Abstract
Background
Current health care reform efforts are focused on reorganizing health care systems to reduce waste in the US health care system.
Objective
To compare rates of overuse in different health care systems and examine whether certain systems of care or insurers have lower rates of overuse of health care services.
Data Sources
Articles published in MEDLINE between 1978, the year of publication of the first framework to measure quality, and June 21, 2012.
Study Selection
Included studies compared rates of overuse of procedures, diagnostic tests or medications in at least two systems of care.
Data Extraction
Four reviewers screened titles; 2 reviewers screened abstracts and full articles and extracted data
Results
We identified 7 studies which compared rates of overuse of 5 services across multiple different health care settings. National rates of inappropriate coronary angiography were similar in Medicare HMOs and Medicare FFS (13% vs. 13%, p=0.33) and in a state based study comparing 15 hospitals in NY and 4 hospitals in a Massachusetts managed care plan (4% vs. 6%, p>0.1). Rates of carotid endarterectomy in NY State were similar in Medicare HMOs and Medicare FFS plans (8.4% vs. 8.6%, p=0.55) but non-recommended use of antibiotics for the treatment of upper respiratory infection was higher in a managed care organization than a FFS private plan (31% vs. 21%, p=0.02). Rates of inappropriate myocardial perfusion imaging were similar in VA and private settings (22% vs. 16.6%, p=0.24), but rates of inappropriate surveillance endoscopy in the management of gastric ulcers were higher in the VA compared to private settings (37.4% vs. 20.4 to 23.3%, p<0.0001).
Conclusions
The available evidence is limited but there is no consistent evidence that any one system of care has been more effective at minimizing the overuse of health care services. More research is necessary to inform current health care reform efforts directed at reducing overuse.
Introduction
Misaligned incentives and a fee for service payment system are thought to be important drivers of the high utilization of health care services in the US.1-2 Rising health care costs have focused attention on reducing health care waste.3 Overuse, the use of health services with no benefit or for which harms outweigh benefits, is thought to contribute to the high cost of care accounting for up to $226 billion in wasteful spending in 2011.4 Reducing overuse of health care services is a compelling strategy to reduce costs without detracting from the quality of care.5
There is evidence that health care costs and utilization are lower in managed care compared to fee-for-service (FFS) systems,6-10 but the effect of managed care or health care systems for which physicians are salaried on the overuse of health care services is less evident. We conducted a systematic review and collected information on the overuse of health care services in different health care systems and among different coverage types in the US to improve our understanding of whether particular systems of care or insurers have had more success in minimizing overuse of health care services compared to the FFS sector. These findings may be informative to policymakers who are seeking to improve both the quality and efficiency of health care.
Methods
We performed a systematic review of the overuse of procedures, surgeries, diagnostic tests or medications in the United States. We used the PRISMA statement on systematic reviews to guide the methods.11
Data Sources and Search Strategy
We identified studies by searching Medline for articles published between January 1, 1978 and January 1, 2009. We chose a 1978 start date because the first framework to measure quality was published that year.12 The search string is available in the appendix (supplemental digital content). Because there is no specific Medical Subject Heading (MeSH) term for overuse, we used an iterative process to identify MeSH terms. A description of the search is available elsewhere.13 Table 1 lists the terms utilized in the Medline search. One of 4 investigators screened all titles and 1 of 2 investigators (SK and DK) screened abstracts for possible inclusion in the review. A random sample of 100 abstracts was reviewed by both investigators for determination of inter-rater reliability. The same two investigators reviewed all full text articles. Each article was reviewed by 1 investigator with discussion when necessary. We again measured inter-rater reliability on 40 randomly selected articles for the decision to include in the review. We examined reference lists of identified articles and reviewed all publications of every first and last author and any author appearing more than twice in any position in our final pool of articles, and consulted two experts in the field for additional references we may have missed. Cross-referencing was performed once.
Table 1.
Terms Used in Search Strategy
| Medical Subject Headings |
|---|
| Guidelines as Topic |
| Physician’s Practice Patterns |
| Utilization Review |
| Clinical Audit |
| Guideline Adherence |
| Health Services Misuse |
| Small Area Analysis |
| Delphi Technique |
| Diagnostic Techniques/Procedures |
| Laboratory Techniques/Procedures |
| Prescriptions, Drug And Utilization |
| Procedures And Utilization |
| Surgery And Utilization |
| Non-Medical Subject Headings |
| Overuse |
| Appropriateness |
| Inappropriate Procedure |
| Inappropriate Surgery |
| Inappropriate Test |
| Inappropriate Utilization |
| Inappropriate Medication |
Study Selection
Articles were eligible for inclusion if they were original research utilizing an acceptable standard. Acceptable standards included 1) a guideline generated through a multidisciplinary iterative panel process involving a literature review, 2) a guideline from a regional or national organization, or 3) a universally accepted standard of care (e.g. antibiotics are not indicated for the treatment of viral respiratory infections). Studies were excluded if the standards were generated solely by the consensus of the study authors or a local single-discipline panel, or if the supporting literature review was not described. We excluded poor quality studies which we defined as those using potentially biased (non-random, non-consecutive, or not clearly defined) or nongeneralizable (e.g. a sample from one physician’s panel) patient populations, and those with sample size <50 individuals. Given the diverse methodologies there is no appropriate method for quality assessment, so we performed a qualitative assessment of the included studies.
Data Extraction
We developed a data extraction tool to collect information from each study in the original review.13 The purpose of the original review was to develop a better understanding of overuse of healthcare services which could inform efforts to reduce inappropriate care.13 We performed an extensive search for studies of overuse of procedures, diagnostic tests and medications and described the state of the literature. For this sub study, we looked for abstracted rates of overuse across different settings if reported. If rates were not directly reported (e.g. shown in figures) they were calculated using all available data from the publications and averaged among three investigators (SK, DK, and RF). Papers which included data on insurance type or setting but did not specifically report overuse rates within these categories were excluded. Papers which did not give specific information on insurance types (HMO vs. FFS) were also excluded.
Updated Search
Given the depth of our original analysis13, we were not able to include the most recent literature in our main search. To find more recent papers, 2 investigators (SK and DK) performed a targeted search using combinations of the following terms: inappropriate medication, inappropriate procedure, inappropriate test, inappropriate and Medicare, inappropriate and Medicaid, inappropriate and VA, inappropriate and managed care, limited to studies in English, clinical trials, and publication date after 1/1/2009 ending on 6/21/2012. We reviewed an additional 3082 titles in this targeted search, through which we identified 1 additional article meeting inclusion criteria.
Analysis
Given the diversity of the literature, we did not pool data in the review. Inter-rater reliability for both the abstract selection (Cohen’s kappa=0.93) and the decision to include the article in the review (Cohen’s kappa=0.85) was excellent.
Results
Our search yielded 114,831 articles, of which 112,467 were excluded in title review and 172 were included in the final sample of articles (Figure 1). We identified six articles that compared rates of overuse across settings and/or insurers from this original search. We identified one additional article in the updated search for a total of seven papers that met inclusion criteria. Six of the seven studies used the most reliable methods for determining overuse and were considered high quality. The other study used “generally acceptable care” as a standard and may have misclassified some cases and was considered to be of moderate quality. Overall these articles examined rates of overuse of 3 procedures, 1 diagnostic test and 1 medication.
Figure 1.
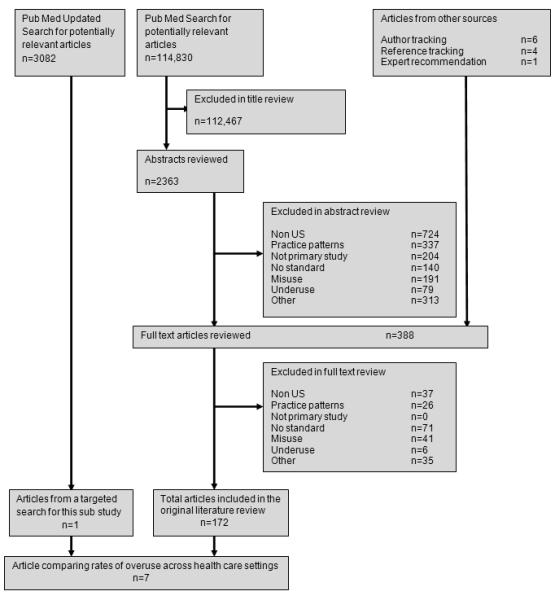
Flow of articles in the review
Rates of Overuse across Managed Care and the FFS Sector
There were limited differences in rates of overuse across different insurers or systems of care for most services (Table 2). There were similar rates of inappropriate coronary angiography (CA) in 15 hospitals in New York and 4 hospitals (staff model and group model) in a managed care organization in Massachusetts (4% vs. 6%, p>0.1).14 There were similar rates of CA nationally in Medicare HMOs and Medicare FFS (13% vs. 13%, p=0.33).15 Rates of overuse of carotid endarterectomy in New York State were similar in Medicare HMOs and Medicare FFS (8.4% vs. 8.6%, p=0.55).16 Rates of overuse of antibiotics for the treatment of upper respiratory infection were higher in a staff model managed care organization than a FFS private plan (31% vs. 21%, P=0.02), similar for acute bronchitis (82% vs. 73%, p=0.11) while overuse of other diagnostic services (e.g. chest x-ray, throat cultures and spirometry) for URI (1% vs.18%, p=0.001) and acute bronchitis were lower in managed care (4% vs.21%, p=0.001). 17
Table 2.
Comparison of Rates of Overuse by System of Care or Insurer†
| Citation | Year | Treatment | Population | Definition of inappropriate care |
Coverage Type and/or Setting |
|
|---|---|---|---|---|---|---|
|
Fee for
Service |
Managed
Care |
|||||
| Halm | 2008 | Carotid Endarterectomy for all indications |
Data was taken from the New York Carotid Artery Study which includes 9761 Medicare beneficiaries in New York State. |
Inappropriate** |
8.6% |
8.4% |
| Guadagnoli | 2000 | Coronary angiography for Acute Myocardial Infarction |
Data for 46,321 patients was taken from the Cooperative Cardiovascular Project and was based on Medicare patients hospitalized in Florida, Texas, California, Ohio, Pennsylvania, New York, and Massachusetts. |
Unlikely to be effective** |
13% |
13% |
| Hueston | 1997 | Antibiotics for URI Use of Diagnostic Tests |
Data on 552 patients was drawn from two organizations; 1) A staff model HMO with over 15,000 members including Medicaid patients, and2) a multispecialty clinic with a large fee for service population . |
Non-recommended antibiotics for URI* Non-recommended antibiotics for acute bronchitis** Non-recommended diagnostic tests for URI* Non-recommended diagnostic tests for acute bronchitis* |
20% 82% 18% 21% |
31% 73% 1% 4% |
| Noonan | 1995 | Coronary Angiography—for all indications |
Data on 292 patients was taken from 4 hospitals from the Harvard Community Health Plan in Massachusetts and patients from 15 hospitals in New York State. |
Inappropriate** | 4% | 6% |
| VA | Non-VA | |||||
| Nelson | 2011 | Radionuclide Myocardial Perfusion Imaging |
Data collected from 300 patients visiting the Miami VA Medical center or the university of Miami |
Inappropriate** |
22% | 16.6% |
| Gonzales | 2006 | Antibiotics for Acute Respiratory Tract Infections |
Data was collected on 2270 patients visiting emergency departments in VA and community settings. |
Inappropriate+ | 57-92% | 43-92% |
| Saini | 2005 | Surveillance Endoscopy |
Data on a sample of 1510 patients across the country was taken from the national Clinical Outcomes Research Initiative database. |
Non-recommended* | 37.4% | 20-23.3% |
P<0.05
p-value not significant
Adjusted rates estimated from figures, p-value not reported
All studies were retrospective cohort studies or cross-sectional studies.
Rates of Overuse across the VA and Non-VA Settings
Three articles compared rates of overuse of health care services in the VA compared to other settings.18-20 One paper focused on antibiotic use for acute respiratory tract infections in 7 VA vs. non-VA emergency departments across 7 cities, another examined inappropriate surveillance upper endoscopy for gastric ulcer management, and the third paper compared rates of inappropriate radionuclide myocardial perfusion imaging. Rates of overuse of antibiotics were similar across four VA and non-VA emergency rooms in 4 cities, but rates were higher in 3 VA compared to non-VA emergency departments.18 Rates of inappropriate use of surveillance upper endoscopy were higher in the VA compared to non-VA settings (37.4% vs. 23.3-20.4%, p<0.0001).20 Rates of myocardial perfusion imaging (22% vs. 16.6%, p=0.24) were similar in the VA and private settings19 (Table 2).
Discussion
Past research13 has demonstrated that overuse of health care services is present in all insurance types and settings in the US including Medicare FFS21, Medicaid22, VA23, and in staff and group Model HMOs.24-25 However, the limited literature that compares overuse across settings does not provide consistent evidence to support the notion that any one system of care or insurer has been more effective at minimizing the overuse of health care services.
Both managed care and the VA have a financial incentive to reduce unnecessary care. Managed care organizations have a profit motive to limit costs and in the case of the VA, resources could be better directed to other needed areas for the care of veterans. There may be several explanations for this lack of evidence of lower rates of overuse in these two systems compared to the FFS sector. Examining the appropriateness of care across settings is challenging and requires resources and therefore the literature is limited. Further, few studies included physicians practicing exclusively within a given payment structure; since the behavior of a physician is likely to be consistent across practice settings, studies comparing practice in non-overlapping settings may be more informative.
On the other hand it is possible that since health systems have not focused on limiting overuse, rates of overuse are similar across settings. Studies on the delivery of preventive care and the management of chronic diseases have demonstrated that managed care and the VA have less underuse of specific needed therapies compared to the private FFS system. 26-30 However, this superior performance is defined by specific quality metrics which were the result of the quality improvement movement and the development of national performance measures.28-30 While in recent years there has been greater focus on overuse by groups such as the National Quality Forum and the National Priorities Partnership,31 this attention has not translated into tangible investment in overuse measures. For example, among the 42 Effectiveness of Care performance metrics in the 2012 Health care Effectiveness Data and Information Set (HEDIS), four are overuse measures of which two pertain to adults.32 Among the 33 proposed measures for Accountable Care Organizations (ACOs)33, none pertains to overuse despite an evidence base available to inform the development of such measures.34 Systems such as the VA and managed care are well structured to incorporate performance measures to reduce the underuse of preventive care and improve chronic disease management. These health care systems could also support efforts directed at reducing overuse if performance measures were developed and if national reporting of these measures created an incentive to decrease rates of overuse. The relative similarity in rates of overuse across settings we identified may be partly due to the lack of national focus on this quality problem.
Limitations
This study has a number of limitations. There is no standardized MeSH search terminology for overuse. We attempted to address this through an iterative process to include as many articles as possible, and through reference tracking and author tracking. In addition, the large number of abstracts and articles for review precluded 2 reviewers examining each, which may have lead to errors or lack of reproducibility. However our high inter-rater reliability for a randomly selected sub-set of abstracts and full text articles suggests methodological consistency. We excluded articles without a generally accepted standard to define appropriate care, including articles in which a few authors reviewed the literature and developed guidelines for practice. Since members of formal expert panels often disagree when defining inappropriate care35, definitions of appropriate care by a few like-minded individuals may be biased. Finally, since the scope of our article selection process precluded repeating the full search, we performed a less complete updated search. However, it is unlikely we missed any major recent publications.
In conclusion, the evidence examining rates of overuse of services in different systems of care is limited, but does not suggest that one system of care is more effective at minimizing overuse. More research is clearly needed to better inform health care reform efforts directly at eliminating overuse in the US health care system.
Supplementary Material
Acknowledgments
Funding: This project was supported by the Commonwealth Fund. Dr. Keyhani is also supported by a VA HSR&D Career Development Award.
Footnotes
Financial Disclosures: None reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Coller BS. Realigning Incentives to Achieve Health Care Reform. JAMA: the journal of the American Medical Association. 306:204. doi: 10.1001/jama.2011.978. [DOI] [PubMed] [Google Scholar]
- 2.Wallack SS, Tompkins CP. Realigning incentives in fee-for-service Medicare. Health Affairs. 2003;22:59–70. doi: 10.1377/hlthaff.22.4.59. [DOI] [PubMed] [Google Scholar]
- 3.Pear R. Health Care Spending Disparities Stir a Fight. The New York Times. 2009 Jun 8; [Google Scholar]
- 4.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307:1513–6. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 5.Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280:1000–5. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- 6.Miller RH, Luft HS. Managed care plan performance since 1980. A literature analysis. JAMA. 1994;271:1512–9. [PubMed] [Google Scholar]
- 7.Cher DJ, Lenert LA. Method of Medicare reimbursement and the rate of potentially ineffective care of critically ill patients. JAMA. 1997;278:1001–7. [PubMed] [Google Scholar]
- 8.Bundorf MK, Schulman KA, Stafford JA, Gaskin D, Jollis JG, Escarce JJ. Impact of managed care on the treatment, costs, and outcomes of fee-for-service Medicare patients with acute myocardial infarction. Health Serv Res. 2004;39:131–52. doi: 10.1111/j.1475-6773.2004.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heidenreich PA, McClellan M, Frances C, Baker LC. The relation between managed care market share and the treatment of elderly fee-for-service patients with myocardial infarction. Am J Med. 2002;112:176–82. doi: 10.1016/s0002-9343(01)01098-1. [DOI] [PubMed] [Google Scholar]
- 10.Baker LC. Association of managed care market share and health expenditures for fee-for-service Medicare patients. JAMA. 1999;281:432–7. doi: 10.1001/jama.281.5.432. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 12.Donabedian A. The quality of medical care. Science. 1978;200:856–64. doi: 10.1126/science.417400. [DOI] [PubMed] [Google Scholar]
- 13.Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172:171–8. doi: 10.1001/archinternmed.2011.772. [DOI] [PubMed] [Google Scholar]
- 14.Noonan SJ, Cook JL, Keller CE, et al. Relationship of anatomic disease to appropriateness ratings of coronary angiography. Arch Intern Med. 1995;155:1209–13. [PubMed] [Google Scholar]
- 15.Guadagnoli E, Landrum MB, Peterson EA, Gahart MT, Ryan TJ, McNeil BJ. Appropriateness of coronary angiography after myocardial infarction among Medicare beneficiaries—managed care versus fee for service. New England Journal of Medicine. 2000;343:1460–6. doi: 10.1056/NEJM200011163432006. [DOI] [PubMed] [Google Scholar]
- 16.Halm EA, Press MJ, Tuhrim S, Wang J, Rojas M, Chassin MR. Does managed care affect quality? Appropriateness, referral patterns, and outcomes of carotid endarterectomy. Am J Med Qual. 2008;23:448–56. doi: 10.1177/1062860608323926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hueston WJ, Mainous AG, 3rd, Brauer N, Mercuri J. Evaluation and treatment of respiratory infections: does managed care make a difference? J Fam Pract. 1997;44:572–7. [PubMed] [Google Scholar]
- 18.Gonzales R, Camargo CA, Jr., MacKenzie T, et al. Antibiotic treatment of acute respiratory infections in acute care settings. Acad Emerg Med. 2006;13:288–94. doi: 10.1197/j.aem.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 19.Nelson KH, Willens HJ, Hendel RC. Utilization of radionuclide myocardial perfusion imaging in two health care systems: assessment with the 2009 ACCF/ASNC/AHA appropriateness use criteria. J Nucl Cardiol. 2012;19:37–42. doi: 10.1007/s12350-011-9467-8. [DOI] [PubMed] [Google Scholar]
- 20.Saini SD, Eisen G, Mattek N, Schoenfeld P. Utilization of upper endoscopy for surveillance of gastric ulcers in the United States. Am J Gastroenterol. 2008;103:1920–5. doi: 10.1111/j.1572-0241.2008.01945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ko DT, Wang Y, Alter DA, et al. Regional variation in cardiac catheterization appropriateness and baseline risk after acute myocardial infarction. J Am Coll Cardiol. 2008;51:716–23. doi: 10.1016/j.jacc.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 22.Lohr KN, Brook RH. Quality of care in episodes of respiratory illness among Medicaid patients in New Mexico. Annals of Internal Medicine. 1980;92:99. doi: 10.7326/0003-4819-92-1-99. [DOI] [PubMed] [Google Scholar]
- 23.Merrick NJ, Brook RH, Fink A, Solomon DH. Use of carotid endarterectomy in five California Veterans Administration medical centers. JAMA: the journal of the American Medical Association. 1986;256:2531–5. [PubMed] [Google Scholar]
- 24.Noonan SJ, Cook JL, Keller CE, et al. Relationship of anatomic disease to appropriateness ratings of coronary angiography. Archives of internal medicine. 1995;155:1209. [PubMed] [Google Scholar]
- 25.Selby JV, Fireman BH, Lundstrom RJ, et al. Variation among hospitals in coronary-angiography practices and outcomes after myocardial infarction in a large health maintenance organization. New England Journal of Medicine. 1996;335:1888–96. doi: 10.1056/NEJM199612193352506. [DOI] [PubMed] [Google Scholar]
- 26.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:2218–27. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 27.Keyhani S, Ross JS, Hebert P, Dellenbaugh C, Penrod JD, Siu AL. Use of preventive care by elderly male veterans receiving care through the Veterans Health Administration, Medicare fee-for-service, and Medicare HMO plans. American journal of public health. 2007;97:2179. doi: 10.2105/AJPH.2007.114934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landon BE, Zaslavsky AM, Bernard SL, Cioffi MJ, Cleary PD. Comparison of performance of traditional Medicare vs Medicare managed care. JAMA: the journal of the American Medical Association. 2004;291:1744–52. doi: 10.1001/jama.291.14.1744. [DOI] [PubMed] [Google Scholar]
- 29.Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Annals of Internal Medicine. 2004;141:272–81. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 30.Ross JS, Keyhani S, Keenan PS, et al. Use of recommended ambulatory care services: is the Veterans Affairs quality gap narrowing? Arch Intern Med. 2008;168:950–8. doi: 10.1001/archinte.168.9.950. [DOI] [PubMed] [Google Scholar]
- 31.Bauer M, Monz BU, Montejo AL, et al. Prescribing patterns of antidepressants in Europe: results from the Factors Influencing Depression Endpoints Research (FINDER) study. Eur Psychiatry. 2008;23:66–73. doi: 10.1016/j.eurpsy.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 32. [Accessed June 28, 2012];Healthcare Effectiveness Data and Information Set (HEDIS) 2012 Measures. 2012 at http://www.ncqa.org/tabid/1415/Default.aspx.
- 33.Accountable Care Organization 2012 Program Analysis: Final Report Prepared for Quality Measurment and Health Assessment Group. Office of Clinical Standards and Quality. Centers for Medicare &Medicaid Services 2011.
- 34.Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296:2336–42. doi: 10.1001/jama.296.19.2336. [DOI] [PubMed] [Google Scholar]
- 35.Sanmartin C, Murphy K, Choptain N, et al. Appropriateness of healthcare interventions: Concepts and scoping of the published literature. International Journal of Technology Assessment in Health Care. 2008;24:342–9. doi: 10.1017/S0266462308080458. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


