Abstract
Background
Dystonia is a neurological disorder characterized by involuntary twisting movements and postures. The neck is among the most commonly affected regions, and diagnosis can be made readily through a simple clinical evaluation. The goal of this study was to explore how long it took patients to receive a diagnosis of cervical dystonia after symptom onset.
Methods
A structured questionnaire was administered at outpatient clinics of a tertiary care academic medical center to 146 consecutively evaluated patients. The questionnaire addressed the length of time from symptom onset to diagnosis, the numbers and types of providers seen before reaching a diagnosis, and treatments attempted prior to receiving botulinum toxin.
Results
A total of 108 patients saw a mean of 3.5 providers over a mean period of 44 months from symptom onset to diagnosis. For patients with symptom onset in the last decade only, patients saw a mean of 3.0 providers over a mean of 14 months.
Conclusions
Although cervical dystonia is the most common form of dystonia with clinical features readily identifiable by a simple history and examination, patients typically see multiple providers over more than a year before reaching a diagnosis and receiving optimal therapy. Improved awareness of the clinical features will enable patients to obtain appropriate therapy more rapidly.
Keywords: Dystonia, cohort studies, torticollis, diagnosis
Introduction
The dystonias are a group of disorders characterized by excessive involuntary contractions of muscles, often leading to abnormal postures, or twisting or repetitive movements (1). The most commonly affected region is the neck, a condition known as cervical dystonia (CD) or torticollis. Patients suffer from turning or tilting of the head, sometimes combined with tremor-like head movements and neck pain (2). CD substantially degrades quality of life due to disability related to keeping the head still, neck pain, and social embarrassment (3, 4). Fortunately, effective therapy is available. Local injections of botulinum toxin provide substantial relief and now are viewed as the treatment of choice (5, 6).
For most patients with CD, a complete diagnostic workup involving laboratory testing and imaging of the brain or spine typically is unrevealing and considered unnecessary. Instead, the diagnosis rests primarily on the recognition of its characteristic clinical features, and an informed provider can make a diagnosis in a few minutes. Despite the ease of diagnosis, many patients report seeing multiple providers over many years and trying many ineffective treatments before reaching a diagnosis and receiving effective therapy. The purpose of the present study was to examine how long it takes to reach a diagnosis of CD after symptom onset.
Methods
Between March 2011 and January 2012, 146 consecutive patients with CD were recruited prospectively from Movement Disorders Clinic at Emory University. To be eligible for the study, participants had to be diagnosed by an experienced neurologist with training in movement disorders with idiopathic isolated CD and be 18 years or older. Patients with psychogenic and drug-induced CD were excluded. Each participant completed a questionnaire to determine the interval between symptom onset and diagnosis, the number and types of medical providers seen, and interventions applied. The study was approved by the Emory Institutional Review Board and all participants gave written informed consent.
Results
Of 146 consecutive patients who met inclusion criteria, 108 agreed to participate. Of those who declined, 30 indicated they did not have enough time to complete the questionnaire, and 8 cited privacy concerns.
The mean age at study enrollment was 61.4 years old (range 34–85) and 80% were female. The mean age at symptom onset was 47.0 years (range 19–75) with a mean duration of 14.4 years (range 0–58). The mean interval from symptom onset until diagnosis was 43.7 months (range 0–336). To determine if this delay to diagnosis was being driven by participants who had disease onset many years ago prior to more widespread recognition of CD, the data were examined in two ways. First, the duration of illness was correlated with the length of time required to reach a diagnosis. This analysis showed only weak correlation (R2=0.17), suggesting that patients with the longest duration of illness were not necessarily experiencing the longest time to diagnosis (Figure 1). Second, participants were stratified according to disease duration and the whole group divided into two at the median, which was 10 years. The group with disease duration ≤10 years experienced more rapid diagnosis (Figure 2). The mean time to diagnosis was 14.8 months in this group, compared to 73.8 months in the group with duration of more than 10 years (p<0.001 by independent t-test). These results imply shorter times to reach diagnosis in the last decade.
Figure 1.
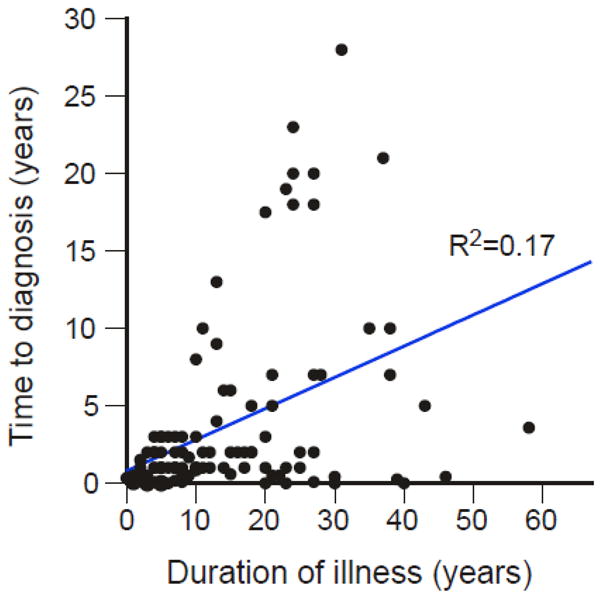
Scatter plot of duration of illness versus the time it took to reach a diagnosis. All cases were plotted individually and the correlation established by linear regression.
Figure 2.
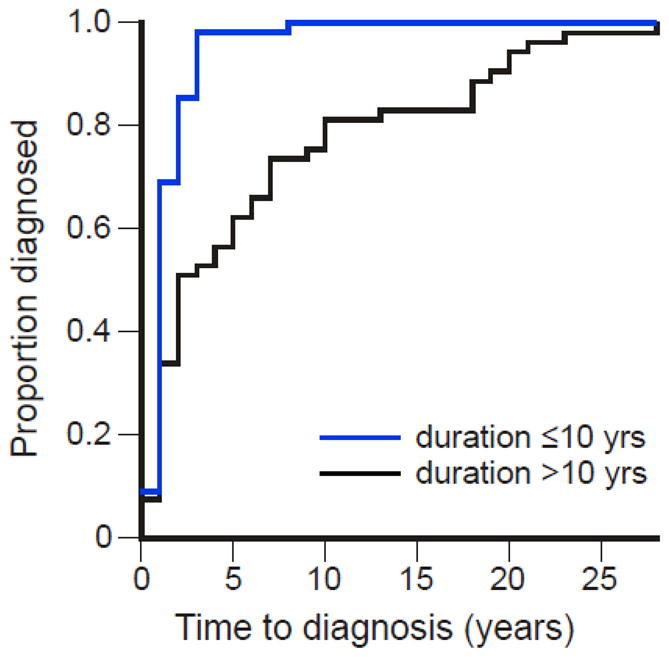
Modified survival plot of the time it took to reach a diagnosis versus the proportion of cases diagnosed, divided by median duration of illness of 10 years.
Prior to receiving a diagnosis, the 108 participants in the study saw a mean of 3.5 providers (range 0–12). Participants with disease duration ≤10 years saw a mean of 3.0 providers, (range 0–12) while those with disease duration >10 saw a mean of 3.9 providers (range 1–12), a difference that was statistically significant (p<0.001). Not surprisingly, most saw their primary care provider (62% of all cases) prior to receiving a diagnosis (Table 1). However, an unexpectedly large number of patients also saw at least one (89% of all cases) or at least two (36% of all cases,) neurologists before reaching a diagnosis. These results imply poor recognition of CD, even among neurologists.
Table 1.
Types of providers evaluating CD
| Type of provider | All patients (% of total) | Disease duration >10 years | Disease duration <10 years |
|---|---|---|---|
| Neurology | 89 | 91 | 85 |
| Primary care | 63 | 58 | 65 |
| Orthopedic surgery | 17 | 19 | 15 |
| Chiropractor | 11 | 7 | 4 |
| Neurosurgery | 4 | 2 | 5 |
| Pain management | 3 | 0 | 5 |
| Psychiatry | 3 | 6 | 0 |
| Otolarngology | 3 | 2 | 4 |
| Physical medicine & rehab | 2 | 0 | 4 |
| Physical therapist | 2 | 0 | 2 |
| Endocrinologist | 2 | 0 | 4 |
| Rheumatologist | 1 | 0 | 2 |
The total number of patients evaluated was 108. Primary care includes internists, family doctors, nurse practitioners, and others considered by patients to be their primary provider.
The majority (63%) of participants tried a variety of oral medications prior to starting botulinum toxin treatments, with only a minority reporting partial or temporary relief. Overall, patients started botulinum toxin therapy a mean 6.8 years (range 0–36) after the onset of symptoms, and 97% of patients were still receiving botulinum toxin as therapy at study entry. Patients with disease duration of ≤10 years started botulinum toxin therapy after a mean of 1.1 years (range 0–4) while those with disease duration >10 years started receiving these injections after a mean of 12.5 years (range 0–36).
Discussion
Despite being the most common form of dystonia with clinical characteristics that can be easily recognized by an educated examiner, CD is not readily diagnosed. Although there have been improvements in the past decade, the results of this study imply that patients still see multiple providers after symptom onset and wait more than a year before reaching a diagnosis. There are many potential reasons for the delays in diagnosis. These reasons may include poor awareness of the many different motor manifestations of CD, such as tonic, phasic and tremor-dominant phenotypes. They may also include prominent complaints of pain leading to concerns for musculoskeletal causes that are evaluated with imaging studies of the neck, which may reveal misleading coincidental structural abnormalities of the spine. The development of formal diagnostic criteria for CD along with studies exploring the reasons for delayed diagnosis seem an important step towards shortening times to diagnosis.
The current study suffers some obvious limitations. As a single site study, the most important one is a referral bias. Because patients were recruited from a tertiary care center, it is possible that many had unusual manifestations that were particularly hard to recognize. However, the current study population had clinical features very similar to reports from other centers (7–10), making this type of bias unlikely. A more likely bias is ascertainment, with exclusion of patients with milder disease who may not be recognized to have CD even after many years. These cases may not yet have been referred for diagnosis and management. In this case, it is likely that the current study underestimates the time required to reach diagnosis. Obtaining timely appointments in our tertiary care center should not present a barrier to patients in the current study as it might for studies in more rural locations where such centers might have fewer provides with long wait times for appointments and extensive travel distances, although we cannot rule out financial barriers placed by insurance providers.
Another limitation of our study is that it is not possible to determine what proportion of the total time to reach diagnosis involved the time patients waited before seeking medication attention versus the time providers took to reach a diagnosis. However, the observation that patients saw an average of 3.5 providers argues that a substantial proportion of this time elapsed after seeking initial medical attention. A final limitation of the current study involves recall bias, since information was collected from patients many years after symptom onset and diagnosis. Such a bias is difficult to exclude without collecting and reviewing historical records going back for several decades, many of which were not available.
Although the current study suffers some methodological limitations, the results are consistent with a similar study in Canada, which revealed an even longer mean lag time of 6.4 years between symptom onset and diagnosis, with patients visiting an mean of 3.3 medical providers before reaching a diagnosis and receiving optimal treatment (11). Similar results recently were presented in abstract form for Australia, where a survey of 48 patients revealed an average of 6.8 years from symptom onset to diagnosis (12). Obviously, results from Canada and Australia cannot be extrapolated to all countries, because accessing the health care systems varies in different countries, with potentially long delays in seeking or receiving medical attention for patients who live in rural areas far from experience providers. However, the results from all three studies all point to lengthy delays in reaching a diagnosis.
Early recognition of the symptoms and signs of CD is important because effective treatment is available. Many patients receive muscle relaxants and analgesics, which may attenuate the problem but rarely solve it. The current treatment of choice involves local injections with botulinum toxin (5, 6). When administered by experienced providers, the majority of patients receive substantial relief and improved quality of life. One of the consequences of delayed diagnosis is that many patients are now turning to internet resources such as YouTube, where other individuals may present videos of their own problems as examples (13). In a recent study of these videos (13), the dystonias were among the most common movement disorders viewed on YouTube. Unfortunately, the majority of the videos were considered by an expert panel to be examples of psychogenic dystonia, suggesting that many patients are obtaining unreliable information from the internet. Better recognition among medical providers seems essential for proper diagnosis and more rapid institution of effective treatment.
A larger, multicenter, population-based study with complete review of medical records would be needed to address some of the limitations of the available studies. A larger study could also be useful to identify the types of providers or regions in the world where education regarding CD might have the greatest impact. Since most patients first seek attention from their primary care providers, this audience seems particularly important. Fortunately, a simple 5 item screening questionnaire is available with high sensitivity and specificity to aid in the diagnosis of CD (14), and video demonstrations of the key features are available through online resources (e.g. www.neurotoxininstitute.com). While education directed towards primary care seems intuitively valuable, our results imply that education should be also directed towards neurologists, since many patients saw more than one before reaching a diagnosis. Considerable efforts now are directed towards educating all types of providers regarding the application of treatments, but it seems that more education regarding recognition and diagnosis are still needed.
Acknowledgments
This study was supported in part by a National Institutes of Health grant (U54 NS065701) from the National Institutes of Neurological Disorders and Stroke and the Office of Rare Diseases Research at the National Center for Advancing Translational Sciences.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Albanese A, Bhatia K, Bressman SB, DeLong MR, Fahn S, Fung VSC, et al. Phenomenology and classification of dystonia: A consensus update. Mov Disord. 2013;28:863–73. doi: 10.1002/mds.25475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jinnah HA, Berardelli A, Comella C, Defazio G, DeLong M, Factor S, et al. The focal dystonias: Current views and challenges for future research. Mov Disord. 2013;7:926–43. doi: 10.1002/mds.25567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slawek J, Friedman A, Potulska A, Krystkowiak P, Gervais C, Banach M, et al. Factors affecting the health-related quality of life of patients with cervical dystonia and the impact of botulinum toxin type A injections. Funct Neurol. 2007;22:95–100. [PubMed] [Google Scholar]
- 4.Evatt ML, Freeman A, Factor S. Adult-onset dystonia. Handb Clin Neurol. 2011;100:481–511. doi: 10.1016/B978-0-444-52014-2.00037-9. [DOI] [PubMed] [Google Scholar]
- 5.Simpson DM, Blitzer A, Brashear A, Comella C, Dubinsky R, Hallett M, et al. Assessment: Botulinum neurotoxin for the treatment of movement disorders (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2008;70:1699–706. doi: 10.1212/01.wnl.0000311389.26145.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jankovic J. Treatment of dystonia. Lancet Neurol. 2006;5:864–72. doi: 10.1016/S1474-4422(06)70574-9. [DOI] [PubMed] [Google Scholar]
- 7.Chan J, Brin MF, Fahn S. Idiopathic cervical dystonia: clinical characteristics. Mov Disord. 1991;6:119–26. doi: 10.1002/mds.870060206. [DOI] [PubMed] [Google Scholar]
- 8.Jankovic J, Leader S, Warner D, Schwartz K. Cervical dystonia: clinical findings and associated movement disorders. Neurology. 1991;41:1088–91. doi: 10.1212/wnl.41.7.1088. [DOI] [PubMed] [Google Scholar]
- 9.Rondot P, Marchand MP, Dellatorlas G. Spasmodic torticollis-review of 220 patients. Can J Neurol Sci. 1991;18:143–51. doi: 10.1017/s0317167100031619. [DOI] [PubMed] [Google Scholar]
- 10.Dauer WT, Burke RE, Greene P, Fahn S. Current concepts on the clinical features, aetiology and management of idiopathic cervical dystonia. Brain. 1998;121:547–60. doi: 10.1093/brain/121.4.547. [DOI] [PubMed] [Google Scholar]
- 11.Jog M, Chouinard S, Hobson D, Grimes D, Chen R, Bhogal M, et al. Causes for treatment delays in dystonia and hemifacial spasm: a Canadian survey. Can J Neurol Sci. 2011;38:704–11. doi: 10.1017/s0317167100012270. [DOI] [PubMed] [Google Scholar]
- 12.Bertram KL, Williams DP. Diagnostic delay in cervical dystonia. Movement Disorders. 2012;27 (Suppl 1):S333. [Google Scholar]
- 13.Stamelou M, Edwards MJ, Espay AJ, Fung VS, Hallett M, Lang AE, et al. Movement disorders on YouTube--caveat spectator. N Engl J Med. 2011;365:1160–1. doi: 10.1056/NEJMc1107673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saunders-Pullman R, Soto-Valencia J, Costan-Toth C, Shriberg J, Raymond D, Derby CA, et al. A new screening tool for cervical dystonia. Neurology. 2005;64:2046–9. doi: 10.1212/01.WNL.0000166030.05756.9F. [DOI] [PubMed] [Google Scholar]


