Abstract
Background
Elderly patients are frequently under-triaged. However, the associations between triage patterns and outcomes from a population perspective are unknown. We hypothesized that triage patterns would be associated with differences in outcomes.
Study Design
This is a population-based, retrospective cohort study of all injured adults aged ≥55 years from 3 counties in California and 4 in Utah (2006–2007). Pre-hospital data were linked to trauma registry data, state-level discharge data, emergency department (ED) records, and death files. The primary outcome was 60-day mortality. Patients treated at trauma centers were compared to those treated at non-trauma centers. Under-triage was defined as an injury severity score (ISS)>15 with transport to a non-trauma center.
Results
There were 6,015 patients in the analysis. Patients who were taken to non-trauma centers were on average older (79.4 vs. 70.7 years, p<0.001), more often female (68.6% vs. 50.2%, p<0.01), and less often had an ISS>15 (2.2% vs. 6.7%, p<0.01). The number of patients with an ISS>15 was 244 and the under-triage rate was 32.8% (N=80). Overall 60-day mortality for patients with an ISS>15 was 17%, with no difference between trauma and non-trauma centers in unadjusted or adjusted analyses. However, the median per-patient costs were $21,000 higher for severely injured patients taken to trauma centers.
Conclusions
This is the first population-based analysis of triage patterns and outcomes in the elderly. We have shown high rates of under-triage that are not associated with higher mortality, but are associated with higher costs. Future work should focus on determining how to improve outcomes for this population.
BACKGROUND
Injuries among elderly patients accounted for only 13% of all emergency room visits in 2008, but constituted 45% of all admissions and 62% of all hospital deaths.1 The costs associated with injuries in the elderly are substantial. It is estimated that trauma-related disorders for patients age 65 and older resulted in costs close to $20 billion in 2008. According to the U.S. Census Bureau, the number of U.S. citizens 65 years or older in 2030 is projected to be twice as large as in 2000, growing from 35 million to 72 million and representing nearly 20 percent of the total U.S. population.2
As geriatric injuries are increasing in frequency, there is evidence that care could be improved for these patients.3 Even with minor injuries, there is at least a 2 to 5-fold increase in mortality compared to the young.4,5 Although some of this is likely due to the higher rate of comorbidities in the elderly, it also may be due to the fact that elderly patients with severe injuries are frequently under-triaged.6–8 Age has been shown to be inversely correlated to admission to a trauma center, even when controlling for injury, patient, and geographic factors.6
We hypothesized that there would be high rates of under-triage for severely-injured elderly patients and that triage patterns would be associated with differences in mortality. We used a population-based database in order to determine the current state of triage practice and the associated outcomes. The study included all injured older patients presenting through the 9-1-1 emergency medical systems (EMS) and transported by EMS to acute care hospitals within the study regions to determine the associations between triage patterns, hospital length of stay, mortality, and costs.
METHODS
Study population and data sources
This is a population-based retrospective cohort study involving three counties in California (San Francisco, Santa Clara, and San Mateo Counties) and the state of Utah. We included patients evaluated by the EMS agencies in these counties and state over a 24-month period (January 2006 – December 2007). Data were collected as part of a larger effort, the Western Emergency Services Translational Research Network (WESTRN), which is a consortium of geographic regions, EMS agencies, and hospitals in the Western U.S. that collected data between January 1, 2006 and December 31, 2008. These regions and centers are linked through the National Institutes of Health Clinical and Translational Science Award (CTSA) centers. Each site represents a pre-defined geographic “footprint” consisting of a central metropolitan area and surrounding regions, defined by emergency medical service agency areas. The purpose of the overall WESTRN project was to create a population-based injury database which could be used to study and improve triage criteria. The subsets of data used in the current study include three counties in California and the state of Utah because complete data on 60-day mortality were available for these regions. Methodology for the data linkage is described in detail in previous publications.8–10 Within this dataset, match rates for patients transported to the hospital were greater than 80% and for vital statistics linkage was greater than 88%.10
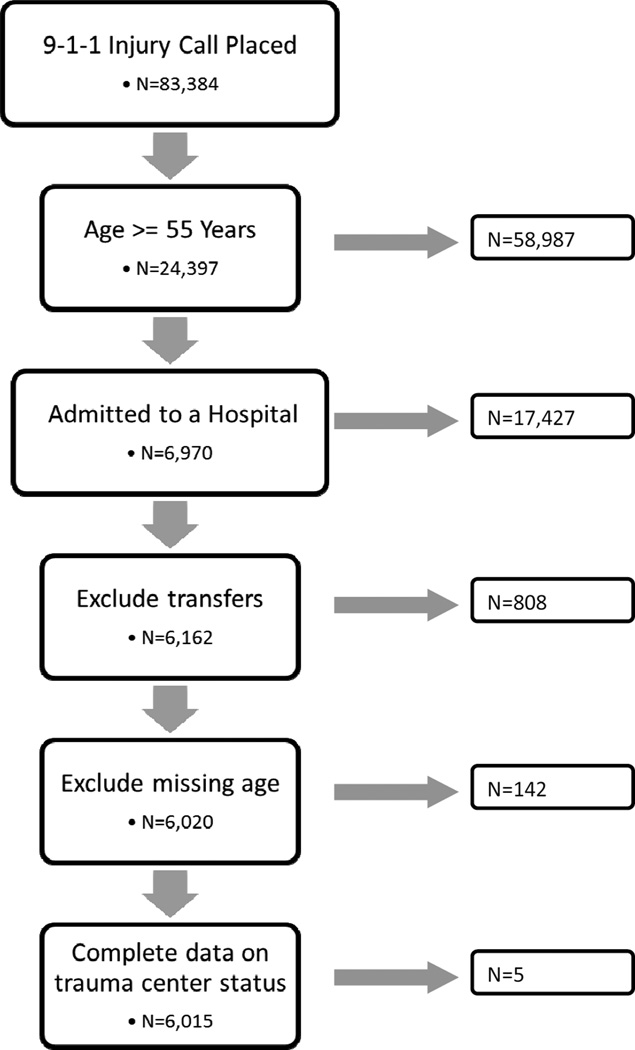
Patients were eligible for the study if they had an injury call placed to 9-1-1, were ≥ 55 years of age, and were admitted to the hospital. (Figure 1) We chose the age of 55 as this age has been noted to be associated with increased mortality rates after trauma.11–13 Patients without data on age were excluded from the analysis. Patients were also excluded if they were transferred between hospitals to avoid being counted twice in the dataset. To ensure that the exclusion of trauma patients did not introduce bias, we repeated analyses with and without the cohort of patients who were transferred.
Figure 1.
Inclusion and exclusion criteria for the study.
Outcomes and Analysis
Patients who were admitted to a Level I or II trauma center were compared to patients admitted to a non-trauma hospital. At the time of the study, there were no Level III or IV centers in the regions studied. The primary outcome was 60-day mortality. This metric was selected rather than in-hospital mortality as the majority of trauma-related deaths in the elderly occur after discharge, with 89% occurring by 60 days.12,14 Mortality data were obtained through linkage to national vital statistics data. Secondary outcomes included in-hospital costs and hospital length of stay. Hospital charges were obtained from state-level administrative databases. In-hospital costs were calculated from facility charges using year- and hospital-specific cost-to-charge ratios. All costs were adjusted to 2008 U.S. dollars using a region-specific medical consumer price index.
Variables included in the analysis include demographics, injury characteristics, pre-hospital physiology, and procedures. Demographic variables included age and sex. Race and ethnicity were not reliably recorded in the hospital and pre-hospital records. Injury characteristics included mechanism of injury (when available) and injury severity score (ISS). Because the ISS is not collected in state discharge or emergency department databases, we used a mapping function (ICDPIC module for Stata v11; StataCorp, College Station, TX) and International Classification of Diseases—9th Revision diagnosis codes to generate injury severity measures.15 Previous studies have validated software for mapping administrative diagnosis codes to anatomic injury scores.16–18 We have also validated the ICDPIC-generated ISS against chart-abstracted ISS in this database.19
Pre-hospital physiology included pre-hospital systolic blood pressure (SBP), heart rate (HR), and Glasgow Coma Score (GCS). Whether the patient had an interventional radiology procedure performed or major, non-orthopedic surgery was also recorded. Under-triage was defined as patients with an ISS>15 who were initially transported to and discharged from a non-trauma center.
Statistical analysis
Statistical analyses were performed using STATA version 10.1 for Windows (StataCorp LP, College Station, TX). Patients treated at trauma vs. non-trauma centers were compared. Categorical data were compared using chi-square tests. Continuous data were compared using Student’s t-test for data satisfying normality assumptions (blood pressure and heart rate) and Wilcoxon rank sum test for all other continuous variables.
Logistic regression and linear regression were used to identify predictors for the outcome measures of 60-day mortality and costs, respectively. Independent variables included in the regressions included demographics (age, sex), injury characteristics (injury severity, mechanism), and the pre-hospital physiology variables listed above. These variables were selected for inclusion in the model as they are recommended as necessary for trauma outcome prediction.20 Information on comorbidities would have been included, but was largely absent from the data. Whether the patient had a procedure was included as another indicator of severity of injury. Trauma center status was included as a covariate in the model. Model discrimination was determined using receiver-operating characteristic (ROC) analysis and calibration using the Hosmer-Lemeshow goodness-of-fit test.
This study received Institutional Review Board approval by all participating trauma centers. Adherence to guidelines on the treatment of human subjects was maintained.
RESULTS
There were a total of 6,015 patients who were ≥55 years of age, had a 9-1-1 call placed for injury, and who were admitted to the hospital. Patients transported to non-trauma centers were different from those taken to trauma centers in all measures. (Table 1) Patients who were taken to non-trauma centers were on average older (79.4 vs. 70.7 years, p<0.001), more often female (68.6% vs. 50.2%, p<0.001), less injured as measured by proportion of patients with an ISS>15 (2.2% vs. 6.7%, p<0.001), and more often injured by a fall mechanism (63.4% vs. 33.9%, p<0.001). Patients who were taken to trauma centers more often had a pre-hospital GCS less than 14 (10.3% vs. 3.2%, p<0.001). There were also significant differences in the mean pre-hospital heart rate between patients taken to non-trauma centers versus trauma centers, but the magnitude of the difference was not large.
Table 1.
Patient Characteristics for all Patients ≥55 Years of Age who Were Injured, Transported and Admitted to a Hospital (January 2006 to December 2007)
| All patients | Non-trauma center | Trauma center | p Value | |
|---|---|---|---|---|
| n (%) | 6,015 | 3,569 (59.3) | 2,446 (40.7) | |
| Demographics | ||||
| Age, y, mean ± SD | 75.9 ± 11.9 | 79.4 (10.8) | 70.7 ± 11.7 | <0.001 |
| Female, n (%) | 3,676 (61.1) | 2,449 (68.8) | 1,227 (50.2) | <0.001 |
| Injury characteristics, n (%) | ||||
| ISS>15 | 244 (4.1) | 80 (2.2) | 164 (6.7) | <0.001 |
| Mechanism type | <0.001 | |||
| Fall | 3,092(51.4) | 2,264 (63.4) | 828 (33.9) | |
| MVC | 791(13.2) | 171 (4.8) | 620 (25.3) | |
| Other | 639(10.6) | 266 (7.5) | 373 (15.2) | |
| Missing | 1,493(24.8) | 868 (24.3) | 625 (25.6) | |
| Blunt mechanism | 4,128(68.6) | 2,479 (69.5) | 1,649 (67.4) | <0.001 |
| Physiology | ||||
| Prehospital SBP, mmHg, mean ±SD | 145.5 ± 28.0 | 145.6 ± 27.6 | 145.2 ± 28.6 | 0.59 |
| Prehospital HR, mean ± SD | 85.2 ± 17.0 | 84.4 ± 16.4 | 86.4 ± 17.6 | <0.001 |
| Prehospital GCS<14, n (%) | 366 (6.1) | 114 (3.2) | 252 (10.3) | <0.001 |
| Procedures, n (%) | ||||
| IR Procedure | 8 (0.1) | 4 (0.1) | 4 (0.2) | <0.001 |
| Nonorthopaedic surgery | 363 (6.0) | 170 (4.8) | 193 (7.9) | <0.001 |
| Outcomes | ||||
| 60-d mortality, n (%) | 460 (7.6) | 320 (9.0) | 140 (5.7) | <0.001 |
| Total costs in dollars, median (IQR) | $12,062 ($5,128–$21,255) | $9,642 ($1,933–$18,252) | $17,875 ($10,644–$32,914) | <0.001 |
| Length of stay, d, median (IQR) | 4.0 (2.0–6.0) | 4.0 (3.0–6.0) | 3.0 (1.0–5.0) | <0.001 |
SD Standard Deviation; ISS Injury Severity Score; SBP Systolic Blood Pressure; HR Heart Rate; GCS Glasgow Coma Score; IR Interventional Radiology; mmHG Millimeter of Mercury; IQR Interquartile range.
There were significant differences in the unadjusted outcomes between patients taken to non-trauma centers versus trauma centers. Non-trauma centers had higher unadjusted 60-day mortality (9.0% vs. 5.7%, p<0.001) and length of stay (median 4.0 days vs. 3.0 days, p<0.001), but lower in-hospital costs (median $9,642 vs. $17,875, p<0.001). Patients who were taken to non-trauma centers also had fewer interventions performed and fewer major non-orthopedic surgeries.
We next evaluated only those patients who had an ISS>15 to determine the rates and outcomes associated with under-triage (defined by having an ISS>15 and treatment at non-trauma centers). (Table 2) Of the 6,105 patients, 244 (4.1%) had an ISS>15. The under-triage rate for this group was 32.8%. If the definition of under-triage was expanded to include patients transported to a non-trauma center who had either an ISS>15 or a procedure (interventional radiology or non-orthopedic surgery), the under-triage rate increased to 44%. Patients with an ISS>15 who were under-triaged were different than those taken to a trauma center. Under-triaged patients were older (mean 71.9 vs. 70.7 years, p<0.001) and more commonly injured by a fall or MVC mechanism versus other mechanisms.
Table 2.
Patient Characteristics for all Patients ≥55 Years of Age who Were Injured, Transported, and Admitted to a Hospital, and who Had an ISS>15 (January 2006 to December 2007)
| All patients with ISS>15 | Non-trauma center | Trauma center | p Value |
|
|---|---|---|---|---|
| n (%) | 244 | 80 (32.8) | 164 (67.2) | |
| Demographics | ||||
| Age, y, mean ± SD | 71.1 ± 11.6 | 71.9 ± 12.0 | 70.7 ± 11.3 | <0.001 |
| Female, n (%) | 89 (36.5) | 27 (33.8) | 62 (37.8) | 0.48 |
| Mechanism | ||||
| Mechanism type, n (%) | 0.04 | |||
| Fall | 74 (30.3) | 29 (36.3) | 45 (27.4) | |
| MVC | 87 (35.7) | 35 (43.8) | 52 (31.7) | |
| Other | 28 (11.5) | 12 (15.0) | 43 (26.2) | |
| Missing | 55 (22.5) | 4 (5.0) | 24 (14.6) | |
| Blunt mechanism, n (%) | 182 (74.6) | 65 (81.3) | 117 (71.3) | 0.10 |
| Physiology | ||||
| Prehospital SBP, mmHg, mean ± SD | 140.1 ± 32.9 | 145.6 ± 27.6 | 145.2 ± 28.6 | 0.59 |
| Prehospital HR, mean ± SD | 86.8 ± 20.0 | 88.6 ± 19.6 | 85.9 ± 20.2 | 0.35 |
| Prehospital GCS<14, n (%) | 61 (25.0) | 20 (25.0) | 41 (25.0) | >0.99 |
| Outcomes | ||||
| 60-d mortality, n (%) | 41 (16.8) | 13 (16.3) | 28 (17.1) | 0.87 |
| Total costs in dollars, median (IQR) | $30,748 ($14,756–$76,670) | $14,332 ($5,112–$29,321) | $35,069 ($19,321–$88,357) | <0.001 |
| Length of stay, d, median (IQR) | 4.0 (2.0–6.0) | 5.0 (1.5–8.0) | 6.0 (3.0–14.0) | 0.01 |
SD Standard Deviation; ISS Injury Severity Score; SBP Systolic Blood Pressure; HR Heart Rate; GCS Glasgow Coma Score; mmHG Millimeter of Mercury; IQR Interquartile range.
The unadjusted 60-day mortality rate for patients with an ISS>15 was not statistically significantly different for patients triaged to a non-trauma vs. a trauma center (16% vs. 17%, p=0.87). However, trauma center care was associated with higher unadjusted costs and longer lengths of stay. The median per-patient costs were $35,069 for patients with an ISS>15 taken to trauma centers vs. $14,332 for those who did not go to trauma centers (p<0.001). Median length of stay was 6.0 vs. 5.0 for patients with an ISS>15 taken to trauma centers vs. non-trauma centers (p=0.01).
Since patients with an ISS>15 who were transported to trauma centers differed in many characteristics from patients transported to non-trauma centers, we performed logistic regression to determine the odds ratio (OR) for 60-day mortality while adjusting for demographics, mechanism, and physiology. After controlling for the above variables, there was still no statistical difference in mortality for patients with an ISS>15 transported to trauma centers (OR 1.87, 95% confidence interval 0.50–6.95). (Table 3) We also performed regression analysis to adjust for differences in costs between trauma centers and non-trauma centers using the same variables. (Table 4) After adjusting for age, ISS, gender, mechanism of injury, physiologic variables, and having a procedure, trauma center care remained associated with higher costs ($71,621 vs. 48,682, p=0.03).
Table 3.
Adjusted Odds Ratios for 60-Day Mortality for 143 Patients with ISS>15.
| Patients with ISS>15 | Adjusted Odds Ratio 60-d mortality |
95% Confidence Interval | ||
|---|---|---|---|---|
| Low | High | |||
| Demographics | ||||
| Age (per y) | 1.10 | 1.05 | 1.16 | |
| Female | 0.35 | 0.11 | 1.11 | |
| Mechanism of injury (vs fall) | ||||
| Fall | 1.00 | -reference- | ||
| MVC | 0.51 | 0.13 | 1.93 | |
| Other | 0.65 | 0.11 | 3.78 | |
| Physiology | ||||
| Prehospital HR>90 | 0.95 | 0.32 | 2.82 | |
| Prehospital SBP<90 | 4.57 | 0.70 | 30.06 | |
| Prehospital GCS<14 | 3.83 | 1.26 | 11.58 | |
| IR Procedure or nonorthopaedic surgery | 2.33 | 0.73 | 7.38 | |
| Trauma center (vs non-trauma center) | 1.87 | 0.50 | 6.95 | |
ROC=0.837. Hosmer-Lemeshow, p=0.37.
ISS, Injury Severity Score; SBP, systolic blood pressure; HR, heart rate; GCS, Glasgow Coma Score; IR, interventional radiology.
Table 4.
Comparison of Unadjusted vs Adjusted Costs for Patients with an ISS>15 Treated at Non-Trauma Centers and Trauma Centers
| Patients with ISS>15 | Non-trauma center | Trauma center | Difference | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Unadjusted costs | $ 14,332 | $5,112–$29,321 | $ 35,069 | $19,321–$88,357 | <0.001 |
| Adjusted costs* | $ 48,682 | $32,615–$69,993 | $ 71,621 | $29,126–$98,268 | 0.03 |
n for unadjusted analysis=131, n for adjusted analysis=54.
Adjusted for age, injury severity score, gender, mechanism of injury, pre-hospital heart rate, pre-hospital systolic blood pressure, pre-hospital GCS, having an interventional radiology or non-orthopedic surgery.
ISS, injury Severity Score; IQR, Interquartile Range.
Because there was no associated mortality difference between trauma centers and nontrauma centers for severely-injured patients, we next evaluated the characteristics of all injured elderly patients who lived vs. died while stratifying by various patient characteristics. (Table 5) Greater than 80% of patients were >75 years of age, 82% suffered a fall, 85% had a GCS>=14, 86% had an SBP>110, and 82% were not severely injured (i.e. have an ISS<15).
Table 5.
Patient Characteristics for All Patients ≥55 Years of Age (Regardless of ISS) who Survived vs Died (January 2006 to December 2007)
| All patients alive at 60 d | All patients dead by 60 d | p Value | ||
|---|---|---|---|---|
| n (%) | 5,555 (92.4) | 460 (7.6) | ||
| Age group, y, n (%) | ||||
| 55–65 | 1,504 (27.1) | 42 (9.1) | <0.001 | |
| 66–75 | 1,035 (18.6) | 47 (10.2) | ||
| 76–85 | 1,714 (30.9) | 182 (39.6) | ||
| >85 | 1,302 (23.4) | 189 (41.1) | ||
| Sex, n (%) | ||||
| Female | 3,441 (62.4) | 235 (51.9) | <0.001 | |
| Male | 2,072 (37.6) | 218 (48.1) | ||
| Mechanism of injury, n (%) | ||||
| Fall | 2,811 (67.2) | 281 (82.4) | <0.001 | |
| MVC | 765 (18.3) | 26 (7.6) | ||
| Other | 605 (14.5) | 34 (10.0) | ||
| ISS, n (%) | ||||
| ISS<=9 | 2,173 (84.7) | 163 (73.8) | <0.001 | |
| ISS 10–15 | 190 (7.4) | 17 (7.7) | ||
| ISS 16–25 | 167 (6.5) | 28 (12.7) | ||
| ISS>25 | 36 (1.4) | 13 (5.9) | ||
| Head injury, n (%) | ||||
| GCS<14 | 302 (5.9) | 64 (15.3) | <0.001 | |
| GCS>=14 | 4,801 (94.1) | 355 (84.7) | ||
| Systolic blood pressure, mmHg, n (%) | ||||
| <90 | 71 (1.3) | 20 (4.6) | <0.001 | |
| 90–109 | 325 (6.0) | 40 (9.2) | ||
| 110–129 | 965 (17.9) | 100 (23.0) | ||
| 130–149 | 1,634 (30.2) | 120 (27.6) | ||
| 150–169 | 1,287 (23.8) | 96 (22.1) | ||
| >=170 | 1,120 (20.7) | 59 (13.6) | ||
| Heart rate, n (%) | ||||
| <90 | 3,387 (62.5) | 261 (59.0) | 0.03 | |
| 90–99 | 950 (17.5) | 70 (15.8) | ||
| 100–119 | 860 (15.9) | 83 (18.8) | ||
| 120–129 | 137 (2.5) | 22 (5.0) | ||
| 130–139 | 48 (0.9) | 3 (0.7) | ||
| >=140 | 34 (0.6) | 3 (0.7) | ||
Percentage is calculated as percentage of non-missing values.
SD, Standard Deviation; ISS, Injury Severity Score; SBP, Systolic Blood Pressure; HR, Heart Rate; GCS, Glasgow Coma Score.
We also explored the possibility of including a propensity score analysis in this study: however, we found that the propensity score techniques produced weak analyses. Performing a matched propensity score analysis resulted in unbalanced comparison groups due to the small number. We also attempted to use propensity scores in a manner less dependent on the small number by including a propensity score in the logistic regression analyses. We found that neither the result nor the model performance changed when a propensity score was included in the analysis. Ultimately, all propensity score analyses resulted in the same findings as the above analyses and showed no difference in outcomes for trauma centers vs. non-trauma centers.
DISCUSSION
This is the first study to evaluate outcomes and costs associated with the triage of trauma patients ≥55 years of age from a population perspective. The advantage of the current study design is that it allows for a complete picture of triage patterns and the associated outcomes for an entire community, and not just patients transported to trauma centers. We also are able to determine 60-day mortality, which is necessary when analyzing mortality data in elderly patients as the majority of trauma-related death occurs after discharge.13,14 We found high rates of under-triage in this population. The under-triage rate was 33% when using a definition for major trauma of an ISS>15. When the definition was expanded to include patients who had a surgical or interventional radiology procedure, the under-triage rate increased to 44%. We also considered that the exclusion of the transferred patients may affect this rate. When we determine the under-triage rate while including transferred patients, the under-triage rate increased to 49%. The modest increase was due to the fact that 87% of the transfer records were associated with transfers between non-trauma centers.
The high rates of under-triage observed in this study cohort were not associated with higher 60-day mortality, contrary to our initial hypothesis. In both unadjusted and adjusted analyses, severely injured patients ≥55 years of age did not experience higher mortality when triaged to non-trauma centers. The National Study on Costs and Outcomes of Trauma (NSCOT) demonstrated similar findings. This was a prospective study of 5,000 major trauma patients, including patients older than 55 years of age.21 While severely-injured patients in that study were shown to have better outcomes when treated at trauma centers, the cohort of severely-injured patients ≥55 years did not experience the same benefit.
Why treatment at trauma centers does not benefit the severely-injured elderly trauma patient as it does for the young is not clear. It is likely that mortality in the elderly population is a result of more factors than the injury alone. This would result in a high “background” mortality rate that could obscure any measurable benefit from trauma center care. To explore whether this may be the case, we evaluated all patients who died, including those with an ISS<15. A striking pattern emerged. Most of the elderly patients who died after trauma sustained minor injuries from low-energy mechanisms. Greater than 80% of patients who died were >75 years of age, had suffered a fall, did not have a depressed GCS, were not hypotensive, and were not severely injured (i.e. have an ISS<15). The fact that most of the deaths in the elderly occur after sustaining minor injuries from low-energy mechanisms suggest that death is due to more than just the injury. It is likely that death results from the synergistic combination of baseline health, frailty, and injury. Furthermore, it is possible that in elderly trauma patients, injury is a marker for risk of death rather than an immediate cause of death.. These findings suggest that future interventions to improve outcomes might need to address the management of the non-severely injured elderly patient. If trauma centers successfully improve outcomes in these patients, it may be that “under-triage” should be redefined to direct even minor injuries to trauma centers.
It is likely that within the cohort of severely-injured elderly patients, there are those who do benefit from trauma center care. The limitations of currently available data prevent us from teasing out which injured elderly patients fall in this category. For example, robust and healthy elderly patients with severe injuries may be more similar to younger trauma patients. In this case, the care provided by trauma centers may help avert mortality after a severe injury. Even if we are unable to identify this group, we should conservatively assume they exist. Therefore, we should strive to reduce the high rates of under-triage while simultaneously studying which patients are in particular need of trauma center resources. This will likely involve novel data collection efforts, such as those that include information on pre-injury health and function, in order to allow for proper risk adjustment. We also should consider if there are resources that may benefit the injured elderly population that should be incorporated at trauma centers. For example, it may be that this population would benefit from the presence of specialized geriatric services after injury.
These differences in patients at risk for death after injury also help to explain the reason why trauma center care was not shown to be cost effective using data derived from the NSCOT study.22 The estimated incremental cost per life-year gained for an elderly patient (defined as ≥55) was $174,818 compared to $25,123 in the young. They concluded that regionalization of trauma care is cost effective for the general population, but that it appeared to be less so for the elderly population.
There are several limitations to this study. Trauma registry data can have inconsistent records on complications and diagnoses. Statewide databases contain administrative data but lack hospital-based data such as patient physiology and are limited in the number of diagnoses they contain. This limits our ability to know patient-level details, such as comorbidities, functional status, and presenting physiology. We also are lacking information on hospital-level details, such as nursing ratios, specialized services, or trauma-related protocols. The population was selected based on the determination of dispatch and pre-hospital personnel. There may be some patients who are included who had predominantly medical conditions, and others not included who may have been categorized as a medical condition by dispatch. Another limitation is the process of probabilistic linkage when utilizing disparate data sources. We are not able to determine the “true” matches and non-matches for any site as such information would have required access to the original medical records.
With the country’s aging demographic, it is important for us to understand and address the patterns of injury and outcomes of elderly patients. It is also important to consider how we manage these patients within our current system of care. The current body of literature and the present study certainly suggest opportunities for improvement in care of the injured elderly population. Further study is required to determine what interventions may be beneficial to the elderly, such as specialized geriatric hospitalist services. We also need to better understand the determinants of mortality in the lesser-injured older patient. Future work exploring this topic will use databases specifically designed to capture functional status, frailty, and comorbidities in the elderly.
Acknowledgments
Disclosure information. Nothing to disclose.
Supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program; the Oregon Clinical and Translational Research Institute (grant # UL1 RR024140); Stanford Center for Clinical and Translational Education and Research (grant # 1UL1 RR025744); University of Utah Center for Clinical and Translational Science (grant # UL1-RR025764 and C06-RR11234); and UCSF Clinical and Translational Science Institute (grant # UL1 RR024131). All Clinical and Translational Science Awards are from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abstract presented at the American Association for the Surgery of Trauma Annual Meeting, Kauai, HI, September 2012.
REFERENCES
- 1.HCUPnet. [Accessed April 10, 2011];2008 http://hcupnet.ahrq.gov/HCUPnet.jsp.
- 2.He W, Sengupta M, Velkoff V, DeBarros K. Census US. Washington DC: U.S. Government Printing Office; 2005. 65+ in the United States: 2005. [Google Scholar]
- 3.Champion HR, Copes WS, Buyer D, et al. Major trauma in geriatric patients. Am J Public Health. 1989;79:1278–1282. doi: 10.2105/ajph.79.9.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shifflette VK, Lorenzo M, Mangram AJ, et al. Should age be a factor to change from a level II to a level I trauma activation? J Trauma. 2010;69:88–92. doi: 10.1097/TA.0b013e3181e291e9. [DOI] [PubMed] [Google Scholar]
- 5.Morris JA, Jr, MacKenzie EJ, Damiano AM, Bass SM. Mortality in trauma patients: the interaction between host factors and severity. J Trauma. 1990;30:1476–1482. [PubMed] [Google Scholar]
- 6.Hsia RY, Wang E, Saynina O, et al. Factors associated with trauma center use for elderly patients with trauma: a statewide analysis, 1999–2008. Arch Surg. 2011 Jan 17; doi: 10.1001/archsurg.2010.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vassar MJ, Holcroft JJ, Knudson MM, Kizer KW. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003;197:717–725. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 8.Newgard CD, Zive D, Holmes JF, et al. A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213:709–721. doi: 10.1016/j.jamcollsurg.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Newgard C, Malveau S, Staudenmayer K, et al. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19:469–480. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 12.Mullins RJ, Mann NC, Hedges JR, et al. Adequacy of hospital discharge status as a measure of outcome among injured patients. JAMA. 1998;279:1727–1731. doi: 10.1001/jama.279.21.1727. [DOI] [PubMed] [Google Scholar]
- 13.Davidson GH, Hamlat CA, Rivara FP, et al. Long-term survival of adult trauma patients. JAMA. 2011;305:1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- 14.Fleischman RJ, Adams AL, Hedges JR, et al. The optimum follow-up period for assessing mortality outcomes in injured older adults. J Am Geriatr Soc. 2010;58:1843–1849. doi: 10.1111/j.1532-5415.2010.03065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark D, Osler T, Hahn D. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores: Boston College Department of Economics. 2010 [Google Scholar]
- 16.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27:412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Meredith JW, Evans G, Kilgo PD, et al. A comparison of the abilities of nine scoring algorithms in predicting mortality. J Trauma. 2002;53:621–628. doi: 10.1097/00005373-200210000-00001. discussion 628–629. [DOI] [PubMed] [Google Scholar]
- 18.Glance LG, Osler TM, Mukamel DB, et al. Expert consensus vs empirical estimation of injury severity: effect on quality measurement in trauma. Arch Surg. 2009;144:326–332. doi: 10.1001/archsurg.2009.8. discussion 332. [DOI] [PubMed] [Google Scholar]
- 19.Fleischman R, Mann NC, Wang NE, et al. Validating the use of ICD9 codes to generate Injury Severity Score: the ICDPIC mapping procedure. [Abstract] Acad Emerg Med. 2012;19:S314. [Google Scholar]
- 20.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214:756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 22.MacKenzie EJ, Weir S, Rivara FP, et al. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]