gudnason V, Shuldiner AR, Coresh J, Schmidt R, Ferrucci L, Siscovick DS, van Duijn CM, Borecki I, Kardia SL, Liu Y, Curhan GC, Rudan I, Gyllensten U, Wilson JF, Franke A, Pramstaller PP, Rettig R, Prokopenko I, Witteman JC, Hayward C, Ridker P, Parsa A, Bochud M, Heid IM, Goessling W, Chasman DI, Kao WH, Fox CS, CARDIoGRAM Consortium. ICBP Consortium. CARe Consortium. Wellcome Trust Case Control Consortium 2 (WTCCC2) : Genome-wide association and functional follow-up reveals new loci for kidney function. PLoS Genet 8: e1002584, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pattaro C, De Grandi A, Vitart V, Hayward C, Franke A, Aulchenko YS, Johansson A, Wild SH, Melville SA, Isaacs A, Polasek O, Ellinghaus D, Kolcic I, Nöthlings U, Zgaga L, Zemunik T, Gnewuch C, Schreiber S, Campbell S, Hastie N, Boban M, Meitinger T, Oostra BA, Riegler P, Minelli C, Wright AF, Campbell H, van Duijn CM, Gyllensten U, Wilson JF, Krawczak M, Rudan I, Pramstaller PP, EUROSPAN consortium : A meta-analysis of genome-wide data from five European isolates reveals an association of COL22A1, SYT1, and GABRR2 with serum creatinine level. BMC Med Genet 11: 41, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Köttgen A, Pattaro C, Böger CA, Fuchsberger C, Olden M, Glazer NL, Parsa A, Gao X, Yang Q, Smith AV, O’Connell JR, Li M, Schmidt H, Tanaka T, Isaacs A, Ketkar S, Hwang SJ, Johnson AD, Dehghan A, Teumer A, Paré G, Atkinson EJ, Zeller T, Lohman K, Cornelis MC, Probst-Hensch NM, Kronenberg F, Tönjes A, Hayward C, Aspelund T, Eiriksdottir G, Launer LJ, Harris TB, Rampersaud E, Mitchell BD, Arking DE, Boerwinkle E, Struchalin M, Cavalieri M, Singleton A, Giallauria F, Metter J, de Boer IH, Haritunians T, Lumley T, Siscovick D, Psaty BM, Zillikens MC, Oostra BA, Feitosa M, Province M, de Andrade M, Turner ST, Schillert A, Ziegler A, Wild PS, Schnabel RB, Wilde S, Munzel TF, Leak TS, Illig T, Klopp N, Meisinger C, Wichmann HE, Koenig W, Zgaga L, Zemunik T, Kolcic I, Minelli C, Hu FB, Johansson A, Igl W, Zaboli G, Wild SH, Wright AF, Campbell H, Ellinghaus D, Schreiber S, Aulchenko YS, Felix JF, Rivadeneira F, Uitterlinden AG, Hofman A, Imboden M, Nitsch D, Brandstätter A, Kollerits B, Kedenko L, Mägi R, Stumvoll M, Kovacs P, Boban M, Campbell S, Endlich K, Völzke H, Kroemer HK, Nauck M, Völker U, Polasek O, Vitart V, Badola S, Parker AN, Ridker PM, Kardia SL, Blankenberg S, Liu Y, Curhan GC, Franke A, Rochat T, Paulweber B, Prokopenko I, Wang W, Gudnason V, Shuldiner AR, Coresh J, Schmidt R, Ferrucci L, Shlipak MG, van Duijn CM, Borecki I, Krämer BK, Rudan I, Gyllensten U, Wilson JF, Witteman JC, Pramstaller PP, Rettig R, Hastie N, Chasman DI, Kao WH, Heid IM, Fox CS: New loci associated with kidney function and chronic kidney disease. Nat Genet 42: 376–384, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Köttgen A, Glazer NL, Dehghan A, Hwang SJ, Katz R, Li M, Yang Q, Gudnason V, Launer LJ, Harris TB, Smith AV, Arking DE, Astor BC, Boerwinkle E, Ehret GB, Ruczinski I, Scharpf RB, Chen YD, de Boer IH, Haritunians T, Lumley T, Sarnak M, Siscovick D, Benjamin EJ, Levy D, Upadhyay A, Aulchenko YS, Hofman A, Rivadeneira F, Uitterlinden AG, van Duijn CM, Chasman DI, Paré G, Ridker PM, Kao WH, Witteman JC, Coresh J, Shlipak MG, Fox CS: Multiple loci associated with indices of renal function and chronic kidney disease. Nat Genet 41: 712–717, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chambers JC, Zhang W, Lord GM, van der Harst P, Lawlor DA, Sehmi JS, Gale DP, Wass MN, Ahmadi KR, Bakker SJ, Beckmann J, Bilo HJ, Bochud M, Brown MJ, Caulfield MJ, Connell JM, Cook HT, Cotlarciuc I, Davey Smith G, de Silva R, Deng G, Devuyst O, Dikkeschei LD, Dimkovic N, Dockrell M, Dominiczak A, Ebrahim S, Eggermann T, Farrall M, Ferrucci L, Floege J, Forouhi NG, Gansevoort RT, Han X, Hedblad B, Homan van der Heide JJ, Hepkema BG, Hernandez-Fuentes M, Hypponen E, Johnson T, de Jong PE, Kleefstra N, Lagou V, Lapsley M, Li Y, Loos RJ, Luan J, Luttropp K, Maréchal C, Melander O, Munroe PB, Nordfors L, Parsa A, Peltonen L, Penninx BW, Perucha E, Pouta A, Prokopenko I, Roderick PJ, Ruokonen A, Samani NJ, Sanna S, Schalling M, Schlessinger D, Schlieper G, Seelen MA, Shuldiner AR, Sjögren M, Smit JH, Snieder H, Soranzo N, Spector TD, Stenvinkel P, Sternberg MJ, Swaminathan R, Tanaka T, Ubink-Veltmaat LJ, Uda M, Vollenweider P, Wallace C, Waterworth D, Zerres K, Waeber G, Wareham NJ, Maxwell PH, McCarthy MI, Jarvelin MR, Mooser V, Abecasis GR, Lightstone L, Scott J, Navis G, Elliott P, Kooner JS: Genetic loci influencing kidney function and chronic kidney disease. Nat Genet 42: 373–375, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Böger CA, Gorski M, Li M, Hoffmann MM, Huang C, Yang Q, Teumer A, Krane V, O’Seaghdha CM, Kutalik Z, Wichmann HE, Haak T, Boes E, Coassin S, Coresh J, Kollerits B, Haun M, Paulweber B, Köttgen A, Li G, Shlipak MG, Powe N, Hwang SJ, Dehghan A, Rivadeneira F, Uitterlinden A, Hofman A, Beckmann JS, Krämer BK, Witteman J, Bochud M, Siscovick D, Rettig R, Kronenberg F, Wanner C, Thadhani RI, Heid IM, Fox CS, Kao WH, CKDGen Consortium : Association of eGFR-related loci identified by GWAS with incident CKD and ESRD. PLoS Genet 7: e1002292, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Böger CA, Chen MH, Tin A, Olden M, Köttgen A, de Boer IH, Fuchsberger C, O’Seaghdha CM, Pattaro C, Teumer A, Liu CT, Glazer NL, Li M, O’Connell JR, Tanaka T, Peralta CA, Kutalik Z, Luan J, Zhao JH, Hwang SJ, Akylbekova E, Kramer H, van der Harst P, Smith AV, Lohman K, de Andrade M, Hayward C, Kollerits B, Tönjes A, Aspelund T, Ingelsson E, Eiriksdottir G, Launer LJ, Harris TB, Shuldiner AR, Mitchell BD, Arking DE, Franceschini N, Boerwinkle E, Egan J, Hernandez D, Reilly M, Townsend RR, Lumley T, Siscovick DS, Psaty BM, Kestenbaum B, Haritunians T, Bergmann S, Vollenweider P, Waeber G, Mooser V, Waterworth D, Johnson AD, Florez JC, Meigs JB, Lu X, Turner ST, Atkinson EJ, Leak TS, Aasarød K, Skorpen F, Syvänen AC, Illig T, Baumert J, Koenig W, Krämer BK, Devuyst O, Mychaleckyj JC, Minelli C, Bakker SJ, Kedenko L, Paulweber B, Coassin S, Endlich K, Kroemer HK, Biffar R, Stracke S, Völzke H, Stumvoll M, Mägi R, Campbell H, Vitart V, Hastie ND, Gudnason V, Kardia SL, Liu Y, Polasek O, Curhan G, Kronenberg F, Prokopenko I, Rudan I, Arnlöv J, Hallan S, Navis G, Parsa A, Ferrucci L, Coresh J, Shlipak MG, Bull SB, Paterson NJ, Wichmann HE, Wareham NJ, Loos RJ, Rotter JI, Pramstaller PP, Cupples LA, Beckmann JS, Yang Q, Heid IM, Rettig R, Dreisbach AW, Bochud M, Fox CS, Kao WH, CKDGen Consortium : CUBN is a gene locus for albuminuria. J Am Soc Nephrol 22: 555–570, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reznichenko A, Böger CA, Snieder H, van den Born J, de Borst MH, Damman J, van Dijk MC, van Goor H, Hepkema BG, Hillebrands JL, Leuvenink HG, Niesing J, Bakker SJ, Seelen M, Navis G, REGaTTA (REnal GeneTics TrAnsplantation) Groningen group : UMOD as a susceptibility gene for end-stage renal disease. BMC Med Genet 13: 78, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gudbjartsson DF, Holm H, Indridason OS, Thorleifsson G, Edvardsson V, Sulem P, de Vegt F, d’Ancona FC, den Heijer M, Wetzels JF, Franzson L, Rafnar T, Kristjansson K, Bjornsdottir US, Eyjolfsson GI, Kiemeney LA, Kong A, Palsson R, Thorsteinsdottir U, Stefansson K: Association of variants at UMOD with chronic kidney disease and kidney stones-role of age and comorbid diseases. PLoS Genet 6: e1001039, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tobin MD, Tomaszewski M, Braund PS, Hajat C, Raleigh SM, Palmer TM, Caulfield M, Burton PR, Samani NJ: Common variants in genes underlying monogenic hypertension and hypotension and blood pressure in the general population. Hypertension 51: 1658–1664, 2008 [DOI] [PubMed] [Google Scholar]
- 25.Teslovich TM, Musunuru K, Smith AV, Edmondson AC, Stylianou IM, Koseki M, Pirruccello JP, Ripatti S, Chasman DI, Willer CJ, Johansen CT, Fouchier SW, Isaacs A, Peloso GM, Barbalic M, Ricketts SL, Bis JC, Aulchenko YS, Thorleifsson G, Feitosa MF, Chambers J, Orho-Melander M, Melander O, Johnson T, Li X, Guo X, Li M, Shin Cho Y, Jin Go M, Jin Kim Y, Lee JY, Park T, Kim K, Sim X, Twee-Hee Ong R, Croteau-Chonka DC, Lange LA, Smith JD, Song K, Hua Zhao J, Yuan X, Luan J, Lamina C, Ziegler A, Zhang W, Zee RY, Wright AF, Witteman JC, Wilson JF, Willemsen G, Wichmann HE, Whitfield JB, Waterworth DM, Wareham NJ, Waeber G, Vollenweider P, Voight BF, Vitart V, Uitterlinden AG, Uda M, Tuomilehto J, Thompson JR, Tanaka T, Surakka I, Stringham HM, Spector TD, Soranzo N, Smit JH, Sinisalo J, Silander K, Sijbrands EJ, Scuteri A, Scott J, Schlessinger D, Sanna S, Salomaa V, Saharinen J, Sabatti C, Ruokonen A, Rudan I, Rose LM, Roberts R, Rieder M, Psaty BM, Pramstaller PP, Pichler I, Perola M, Penninx BW, Pedersen NL, Pattaro C, Parker AN, Pare G, Oostra BA, O’Donnell CJ, Nieminen MS, Nickerson DA, Montgomery GW, Meitinger T, McPherson R, McCarthy MI, McArdle W, Masson D, Martin NG, Marroni F, Mangino M, Magnusson PK, Lucas G, Luben R, Loos RJ, Lokki ML, Lettre G, Langenberg C, Launer LJ, Lakatta EG, Laaksonen R, Kyvik KO, Kronenberg F, König IR, Khaw KT, Kaprio J, Kaplan LM, Johansson A, Jarvelin MR, Janssens AC, Ingelsson E, Igl W, Kees Hovingh G, Hottenga JJ, Hofman A, Hicks AA, Hengstenberg C, Heid IM, Hayward C, Havulinna AS, Hastie ND, Harris TB, Haritunians T, Hall AS, Gyllensten U, Guiducci C, Groop LC, Gonzalez E, Gieger C, Freimer NB, Ferrucci L, Erdmann J, Elliott P, Ejebe KG, Döring A, Dominiczak AF, Demissie S, Deloukas P, de Geus EJ, de Faire U, Crawford G, Collins FS, Chen YD, Caulfield MJ, Campbell H, Burtt NP, Bonnycastle LL, Boomsma DI, Boekholdt SM, Bergman RN, Barroso I, Bandinelli S, Ballantyne CM, Assimes TL, Quertermous T, Altshuler D, Seielstad M, Wong TY, Tai ES, Feranil AB, Kuzawa CW, Adair LS, Taylor HA, Jr, Borecki IB, Gabriel SB, Wilson JG, Holm H, Thorsteinsdottir U, Gudnason V, Krauss RM, Mohlke KL, Ordovas JM, Munroe PB, Kooner JS, Tall AR, Hegele RA, Kastelein JJ, Schadt EE, Rotter JI, Boerwinkle E, Strachan DP, Mooser V, Stefansson K, Reilly MP, Samani NJ, Schunkert H, Cupples LA, Sandhu MS, Ridker PM, Rader DJ, van Duijn CM, Peltonen L, Abecasis GR, Boehnke M, Kathiresan S: Biological, clinical and population relevance of 95 loci for blood lipids. Nature 466: 707–713, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tryggvason K, Patrakka J, Wartiovaara J: Hereditary proteinuria syndromes and mechanisms of proteinuria. N Engl J Med 354: 1387–1401, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Hildebrandt F: Genetic kidney diseases. Lancet 375: 1287–1295, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fox C: CKDGen meta-analysis data. Available from: http://www.nhlbi.nih.gov/research/intramural/researchers/pi/fox-caroline/ckdgen-meta-analysis-data/ckdgen-meta-analysis-data.html Updated April 26, 2013. Accessed August 14, 2013.
- 29.Conneely KN, Boehnke M: Meta-analysis of genetic association studies and adjustment for multiple testing of correlated SNPs and traits. Genet Epidemiol 34: 739–746, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Conneely KN, Boehnke M: So many correlated tests, so little time! Rapid adjustment of P values for multiple correlated tests. Am J Hum Genet 81: 1158–1168, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chasman DI, Fuchsberger C, Pattaro C, Teumer A, Böger CA, Endlich K, Olden M, Chen MH, Tin A, Taliun D, Li M, Gao X, Gorski M, Yang Q, Hundertmark C, Foster MC, O’Seaghdha CM, Glazer N, Isaacs A, Liu CT, Smith AV, O’Connell JR, Struchalin M, Tanaka T, Li G, Johnson AD, Gierman HJ, Feitosa MF, Hwang SJ, Atkinson EJ, Lohman K, Cornelis MC, Johansson A, Tönjes A, Dehghan A, Lambert JC, Holliday EG, Sorice R, Kutalik Z, Lehtimäki T, Esko T, Deshmukh H, Ulivi S, Chu AY, Murgia F, Trompet S, Imboden M, Coassin S, Pistis G, Harris TB, Launer LJ, Aspelund T, Eiriksdottir G, Mitchell BD, Boerwinkle E, Schmidt H, Cavalieri M, Rao M, Hu F, Demirkan A, Oostra BA, de Andrade M, Turner ST, Ding J, Andrews JS, Freedman BI, Giulianini F, Koenig W, Illig T, Meisinger C, Gieger C, Zgaga L, Zemunik T, Boban M, Minelli C, Wheeler HE, Igl W, Zaboli G, Wild SH, Wright AF, Campbell H, Ellinghaus D, Nöthlings U, Jacobs G, Biffar R, Ernst F, Homuth G, Kroemer HK, Nauck M, Stracke S, Völker U, Völzke H, Kovacs P, Stumvoll M, Mägi R, Hofman A, Uitterlinden AG, Rivadeneira F, Aulchenko YS, Polasek O, Hastie N, Vitart V, Helmer C, Wang JJ, Stengel B, Ruggiero D, Bergmann S, Kähönen M, Viikari J, Nikopensius T, Province M, Ketkar S, Colhoun H, Doney A, Robino A, Krämer BK, Portas L, Ford I, Buckley BM, Adam M, Thun GA, Paulweber B, Haun M, Sala C, Mitchell P, Ciullo M, Kim SK, Vollenweider P, Raitakari O, Metspalu A, Palmer C, Gasparini P, Pirastu M, Jukema JW, Probst-Hensch NM, Kronenberg F, Toniolo D, Gudnason V, Shuldiner AR, Coresh J, Schmidt R, Ferrucci L, Siscovick DS, van Duijn CM, Borecki IB, Kardia SL, Liu Y, Curhan GC, Rudan I, Gyllensten U, Wilson JF, Franke A, Pramstaller PP, Rettig R, Prokopenko I, Witteman J, Hayward C, Ridker PM, Parsa A, Bochud M, Heid IM, Kao WH, Fox CS, Köttgen A, CARDIoGRAM Consortium. ICBP Consortium. CARe Consortium. WTCCC2 : Integration of genome-wide association studies with biological knowledge identifies six novel genes related to kidney function. Hum Mol Genet 21: 5329–5343, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The 1000 Genomes Project. Available at: http://www.1000genomes.org Accessed August 14, 2013
- 33.Willer CJ, Li Y, Abecasis GR: METAL: Fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26: 2190–2191, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]