Abstract
Lentiviruses are becoming progressively more popular as gene therapy vectors due to their ability to integrate into quiescent cells and recent clinical trial successes. Directing these vectors to specific cell types and limiting off-target transduction in vivo remains a challenge. Replacing the viral envelope proteins responsible for cellular binding, or pseudotyping, remains a common method to improve lentiviral targeting. Here, we describe the development of a high titer, 3rd generation lentiviral vector pseudotyped with Nipah virus fusion protein (NiV-F) and attachment protein (NiV-G). Critical to high titers was truncation of the cytoplasmic domains of both NiV-F and NiV-G. As known targets of wild-type Nipah virus, primary endothelial cells are shown to be effectively transduced by the Nipah pseudotype. In contrast, human CD34+ hematopoietic progenitors were not significantly transduced. Additionally, the Nipah pseudotype has increased stability in human serum compared to VSV pseudotyped lentivirus. These findings suggest that the use of Nipah virus envelope proteins in 3rd generation lentiviral vectors would be a valuable tool for gene delivery targeted to endothelial cells.
Keywords: lentivirus, pseudotype, endothelial cell, Nipah virus
INTRODUCTION
Gene therapy holds the appeal of a “one-shot” cure for human disease (see 1 for review). This is particularly true for the treatment of monogenic diseases. Since permanent gene correction is often necessary for maximal therapeutic benefit, the use of retroviral vectors has steadily expanded. In contrast with other viral vectors and plasmid DNA, gamma retroviruses efficiently integrate into the cellular genome. However, the ability to integrate into the genome brings with it a significant risk of insertional oncogenesis. Reducing this risk has led to several improvements in retroviral vector design including self-inactivating long terminal repeats (LTRs) 2, insulator sequences 3, and the use of endogenous promoters 4. Nevertheless, lentiviral vectors are also garnering increasing attention for their use in clinical trials 5–6. These vectors have several key advantages over gamma retrovirus vectors including the ability to transduce non-dividing cells 2 and less risk of insertional oncogenesis 7.
Targeting of lentiviral vectors to specific cell types can be accomplished in a number of ways. Controlling the route of administration may be the simplest means; however, this method is largely limited to ex vivo approaches. Using cell-specific promoters is an effective method for limiting transgene expression, but still does not prevent genome integration effects in off-target cells. In contrast, altering the viral cell attachment protein to limit or target vectors to specific cell types is a highly effective technique. Often referred to as ‘pseudotyping’, attachment proteins from a wide variety of viruses have successfully replaced the gp160 envelope protein in HIV-1 based lentiviral vectors for gene therapy use (see 8 for a comprehensive list of examples). The glycoprotein from the Vesicular stomatitis virus (VSV-G) is the most widely used due to its broad cellular tropism and high titer production. The broad tropism of VSV-G serves as a disadvantage in some gene therapy applications where transduction of only a specific cell type is desired. The VSV-G pseudotype may also enhance peripheral dendritic cell activation to lentiviral vectors in vivo 9. Consequently, alternative lentiviral pseudotypes are continually being developed. Membrane-anchored glycoproteins from the Paramyxoviridae family are excellent candidates to pseudotype lentiviruses. For example, glycoproteins from Measles 10–11, Sendai 12, and more recently, Tupaia viruses 13 have all pseudotyped lentiviruses successfully. Therefore, it is feasible that glycoproteins from Nipah virus, a Paramyxoviridae family member, may also incorporate into lentiviral particles. Indeed, one laboratory reported it is possible to pseudotype with Nipah virus proteins using 1st generation HIV vectors 14.
Nipah virus is a deadly pathogen which is transmitted by bodily fluids from pteropid fruit bats and livestock to humans 15–16. The Nipah virus envelope contains two surface glycoproteins required for cellular entry: the attachment protein (NiV-G) and fusion protein (NiV-F). Niv-G allows for attachment of the virion to cellular receptors; whereas NiV-F mediates the direct union of the virus and cellular membranes. Unlike most attachment proteins of the Paramyxoviridae family, Niv-G does not contain hemagglutinin nor neuraminidase activities. The cellular receptors for Nipah virus are ephrin-B2 17–18 and, at a 10-fold lower affinity, ephrin-B3 19. Ephrin-B2 expression is strongest in arterial endothelial cells, but is also expressed in vascular smooth muscle cells and pericytes 20–21. As a result, using Nipah envelope proteins may be an effective solution for targeted gene therapy vectors to the vasculature where permanent gene integration is desirable. For example, several methods are available to expose the coronary vasculature to gene therapy vectors 22. The use of a Nipah-based vector may improve upon low endothelial transduction rates observed with adenoviruses 23 and the lack of persistence of plasmid vectors 24. Ephrin-B2 is also highly expressed in tumor endothelium 25–26. In coordination with endothelial-specific promoter sequences 27, tumor vasculature could be targeted in a highly specific way with a Nipah-based vector. Additionally, Nipah virus is exceedingly rare so existing humoral immunity is highly unlikely to be present in humans and laboratory animals to interfere with gene delivery.
In the present study, we describe the production and optimization of a 3rd generation, HIV-based, lentiviral vector pseudotyped with Nipah virus envelope glycoproteins for potential use in gene therapy applications. Critical to our success was truncation of NiV-G. Combined with previous findings on the importance of NiV-F truncation 14, high titers can be obtained.
RESULTS
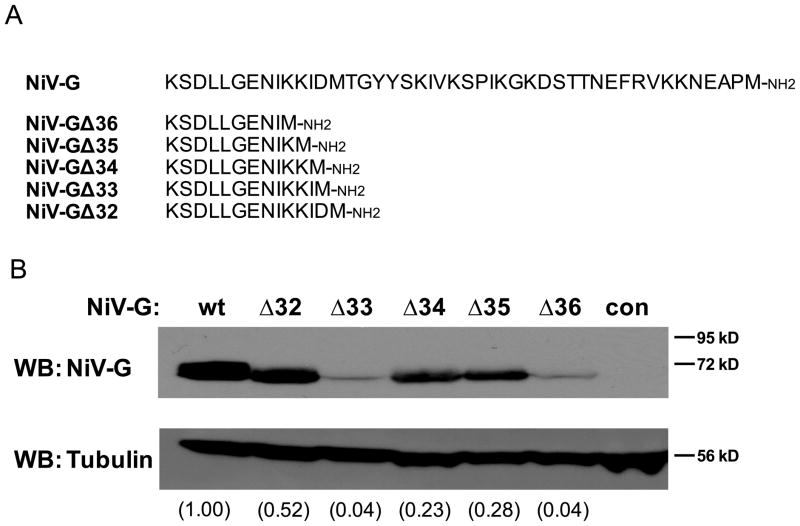
A number of other previously published studies where truncation of envelope protein cytoplasmic domains was used as a strategy to successfully pseudotype both murine retroviruses 28–29 and lentiviruses 12 have been described. Studies using a related Paramyxoviridae family member, Measles virus, observed that a truncation leaving 10 10 or 16 11 amino acids in the cytoplasmic domain of the attachment glycoprotein H led to optimal titers. Therefore, we designed a series of five NiV-G cytoplasmic domain truncation mutants with between 10 and 14 amino acids (Fig. 1a). All of the NiV-G mutants eliminate the YY sorting signal 30; however, this signal appears important only in polarized cells and should not affect production in non-polarized HEK293T cells. To confirm expression of NiV-G mutants in HEK293T producer cells, co-transfected was performed with wild-type NiV-F. Compared to wild-type NiV-G, mutants expressed at significantly lower levels (Fig. 1b). This result suggests differences in protein stability or translation between the mutants. Differences in lower molecular weight bands were not observed upon overexposure of anti-NiV-G western blots (data not shown).
Figure 1. Nipah G cytoplasmic domain truncation mutants and their expression in HEK293T cells.
A) Schematic of the Nipah G mutants compared to the wild-type sequence. Only the cytoplasmic domain is shown. B) Equal amounts of plasmid expressing the Nipah G proteins from ‘A’ with wild-type Nipah F were transfected into HEK293T cells (lentiviral plasmids were excluded). Untransfected cells were loaded in the lane marked “con”. A representative western blot is shown (n=2). Densitometry readings are displayed in parenthesis and correspond to the Nipah G signal divided by the tubulin signal. Densitometry readings were normalized to the wild-type value.
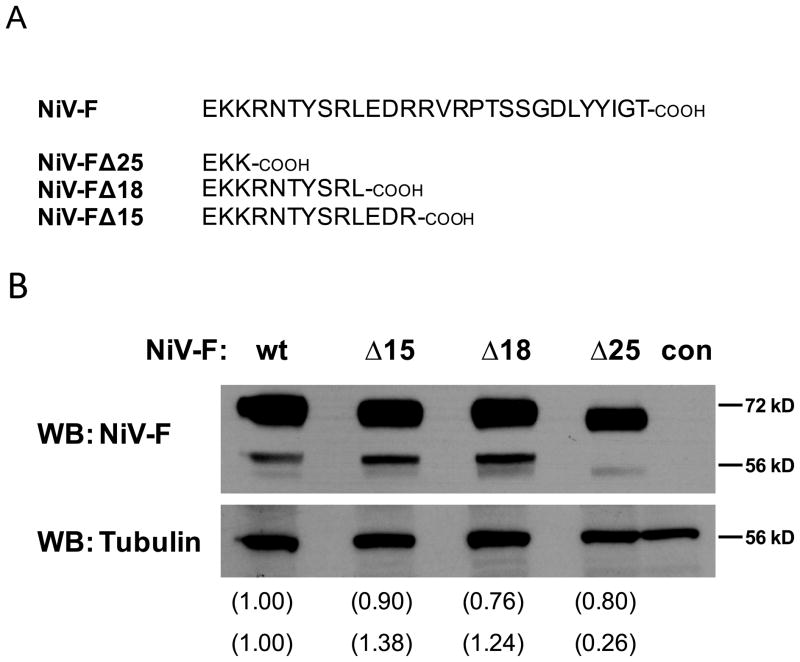
Previous work has shown the optimal Measles virus fusion protein modification involved a truncation to only three cytoplasmic amino acids 11. Accordingly, we created a comparable truncation of the NiV-F protein, FΔ25 (Fig. 2a). However, a unique aspect of NiV-F needed to be addressed: it requires endocytosis after its initial appearance at the cell surface to be fully processed into the active mature form 31. Upon endocytosis, unprocessed NiV-F protein (F0) is cleaved into two, disulfide-linked subunits (F1 and F2) by cathepsin B 32 or cathepsin L 33 and is then returned to the cell surface. The specific amino acid motif located in the cytoplasmic domain responsible for NiV-F maturation is “YSRL” 31. Consequently, we utilized additional NiV-F truncations containing this endocytosis motif (FΔ18), and another containing a highly charged region (FΔ15) 34, to address their potential contributions to successful lentiviral incorporation (Fig. 2a). A previous study described co-expression of NiV-F truncated to “EKKR” (FΔ24 by our naming convention) and wild-type NiV-G allowed pseudotyping of a 1st generation HIV vector 14. Similar constructs to FΔ15 and FΔ18 were also examined but had poor infectivity 14. Since we used a different vector system (3rd generation HIV) and were combining NiV-F AND NiV-G truncations, we thought it would be interesting to include FΔ15 and FΔ18 in our study. When confirming expression levels in HEK293T cells (co-transfected with wild-type NiV-G), all NiV-F proteins were expressed at similar levels (Fig. 2b). As would be expected, removal of the endocytosis motif reduced the levels of mature F1 protein in FΔ25 (Fig. 2b).
Figure 2. Nipah F cytoplasmic domain truncation mutants and their expression in HEK293T cells.
A) Schematic of the Nipah F mutants compared to the wild-type sequence. Only the cytoplasmic domain is shown. B) Equal amounts of plasmid expressing the Nipah F proteins from ‘A’ with wild-type Nipah G were transfected into HEK293T cells (lentiviral plasmids were excluded). A representative western blot is shown (n=2). Untransfected cells were loaded in the lane marked “con”. The top band in the NiV-F blot corresponds to NiV-F0 the lower band to NiV-F1. Densitometry readings are displayed in parenthesis and correspond to the Nipah F signal divided by the tubulin signal (the upper densitometry value corresponds to NiV-F0 and the lower to NiV-F1). Densitometry readings were normalized to the wild-type values.
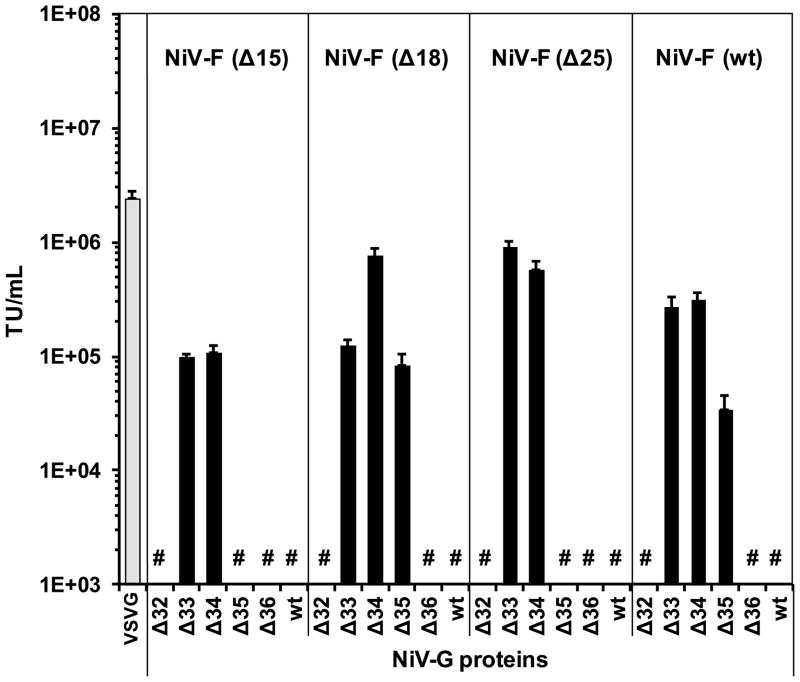
Next, we examined the ability of the modified Nipah proteins to create functional lentiviral particles. Combinations of each NiV-G and NiV-F mutant were co-transfected with a standard 3rd generation lentiviral packaging system which expresses EGFP 2. Lentivirus packaged with VSV-G envelope (VpL) was used as a positive control and a basis of comparison. Filtered supernatants were incubated with HEK293 cells which are commonly used to titer VpL but also endogenously express the Nipah receptor ephrin-B2 18. Figure 3 shows the combined results of two independent experiments. The NiV-G truncations GΔ33 and GΔ34 appeared to be the most consistent at producing relatively high titers and wild-type NiV-G was not able to produce a measureable titer with any NiV-F combination (Fig. 3). The NiV-F truncations, in contrast, had only a modest effect on titer with FΔ25 having the best performance (Fig. 3). Pretreatment and inclusion of 50 μM 3′-azido-3′-deoxythymidine (AZT) in the titer assay prevented approximately 92% of the GFP positive reading in both VpL and FΔ25/GΔ33 transduced HEK293 cells (data not shown). Titer assays of VpL and FΔ25/GΔ33 were also performed after pre-incubation with soluble human ephrin-B2 to confirm specificity to ephrin-B2. The data in figure 4 demonstrates that the transduction of permissive cells by FΔ25/GΔ33 is dependent on binding ephrin-B2. Furthermore, Chinese hamster ovary cells, which are not permissive to Nipah virus infection 35, were not transduced by FΔ25/GΔ33 (data not shown). Our results indicate that several combinations, particularly FΔ25/GΔ33, can successfully pseudotype lentiviral vectors at titers within 2–3 fold of VpL and display the predicted specificity to ephrin-B2.
Figure 3.
Titers of lentiviral productions using different combinations of Nipah envelope proteins compared to the Vesicular Stomatitis Virus (VSVG) envelope. Lentivirus was produced by transient transfection as described in the methods section. Titers were measured by exposing HEK293 cells to viral supernatants for 16 hr and represented as transducing units per mL (TU/mL). The displayed results are the average of two independent experiments. Grey bar = VSVG. Black bars = Nipah envelopes. # denotes below assay detection limit.
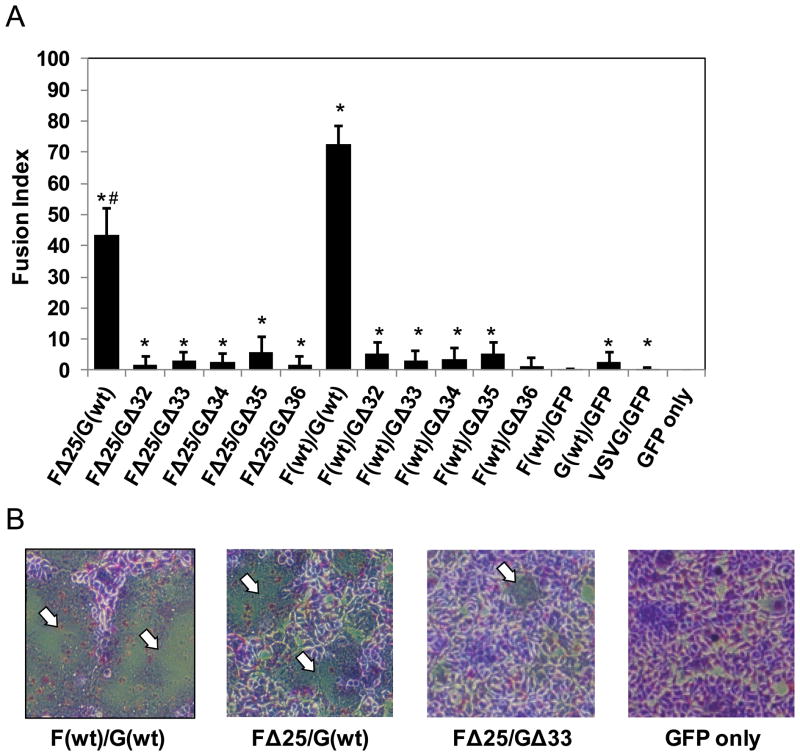
Figure 4. Analysis of cell fusion abilities of wild-type Nipah F and FΔ25 with Nipah G proteins.
HEK293T cells were transfected with equal amounts of Nipah F and Nipah G plasmids (lentiviral plasmids were excluded). Plasmids expressing VSVG and EGFP served as controls. A) The average percent area of cytopathic effect from cell fusion per 100× field is defined as the ‘fusion index’. * denotes significant difference compared to GFP only cells (p ≤ 0.05 by two-tailed t-test). # denotes significant difference compared to F(wt)/G(wt) cells (p ≤ 0.001 by two-tailed t-test). B) Representative images of fusion experiment. White arrows label areas of cytopathic effects/cell fusion. Note the lack of cytopathic effects/cell fusion in the ‘GPF only’ image. The remaining experimental groups not shown appear similar to FΔ25/GΔ33.
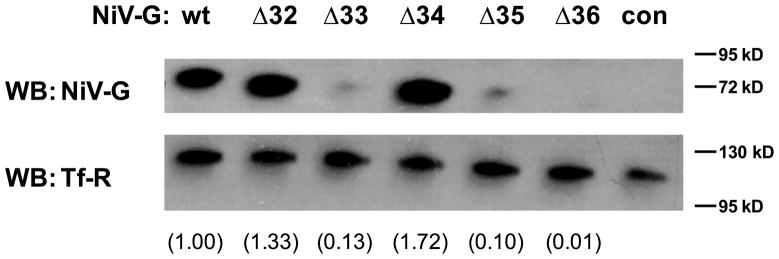
It was interesting how NiV-G truncation had a more profound overall effect on titer when compared to NiV-F truncation alone (Fig. 3). As a result, we further investigated the mechanism behind the titer differences. It is known that co-transfection of wild-type NiV-G and NiV-F in ephrin-B2 positive cells leads to cell fusion 34, 36. Therefore, extensive producer cell fusion may be a limiting factor when producing lentivirus. To explore this possibility, HEK293T cells were transfected with combinations of plasmids expressing wild-type or truncated Nipah G with FΔ25 or wild-type NiV-F. As shown in Figure 5a, co-expression of wild-type NiV-G with either FΔ25 or wild-type NiV-F led to extensive cytopathic effect (CPE) due to cell fusion. Likely because of the reduction of mature F1 protein produced by FΔ25 (Fig. 2b), less CPE was observed with this mutant (Fig. 5a). In contrast, inclusion of any NiV-G truncation mutant abrogated CPE independent of the NiV-F construct used (Fig. 5a). Representative images of the striking differences in CPE between wild-type NiV-G and GΔ33 are displayed in Figure 5b. The lack of CPE when using NiV-G truncation could be due to the absence of NiV-G on the cell surface for binding to ephrin-B2. Thus, we performed cell surface biotinylation followed by NiV-G western blotting of isolated biotinylated proteins to determine the relative abundance of NiV-G mutants in the plasma membrane. Transferrin receptor, a ubiquitous plasma membrane protein, was used as a loading control. We found that only GΔ32 and GΔ34 are well expressed at the cell surface when compared with wild-type NiV-G (Fig. 6). Similar results were obtained when lentiviral packaging plasmids were included (data not shown). However, neither GΔ32 nor GΔ34 was able to cause appreciable CPE (Fig. 5a) and only GΔ34 is associated with high titers (Fig. 3). Taken together, these results imply that the cell surface presence of the NiV-G truncation mutants per se does not correlate with CPE or titers.
Figure 5. Cell surface biotinylation of HEK293T cells expressing NiV-G proteins.
HEK293T cells were transfected with individual NiV-G plasmids (lentiviral plasmids were excluded). Cell monolayers were then biotinylated and the biotinylated protein fractions used in western blotting procedures for NiV-G and transferrin receptor (Tf-R). Untransfected cells were loaded in the lane marked “con”. A representative western blot is shown (n=2). Densitometry readings are displayed in parenthesis and correspond to the NiV-G signal divided by the Tf-R signal. Densitometry readings were normalized to the wild-type value.
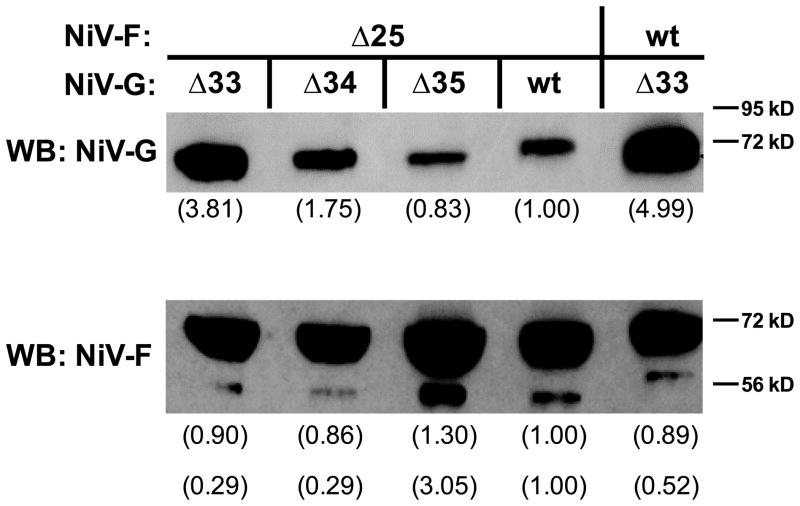
Figure 6. Western blot analysis of lentiviral particles.
Lentivirus was produced by transient transfection and concentrated by low speed centrifugation as described in the methods section. A p24 assay was performed to normalize the lentiviral particles and 350 ng per lane was separated by SDS-PAGE. A western blot was performed for Nipah G and the same filter re-probed for Nipah F. Densitometry readings are displayed in parenthesis (the upper densitometry value for Nipah F corresponds to NiV-F0 and the lower to NiV-F1). Densitometry readings were normalized to the wild-type value. A representative blot is shown (n=2).
Another potential mechanism for titer improvement seen with NiV-G truncation is the final levels of envelope proteins incorporated into the lentiviral particles. Consequently, we performed western blots (normalized to p24 content) on viral supernatants from the following combinations of NiV-F and NiV-G with relatively high titers: FΔ25/GΔ33, FΔ25/GΔ34, and F(wt)/GΔ33. As a comparison, in the western blot we included combinations without detectable titers: FΔ25/GΔ35 and FΔ25/G(wt). Lentiviral particles displaying the highest content of Nipah G protein, GΔ33 and GΔ34 (Fig. 7), were also the mutants which yielded superior titers (Fig. 3). These results suggest that the relative level of lentiviral NiV-G content is associated with the highest titers for this pseudotype.
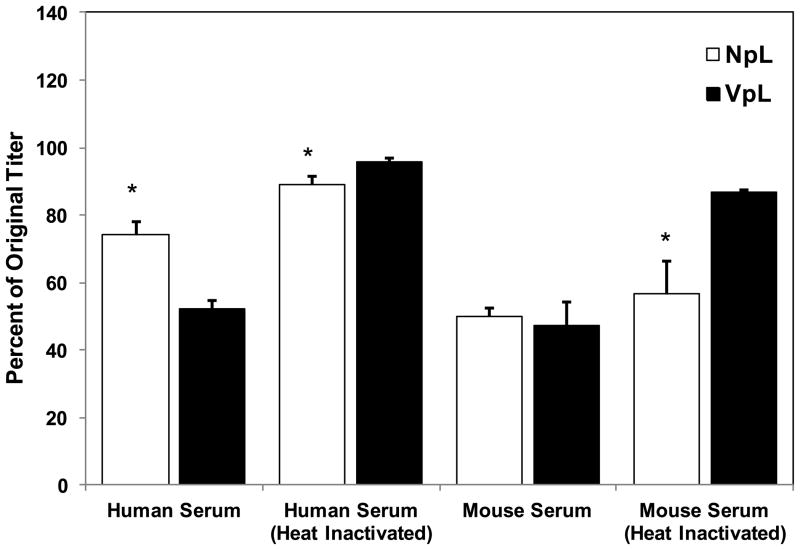
Figure 7. The stability of NpL and VpL in human or mouse serum.
Aliquots of unconcentrated virus were incubated 1:1 with serum or D10 media at 37° C for 1hr and titered on HEK293 cells. The percent remaining titer was calculated by dividing the serum treated aliquots by D10 treated aliquots. The inclusion of VpL, known to be inactivated by serum, served as a control. A representative experiment is shown (n=2). * denotes significant difference compared to identically treated VpL (p 0.05 by two-tailed t-test).
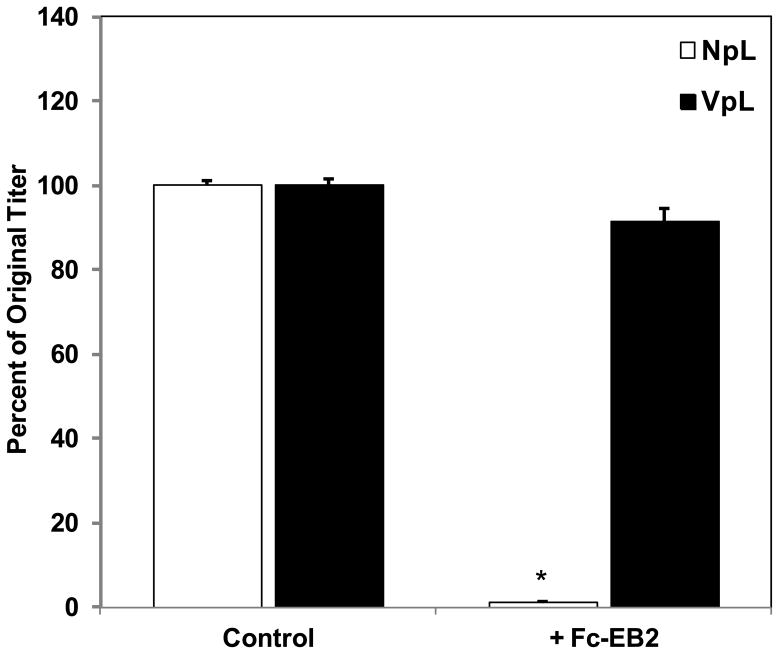
Since in vivo studies require large quantities of a relatively stable lentivirus, we investigated ways to maximize titer and tested the serum stability of FΔ25/GΔ33. For clarity, from this point on we will refer to FΔ25/GΔ33 as Nipah pseudotyped lentivirus (NpL). The Measles lentiviral pseudotype required adjustment of the ratio of envelope plasmids to maximize titer 11. A modest 1.5 fold gain in titer was obtained by lowering the amount of FΔ25 plasmid; however, no other alterations to the envelope plasmid ratios had any significant effect (data not shown). The final optimized plasmid ratios are reported in the “Materials and Methods” section. We also examined the ability of NpL to be concentrated by low speed centrifugation and ultracentrifugation. NpL could be concentrated by at least 72-fold, but appeared sensitive to the ultracentrifugation method (Table 1). To compare the serum stabilities of NpL and VpL, we incubated unconcentrated viral supernatant with an equal amount of mouse or human serum for 1 hr and then compared the titer to supernatant incubated with D10 media (contains 10% FBS). Both pseudotypes are inactivated by mouse serum to a similar extent (Fig. 8). However, NpL is less sensitive to human serum inactivation (Fig. 8). Taken together, NpL can be effectively concentrated to high titer and may have a stability advantage compared to VpL in gene therapy applications where exposure to human serum is necessary.
Table 1.
Concentration of NpL and VpL using two different methods.
| Virus | Titer (TU/mL × 107)
|
||
|---|---|---|---|
| Unconcentrated | Low speed concentration | Ultracentrifuge concentration | |
| VpL | 3.6 | 220 (61) | 320 (89) |
| NpL | 1.1 | 77 (72) | 41 (38) |
A production of each pseudotype was divided into two fractions that were concentrated using either a low speed centrifugation (3,600 g overnight) or an ultracentrifugation (100,000 g for 1 hr) method to reduce the volume 100-fold. Aliquots were then titered using HEK293 cells. The values in parenthesis corresponds to the fold-increase from unconcentrated titer. Data is representative of two independent experiments.
Figure 8. Titers of NpL and VpL after pre-incubation with soluble ephrin-B2 receptor.
Aliquots of unconcentrated virus were incubated with 1 μg/mL human ephrin-B2/Fc chimera or buffer control for 30 min before titering on HEK293 cells. The percent remaining titer was calculated by dividing the ephrin-B2/Fc chimera treated values by buffer control values. A representative experiment is shown (n=2). * denotes significant difference compared to identically treated VpL (p ≤ 0.05 by two-tailed t-test).
We next compared the transduction ability of NpL with VpL using primary endothelial cells in vitro. Endothelial cells have been shown to be highly permissive to Nipah virus infection in vitro 37–38. Human umbilical vein (HUVECs), human dermal microvascular (HDMECs), and mouse lung microvascular (MLMECs) endothelial cells were transduced over a range of concentrations. Table 1 shows a representative experiment where NpL is compared to VpL in transduction ability. HUVECs, particularly at 25 and 100 MOI, are highly transduced by both lentiviruses. However, NpL only modestly transduced HDMECs and MLMECs. We also observed that GFP+ cells of the HDMECs and MLMECs had a drastically reduced median fluorescent intensity when transduced with NpL (Table 1). These transduction results are likely the result of HUVECs being a relatively homogeneous population of cells expressing ephrin-B2; whereas microvascular endothelial cells are comprised of both arterial and venous sources known to be either positive or negative for ephrin-B2, respectively 39–40. To test this possibility, we performed a western blot analysis of ephrin-B2 expression in confluent cultures of HUVECs and HDMECs. The data in figure 9 confirms that HDMECs express reduced levels of ephrin-B2. Overall, our data shows that NpL can transduce both mouse and human endothelial cells.
Figure 9. Western blot analysis of ephrin-B2 expression in human endothelial cells.
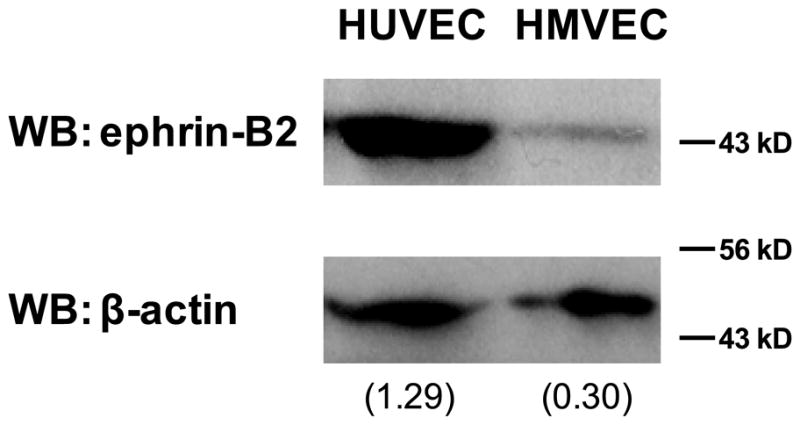
A western blot was performed on cellular extracts from HUVECs and HDMECs probing for ephrin-B2. The membrane was stripped and re-probed for β-actin as a loading control. Densitometry readings are displayed in parenthesis. A representative blot is shown (n=2).
Recent data demonstrated that human monocytes, macrophages, and lymphocytes are non-permissive to Nipah virus infection 41. However, it is unknown if wild type Nipah virus infects hematopoietic progenitors. VsL vectors have been used to transduce CD34+ hematopoietic progenitor cells 42–43. This property is beneficial in ex vivo gene therapy but not with in vivo approaches where off-target CD34+ cell transduction is potentially harmful. Therefore, we examined the ability of NpL to transduce human CD34+ cells from cord blood. NpL was found to have a low maximal transduction rate of only 2.8% (Table 3). This suggests that compared to VpL, NpL is better suited to gene therapy involving intravenous administration as the risk of hematopoietic progenitor cell transduction is low.
Table 3.
A comparison between NpL and VpL in the transduction of human CD34+ progenitor cells.
| Cells | Virus | Percent GFP+
|
|
|---|---|---|---|
| MOI = 50 | MOI = 100 | ||
| CD34+ | VpL | 63.6 ± 0.6 (25) | 68.9 ± 0.1 (27) |
| NpL | 2.3 ± 0.3 (14)1 | 2.8 ± 0.1 (15)1 | |
Cord blood CD34+ cells were exposed to lentivirus for 16 hr and GFP positive cells determined by flow cytometry 3 days after virus incubation. The value in parenthesis corresponds to the median fluorescence intensity channel of the GFP positive cells (min=1, max=9910). Untreated cells had a median fluorescence intensity channel of 2.
denotes significant difference compared to VpL for indentical MOI (p ≤ 0.001 by two-tailed t-test).
DISCUSSION
We demonstrated that NpL can be produced at high titer in a 3rd generation lentivirus system, concentrated, and has improved stability in human serum when compared with VpL. NpL was also shown to transduce primary endothelial cells but not significantly transduce CD34+ hematopoietic progenitors. Therefore, NpL may be a useful vector for in vivo gene transfer to the vascular system.
Since shortened cytoplasmic tails (10–16 amino acids) of the attachment proteins enabled high lentiviral titers of other Paramyxoviridae pseudotypes 10–11, 13, it is not unexpected that this strategy was successful with the Nipah virus pseudotype. Several factors were examined to determine the mechanism of using truncated Nipah attachment protein (NiV-G) in a lentiviral pseudotype. The relative total cellular expression levels of the NiV-G mutants (Fig. 1b) did not appear to influence titers (Fig. 3). Likewise, relative cell surface presence of truncated NiV-G did not affect titers (Fig. 5). Instead, the key determinant was efficient packaging into lentiviral particles (Fig. 6). These findings are consistent with previous work which demonstrated lentiviral particles primarily assemble in endosomal compartments with some pseudotypes 44–45. It has been demonstrated that NiV-F and NiV-G do not affect the cell surface expression of each other 36. As only wild-type NiV-G was capable of mediating extensive CPE (Fig. 4a), truncated NiV-G proteins are likely confined to plasma membrane regions sequestered from ephrin-B2 on neighboring cells (i.e. away from cell-cell junctions). This possibility is highlighted by the fact that GΔ34 has a strong cell surface presence (Fig. 5), causes almost no CPE (Fig. 4a), and yet is still capable of efficiently binding ephrin-B2 in the context of a lentivirus particle (Fig. 3). Taken together, NiV-G truncations, particularly GΔ33 and GΔ34, enable more effective incorporation into lentiviral particles.
NiV-F truncation had only a modest effect on titers (Fig. 3). This result is in contrast to the Measles lentiviral pseudotype where truncation led to logarithmic increases in titer 10–11. FΔ25 displayed reduced CPE compared with wild-type NiV-F but the effect on overall titer was less profound because the NiV-G truncation alone had a larger effect (Fig. 5). Similar to previous work 14, removing the endocytosis signal in FΔ25 modestly improved titer – even though less of the mature (F1) form incorporated into lentiviral particles (Fig. 7). Potentially, a relatively small amount of NiV-F1 is an advantage in the context of lentiviral particles. In support of this possibility, both wild-type and FΔ25 incorporated into lentiviral particles with GΔ33 equally well (Fig. 7); yet FΔ25 yielded higher titers (Fig. 3).
NpL was effective in transducing primary endothelial cells (Table 2). This result is not surprising considering that during infection, Nipah virus antigen is present in endothelial cells and leads to significant vasculature pathology in vivo 46–47. In vivo, ephrin-B2 is typically localized to arterial vessels 39–40. HUVECs also express ephrin-B2 and are permissive to Nipah virus infection 37–38. NpL was able to transduce HUVECs almost as efficiently as VpL (Table 2). In contrast, the HDMECs and MLMECs were more difficult to transduce with NpL (Table 2); this was likely due to reduced expression of ephrin-B2 (Figure 9). The fact that we observed transduction of mouse endothelial cells (Table 2) was interesting. Mice have been reported to be non-permissive to Nipah virus infection 46–47. At least in the context of a lentivirus particle, our results show that mouse ephrin-B2 is capable of binding NiV-G and allows for viral entry (Table 2). Of note, heat-inactivated mouse serum retained most of its neutralizing effects against NpL (Figure 8). This finding suggests that a significant contribution to Nipah virus resistance in mice may be heat-stable, innate immunity serum proteins, such as α2-macroglobulin, that are known to bind viruses 48–49. As with any viral vector, delivery methods will need to be optimized before NpL will be useful in testing gene delivery in mouse models of disease. For example, to avoid dilution effects and promote enhanced contact with target cells, it may necessitate isolating the targeted vasculature with catheter systems similar to those used for cardiac gene therapy 22.
Table 2.
A comparison between NpL and VpL in the transduction of three distinct primary endothelial cell lines.
| Cells | Virus | Percent GFP+ | ||
|---|---|---|---|---|
| MOI = 5 | MOI = 25 | MOI = 100 | ||
| HUVEC | VpL | 74.0 ± 0.7 (1534) | 98.8 ± 0.1 (6887) | 99.7 ± 0.1 (9910) |
| NpL | 60.4 ± 0.9 (795)1 | 94.5 ± 0.8 (2605)1 | 98.7 ± 0.2 (9910)1 | |
| HDMEC | VpL | 86.8 ± 0.1 (522) | 95.0 ± 1.6 (2238) | 93.5 ±1.3 (3023) |
| NpL | 5.7 ± 0.6 (30)1 | 38.8 ± 1.7 (404)1 | 62.6 ± 3.5 (594)1 | |
| MLMEC | VpL | 43.8 ± 1.4 (363) | 81.4 ± 1.1 (782) | 91.0 ± 1.4 (2345) |
| NpL | 8.9 ± 1.7 (299)1 | 27.9 ± 0.4 (411)1 | 51.2 ± 1.9 (613)1 | |
Endothelial cells were exposed to various concentrations lentivirus for 16 hr in the presence of 4 μg/mL polybrene. GFP positive cells were determined by flow cytometry three days after virus incubation. The value in parenthesis corresponds to the median fluorescence intensity channel of the GFP positive cells (min=1, max=9910). Untreated cells had median fluorescence intensity channels between 2–4.
Denotes significant difference compared to VpL for indentical MOI and cell type (p ≤ 0.001 by two-tailed t-test).
In animal models, Nipah virus envelope proteins have been reported to possess immunogenicity in the context of viral vectors 50–52 and as recombinant proteins (with adjuvant) 53 in vaccine studies. It is unknown if this immunogenicity would present in humans in the context of a lentivirus vector. For example, lentivirus vectors stimulate mouse dendritic cells in a pseudotype independent manner 54; in contrast, human dendritic cells appear to only respond to the VSV-G pseudotype 9. Although a strong immune reaction to NpL in humans would complicate gene therapy applications, perhaps it would be functional as a vaccine.
During the preparation of this manuscript, a study published ahead of print reported the use of a 2nd generation lentiviral vector pseudotyped with NiV-G and NiV-F to transduce a specific population of human CD34+ hematopoietic stem cells 55. In support of our findings, CD34+ hematopoietic progenitors were not significantly transduced 55. Potential transduction of hematopoietic stem cells will be important to address from a safety standpoint if the Nipah pseudotype is to be used in human gene therapy. For example, can the Nipah pseudotype transduce hematopoietic stem cells when used intravenously? In contrast to our work, the study by Palomares et al did not find NiV-G truncation beneficial to titer. However, only truncation down to an equivalent to our GΔ32 was tested. Interestingly, when their Nipah pseudotype was administered intravenously to mice, vector genomes were only detected in the lung and spleen 55. Conceivably, cells in the lung positive for the vector genomes could be endothelial as we found NpL to transduce MLMECs (Table 1). However, the specific transduced cell types were not identified by microscopy.
In sum, NpL is a useful tool for targeting the ephrin-B2 receptor. It is worth noting that preferential arterial expression of ephrin-B2 exists down to the microvascular level 20; it is conceivable NpL could be directed to this specific subset of endothelial cells. NpL could also be used to target ephrin-B2 on particular cancer cells 56–57 or to areas of neovascularization 26. VpL infects cells using an undefined cellular binding site present on most cells types 58. Therefore, when compared to VpL, NpL transduces endothelial cells with greater specificity. Further specificity of NpL could be obtained by vastly reducing the affinity to ephrin-B3 by two point mutations in NiV-G 59. In addition to mice, we anticipate NpL could be utilized in several different animals already known to be permissive to Nipah virus infection including pigs, Syrian golden hamsters, and primates 46. Further studies are warranted to identify cell types transduced with in vivo administration of NpL and identifying the optimal means of delivery.
MATERIALS AND METHODS
Cell culture
HEK293 cells were obtained from American Type Culture Collection (ATCC) (Manassas, VA) and HEK293T cells from Cell Genesys (San Francisco, CA); both were cultured in D10 media (Dulbecco’s modified eagle medium containing 1x Glutamax, 4.5 gm/L glucose, 5000 U/mL penicillin, 5000 μg/mL streptomycin (Invitrogen, Carlsbad, CA), containing 10% fetal bovine serum (Catalog # S11550, Atlanta Biologicals, Atlanta, GA). Human dermal microvascular endothelial cells (HDMECs) were acquired from Lonza (Walkersville, MD). Human umbilical vein endothelial cells (HUVECs) were isolated as described 60 (the Institutional Review Board at the Indiana University School of Medicine approved all protocols, and informed consent was obtained from the parents of newborns). Mouse lung microvascular cells (MLMECs) were obtained from Cell Biologics (Chicago, IL). All endothelial cells were cultured on collagen coated flasks/plates in EGM-2 BulletKit media (Lonza) with 10% fetal bovine serum (Atlanta Biologicals). We did not use the fetal bovine serum supplied with the EGM-2 BulletKit. Endothelial cells were used in experiments between passages 4–7.
Nipah protein trucations
The plasmid pTM1 61 encoding the Nipah fusion protein (F) or glycoprotein (G) were kind gifts from Dr. Paul Rota (Center for Disease Control, Atlanta, GA). Truncations were made by using PCR to amplify the Nipah F or G cDNAs at the desired lengths. Restriction enzyme cleavage sequences for PmlI in the 5′ primers and EcoRI (for Nipah F) or StuI (for Nipah G) in the 3′ primers allowed cloning into the lentiviral packaging plasmid pMD2.g 2. This cloning step also served to remove the cDNA sequence for VSV-G in pMD2.g. Primer sequences are available upon request.
Production and titer of lentiviruses
We used a third generation lentivirus with components split over several plasmids. A plasmid containing an HIV-based, self-inactivating lentiviral vector, pCSCGW (pCSC-SP-PW-GFP, 62) expressing eGFP from a CMV promoter served as the viral backbone. The remaining packaging plasmids included the following: pMDL, containing the HIV gag-pol gene; pMD2.g, containing envelope proteins (Nipah G, Nipah F, or VSV-G); and pRSV-REV, containing the HIV rev gene 2. HEK293T cells were seeded at 6.2 × 105 per well (6-well plates) or 1.2 × 107 cells per T175 flask in D10 media. The following day, the cells were transfected by the calcium phosphate method as previously described 63. The final transfection mixture had a DNA concentration of 25 μg/mL and CaCl2 concentration of 125 mM. The optimized plasmid molar ratios were 1:0.55:0.38:0.55 (CSCGW:MD2.g:MDL:REV) and 1:1:0.8:0.38:0.55 (CSCGW:NiV-GΔ33:NiV-FΔ25:MDL:REV). Cells were re-fed D10 media 16 hr post-transfection. Culture media containing the lentivirus was harvested 48 hrs post-transfection and filtered with a 0.45 μm cellulose acetate syringe filter to remove debris. When concentrating the lentivirus, filtered lentiviral-containing media was centrifuged at either 3,600 g for 16–18 hr (TX-400 rotor, Thermo, Asheville, NC) or at 100,000 g for 1 hr (SW40Ti rotor, Beckman Coulter, Indianapolis, IN). The supernatant was then removed and the pellet resuspended in one-hundredth of the original volume (120–250 μL). Aliquots of virus were stored at −80° C. For infectious titer determination, HEK293 cells were plated in 6-well plates at a concentration of 1 × 105 cells/well in D10 media. The following day, serial dilutions of lentivirus-containing media with a final concentration of 8 μg/mL polybrene was added to the cells in a final volume of 1 mL. Each dilution had two corresponding wells as replicates. In some experiments, virus was pre-incubated with soluble human ephrin-B2/Fc chimera (R&D Systems, Minneapolis, MN). The cells were re-fed fresh D10 media after 4 hr of virus exposure. Two days later, cells were harvested for flow cytometric analysis using a FACScan with Cellquest software (BD Biosciences, San Jose, CA). Forward and side scatter were used to gate single cells (10,000 counts). The FL1 channel was setup to count GFP positive cells by adjusting the gate such that it excludes >99.5% of an untransduced cell population. Transducing units per mL (TU/mL) were determined using the dilution yielding 2–25% GFP positive cells in the following equation: (dilution x %GFP positive × 100,000) / 100. All titers reported in the present study were determined from aliquots that underwent one freeze/thaw cycle. p24 assay. Serial dilutions of lentivirus-containing media were used with the HIV-1 p24ca Antigen Capture Assay Kit (AIDS Vaccine Program/SAIC-Frederick, Inc., Frederick, MD) to determine p24 concentrations. The manufacturer’s protocol was followed.
Serum stability assay
Unconcentrated, lentiviral-containing media with infectious titers of 2–5 × 106 TU/mL were added to an equal volume of mouse or human serum and incubated for 1 hr at 37° C. An equal volume of D10 media or heat inactivated serum (pre-incubation at 56° C for 1 hr) served as controls. Serial dilutions were used to perform a titer assay on HEK293 cells as described above. Titers obtained with serum treatments were divided by titers of the D10 controls to calculate percent remaining titer. The serum used in these experiments was from pooled donor samples and processed to preserve complement activity: human, Sigma (St. Louis, MO) catalog #S1764, CH50 = 30 U/mL; mouse, MP Biologicals (Solon, OH) catalog #55860, CH50 = 10 U/mL.
Western blotting of Nipah proteins in cell extracts and lentiviral particles
HEK293T cells were transfected with combinations of Nipah G and F plasmids using Fugene HD (Promega, Madison, WI) according to the manufacturer’s protocol. Harvested cells were lysed in RIPA buffer containing 1x Halt Protease Inhibitor Cocktail (Pierce, Rockford, IL). Protein concentrations were determined using a BCA assay kit (Pierce). Equal amounts of cell extract (20–25 μg) were separated on 4–12% Bis-Tris SDS-PAGE gels (Life Technologies, Grand Island, NY) under reducing conditions and transferred to 0.44 μm PVDF membranes. For lentiviral particles, equal amounts of measured p24 protein (350–400 ng) from concentrated stocks were used. EZ-Run pre-stained rec protein ladder (Fisher Scientific, Pittsburg, PA) was used as a molecular weight marker. The membranes were then incubated with blocking solution (50 mM Tris (pH 7.5), 150 mM NaCl, 0.1% Tween 20, and 5% dry milk) for 1 hr. Primary antibodies in blocking solution were incubated with the membranes overnight at 4° C at the following concentrations: rabbit anti-Nipah G, 1:10000; rabbit anti-Nipah F, 1:20000; rabbit anti-β-tubulin (Pierce), 1:2000. The Nipah antibodies 14 were kind gifts from Dr. Christopher Broder (Uniformed Services University, Bethesda, MD). HRP-conjugated goat anti-rabbit antibodies (R&D Systems) at 1:2000 in blocking solution were incubated with the membranes for 1 hour at room temperature. Proteins were visualized using ECL Plus reagent (GE Healthcare, Piscataway, NJ). When reprobing was necessary, membranes were stripped with Restore Western Stripping Buffer (Pierce). Densitometry was performed using ImageJ software (Ver. 1.46, National Institutes of Health, Bethesda, MD).
Western blotting of ephrin-B2 in endothelial cell extracts
HUVECs or HDMECs cell extracts were prepared, separated by SDS-PAGE, and transferred to PVDF as described above. Membranes were probed with anti-ephrin-B2 (H83, Santa Cruz Biotechnology, Dallas, TX), stripped, and then re-probed with anti-β-actin (Pierce). Densitometry was performed using ImageJ software.
Cell surface biotinylation
HEK293T cells in T25 flasks were transfected with Nipah G plasmids (with or without lentiviral packaging plasmids) using Fugene HD according to the manufacturer’s protocol. At 24 hr post-transfection, the cells were washed with Hank’s buffered saline (HBS) and then biotinylated with 0.5 mg/ml EZ-Link Sulfo-NHS-SS-Biotin (Pierce) for 15 min. After quenching with 0.1 M glycine in HBS, cells were harvested in RIPA buffer and protein concentration determined as described above. Between 125–150 μg of cell protein was incubated with 75 μl of a 1:1 slurry of NeutrAvidin Agarose beads (Pierce) for 1 hr. Beads were extensively washed and biotinylated proteins eluted by boiling in LDS sample buffer (Invitrogen) containing 75 mM β-mercapto ethanol. A western blot was performed as described above.
Cell fusion/toxicity assay
HEK293T cells in 6-well plates were transfected with a 1:1 ratio of NiV-G and F plasmids using Fugene HD (Promega, Madison, WI) according to the manufacturer’s protocol. In control wells or wells receiving Nipah G or F alone, pEGFP-C1 (Clontech, Mountain View, CA) was used to replace the missing plasmid in order to equalize the total amount of transfected plasmid. At 24 hr post-transfection, the cells were fixed with 4% paraformaldehyde (in PBS) for 1 hour and then stained overnight with Giemsa stain at room temperature. Stained cells were washed several times with distilled water and examined under a light microscope. To obtain a semi-quantitative value, two blinded observers examined five, 100X fields per treatment and estimated the percent area of cytopathic effects (CPE) in each field with the aid of a gridded ocular. These values were averaged together to obtain a “fusion index”. Representative digital images were obtained using an Olympus (Center Valley, PA) CKX-41 microscope and DP12 imaging system.
Statistics
Data were analyzed by two tailed t-test where applicable. P values under 0.05 were considered significant.
Acknowledgments
We thank Dr. Paul Rota (Center for Disease Control, Atlanta, GA) for plasmids containing the cDNA for NiV-G and NiV-F and Dr. Christopher Broder (Uniformed Services University, Bethesda, MD) for the NiV-G and NiV-F antibodies. We also thank the National Gene Vector Biorepository (Indianapolis, IN) for the lentiviral production plasmids. HUVECs were a kind gift from the laboratory of Dr. Merv Yoder (Indianapolis, IN). This work was supported by National Institutes of Health grant P30HL101337-02.
Footnotes
CONFLICT OF INTEREST
The authors have no financial conflicts of interest to disclose.
References
- 1.Sheridan C. Gene therapy finds its niche. Nature biotechnology. 2011;29(2):121–8. doi: 10.1038/nbt.1769. [DOI] [PubMed] [Google Scholar]
- 2.Zufferey R, Dull T, Mandel RJ, Bukovsky A, Quiroz D, Naldini L, et al. Self-inactivating lentivirus vector for safe and efficient in vivo gene delivery. Journal of virology. 1998;72(12):9873–80. doi: 10.1128/jvi.72.12.9873-9880.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramezani A, Hawley TS, Hawley RG. Combinatorial incorporation of enhancer-blocking components of the chicken beta-globin 5′HS4 and human T-cell receptor alpha/delta BEAD-1 insulators in self-inactivating retroviral vectors reduces their genotoxic potential. Stem Cells. 2008;26(12):3257–66. doi: 10.1634/stemcells.2008-0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewinski MK, Yamashita M, Emerman M, Ciuffi A, Marshall H, Crawford G, et al. Retroviral DNA integration: viral and cellular determinants of target-site selection. PLoS Pathog. 2006;2(6):e60. doi: 10.1371/journal.ppat.0020060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavazzana-Calvo M, Payen E, Negre O, Wang G, Hehir K, Fusil F, et al. Transfusion independence and HMGA2 activation after gene therapy of human beta-thalassaemia. Nature. 2010;467(7313):318–22. doi: 10.1038/nature09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levine BL, Humeau LM, Boyer J, MacGregor RR, Rebello T, Lu X, et al. Gene transfer in humans using a conditionally replicating lentiviral vector. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(46):17372–7. doi: 10.1073/pnas.0608138103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montini E, Cesana D, Schmidt M, Sanvito F, Bartholomae CC, Ranzani M, et al. The genotoxic potential of retroviral vectors is strongly modulated by vector design and integration site selection in a mouse model of HSC gene therapy. J Clin Invest. 2009;119(4):964–75. doi: 10.1172/JCI37630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bischof D, Cornetta K. Flexibility in cell targeting by pseudotyping lentiviral vectors. Methods Mol Biol. 2010;614:53–68. doi: 10.1007/978-1-60761-533-0_3. [DOI] [PubMed] [Google Scholar]
- 9.Rossetti M, Gregori S, Hauben E, Brown BD, Sergi LS, Naldini L, et al. HIV-1-Derived Lentiviral Vectors Directly Activate Plasmacytoid Dendritic Cells, Which in Turn Induce the Maturation of Myeloid Dendritic Cells. Human gene therapy. 2011 doi: 10.1089/hum.2010.085. [DOI] [PubMed] [Google Scholar]
- 10.Frecha C, Costa C, Levy C, Negre D, Russell SJ, Maisner A, et al. Efficient and stable transduction of resting B lymphocytes and primary chronic lymphocyte leukemia cells using measles virus gp displaying lentiviral vectors. Blood. 2009;114(15):3173–80. doi: 10.1182/blood-2009-05-220798. [DOI] [PubMed] [Google Scholar]
- 11.Funke S, Maisner A, Muhlebach MD, Koehl U, Grez M, Cattaneo R, et al. Targeted cell entry of lentiviral vectors. Mol Ther. 2008;16(8):1427–36. doi: 10.1038/mt.2008.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobayashi M, Iida A, Ueda Y, Hasegawa M. Pseudotyped lentivirus vectors derived from simian immunodeficiency virus SIVagm with envelope glycoproteins from paramyxovirus. Journal of virology. 2003;77(4):2607–14. doi: 10.1128/JVI.77.4.2607-2614.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Enkirch T, Kneissl S, Hoyler B, Ungerechts G, Stremmel W, Buchholz CJ, et al. Targeted lentiviral vectors pseudotyped with the Tupaia paramyxovirus glycoproteins. Gene therapy. 2012 doi: 10.1038/gt.2011.209. [DOI] [PubMed] [Google Scholar]
- 14.Khetawat D, Broder CC. A functional henipavirus envelope glycoprotein pseudotyped lentivirus assay system. Virol J. 2010;7:312. doi: 10.1186/1743-422X-7-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eaton BT, Broder CC, Middleton D, Wang LF. Hendra and Nipah viruses: different and dangerous. Nat Rev Microbiol. 2006;4(1):23–35. doi: 10.1038/nrmicro1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with Nipah virus. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2009;49(11):1743–8. doi: 10.1086/647951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonaparte MI, Dimitrov AS, Bossart KN, Crameri G, Mungall BA, Bishop KA, et al. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proceedings of the National Academy of Sciences of the United States of America. 2005;102(30):10652–7. doi: 10.1073/pnas.0504887102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Negrete OA, Levroney EL, Aguilar HC, Bertolotti-Ciarlet A, Nazarian R, Tajyar S, et al. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature. 2005;436(7049):401–5. doi: 10.1038/nature03838. [DOI] [PubMed] [Google Scholar]
- 19.Negrete OA, Wolf MC, Aguilar HC, Enterlein S, Wang W, Muhlberger E, et al. Two key residues in ephrinB3 are critical for its use as an alternative receptor for Nipah virus. PLoS Pathog. 2006;2(2):e7. doi: 10.1371/journal.ppat.0020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shin D, Garcia-Cardena G, Hayashi S, Gerety S, Asahara T, Stavrakis G, et al. Expression of ephrinB2 identifies a stable genetic difference between arterial and venous vascular smooth muscle as well as endothelial cells, and marks subsets of microvessels at sites of adult neovascularization. Dev Biol. 2001;230(2):139–50. doi: 10.1006/dbio.2000.9957. [DOI] [PubMed] [Google Scholar]
- 21.Foo SS, Turner CJ, Adams S, Compagni A, Aubyn D, Kogata N, et al. Ephrin-B2 controls cell motility and adhesion during blood-vessel-wall assembly. Cell. 2006;124(1):161–73. doi: 10.1016/j.cell.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 22.Ishikawa K, Tilemann L, Fish K, Hajjar RJ. Gene delivery methods in cardiac gene therapy. The journal of gene medicine. 2011;13(10):566–72. doi: 10.1002/jgm.1609. [DOI] [PubMed] [Google Scholar]
- 23.Du L, Dronadula N, Tanaka S, Dichek DA. Helper-dependent adenoviral vector achieves prolonged, stable expression of interleukin-10 in rabbit carotid arteries but does not limit early atherogenesis. Human gene therapy. 2011;22(8):959–68. doi: 10.1089/hum.2010.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song YK, Liu F, Liu D. Enhanced gene expression in mouse lung by prolonging the retention time of intravenously injected plasmid DNA. Gene therapy. 1998;5 (11):1531–7. doi: 10.1038/sj.gt.3300770. [DOI] [PubMed] [Google Scholar]
- 25.Djokovic D, Trindade A, Gigante J, Badenes M, Silva L, Liu R, et al. Combination of Dll4/Notch and Ephrin-B2/EphB4 targeted therapy is highly effective in disrupting tumor angiogenesis. BMC cancer. 2010;10:641. doi: 10.1186/1471-2407-10-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abengozar MA, de Frutos S, Ferreiro S, Soriano J, Perez-Martinez M, Olmeda D, et al. Blocking ephrinB2 with highly specific antibodies inhibits angiogenesis, lymphangiogenesis, and tumor growth. Blood. 2012;119(19):4565–76. doi: 10.1182/blood-2011-09-380006. [DOI] [PubMed] [Google Scholar]
- 27.De Palma M, Venneri MA, Naldini L. In vivo targeting of tumor endothelial cells by systemic delivery of lentiviral vectors. Human gene therapy. 2003;14(12):1193–206. doi: 10.1089/104303403322168028. [DOI] [PubMed] [Google Scholar]
- 28.Hohne M, Thaler S, Dudda JC, Groner B, Schnierle BS. Truncation of the human immunodeficiency virus-type-2 envelope glycoprotein allows efficient pseudotyping of murine leukemia virus retroviral vector particles. Virology. 1999;261(1):70–8. doi: 10.1006/viro.1999.9847. [DOI] [PubMed] [Google Scholar]
- 29.Indraccolo S, Minuzzo S, Feroli F, Mammano F, Calderazzo F, Chieco-Bianchi L, et al. Pseudotyping of Moloney leukemia virus-based retroviral vectors with simian immunodeficiency virus envelope leads to targeted infection of human CD4+ lymphoid cells. Gene therapy. 1998;5(2):209–17. doi: 10.1038/sj.gt.3300603. [DOI] [PubMed] [Google Scholar]
- 30.Weise C, Erbar S, Lamp B, Vogt C, Diederich S, Maisner A. Tyrosine residues in the cytoplasmic domains affect sorting and fusion activity of the Nipah virus glycoproteins in polarized epithelial cells. Journal of virology. 2010;84(15):7634–41. doi: 10.1128/JVI.02576-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diederich S, Moll M, Klenk HD, Maisner A. The nipah virus fusion protein is cleaved within the endosomal compartment. The Journal of biological chemistry. 2005;280(33):29899–903. doi: 10.1074/jbc.M504598200. [DOI] [PubMed] [Google Scholar]
- 32.Diederich S, Sauerhering L, Weis M, Altmeppen H, Schaschke N, Reinheckel T, et al. Activation of the Nipah virus fusion protein in MDCK cells is mediated by cathepsin B within the endosomal-recycling compartment. Journal of virology. 2012 doi: 10.1128/JVI.06628-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pager CT, Dutch RE. Cathepsin L is involved in proteolytic processing of the Hendra virus fusion protein. Journal of virology. 2005;79(20):12714–20. doi: 10.1128/JVI.79.20.12714-12720.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aguilar HC, Matreyek KA, Choi DY, Filone CM, Young S, Lee B. Polybasic KKR motif in the cytoplasmic tail of Nipah virus fusion protein modulates membrane fusion by inside-out signaling. Journal of virology. 2007;81(9):4520–32. doi: 10.1128/JVI.02205-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pernet O, Pohl C, Ainouze M, Kweder H, Buckland R. Nipah virus entry can occur by macropinocytosis. Virology. 2009;395(2):298–311. doi: 10.1016/j.virol.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 36.Vogt C, Eickmann M, Diederich S, Moll M, Maisner A. Endocytosis of the Nipah virus glycoproteins. Journal of virology. 2005;79(6):3865–72. doi: 10.1128/JVI.79.6.3865-3872.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mathieu C, Guillaume V, Sabine A, Ong KC, Wong KT, Legras-Lachuer C, et al. Lethal Nipah virus infection induces rapid overexpression of CXCL10. PLoS One. 2012;7(2):e32157. doi: 10.1371/journal.pone.0032157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Erbar S, Diederich S, Maisner A. Selective receptor expression restricts Nipah virus infection of endothelial cells. Virol J. 2008;5:142. doi: 10.1186/1743-422X-5-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adams RH, Wilkinson GA, Weiss C, Diella F, Gale NW, Deutsch U, et al. Roles of ephrinB ligands and EphB receptors in cardiovascular development: demarcation of arterial/venous domains, vascular morphogenesis, and sprouting angiogenesis. Genes & development. 1999;13(3):295–306. doi: 10.1101/gad.13.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang HU, Chen ZF, Anderson DJ. Molecular distinction and angiogenic interaction between embryonic arteries and veins revealed by ephrin-B2 and its receptor Eph-B4. Cell. 1998;93(5):741–53. doi: 10.1016/s0092-8674(00)81436-1. [DOI] [PubMed] [Google Scholar]
- 41.Mathieu C, Pohl C, Szecsi J, Trajkovic-Bodennec S, Devergnas S, Raoul H, et al. Nipah virus uses leukocytes for efficient dissemination within a host. Journal of virology. 2011;85(15):7863–71. doi: 10.1128/JVI.00549-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ailles L, Schmidt M, Santoni de Sio FR, Glimm H, Cavalieri S, Bruno S, et al. Molecular evidence of lentiviral vector-mediated gene transfer into human self-renewing, multi-potent, long-term NOD/SCID repopulating hematopoietic cells. Mol Ther. 2002;6(5):615–26. [PubMed] [Google Scholar]
- 43.Millington M, Arndt A, Boyd M, Applegate T, Shen S. Towards a clinically relevant lentiviral transduction protocol for primary human CD34 hematopoietic stem/progenitor cells. PLoS One. 2009;4(7):e6461. doi: 10.1371/journal.pone.0006461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sandrin V, Cosset FL. Intracellular versus cell surface assembly of retroviral pseudotypes is determined by the cellular localization of the viral glycoprotein, its capacity to interact with Gag, and the expression of the Nef protein. The Journal of biological chemistry. 2006;281(1):528–42. doi: 10.1074/jbc.M506070200. [DOI] [PubMed] [Google Scholar]
- 45.Pelchen-Matthews A, Kramer B, Marsh M. Infectious HIV-1 assembles in late endosomes in primary macrophages. J Cell Biol. 2003;162(3):443–55. doi: 10.1083/jcb.200304008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williamson MM, Torres-Velez FJ. Henipavirus: a review of laboratory animal pathology. Vet Pathol. 2010;47(5):871–80. doi: 10.1177/0300985810378648. [DOI] [PubMed] [Google Scholar]
- 47.Maisner A, Neufeld J, Weingartl H. Organ- and endotheliotropism of Nipah virus infections in vivo and in vitro. Thromb Haemost. 2009;102(6):1014–23. doi: 10.1160/TH09-05-0310. [DOI] [PubMed] [Google Scholar]
- 48.Ryan-Poirier KA, Kawaoka Y. Alpha 2-macroglobulin is the major neutralizing inhibitor of influenza A virus in pig serum. Virology. 1993;193(2):974–6. doi: 10.1006/viro.1993.1208. [DOI] [PubMed] [Google Scholar]
- 49.Cwach KT, Sandbulte HR, Klonoski JM, Huber VC. Contribution of murine innate serum inhibitors toward interference within influenza virus immune assays. Influenza Other Respi Viruses. 2012;6(2):127–35. doi: 10.1111/j.1750-2659.2011.00283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kong D, Wen Z, Su H, Ge J, Chen W, Wang X, et al. Newcastle disease virus-vectored Nipah encephalitis vaccines induce B and T cell responses in mice and long-lasting neutralizing antibodies in pigs. Virology. 2012;432(2):327–35. doi: 10.1016/j.virol.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 51.Guillaume V, Contamin H, Loth P, Georges-Courbot MC, Lefeuvre A, Marianneau P, et al. Nipah virus: vaccination and passive protection studies in a hamster model. Journal of virology. 2004;78(2):834–40. doi: 10.1128/JVI.78.2.834-840.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weingartl HM, Berhane Y, Caswell JL, Loosmore S, Audonnet JC, Roth JA, et al. Recombinant nipah virus vaccines protect pigs against challenge. Journal of virology. 2006;80(16):7929–38. doi: 10.1128/JVI.00263-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chan YP, Lu M, Dutta S, Yan L, Barr J, Flora M, et al. Biochemical, conformational, and immunogenic analysis of soluble trimeric forms of henipavirus fusion glycoproteins. Journal of virology. 2012;86(21):11457–71. doi: 10.1128/JVI.01318-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Breckpot K, Escors D, Arce F, Lopes L, Karwacz K, Van Lint S, et al. HIV-1 lentiviral vector immunogenicity is mediated by Toll-like receptor 3 (TLR3) and TLR7. Journal of virology. 2010;84(11):5627–36. doi: 10.1128/JVI.00014-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Palomares K, Vigant F, Van Handel B, Pernet O, Chikere K, Hong P, et al. Nipah virus envelope-pseudotyped lentiviruses efficiently target ephrinB2-positive stem cell populations in vitro and bypass the liver sink when administered in vivo. Journal of virology. 2013;87(4):2094–108. doi: 10.1128/JVI.02032-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nakada M, Anderson EM, Demuth T, Nakada S, Reavie LB, Drake KL, et al. The phosphorylation of ephrin-B2 ligand promotes glioma cell migration and invasion. Int J Cancer. 2010;126(5):1155–65. doi: 10.1002/ijc.24849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alam SM, Fujimoto J, Jahan I, Sato E, Tamaya T. Coexpression of EphB4 and ephrinB2 in tumor advancement of uterine cervical cancers. Gynecologic oncology. 2009;114(1):84–8. doi: 10.1016/j.ygyno.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 58.Coil DA, Miller AD. Phosphatidylserine is not the cell surface receptor for vesicular stomatitis virus. Journal of virology. 2004;78(20):10920–6. doi: 10.1128/JVI.78.20.10920-10926.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Negrete OA, Chu D, Aguilar HC, Lee B. Single amino acid changes in the Nipah and Hendra virus attachment glycoproteins distinguish ephrinB2 from ephrinB3 usage. Journal of virology. 2007;81(19):10804–14. doi: 10.1128/JVI.00999-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ingram DA, Mead LE, Tanaka H, Meade V, Fenoglio A, Mortell K, et al. Identification of a novel hierarchy of endothelial progenitor cells using human peripheral and umbilical cord blood. Blood. 2004;104(9):2752–60. doi: 10.1182/blood-2004-04-1396. [DOI] [PubMed] [Google Scholar]
- 61.Tamin A, Harcourt BH, Ksiazek TG, Rollin PE, Bellini WJ, Rota PA. Functional properties of the fusion and attachment glycoproteins of Nipah virus. Virology. 2002;296(1):190–200. doi: 10.1006/viro.2002.1418. [DOI] [PubMed] [Google Scholar]
- 62.Marr RA, Guan H, Rockenstein E, Kindy M, Gage FH, Verma I, et al. Neprilysin regulates amyloid Beta peptide levels. J Mol Neurosci. 2004;22(1–2):5–11. doi: 10.1385/JMN:22:1-2:5. [DOI] [PubMed] [Google Scholar]
- 63.Kahl CA, Marsh J, Fyffe J, Sanders DA, Cornetta K. Human immunodeficiency virus type 1-derived lentivirus vectors pseudotyped with envelope glycoproteins derived from Ross River virus and Semliki Forest virus. Journal of virology. 2004;78 (3):1421–30. doi: 10.1128/JVI.78.3.1421-1430.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]