Introduction
Proper lighting is necessary for vision and to carry out one’s daily activities. This aspect of light – light for vision – is well known by the general public and health professionals. What is less well appreciated is the large and growing body of scientific literature on light as a therapeutic agent. Indeed, although much has been documented over the past decades about its therapeutic uses, light is rarely prescribed by physicians and other health care providers. In part this is because much is yet to be understood about the optimum characteristics of light affecting our health and well-being. Published research studies have employed a wide range of light sources, quantities, spectra, and delivery schedules, without yielding a consensus as to how to optimally provide this treatment. However, under-use of light as therapy is also due to the fact that light is naturally available and thus un-patentable, making it unappealing as a research or marketing venue for industries.1
Sleep disorders and depression are extremely common in older persons, and in research trials, light therapy has shown some benefits for treating these disorders. Although drug treatments are available for both conditions, in each case the available drugs fail to work a significant proportion of the time and carry with them considerable risk of adverse effects. Therefore, health care providers treating older persons would benefit from considering light therapy as an alternative for selected patients with sleep disorders or depression. In this paper we review the physiology, scientific evidence, therapeutic uses, and cautions regarding light as a therapeutic agent for these common geriatric conditions, and provide recommendations for clinicians.
Physiology of Light as Therapy
The physiological foundation of light as therapy for sleep/wake cycle disturbances is based on the understanding that living organisms have adapted to the daily rotation of the earth by developing biological rhythms that repeat at approximately 24-hour intervals (i.e., circadian rhythms); the most prominent physiological manifestations of these are the sleep/wake cycle and diurnal variations in melatonin secretion, cortisol, and core body temperature. The regulation of melatonin and temperature is controlled by the suprachiasmatic nucleus (SCN) in the hypothalamus of the brain, which fluctuates cyclically but needs an external stimulus to maintain a consistent 24-hour cycle. That key external stimulus is variation in light and darkness over the course of the day, and, in particular, exposure to high light levels during the morning hours. These cyclical changes in light levels in turn synchronize the SCN to the 24-hour day, assuring that the timing of physiological rhythms, so that we are asleep during nighttime hours and awake during daytime hours.
Impairment of these SCN-mediated circadian rhythms becomes increasingly common with advancing age, diminished health, and Alzheimer’s disease, thereby contributing to the high prevalence of sleep disturbances in these populations.2–4 Older adults have shown depressed melatonin rhythm amplitudes and alterations in the body’s temperature cycle, which may explain the sleep disorders commonly found in these individuals.5 Thus, the mechanism of light therapy for sleep disorders could be via stimulation of the SCN, effectively correcting the timing and/or strengthening the amplitude body’s circadian cycles.
The physiological basis by which light affects mood is less well established. Light therapy is, however, a recognized and consistently demonstrated treatment for seasonal affective disorder (SAD). Although the mechanisms associated with positive effects of light in alleviating SAD symptoms are still unknown, it is believed that the circadian system might be involved. One line of research hypothesizes that the late dawn in winter results in a delayed circadian system and that morning light is an effective treatment to maintain circadian rhythms entrained to the solar day. Another research model suggests that long nights during winter months increase melatonin production. Researchers have established that melatonin in the brain is synthesized by the pineal gland from N-acetyl-serotonin, in response to signals that reaches the SCN via the retinohypothalamic tract. The SCN’s postsynaptic fibers release norepinephrine, thus it is logical to hypothesize that alterations in this cycle could affect mood by influencing the serotoninergic and/or norepinephrinergic system.6 However, research on melatonin levels in both young and older adults has failed to identify a consistent relationship between either the amount or the timing of melatonin secretion and depression.6–8 Therefore, although the ameliorative effects of light on seasonal depression are largely accepted, the mechanism of action is not well understood.
Clinical Effectiveness of Light Therapy in Older Persons
Over two dozen studies have evaluated the efficacy of light therapy in the treatment of circadian sleep disorders and/or depression (including SAD) in older persons. Many of the studies are small, however, and are limited by their design. In addition, wide protocol variation exists in terms of the treatment applied. For instance, in studies reviewed for this article, the duration of treatment ranged from 30 minutes to 8 hours a day; the light levels from 200 to 10,000 lux; the spectrum from polychromatic white light to nearly monochromatic green or blue light; the timing from morning to evening to all day; and the intervention length from days to weeks. Tables 2 and 3 describe each study, and in the following paragraphs we attempt to interpret the overall state of evidence.
Table 2.
Summary of Evidence of Effectiveness for Non-seasonal Depression in Older Persons
| Study | Design | Treatment | Control Procedure | Depression Measure(s)b,c,d,e | Findingsa | ||||
|---|---|---|---|---|---|---|---|---|---|
| Population (n; mean age; depression; circadian disorder; institutional setting; dementia) | Intensity (lux); Duration (hours) | Spectrum | Timing | Adjunct treatment | |||||
| Loving et al., 200551 | Randomized, controlled, parallel-groups trial | 41;68; Y; -; N; Y | 8,500; 1 | White | Morning, mid-day, or evening | Partial sleep deprivation | 10 lux red light | GDS, SIGH-SAD, HAM-D | No difference between treatment and control groups |
| Loving et al., 200552 | Randomized, controlled, parallel-groups trial | 17; 68; Y; Y; N; Y | 1,200; 1 | Green | Within 1 h of waking | Partial sleep deprivation | 10 lux red light | GDS, SIGH-SAD, HAM-D | No difference between treatment and control groups |
| Lyketsos et al., 199953 | Randomized, controlled, crossover trial | 15; 81; N; N; Y; Y | 10,000; 1 | ‘Full spectrum’ | Morning | - | Dim, low-frequency, blinking light | CSDD | No difference between treatment and control groups |
| Ouslander et al., 200656 | Controlled, parallel-groups trial | 77; 84; N; N; Y; N | 1,467; 2 | ‘Full spectrum’ | Between 5pm and 8pm | Exercise, noise reduction, nighttime routine | Usual care | GDS | No difference between treatment and control groups |
| Sumaya et al., 200129 | Randomized, controlled crossover trial | 11; 84; Y; -; Y; N | 10,000; 0.5 | White | Between 9am and 12:30pm | - | 300 lux light | GDS | Greater improvement in treatment group* |
| Tsai et al., 200462 | Randomized, controlled, parallel-groups trial | 30; 75; Y; -; Y; N | 5,000; 0.8 | White | Between 9am and 12:00 pm | - | Usual care | GDS | Greater improvement in treatment group* |
| Yamada at al., 199563 | Randomized, controlled, parallel-groups trial | 18; -; Y;-; Y; - | 2,500; 2 | White | Morning or Evening | - | 500 lux light | HAM-D | Greater improvement in treatment group, irrespective of timing of treatment* |
Significant differences marked with an asterisk (*)
GDS Geriatric Depression Scale
SIGH-SAD Hamilton Depression Rating Scale – Seasonal Affective Disorder Version
HAM-D Hamilton Depression Rating Scale
CSDD Cornell Scale for Depression in Dementia
Table 3.
Comparison and Contrast between Use of Light for Vision and for Therapy
| Parameter | Light for Vision | Light as Therapy |
|---|---|---|
| Intensity needed for effectiveness |
|
Varies with spectrum, but typical recommendation is at least 2500 lux of full-spectrum light at the cornea |
| Duration required for effectiveness | Very short (eye registers visual image in less than a second) | Longer; varies by light exposure from 5 minutes (for bright sunlight to more than an hour (for typical “light box” therapy) |
| Wavelength (in nanometers) to which brain is sensitive | A broad range (350–750 nm) is needed for vision; peak spectral sensitivity is at mid wavelength (555 nm) | 450 – 480 nm (blue light) |
| Timing of exposure | Unimportant | Important |
| Contrast needed for optimal function | Spatial contrast is important (differing light/dark patterns at the same time) | Temporal contrast is important (contrast in amount of exposure across different times during a 24-hour day) |
| Evenness of illumination | Preferred for optimal vision | Not important, though one study showed that light coming from above the horizon (reaching the lower retina) is more effective in suppressing melatonin |
| Glare | Interferes with visual function | Interferes with treatment acceptability |
Sleep Disorders
A large body of literature substantiates the effectiveness of light as therapy in laboratory settings using young persons as subjects. In general, these studies are conducted to better understand the underlying mechanisms through which light affects the circadian system. Although some laboratory studies have included older adults as subjects, very few studies have evaluated light as therapy for older persons in non-laboratory settings. The available literature on light as a therapy for older adults in community settings is less consistent in terms of its efficacy findings, likely due to the shortcomings described above. One Cochrane review examined the effects of light therapy on sleep, behavior, and mood in older adults with dementia. Of only five studies that met the reviewers inclusion criteria, only three were ultimately reviewed due to inappropriate study methodologies. The three articles that were reviewed did not reveal any systematic benefits of light therapy for individuals with dementia.9 Using less stringent inclusion criteria, we identified 21 published studies evaluating the impact of light therapy on sleep quality and efficiency in older persons (Table 1). Many involved small samples; six included 10 or fewer participants. The majority (15 studies) specifically targeted persons with dementia, and three used depression as a selection criterion. Overall, 14 identified significant improvement in one or more clinical outcomes, whereas seven did not. Improved outcomes appeared to be associated with the amount of light exposure: Of the 19 studies reporting these data, seven of nine (78%) with exposures exceeding 6,000 lux-hours had positive results, compared with five of ten (50%) with lower exposure levels. In contrast, no pattern of association was noted between clinical improvement and dementia status, depression status, or the timing of light therapy. The latter finding is particularly noteworthy, because much of the literature on circadian rhythms states that the majority of older persons are phase advanced and would benefit more from evening than morning light; however, this belief is not supported by the results of published clinical studies. In conclusion, the findings on light therapy and sleep in older persons are mixed but overall suggest a favorable effect in older persons.
Table 1.
Summary of Clinical Studies of Light Therapy for Sleep and Circadian Rhythm Disorders in Older Persons
| Study | Design | Treatment | Control Procedure | Sleep or Circadian Rhythm Measure(s)c | Major Findingsa | ||||
|---|---|---|---|---|---|---|---|---|---|
| Population (n; mean age; depression; circadian disorder; institutional setting; dementia) | Intensity (lux); Duration (hours) | Spectrum | Timing | Adjunct treatment | |||||
| Alessi et al., 200544 | Randomized, controlled, parallel-groups trial | 62; 88; N; Y; Y; N | ≥10,00; 0.5 | Sunlight | Generally in morning | Exercise, nighttime routine, noise reduction | Usual care | Actigraphy, oximetry, observations | Reduction in nighttime awakening duration and daytime sleeping in treatment group.* No other differences between groups. |
| Ancoli-Israel et al., 200225 | Randomized, controlled, parallel-groups trial | 77; 86; N; N; Y; Y | 2,500; 2 | White | 9:30–11:30am or 5:30–7:30pm | - | 50 lux red light or daytime sleep restriction | Actigraphy | Phase delay and increased mesor in morning light treatment group.* Phase delay in evening light treatment group. No other differences between groups. |
| Ancoli-Israel et al., 200345 | Randomized, controlled parallel-groups trial | 61; 82; N; N; Y; Y | 2,500; 2 | ‘Full spectrum’ | 9:30–11:30 am or 5:30–7:30pm | - | <300 lux red light | Actigraphy | Increase in maximum sleep bout duration in both treatment groups. No other differences between groups. |
| Colenda et al., 199746 | Pre-post trial | 5; 76; -; Y; N; Y | 2,000; 2 | White | Upon awakening – between 7am and 9:30am | - | - | Actigraphy | No consistent effects across subjects. |
| Dowling et al., 200547 | Randomized, controlled, parallel groups trial | 70; 84; -; Y; Y; Y | ≥2,500; 1 | Sunlight or white light | 9:30–10:30 am or 3:30–4:30 pm | - | Usual care | Actigraphy | Phase delay in control group.* No other differences between the morning and afternoon groups, or control group. |
| Fetveit et al., 200348 | Pre-post trial | 11; 86; N; Y; Y; Y | 6,000–8,000; 2 | White | Between 8am and 11am | - | - | Actigraphy, Sleep-wake questionnaire | Improved sleep efficiency and sleep-wake score, reduced total wake time, sleep onset latency, and mesor in treatment group.* No other differences between groups. |
| Figueiro et al., 200232 | Controlled, crossover trial | 4; -; -; -; Y; Y | 30; 2 | Blue | 6pm–8pm | - | 30 lux red light | Actigraphy, body temperature, nurse observation | Phase delay and improved sleep-wakefulness in treatment period. |
| Kobayashi et al., 200149 | Pre-post trial | 10; 81; -; Y; Y; N | 8,000; 1 | White | 11:30am –12:30pm | - | - | Nurse ratings of sleep and behavior | Improved clinical ratings of sleep-wakefulness in 80% of subjects.* |
| Koyama et al., 199950 | Baseline-intervention trial | 6; 86; N; Y; Y; Y | 4,000; unstated | White | Late morning | - | - | Nurse ratings of sleep and behavior | Phase advance, increased nighttime sleep, and decreased daytime sleep in 50% of subjects. |
| Loving et al., 200551 | Randomized, controlled, parallel-groups trial | 41;68; Y; -; N; Y | 8,500; 1 | White | Morning, mid-day, or evening | Partial sleep deprivation | 10 lux red light | Urinary melatonin, actigraphy, sleep log | Phase advance in morning light treatment group and in females in all treatment groups.*b No other differences between groups. |
| Loving et al., 200552 | Randomized, controlled, parallel-groups trial | 17; 68; Y; Y; N; Y | 1,200; 1 | Green | Within 1 h of waking | Partial sleep deprivation | 10 lux red light | Actigraphy, sleep log | No differences between groups. |
| Lyketsos et al., 199953 | Randomized, controlled, crossover trial | 15; 81; N; N; Y; Y | 10,000; 1 | ‘Full spectrum’ | Morning | - | Dim, low-frequency, blinking light | Sleep log | Greater increase in sleep time in treatment period. |
| Martiny et al., 200415 | Randomized, controlled, single-blind, parallel groups trial | 48; 46; Y; -; N; N | 10,000; 1 | White | Upon awakening, but by 10am | sertraline | 50 lux dim red light + sertraline | Sleep log | Greater increase in sleep duration in control group.* Later wake-up time in treatment group.* |
| Mishima et al., 199854 | Randomized, controlled, crossover trial | 22; 78; -; Y; Y; Y | 5,000–8,000; 2 | White | 9am–11am | - | 300 lux dim light | Actigraphy | Decrease in nighttime activity in treatment period.* |
| Mishima et al., 199455 | Pre-post trial | 14; 75; -; Y; Y; Y | 3,000–5,000; 2 | ‘Full spectrum’ | 9am–11am | - | Usual care | Nurse observation, serum melatonin | Increase in total and nocturnal sleep time, and decrease in daytime sleep time, in treatment group.* No changes in acrophase. |
| Ouslander et al., 200656 | Controlled, parallel-groups trial | 77; 84; N; N; Y; N | 1,467; 2 | ‘Full spectrum’ | Between 5pm and 8pm | Exercise, noise reduction, nighttime routine | Usual care | Actigraphy, oximetry, observation, polysomnography | Decrease in daytime sleeping in treatment group.* No other differences between groups. |
| Rosenthal et al., 199057 | Randomized, controlled, crossover trial | 20; -; N; Y; N; N | 2,500; 2 | ‘Full spectrum’ | Between 6am and 9am | Dark goggles in evening | 300 lux light and clear goggles in evening | Body temperature, questionnaire | Phase advance and improved morning alertness and earlier sleep time in treatment period.* |
| Satlin et al., 199258 | Pre-post trial | 10; 70; -; Y; Y; Y | 1,500–2,000; 2 | White | 7pm – 9pm | - | - | Nurse ratings of sleep-wakefulness disturbances and agitation, Actigraphy | Clinical improvement in sleep-wakefulness*, nocturnal activity*, and intradaily variability. Phase advance. |
| Skjerve et al., 200459 | Pre-post trial | 10; 79; -; Y; Y; Y | 5,000–8,000; 0.75 | White | Between 8am and 10am | - | - | Actigraphy, SWD | Phase advance. No other differences between treatments. |
| Suhner et al., 200260 | Pre-post trial | 15; 72; N; Y; N; N | 4,000; 2 | White | 8pm–11pm | - | - | Body temperature, sleep log, sleep quality | Phase delay in treatment period*. Effect of treatment diminished post-treatment. |
| Van Someren et al., 199761 | Pre-post trial | 22; 79; -; -; Y; Y | 1,136; continuous | White | All day | - | - | Actigraphy | Increase in interdaily stability and decrease in sleep fragmentation.* |
Significant differences marked with an asterisk (*)
Authors point out that this data is of low-quality, due to a low number of usable cases for analysis.
SWD = Short Scale for Sleep-Wake Disturbances
Depression
There is a large body of literature on effectiveness of light therapy on SAD in younger adults, and a modest body of literature supporting its effectiveness in other depressive disorders. A 2004 Cochrane review of randomized controlled trials comparing bright light therapy to inactive placebo treatments found that, among 20 methodologically high-quality studies reviewed, SAD was alleviated to a greater extent when individuals were exposed to bright light versus placebo treatments (standardized mean difference −0.90, 95% CI −1.50 to −0.31).10 The effects of light appear to extend beyond SAD: A review of 20 studies of light therapy for non-seasonal depression found that bright light therapy was effective in reducing non-seasonal depressive symptoms, with an average effect size of .53 (considered “moderate”) across studies.1 The findings have been more consistently positive in studies of light therapy as an adjunct to pharmaceutical treatment for non-seasonal depression in adults (although not necessarily ‘older’ adults).11–13 In one randomized double-blind controlled trial, for example, participants received daily dosages of 50 mg of the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline, combined with either bright light treatment or placebo dim light; participants in the bright light adjunct group experienced greater reductions in depressive symptoms compared to those in the placebo group (p<0.05).11,13
We identified seven published studies of the impact of light therapy on depressive symptoms in older persons (Table 2). Of these, three reported significant improvement with light therapy, and four did not. While the small number of studies (and the relatively modest samples in all published studies) renders any conclusions tentative, reported improvement does not appear to be associated with the total amount of light exposure or the timing of the therapy in the diurnal cycle. Of possible importance is the fact that three of the four negative studies specifically selected persons with dementia, whereas all three of the positive studies studied more general populations; if valid, this conclusion could be the result of either ineffectiveness or of insensitive measures, since depression is difficult to diagnose and measure in persons with dementia. In conclusion, existing studies are inconclusive but suggest that light may have a modest effect on depressive symptoms in older persons, particularly those who do not have dementia. In addition, the strong findings in several studies of bright light as an adjunct to pharmacotherapy, which, although not exclusively conducted in the elderly, included older persons, suggest that this role may be particularly appropriate until further data are available on light as a primary therapeutic agent.12–15
Dose and Application
In this section we review what is known about the influence of light levels, duration, timing, and spectrum of light therapy on clinical outcomes, and – although many questions remain – provide tentative therapeutic recommendations. In general, the optimal characteristics of light as therapy differ from those for vision. Table 3 summarizes optimal lighting characteristics for both the visual and circadian systems.
Quantity of light
The light levels required for a therapeutic effect are considerably higher than that needed for vision.16 In general, the recommended minimum light therapy is 2,500 lux of white, broadband light at the cornea for a 2-hour exposure or as much as 10,000 lux for a 30-minute exposure. If natural light is used, a rough guideline is that 2,500 lux is equivalent to being outside on a cloudy day and 10,000 lux to being outdoors on a sunny but not excessively bright day (outdoor light levels as high as 100,000 lux have been recorded). The higher the light level provided, the more attention must be given to glare reduction. High light levels can result in discomfort, and thus, limit retinal light exposure due to squinting and gaze aversion. Studies conducted in very controlled laboratory conditions showed that much lower light levels (about 100 lux at the cornea of a 4100K fluorescent light) applied for 6.5 hours can phase shift the circadian system of humans.17 However, no studies to date have been able to clearly demonstrate that light levels this low are enough to activate the circadian system outside laboratory conditions. More importantly, light levels used in light therapy for older persons should account for the reduced retinal illuminance due to changes in the aging eye.
Spectrum
Until recently, little was known about the spectral sensitivity of the circadian system, that is, the maximally effective light color. However, a series of recent studies have shown that blue light (peaking between 440 and 460nm) is maximally effective in suppressing melatonin.18–22 The practical implication of these data is displayed in Table 4, which compares the ability of commercial light sources to stimulate the visual and circadian systems.
Table 4.
Relative Strength of Selected Common Light Sources in Stimulating the Visual and Circadian Systems
| Type of Light Bulb | Relative Stimulation Per Watt | |
|---|---|---|
| To the Visual System [lumens/watt] | To the Circadian System [circadian stimulus/watt] | |
| Fluorescent 3000K | 100 | 74 |
| Fluorescent 7500K | 100 | 157 |
| Incandescent | 12 | 12 |
| Daylight 6500K | 70 | 133 |
| Clear Mercury (Hg) | 45 | 18 |
| Blue LED (470 nm) | 8 15 |
223 418 |
Timing of exposure
Although it is well established that timing of exposure is critical in altering circadian rhythms, the optimal timing of light therapy remains controversial. In general, light therapy should be applied in the evening to produce a phase advance, and in the morning to produce a phase delay.21,23–24 However, results contradicting laboratory findings have been reported (e.g. morning light causing a phase delay).25
Duration of exposure
Duration of exposure needed to impact the circadian system is greater than that needed to impact the visual system. The visual system will respond in milliseconds, while it might take several minutes to days before one can detect the impact of light on circadian rhythms.
Light Patterns and history
Finally, vision requires simultaneous light/dark contrast across the visual field, whereas light therapy appears to require light-dark contrast across time, especially to affect circadian rhythms. Moreover, it appears that light reaching the lower retina is more effective for the circadian system than light reaching the upper retina.
Proposed Light Therapy for Clinical Applications
In the absence of consistent findings, the following as a clinical approach should be considered:
Provide white light sources with bluish tint (i.e., 7,500 K fluorescent light bulb) that provide at least 1,000 lux at the eye during daytime hours. If these light levels are considered too high, try to use lower lux blue light delivered via a light box. In this case, the person will have to sit in front of the lights for a certain amount of time daily.
Provide the therapy at the time that is most convenient for the patient, since consistency is important, especially in influencing circadian rhythms. If the circadian timing of the patient is not known, morning light (after wakening) should be able to at least maintain entrainment, which may be just what the patient needs.
If convenience is not an issue, ask if the patient tends to be more tired in the morning or in the late afternoon/early evening, and provide the light therapy during that time interval.
-
If feasible (e.g. by providing high light levels (at least 1,000 lux at the cornea) of environmental bluish white light), consider all-daytime (e.g., 7 a.m. – 8 p.m.) bright light, coupled with dim, warm-color light (e.g., incandescent light bulbs) at night.
Clinical trials of individualized timing, such as that suggested here, remain to be conducted in older persons.
Available Treatment Modalities
Light boxes (Figure 1) are the most common treatment devices available on the market. They are rectangular fixtures that house several light bulbs, usually fluorescent tubes, and that require the user to sit facing them for between half an hour and two hours. In general, light boxes provide a high amount of light (from 2,500 to 10,000 lux at the cornea). The main drawbacks of such devices are the necessity to remain in one place, and the fact that some users experience discomfort from having to face in the general direction of the bright light (a drawback of all light treatments). Most experts recommend the 10,000 lux box, because the recommended duration of exposure is less.
Figure 1.

Light boxes are currently the most common delivery system for light therapy. They are inexpensive and can provide high dosage levels and controlled spectra of light; however, they require the patient to remain in the same location for up to two hours. Photos from http://www.bio-light.com/lightsproducts.html and http://www.outsidein.co.uk/gallery.htm. Used with permission.
A similar product is the high intensity desk lamp (Figure 2). If oriented properly in relation to the eyes (i.e., at the manufacturer’s recommended distance and in front of the user), a desk lamp can produce up to 10,000 lux exposure at the cornea. As with other light sources, visual discomfort can result; the advantage is that the desk lamp can be less obtrusive for office or home use.
Figure 2.
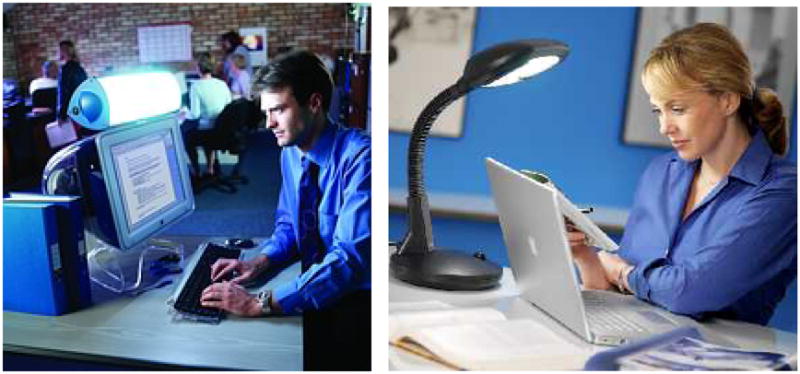
The high intensity desk lamp comes in a variety of shapes and styles, providing a less obtrusive alternative to the light box. Photos from http://www.outsidein.co.uk/gallery.htm. Used with permission.
Light visors (Figure 3) provide a portable alternative to light boxes and are comprised of a head-mounted light source that resembles a tennis visor. The visor is designed to give people mobility during light sessions and portability for travel; however, it can be cumbersome for some users. Because the light source is close to the eye (and preferentially reaches the more sensitive lower portion of the retina), it requires lower intensities, with a 3,000 lux to produce benefits comparable to a 10,000 lux light box.
Figure 3.

Portable light visors allow users to move around and travel while being exposed to therapeutic light levels. The main disadvantage, if present, is wearer discomfort. Photo from http://www.outsidein.co.uk/gallery.htm. Used with permission.
Until recently, all of the available light boxes, visors and desk lamps used “full-spectrum” light. More recently, however, products have become available that use a nearly monochromatic light source, the light emitting diode (LED). Some use blue LEDs, peaking at 470 nm, while others use blue/green LEDs, peaking at about 500 nm. Because the peak wavelength of the blue LEDs is close to the maximum sensitivity of the circadian system, much lower light levels can be used, though not all the manufacturers are taking advantage of this feature. Light boxes using blue LEDs typically provide about 400 lux at the cornea; light visors using the blue/green LED emit intensities ranging from 500 and 12,000 lux.
A low-tech alternative to commercial products would be for an older person to spend 20–30 minutes outdoors daily, preferably at about the same time each morning. Even an overcast day will produce 2,500 lux at the cornea, and bright sunshine can produce exposures greater than 10,000 lux at the cornea.
The dawn simulator is marketed primarily for people with seasonal affective disorder; however, it could be useful for people who are phase delayed (i.e., have trouble getting up in the morning). These use incandescent light bulbs and are programmed to gradually increase the light levels in the morning hours, simulating the sunrise. While the evidence of effectiveness is largely anecdotal, and light intensities achieved are often below those of light boxes, lamps, or visors, dawn simulators may have therapeutic value in certain sleep disorders and/or as a supplement to other lighting treatment modalities.
An experimental, not-yet-proven method of applying light therapy is the use of even, therapeutic light intensities throughout an entire room. However, when high levels of ambient lighting are used in facility common areas, the cost can be high and the light levels can be uncomfortable to some individuals; use of skylights and/or monochromatic blue light sources may reduce these problems. Exposure of all individuals rather than targeting affected patients is also a significant drawback of light therapy in public areas; an intriguing alternative would be the design of systems for use in residential areas, such as private rooms in long-term care facilities or the living areas of private homes.
Adverse Effects
One of the advantages of light as therapy is that it appears to be relatively free of serious adverse effects. Theoretically plausible potential risks include retinal damage, the induction of mania and/or agitation, heightened photosensitivity, and general somatic and psychosomatic complaints (headache, nausea, jitteriness, anxiety). The available randomized trials indicate, however, that the prevalence of major adverse effects are virtually nil, and that minor adverse effects occur at similar or only modestly increased rates among users in comparison to matched controls.
Because exposure to direct sunlight can lead to cataracts and retinal damage, and both ultraviolet radiation and high levels of short-wavelength light can damage the lens and the retina, concern has been raised about the short- and long-term effects of light therapy on the eye.26 To date, such concerns have only been speculative; trials of up to 10,000 lux have not documented eye damage as a result of light therapy, in part because ultraviolet radiation-blocking filters or coatings are applied to most light fixtures.13,27–28 In spite of negative research findings, many experts recommend, as a precautionary measure, excluding patients with degenerative retinal diseases,26,29–30 as well as those without a lens,26 from light therapy.
Some experts are particularly concerned that blue light exposure may be a hazard, compared to full spectrum light. However, outdoor exposure to daylight and sunlight are, in general, more likely to be hazardous than short-duration exposure to blue light therapy, and thus the adverse effects of blue light do not seem significant.22,31–32
Although no serious eye damage has been reported as a result of light therapy, a number of transient visual symptoms have been reported in greater frequency among persons exposed to light therapy than among controls. Commonly reported ocular side effects of light therapy include eyestrain,33–34 blurred vision,10 seeing spots,35 glare,35 and eye burning/irritation.10,35 Nearly all studies reported fast remission of symptoms; thus, side effects may only occur early in treatment as part of an adjustment phase. Other, non-visual symptoms have also been reported in some studies of light therapy including headache,10–11, 33,35–36 nausea,35–36 dizziness,33 agitation,10 and jumpiness/jitteriness/anxiety.33,36 These adverse events are reported to be particularly common in studies in which the light source is close to the eyes, such as with head-mounted units like visors.36 In contrast, a recent randomized trial in two long-term care facilities identified no significant increase in the prevalence of seeing spots, problems with glare, eye burning or irritation, eye redness, jitteriness, severe agitation, skin rash on the face or arms, headache, dizziness, or nausea, when bright light (2,500 lux) was compared to standard light (500 lux).37
Induction of mania has been reported in a few individuals receiving light therapy for treatment of depression.38–40 The induced mania is likely a result from effective treatment of a patient with an underlying undiagnosed bipolar disorder, as has been reported with other depression treatments.38 Hypomania, “wiredness,” and agitation have also been reported in a small proportion of persons treated for depression, which should be kept in mind, especially in treating patients with dementia.27,34–35
Suicide has been reported in a few depressed patients not long after initiation of light therapy;33,41 however, the initiation of any effective antidepressant treatment is known to occasionally lead to suicidal actions in a few persons.42 In fact, antidepressant medications have been reported to increase suicidal risk in adults, and SSRI’s in particular may put elderly populations at increased risk for suicide in the early stages of treatment.43 Thus, the possibility of suicide should be a caution but not a contraindication to light as therapy for depression.
Recommendations for Clinical Practice
High light levels of bluish white light (at least 1,000 lux at the cornea) during morning hours should be considered as a possible therapy for selected older persons with sleep problems and/or depressive symptoms. Particularly appropriate candidates for such treatment would be persons who are at high risk for adverse effects from medications and individuals who rarely go outdoors. In warm climates, half an hour of outdoor daylight exposure each morning would constitute an inexpensive, convenient first-line treatment. When outdoor exposure is impractical, one of the available modalities for indoor light therapy can be prescribed.
Patients with sleep complaints should undergo a thorough medical examination prior to initiation of light therapy. That evaluation should including screening for conditions for which specific therapies are indicated, such as obstructive sleep apnea, medication-related sleep disorders, and alcoholism. Screening for depression is also important in the evaluation of patients with sleep complaints; however, the presence of depression should by no means be a contraindication to light therapy for sleep problems. Treatment for most sleep disorders appears to be best if the light is applied in the morning; however, selected individuals may benefit more from early evening light exposure.
Light appears to have a relatively modest effect as a therapy for depression in older persons. Therefore, except in cases of SAD or of relatively mild symptoms, it is probably used as an adjunct to other treatments, such as selective serotonin reuptake inhibitors (SSRIs) and/or psychotherapy. Light therapy may be of particular complementary value due to its rapid onset of action, which has been demonstrated to occur within days, rather than the weeks required by medication. Patients should time their exposure to the most convenient time of day; if patients have flexibility, however, morning or mid-day light may be optimal.
Because of the theoretical risk of retinal damage, light therapy should likely be avoided in persons with significant retinal damage (e.g. severe macular degeneration) or who have no lens in one or both eyes. Patients initiating light therapy should be cautioned that eye discomfort may result and instructed that, if it is mild, they may continue treatment. They should also be informed that, in some patients, nonspecific symptoms such as headache, dizziness, and jitteriness are sometime observed, but that these are usually mild and may be transient. Both the patient and a family member should be cautioned that, although highly unlikely, they should be on the lookout for and report rashes in light-exposed areas, suicidal thoughts, and/or severe agitation or hypomania. Laboratory monitoring is unnecessary, but periodic follow-up visits and re-evaluations should, of course, be part of the therapeutic plan.
References
- 1.Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence. American Journal of Psychiatry. 2005;162(4):656–662. doi: 10.1176/appi.ajp.162.4.656. [DOI] [PubMed] [Google Scholar]
- 2.Van Someren EJ, Hagebeuk EE, Lijzenga C, et al. Circadian rest-activity rhythm disturbances in Alzheimer’s disease. Biological Psychiatry. 1996;40(4):259–270. doi: 10.1016/0006-3223(95)00370-3. [DOI] [PubMed] [Google Scholar]
- 3.Van Someren EJ. Circadian rhythms and sleep in human aging. Chronobiology International. 2000;17(3):233–43. doi: 10.1081/cbi-100101046. [DOI] [PubMed] [Google Scholar]
- 4.Ancoli-Israel S, Poceta JS, Stepnowsky C, Martin J, Gehrman P. Identification and treatment of sleep problems in the elderly. Sleep Medicine Reviews. 1997;1(1):3–17. doi: 10.1016/s1087-0792(97)90002-2. [DOI] [PubMed] [Google Scholar]
- 5.Van Someren EJW, Raymann RJEM, Scherder EJA, Daanen HAM, Swaab DF. Circadian and age-related modulation of thermoreception and temperature regulation: mechanisms and functional implications. Aging Research Reviews. 2002;1(a):721–778. doi: 10.1016/s1568-1637(02)00030-2. [DOI] [PubMed] [Google Scholar]
- 6.Pandi-Perumal SR, Srinivasan V, Maestroni GJM, et al. Melatonin: Nature’s most versatile biological signal? Journal of the Federation of European Biochemical Societies. 2006;273:2813–2838. doi: 10.1111/j.1742-4658.2006.05322.x. [DOI] [PubMed] [Google Scholar]
- 7.Kripke DF, Youngstedt SD, Rex KM, Klauber MR, Elliott JA. Melatonin excretion with affect disorders over age 60. Psychiatry Research. 2003;118:47–54. doi: 10.1016/s0165-1781(03)00060-x. [DOI] [PubMed] [Google Scholar]
- 8.Thalen B-E, Kjellman F, Morkid L, Wetterberg L. Melatonin in light treatment of patients with seasonal and nonseasonal depression. Acta Psychiatrica Scandinavica. 1995;92:274–284. doi: 10.1111/j.1600-0447.1995.tb09583.x. [DOI] [PubMed] [Google Scholar]
- 9.Forbes D, Morgan DG, Bangma J, Peacock S, Adamson J. Light therapy for managing sleep, behaviour, and mood disturbances in dementia. Cochrane Database of Systematic Reviews. 2004;2:1–35. doi: 10.1002/14651858.CD003946.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Tuunainen A, Kripke DF, Endo T. Light therapy for non-seasonal depression. The Cochrane Database of Systematic Reviews. 2004:2. doi: 10.1002/14651858.CD004050.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martiny K. Adjunctive bright light in non-seasonal major depression. Acta Psychiatrica Scandinavica. 2004;110(Suppl 425):7–28. doi: 10.1111/j.1600-0447.2004.00460_2.x. [DOI] [PubMed] [Google Scholar]
- 12.Benedetti F, Colombo C, Pontiggia A, et al. Morning light treatment hastens the antidepressant effect of citalopram: A placebo-controlled trial. Journal of Clinical Psychiatry. 2003;64(6):648–653. doi: 10.4088/jcp.v64n0605. [DOI] [PubMed] [Google Scholar]
- 13.Martiny K, Lunde M, Unden M, Dam H, Bech P. Adjunctive bright light in non-seasonal major depression: Results from patient-reported symptom and well-being scales. Acta Psychiatrica Scandinavica. 2005;111:453–459. doi: 10.1111/j.1600-0447.2005.00532.x. [DOI] [PubMed] [Google Scholar]
- 14.Loving RT, Kripke DF, Shuchter SR. Bright light augments antidepressant effects of medication and wake therapy. Depression and Anxiety. 2002;16:1–3. doi: 10.1002/da.10036. [DOI] [PubMed] [Google Scholar]
- 15.Martiny K. Adjunctive bright light in non-seasonal major depression. Acta Psychiatrica Scandinavica. 2004;110(Suppl 425):7–28. doi: 10.1111/j.1600-0447.2004.00460_2.x. [DOI] [PubMed] [Google Scholar]
- 16.Rea MS. Light – Much more than vision. The Lighting Research Office of the Electric Power Research Institute. 2002:1–15. [Google Scholar]
- 17.Zeitzer JM, Dijk DJ, Kronauer R, Brown E, Czeisler C. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. The Journal of Physiology. 2000;526(Pt. 3):695–702. doi: 10.1111/j.1469-7793.2000.00695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brainard GC, Hanifin JP, Greeson JM, et al. Action spectrum for melatonin regulation in humans: Evidence for a novel circadian photoreceptor. Journal of Neuroscience. 2001;21(16):6405–6412. doi: 10.1523/JNEUROSCI.21-16-06405.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thapan K, Arendt J, Skene DJ. An action spectrum for melatonin suppression: Evidence for a novel non-rod, non-cone photoreceptor system in humans. The Journal of Physiology. 2001;535:261–267. doi: 10.1111/j.1469-7793.2001.t01-1-00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright HR, Lack LC, Kennaway DJ. Differential effects of light wavelength in phase advancing the melatonin rhythm. Journal of Pineal Research. 2004;36:140–144. doi: 10.1046/j.1600-079x.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- 21.Figueiro MG, Bullough JD, Parsons RH, Rea MS. Preliminary evidence for spectral opponency in the suppression of melatonin by light in humans. Neuroreport. 2004;15(2):313–316. doi: 10.1097/00001756-200402090-00020. [DOI] [PubMed] [Google Scholar]
- 22.Figueiro MG, Rea MS. LEDs: Improving the Sleep Quality of Older Adults. Proceedings of the CIE Midterm Meeting and International Lighting Congress; Leon, Spain. 2005;May 18–21. [Google Scholar]
- 23.Lack L, Wright H, Kemp K, Gibbon S. The treatment of early-morning awakening insomnia with two evenings of bright light. Sleep. 2005;28(5):616–623. doi: 10.1093/sleep/28.5.616. [DOI] [PubMed] [Google Scholar]
- 24.Zeitzer JM, Khalsa SBS, Boivin DB, et al. Temporal dynamics of late-night photic stimulation of the human circadian timing system. American Journal of Physiology Regulatory, Iintegrative and Comparative Physiology. 2005;289:839–844. doi: 10.1152/ajpregu.00232.2005. [DOI] [PubMed] [Google Scholar]
- 25.Ancoli-Israel S, Martin JL, Kripke DF, Marler M, Klauber MR. Effect of light treatment on sleep and circadian rhythms in demented nursing home residents. Journal of the American Geriatrics Society. 2002;50:282–289. doi: 10.1046/j.1532-5415.2002.50060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Remé CE, Terman M. Does light therapy present an ocular hazard? American Journal of Psychiatry. 1992;149(12):1762–1763. doi: 10.1176/ajp.149.12.1762. [DOI] [PubMed] [Google Scholar]
- 27.Labbate LA, Lafer B, Thibault A, Sachs GS. Side effects induced by bright light treatment for Seasonal Affective Disorder. Journal of Clinical Psychiatry. 1994;55:5. [PubMed] [Google Scholar]
- 28.Waxler M, James RH, Brainard GC, et al. Retinopathy and bright light therapy. American Journal of Psychiatry. 1992;149:11. [PubMed] [Google Scholar]
- 29.Sumaya IC, Rienzi BM, Deegan JF, Moss DE. Bright light treatment decreases depression in institutionalized older adults: a placebo-controlled crossover study. The Journals Of Gerontology Series A, Biological Sciences and Medical Sciences. 2001;56A(6):M356–M360. doi: 10.1093/gerona/56.6.m356. [DOI] [PubMed] [Google Scholar]
- 30.Roberts JE. Hazards of sunlight exposure to the eye. In: Giacomoni Paolo U., editor. Sun Protection in Man. Elsevier Science, B.V; Amsterdam, The Netherlands: 2001. [Google Scholar]
- 31.Bullough JD. The blue-light hazard: A review. Journal of the Illuminating Engineering Society. 2000;9(2):6–14. 141. [Google Scholar]
- 32.Figueiro MG, Eggleston G, Rea MS. Effects of light exposure on behavior of Alzheimer’s patients – a pilot study. Light and Human Health: EPRI/LRO 5th International Lighting Research Symposium; 2002. pp. 151–156. [Google Scholar]
- 33.Genhart MJ, Kelley KA, Coursey RD, Datiles M, Rosenthal NE. Effects of bright light on mood in normal elderly women. Psychiatry Research. 1993;47(3):87–97. doi: 10.1016/0165-1781(93)90058-o. [DOI] [PubMed] [Google Scholar]
- 34.Levitt AJ, Joffe RT, Moul DE, et al. Side effects of light therapy in seasonal affective disorder. American Journal of Psychiatry. 1993;150(4):650–652. doi: 10.1176/ajp.150.4.650. [DOI] [PubMed] [Google Scholar]
- 35.Kogan AO, Guilford PM. Side effects of short-term 10,000-lux light therapy. American Journal of Psychiatry. 1998;155(2):293–294. doi: 10.1176/ajp.155.2.293. [DOI] [PubMed] [Google Scholar]
- 36.Terman M, Terman JS. Bright light therapy: Side effects and benefits across the symptom spectrum. Journal of Clinical Psychiatry. 1999;60(11):799–808. [PubMed] [Google Scholar]
- 37.Sloane PD, Barrick AL, Hickman S, Zimmerman S, Williams CS, Mitchell CM. High intensity, low glare environmental light (HILGEL) as therapy in Alzheimer’s disease: Results of a clinical trial. The Gerontological Society of America, 58th Annual Conference; 2005. [Google Scholar]
- 38.Chan PK, Lam RW, Perry KF. Mania precipitated by light therapy for patients with SAD (letter) Journal of Clinical Psychiatry. 1994;55:454. [PubMed] [Google Scholar]
- 39.Kantor DA, Browne M, Ravindran A, Horn E. Manic-like response to phototherapy. Canadian Journal of Psychiatry. 1991;36(9):697–698. doi: 10.1177/070674379103600920. [DOI] [PubMed] [Google Scholar]
- 40.Schwitzer J, Neudorfer C, Blecha H, Fleischhacker WW. Mania as a side effect of phototherapy. Biological Psychiatry. 1990;28:532–534. doi: 10.1016/0006-3223(90)90489-o. [DOI] [PubMed] [Google Scholar]
- 41.Praschak-Rieder N, Neumeister A, Hesselmann B, et al. Suicidal tendencies as a complication of light therapy for seasonal affective disorder: A report of three cases. Journal of Clinical Psychiatry. 1997;58:9. doi: 10.4088/jcp.v58n0903. [DOI] [PubMed] [Google Scholar]
- 42.Food and Drug Administration. Suicidality in adults being treated with antidepressant medications. Food and Drug Administration Public Health Advisory; 2005. Available online at http://www.fda.gov/cder/drug/advisory/SSRI200507.htm. [Google Scholar]
- 43.Juurlink DN, Mamdani MM, Kopp A, Redelmeier DA. The risk of suicide with selective serotonin reuptake inhibitors in the elderly. American Journal of Psychiatry. 2006;163(5):813–821. doi: 10.1176/ajp.2006.163.5.813. [DOI] [PubMed] [Google Scholar]
- 44.Alessi CA, Martin JL, Webber AP, et al. Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. Journal of the American Geriatrics Society. 2005;53:803–810. doi: 10.1111/j.1532-5415.2005.53251.x. [DOI] [PubMed] [Google Scholar]
- 45.Ancoli-Israel S, Gehrman P, Martin JL, et al. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behavioral Sleep Medicine. 2003;1(1):22–36. doi: 10.1207/S15402010BSM0101_4. [DOI] [PubMed] [Google Scholar]
- 46.Colenda C, Cohen W, McCall WV, Rosenquist PB. Phototherapy for patients with Alzheimer’s disease with disturbed sleep patterns: Results of a community-based pilot study. Alzheimer Disease and Associated Disorders. 1997;11(3):175–178. doi: 10.1097/00002093-199709000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Dowling GA, Mastick J, Hubbard EM, Luxenberg JS, Burr RL. Effect of timed bright light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s disease. International Journal of Geriatric Psychiatry. 2005;20:738–743. doi: 10.1002/gps.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fetveit A, Skjerve A, Bjorvatn B. Bright light treatment improves sleep in institutionalised elderly—an open trial. International Journal of Geriatric Psychiatry. 2003;18:520–526. doi: 10.1002/gps.852. [DOI] [PubMed] [Google Scholar]
- 49.Kobayashi R, Fukuda N, Kohsaka M, et al. Effects of bright light at lunchtime on sleep of patients in a geriatric hospital I. Psychiatry and Clinical Neurosciences. 2001;55(3):287–289. doi: 10.1046/j.1440-1819.2001.00863.x. [DOI] [PubMed] [Google Scholar]
- 50.Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry and Clinical Neurosciences. 1999;53:227–229. doi: 10.1046/j.1440-1819.1999.00483.x. [DOI] [PubMed] [Google Scholar]
- 51.Loving RT, Kripke DF, Elliot JA, Knickerbocker NC, Grandner MA. Bright light treatment of depression for older adults. BMC Psychiatry. 2005;5:41. doi: 10.1186/1471-244X-5-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Loving RT, Kripke DF, Knickerbocker NC, Grandner MA. Bright green light treatment of depression for older adults. BMC Psychiatry. 2005;5:42. doi: 10.1186/1471-244X-5-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lyketsos CG, Veiel LL, Baker A, Steele C. A randomized, controlled trial of bright light therapy for agitated behaviors in dementia patients residing in long-term care. International Journal of Geriatric Psychiatry. 1999;14:520–525. [PubMed] [Google Scholar]
- 54.Mishima K, Hishikawa Y, Okawa M. Randomized, dim light controlled, crossover test of morning bright light therapy for rest-activity rhythm disorders in patients with vascular dementia and dementia of Alzheimer’s type. Chronobiology International. 1998;15(6):647–654. doi: 10.3109/07420529808993200. [DOI] [PubMed] [Google Scholar]
- 55.Mishima K, Okawa M, Hishikawa Y, et al. Morning bright light therapy for sleep and behavior disorders in elderly patients with dementia. Acta Psychiatrica Scandinavica. 1994;89:1–7. doi: 10.1111/j.1600-0447.1994.tb01477.x. [DOI] [PubMed] [Google Scholar]
- 56.Ouslander JG, Connell BR, Bliwise DL, et al. A nonpharmacological intervention to improve sleep in nursing home patients: Results of a controlled clinical trial. Journal of the American Geriatrics Society. 2006;54:38–47. doi: 10.1111/j.1532-5415.2005.00562.x. [DOI] [PubMed] [Google Scholar]
- 57.Rosenthal NE, Joseph-Vanderpool JR, Levendosky AA, et al. Phase-shifting effects of bright morning light as treatment for delayed sleep phase syndrome. Sleep. 1990;13(4):354–361. [PubMed] [Google Scholar]
- 58.Stalin A, Volicer L, Ross V, Herz L, Campbell S. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. American Journal of Psychiatry. 1992;149(8):1028–1032. doi: 10.1176/ajp.149.8.1028. [DOI] [PubMed] [Google Scholar]
- 59.Skjerve A, Holsten F, Aarsland D, et al. Improvement in behavioral symptoms and advance of activity acrophase after short-term bright light treatment in severe dementia. Psychiatry and Clinical Neurosciences. 2004;58:343–347. doi: 10.1111/j.1440-1819.2004.01265.x. [DOI] [PubMed] [Google Scholar]
- 60.Suhner AG, Murphy PJ, Campbell SS. Failure of timed bright light exposure to alleviate age-related sleep maintenance insomnia. Journal of the American Geriatrics Society. 2002;50:617–623. doi: 10.1046/j.1532-5415.2002.50154.x. [DOI] [PubMed] [Google Scholar]
- 61.Van Someren EJW, Kessler A, Mirmiran M, Swaab DF. Indirect bright light improves circadian rest-activity rhythm disturbances in demented patients. Biological Psychiatry. 1997;41:955–963. doi: 10.1016/S0006-3223(97)89928-3. [DOI] [PubMed] [Google Scholar]
- 62.Tsai Y, Wong TKS, Juang Y, Tsai H. The effects of light therapy on depressed elders. International Journal of Geriatric Psychiatry. 2004;19:545–548. doi: 10.1002/gps.1125. [DOI] [PubMed] [Google Scholar]
- 63.Yamada N, Martin-Iverson MT, Daimon Z, Tsujimoto T, Takahashi S. Clinical and chronobiological effects of light therapy on nonseasonal affective disorders. Biological Psychiatry. 1995;37:866–873. doi: 10.1016/0006-3223(94)00221-N. [DOI] [PubMed] [Google Scholar]


