Abstract
Background and Purpose
Secondary stroke prevention guidelines recommend statins for the management of dyslipidemia in ischemic stroke and transient ischemic attack (TIA). This study assessed the guideline-based statin prescription (GBSP) rate in Korea and the associated physician and patient factors.
Methods
A survey was conducted to assess Korean neurologists' knowledge of and attitude toward the current dyslipidemia management guidelines. The characteristics and discharge statin prescription for all consecutive patients with acute ischemic stroke or TIA treated by participating neurologists during the 6 months prior to the survey were abstracted. Using algorithms to determine GBSP, we assessed the rate and independent factors of GBSP.
Results
Of the 174 participating neurologists, 79 (45.4%) were categorized as a higher-level knowledge group. For the 4407 patients (mean age, 66.4 years; female, 42.5%; 90.6% with ischemic stroke and 9.4% with TIA) enrolled in this study, the GBSP rate at discharge was 78.6%. The GBSP rate increased significantly with increasing physician knowledge level (test for trend, p<0.0001), and was higher among patients treated by the higher-level knowledge group than for those treated by the lower-level knowledge group (81.6% vs. 74.7%; unadjusted p<0.0001 and adjusted p=0.045). Other independent factors associated with a higher GBSP rate were hypercholesterolemia and higher low-density lipoprotein cholesterol level, while those associated with a lower GBSP rate were cardioembolism, undetermined etiology due to negative or incomplete work-up, other determined etiology, and TIA presentation.
Conclusions
More than three-quarters of acute ischemic stroke survivors and TIA patients receive a GBSP at discharge, and this proportion would be further improved by improving the knowledge of dyslipidemia management guidelines among neurologists.
Keywords: statin, guideline, adherence, ischemic stroke, transient ischemic attack, secondary stroke prevention
Introduction
Korea, stroke is the second leading cause of death after cancer and the first leading cause of death due to a single-organ disease. Every year more than 100000 Korean people experience a new or recurrent stroke, and ischemic stroke accounts for more than 75% of all strokes.1 One in five ischemic strokes is a recurrent stroke, which usually leads to greater mortality or disability.2,3 With the evolution of vascular prevention treatments, recurrent strokes, fatal strokes, and major cardiovascular events in stroke survivors treated using therapies with proven efficacy have substantially declined over the last 5 decades.4
Statins are one of the therapies with proven efficacy for both primary and secondary stroke prevention,5,6 and most guidelines recommend statins for patients with non-cardioembolic ischemic stroke and low-density lipoprotein cholesterol (LDL-C) levels ≥100 mg/dL. However, a lack of familiarity or disagreement with the guidelines among physicians can hamper the appropriate use of statins. In addition, the gap between the physicians' perception and their actual practices may further increase the failure of appropriate dyslipidemia management.7
In the USA, the number of patients with acute ischemic stroke who were discharged on statins increased between 2005 and 2007, but the rates of discharge statin use varied substantially across hospitals, with 20% of eligible patients not receiving statin medication at discharge.8 The current Korean stroke guidelines also recommend statins for eligible patients with ischemic stroke or transient ischemic attack (TIA), generally in accordance with the National Cholesterol Education Program-Adults Treatment Panel III (NCEP-ATP III) guidelines. In brief, the target LDL-C level is <100 mg/dL for patients with atherothrombotic stroke or TIA, or those with coexisting coronary heart disease (CHD), and a more aggressive lowering might be considered for high-risk patients with multiple risk factors. According to a nationwide, hospital-based Korean stroke registry, 22% of patients admitted in 2010 due to acute ischemic stroke or TIA had hypercholesterolemia defined as current use of a lipid-lowering agent, total cholesterol >240 mg/dL, or LDL-C >160 mg/dL.2 However, the management of dyslipidemia by Korean neurologists has not been systematically investigated. The aim of this study, entitled the ROLLERKOST (Real World of Lipid-Lowering Therapy in Korean Stroke Patients), was to elucidate the knowledge of and attitude toward the current guidelines of Korean neurologists, to determine the rate of guideline-based statin prescription (GBSP) at discharge, and to identify the factors of physicians and patients associated with guideline adherence for dyslipidemia management in patients hospitalized with acute ischemic stroke or TIA in Korea.
Methods
Physician survey
Among 86 neurology training hospitals in Korea, we selected 33 centers which actively enroll their patients in the Korean Stroke Registry.2 The principal investigator (B.-C. Lee) sent an e-mail describing the purpose of this study to the physicians in charge of stroke care in the 33 centers, and received an agreement to participate from 27 centers. A survey was then conducted in which the neurologists (board-certified neurologists and residents) of the 27 centers were directly interviewed with the aid of a structured questionnaire between November 2010 and December 2011. The questionnaire comprised the following four main physician domains: characteristics (5 items), practice pattern of dyslipidemia management (15 items), knowledge of the current dyslipidemia management guidelines (10 items), and attitude toward the current guidelines (21 items) (Table 1).
Table 1.
Domains and items included in the questionnaire
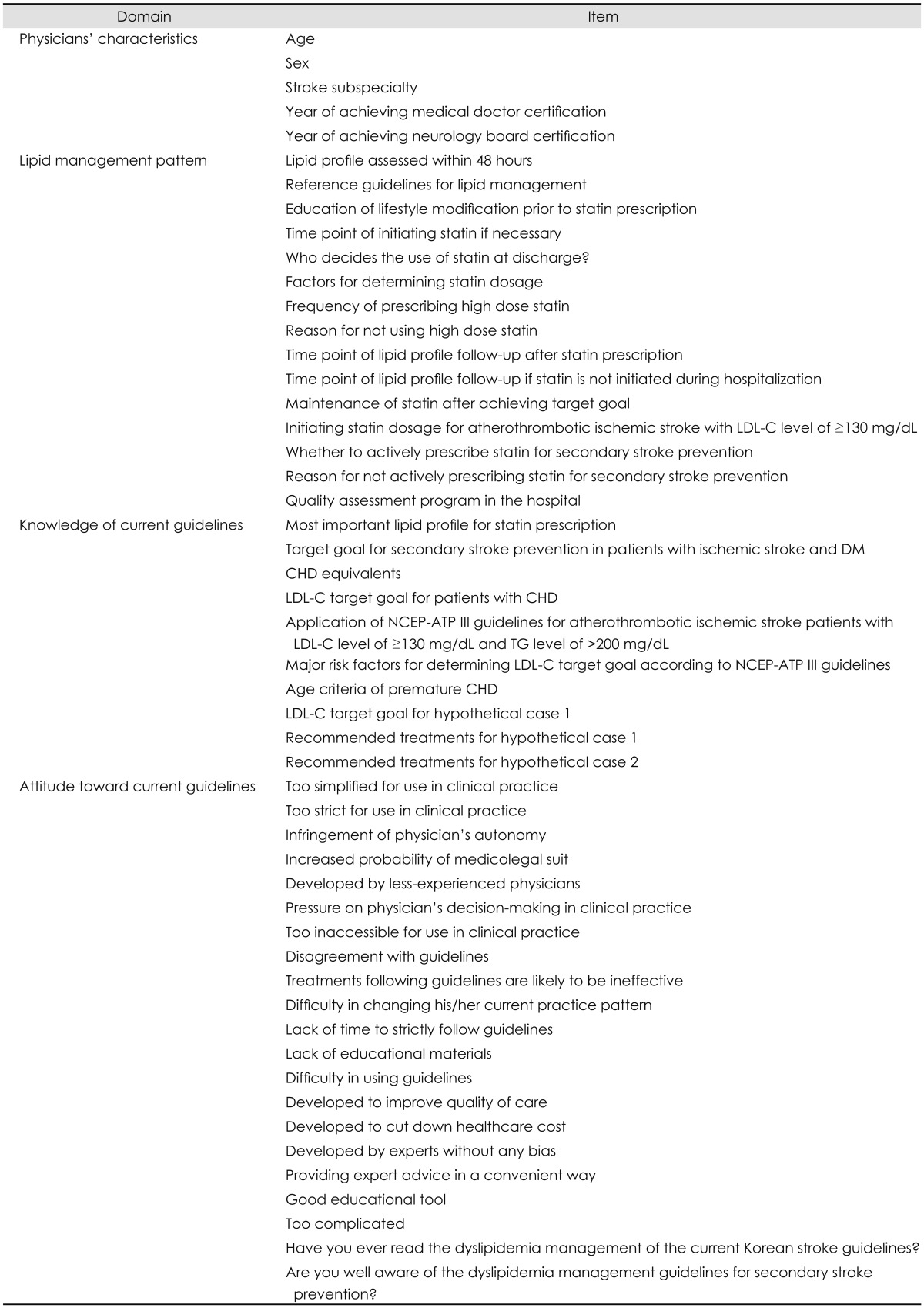
CHD: coronary heart disease, DM: diabetes mellitus, LDL-C: low-density lipoprotein cholesterol, NCEP-ATP III: National Cholesterol Education Program-Adults Treatment Panel III, TG: triglyceride.
Patient demographics and prescription of a lipid-lowering agent
A retrospective review was undertaken of the medical records of patients with ischemic stroke or TIA who were 1) treated by participating neurologists, 2) hospitalized during the 6 months prior to the survey, and 3) hospitalized within 48 hours from symptom onset. The following data were obtained for each patient: 1) demographics of age, sex, height, weight, abdominal circumference, body mass index (BMI), and blood pressure at admission, 2) past medical history of stroke, CHD, peripheral artery disease, symptomatic carotid artery disease, abdominal aortic aneurysm, or other cardiac disease, 3) vascular risk factors of current or ex-smoker, diabetes, familial history of premature CHD, hypertension, hypercholesterolemia (defined as current use of a lipid-lowering agent, total cholesterol >240 mg/dL, or LDL-C >160 mg/dL), and atrial fibrillation (AF), 4) stroke subtype based on the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification, 5) baseline laboratory data including fasting blood glucose, glycosylated hemoglobin (HbA1c), total cholesterol, triglyceride, LDL-C, and high-density lipoprotein cholesterol (HDL-C), and 6) statin prescription at discharge. This study was approved by the institutional review boards of the 27 participating hospitals.
Outcomes
The primary outcome of interest was the percentage of patients discharged with a GBSP for secondary stroke prevention. Algorithms were developed to determine the GBSP rate, based on the Korean guidelines as well as those of the American Stroke Association/American Heart Association and NCEP-ATP III (Table 2). The GBSP group included patients who were 1) indicated for and received statin therapy and 2) not indicated for and did not receive statin therapy. In contrast, the non-GBSP group included patients who were 1) indicated for but did not receive statin therapy and 2) not indicated for but received statin therapy.
Table 2.
Algorithms for determining a GBSP
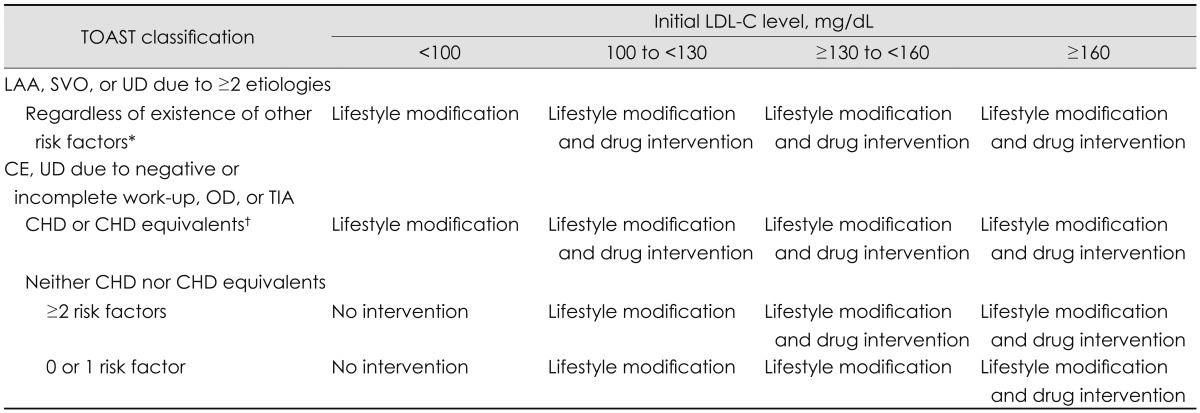
*Risk factor: hypertension, current smoking, familial history of premature CHD, HDL-C<40 mg/dL, age, †CHD equivalent: >50% carotid stenosis, peripheral arterial disease, abdominal aortic aneurysm, or DM.
CE: cardioembolism, CHD: coronary heart disease, DM: diabetes mellitus, GBSP: guideline-based statin prescription, HDL-C: high-density lipoprotein cholesterol, LAA: large-artery atherosclerosis, LDL-C: low-density lipoprotein cholesterol, OD: other determined etiology, SVO: small-vessel occlusion, TIA: transient ischemic attack, TOAST: Trial of Org 10172 in Acute Stroke Treatment, UD: undetermined etiology.
To explore whether the physician's knowledge of current guidelines was associated with the GBSP rate, the knowledge level of each of the participating physicians was quantified using the number of correct responses to ten questions in the physician's knowledge domain (a score of 10 was assigned to each question, so a score of 100 was a perfect score). For analytical purposes, the physicians were then categorized into two groups: 1) the higher-level knowledge group, who achieved a score that was higher than the median value, and 2) a lower-level knowledge group, who achieved a score that was equal to or lower than the median. The physicians' preference for guidelines was calculated by summing the ratings (5 grades) of responses to 21 questions in the physicians' attitude domain. The physicians were then categorized into the higher- and lower-preference groups (preference of guidelines) according to a median value.
Sample size calculation and power estimation
We assumed that the GBSP rate in the higher-level knowledge group would be 90%, based on a projection from the observation of statin prescription for 4018 patients enrolled in the Clinical Research Center for Stroke Registry (http://www.stroke-crc.or.kr/). The GBSP rate in the lower-level knowledge group was assumed to be 87%, which was determined by a consensus among experts. When recruiting the 33 centers that actively enroll their patients in the Korean Stroke Registry,2 the projected sample size of neurologists was 211, and that of patients admitted during the previous 6 months was 5200. Taking into account a refusal rate of 10-15%, the final projected sample size was 180-190 for neurologists and 4400-4700 for patients. If the ratio of the higher-level knowledge group versus the lower-level knowledge group was 1 : 1, a sample size of 4500 patients could detect the absolute 3% difference with 88% power and 5% alpha error, whereas for a 2 : 1 ratio the power would decrease to 85%.
Statistical analysis
Categorical variables are summarized as frequencies and percentages, while continuous variables are presented as mean±SD values. Variables exhibiting substantial skewing are reported using geometric means and geometric SDs. Among the physician survey responses, data not provided by physicians were treated as missing values. For group comparisons, categorical variables were compared using the chi-square test or Fisher's exact test as appropriate, while continuous variables were compared using Student's t-test. Variables with a substantial skewed distribution were compared using logarithmically transformed values. The Cochran-Armitage test of trend was used to determine whether there was an increasing trend for the GBSP rate relative to the physicians' knowledge scores.
A generalized estimating equation (GEE) model was employed to account for the multilevel structure of the data set, which comprised the physician's level and the associated patient's level variables. The GEE model was used to explore whether the physician's knowledge level and their characteristics were independent factors influencing the GBSP rate, after adjusting for those of the patients. This multivariable analysis included all covariates of the physicians' demographic factors of knowledge level group, age, sex, and stroke subspecialty. Among the patients' factors, covariates with p<0.1 on the comparisons of baseline characteristics between the GBSP group and the non-GBSP group were included, in addition to age. Furthermore, the variable of history of CHD was included; statin therapy is generally recommended for patients with a history of CHD. Since most patients were cared for by both a board-certified neurologist and a resident, the knowledge of the board-certified neurologist was used in the analysis of the association between the physician's knowledge level and their patient's statin prescription status. Where the patient was matched only to a resident (18 out of 4407), the resident's knowledge level was used for that analysis. Statistical analyses were performed using SAS version 9.2 (SAS, Cary, NC, USA). The level of statistical significance was set at p<0.05 (all two-tailed).
Results
Physicians' characteristics
Of the 33 centers contacted, 174 neurologists from 27 centers agreed to participate in this study. The characteristics of the participating neurologists are presented in Table 3. In brief, 73 (42.0%) were board-certified neurologists, and 66 (37.9%) responded that their subspecialty was stroke. They were aged 33.6±7.1 years, and 49 (28.2%) were female. Among the participating neurologists, 173 (99.4%) responded that they assessed their patients' LDL-C level within 48 hours of hospitalization. The response rates of measuring total cholesterol, HDL-C, and triglyceride levels within 48 hours were greater than 97%. For statin prescription, 167 (96.0%) neurologists chose the LDL-C level as an indicator. For referencing guidelines, 111 (63.8%) used the Korean guidelines and 56 (32.2%) the American Stroke Association guidelines.
Table 3.
Physicians' characteristics
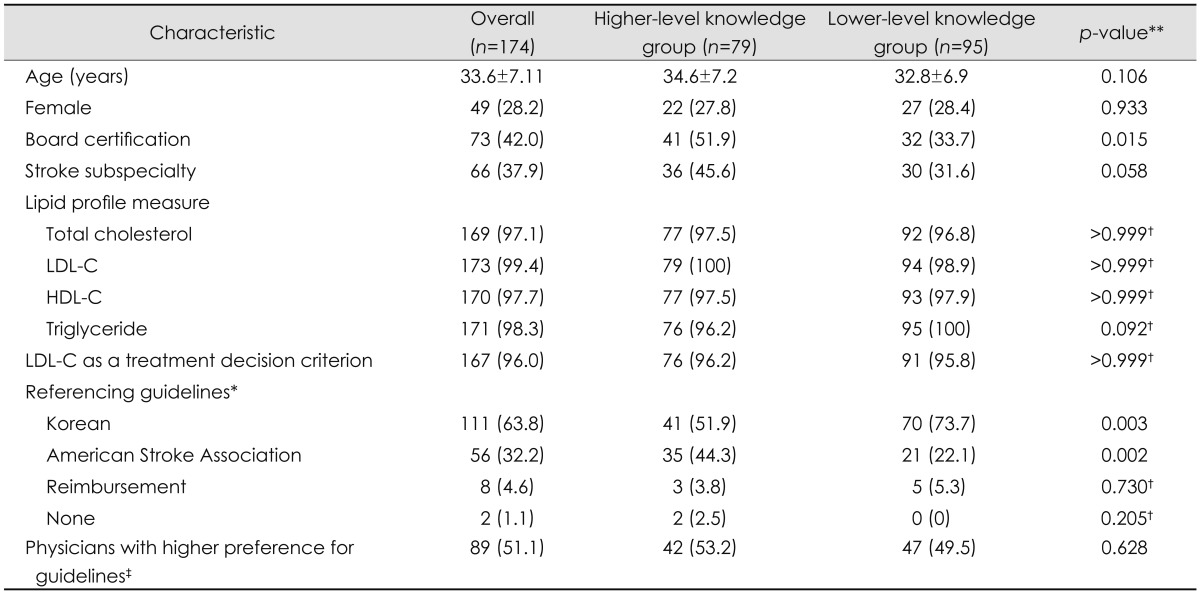
Data are number of patients (%) or mean±SD values.
*Multiple responses were made, **Values of p were obtained using Student's t-test or chi-square test, unless otherwise specified, †By Fisher's exact test, ‡Physicians with higher preference for guidelines indicate those who had a score greater than the median value on rating of responses to 21 questions in physicians' attitude to guidelines.
HDL-C: high-density lipoprotein cholesterol, LDL-C: low-density lipoprotein cholesterol.
The median score for the neurologists' knowledge of the current dyslipidemia management guidelines was 70 (range, 30-100); 79 (45.4%) neurologists were thus categorized into the higher-level knowledge group (achieving a score of >70), and 95 (54.6%) were categorized into the lower-level knowledge group. Those in the higher-level knowledge group were more likely to have a neurology board certification and to use the American Stroke Association guidelines than those in the lower-knowledge group. However, age, sex, stroke subspecialty, lipid assessment within 48 hours of hospitalization, using LDL-C as an indicator, and guideline preference did not differ significantly between the two groups.
Patients' characteristics
Of the 4476 eligible patients, 4407 (98.5%) were included in the current analysis; 69 patients were excluded due to lack of a lipid profile (lipid profiles were not available for 82 patients; however, 13 of those patients were registered as having hypercholesterolemia and discharged with a statin, and were thus included and assigned to the GBSP group) (Table 4). The patients were aged 66.4±13.1 years, and 1872 (42.5%) were female. The qualifying event was ischemic stroke in 3993 (90.6%) patients (large-artery atherosclerosis, 32%; cardioembolism, 18.3%; small-vessel occlusion, 20.8%; undetermined etiology, 18.5%; and other determined etiology, 0.9%) and TIA in 414 (9.4%) patients. The following risk factors were noted among the patients: hypertension, 66.9%; diabetes, 33.5%; AF, 17.5%; hypercholesterolemia, 31.0%; current or ex-smoker, 37.4%; CHD, 6.5%; and symptomatic carotid stenosis, 2.7%. Regarding lipid profiles, the levels of LDL-C, total cholesterol, HDL-C, and triglyceride were 110.8±36.7, 174.3±42.8, 44.4±13.2, and 122.6±91.6 mg/dL, respectively.
Table 4.
Patients' characteristics
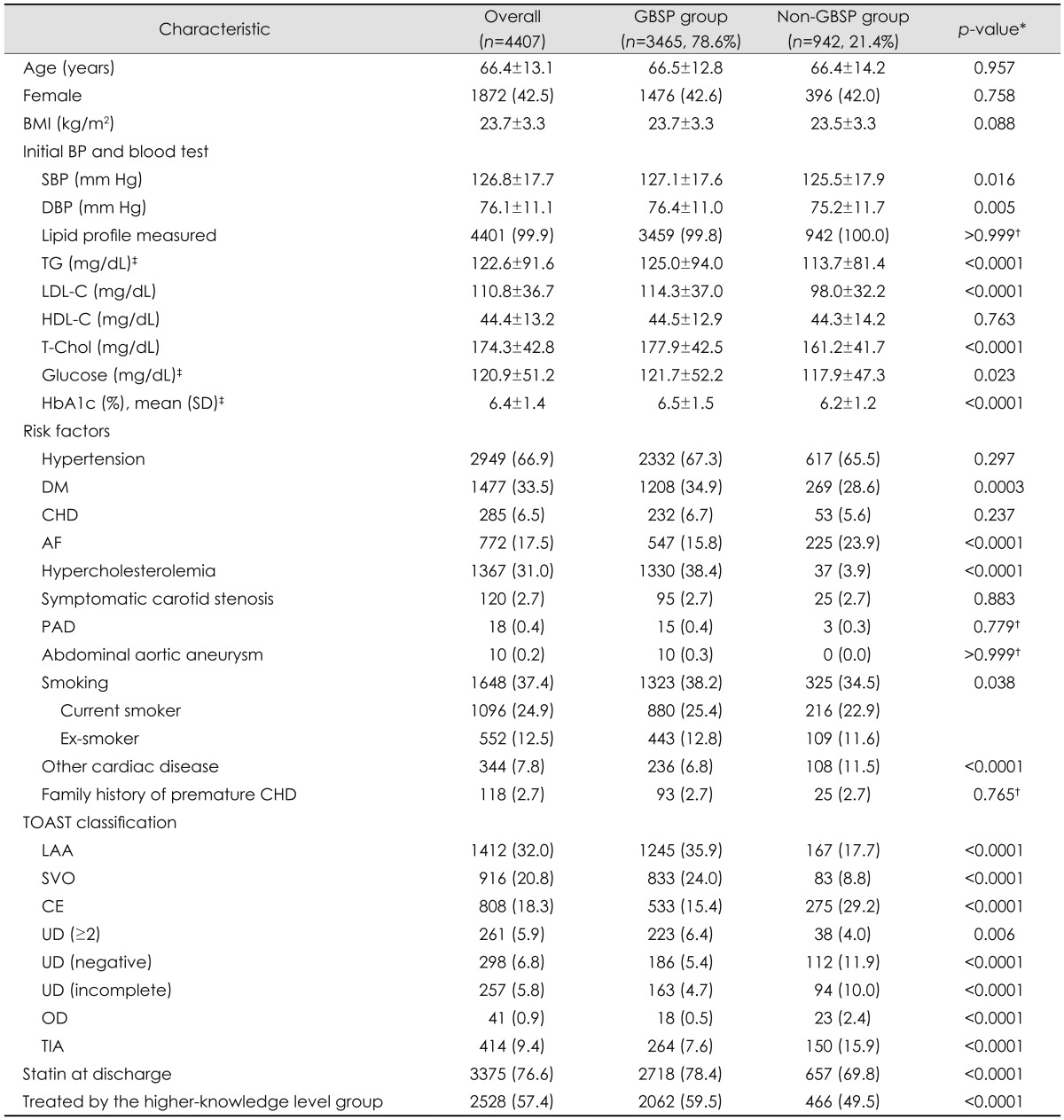
Data are number of patients (%) or mean±SD values.
*p-values for Student's t-test or chi-square test as appropriate, comparing the GBSP group with the non-GBSP group, unless otherwise specified, †Fisher's exact test, ‡Geometric mean and SD, and logarithmically transformed values were used to compare the two groups. AF: atrial fibrillation, BMI: body mass index, BP: blood pressure, CE: cardioembolism, CHD: coronary heart disease, DBP: diastolic blood pressure, DM: diabetes mellitus, GBSP: guideline-based statin prescription, HDL-C: high-density lipoprotein cholesterol, LAA: large-artery atherosclerosis, LDL-C: low-density lipoprotein cholesterol, OD: other determined etiology, PAD: peripheral arterial disease, SBP: systolic blood pressure, SVO: small-vessel occlusion, TG: triglyceride, TIA: transient ischemic attack, UD: undetermined etiology.
Statin prescription at discharge
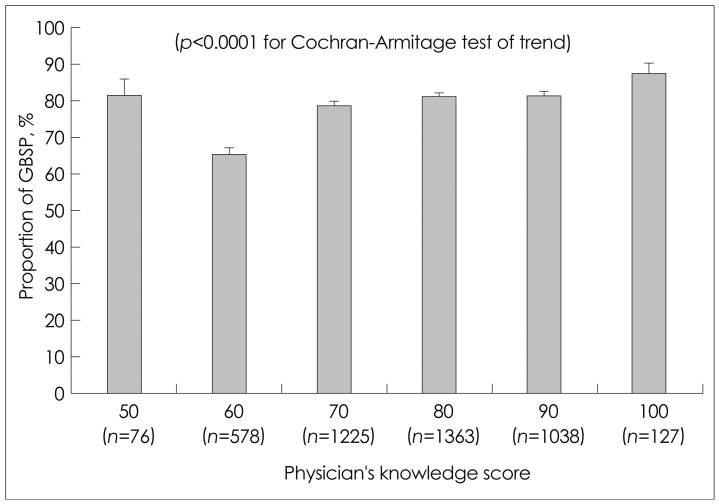
The GBSP rate at discharge among the 4407 patients was 78.6% (Table 4). Of the 2528 patients treated by the higher-level knowledge group, 2062 (81.6%) were on GBSP at discharge. In contrast, of the 1879 patients managed by the lower-level knowledge group, 1403 (74.7%) were on GBSP at discharge. The proportion of patients with a GBSP differed significantly between the higher- and lower-level knowledge groups (p<0.0001). In addition, the proportion of patients with a GBSP increased significantly with increasing physicians' knowledge (p<0.0001 for Cochran-Armitage's chi-square trend test) (Fig. 1).
Fig. 1.
GBSP rate according to physician's knowledge level. The number (n) in the parenthesis indicates the number of patients treated by physicians with each knowledge score. Error bars indicate standard errors. GBSP: guideline-based statin prescription.
On univariable analyses, patients in the GBSP group were more likely to have higher systolic and diastolic blood pressure, higher levels of LDL-C, total cholesterol, triglyceride, glucose, and HbA1c, higher frequencies of diabetes, dyslipidemia, and smoking, lower frequencies of AF and other cardiac disease, and (for TOAST classification) higher frequencies of large-artery atherosclerosis, small-vessel occlusion, and undetermined etiology due to having two or more etiologies, and lower frequencies of cardioembolism, undetermined etiology due to negative or incomplete work-up, other determined etiology, and TIA. The rate of overall statin prescription at discharge was 76.6%, and was higher in the GBSP group than in the non-GBSP group (78.4% vs. 69.8%; p<0.0001).
Factors independently associated with GBSP rate are presented in Table 5. The current multivariable model included covariates of the physician factors of knowledge level, age, sex, and stroke subspecialty and the patient factors of age, BMI, TOAST classification, diabetes, CHD, AF, dyslipidemia, other cardiac disease, smoking, blood pressure, and levels of LDL-C, triglyceride, total cholesterol, glucose, and HbA1c. The higher-level knowledge group, hypercholesterolemia, and LDL-C level were independently associated with GBSP rate. In contrast, stroke mechanisms of cardioembolism and undetermined etiology due to negative or incomplete work-up, and other determined etiology, and presentation with TIA were independent factors that were negatively associated with GBSP rate.
Table 5.
Estimated adjusted ORs and 95% CIs for a GBSP at discharge
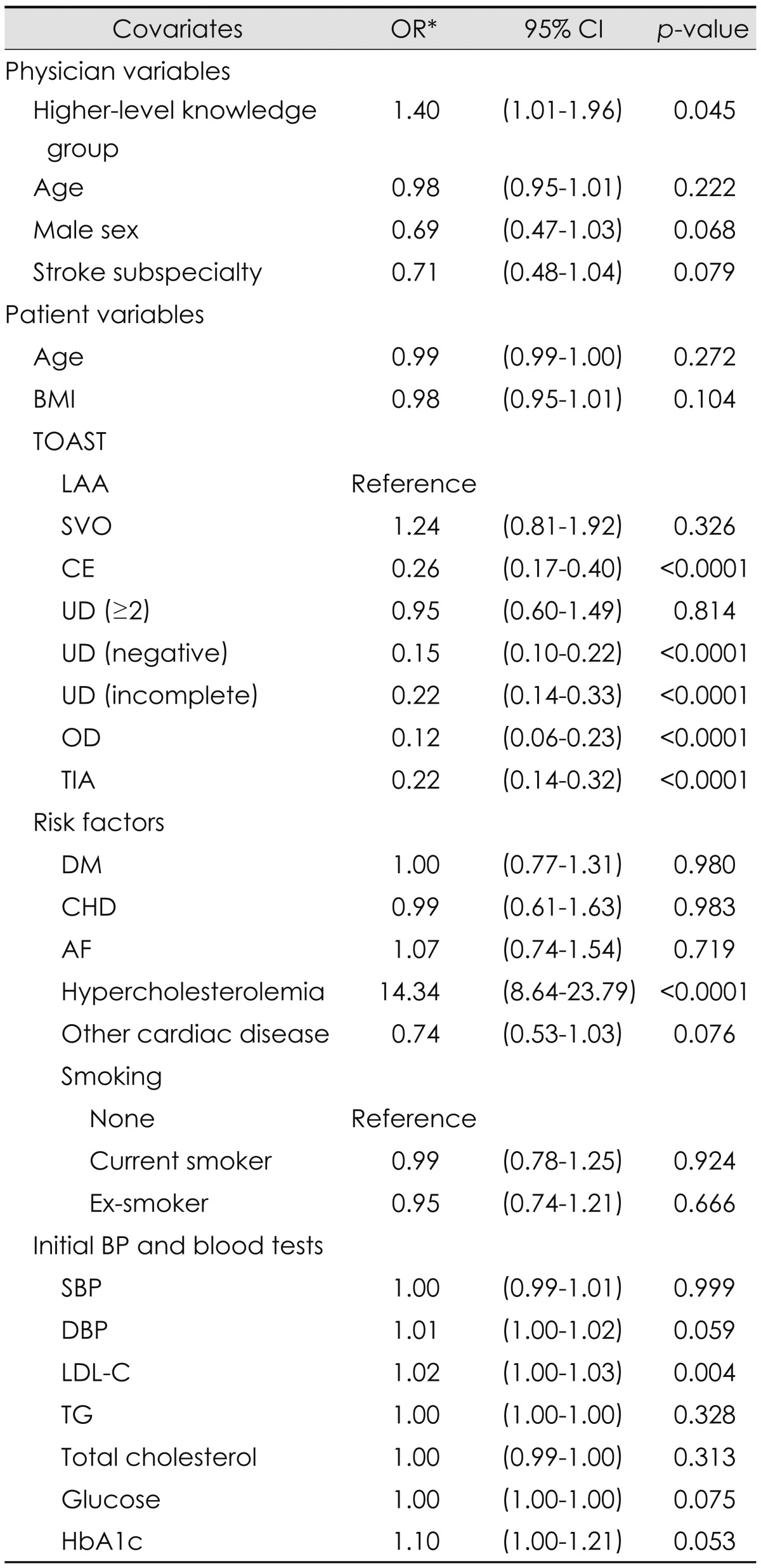
*By GEE analysis, which accounts for a multilevel structure of variables comprising the physicians' and associated patient levels. AF: atrial fibrillation, BMI: body mass index, BP: blood pressure, CE: cardioembolism, CHD: coronary heart disease, CI: confidence interval, DBP: diastolic blood pressure, DM: diabetes mellitus, GBSP: guideline-based statin prescription, GEE: generalized estimating equation, LAA: large-artery atherosclerosis, LDL-C: lowdensity lipoprotein cholesterol, OD: other determined etiology, OR: odds ratio, SBP: systolic blood pressure, SVO: small-vessel occlusion, TG: triglyceride, TIA: transient ischemic attack, TOAST: Trial of Org 10172 in Acute Stroke Treatment, UD: undetermined etiology, UD: undetermined etiology.
Analysis of statin prescription instead of GBSP at discharge revealed that the rates of statin prescription at discharge were 77.7% and 75.5% among patients treated by the higher- and lower-knowledge level groups, respectively; the difference was significant on univariable analysis, [unadjusted odds ratio (OR)=1.161, 95% confidence interval (CI)=1.01-1.34; p=0.037]. On multivariable analysis, in contrast to the association between physician's knowledge level and GBSP, the higher-level knowledge group was not independently associated with statin prescription at discharge (adjusted OR=0.99, 95% CI=0.36-2.74; p=0.992).
Discussion
The GBSP rate at discharge among patients with acute ischemic stroke or TIA was 78.6% in this study, which suggests that Korean neurologists are generally familiar with and adhere to guidelines in clinical practice. The higher percentages of lipid profile assessment, recognition of LDL-C level as an indicator for statin therapy, and referencing the dyslipidemia management guidelines of the Korean or American Stroke Association in their clinical practice would support the relevance of the current findings. However, given that at least one in five patients was discharged without a GBSP, there remains room for improvement.
It is noteworthy that neurologists with a higher knowledge level were more likely to adhere to GBSP. The absolute difference in the proportion of patients on a GBSP between the higher- and lower-knowledge level groups was 6.9%, and the difference was significant in both the adjusted and unadjusted analyses. The significance of the increased GBSP rate with higher levels of physician's knowledge (Fig. 1) would further support the robustness of the finding. It is assumed - but has not been well demonstrated - that the knowledge level of a neurologist is associated with the adherence to guidelines in clinical practice. A previous study from the USA analyzing data of patients enrolled in the Get With The Guidelines-Stroke participating hospitals found that the rate of statin prescription at discharge among hospitalized patients with ischemic stroke or TIA increased over time between 2005 and 2007,8 which coincided with a period of dissemination of the results of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial and secondary stroke prevention guidelines.5,9 The physician's increased familiarity with and improved knowledge of the guidelines might account for this improvement, but that study did not directly demonstrate an association between neurologists' knowledge and statin use. In the secondary prevention of CHD, physicians having knowledge of guidelines were more likely to initiate lipid-lowering treatment and to comply with an overall measure of guideline adherence.10 Another study also showed that a physician's lack of familiarity with and knowledge of guidelines were identified as important barriers to an appropriate management of dyslipidemia.11 Regarding the management of blood pressure, physicians familiar with the Joint National Committee guidelines were more likely to recognize the blood pressure threshold for initiating blood-pressure-lowering therapy as recommended in the guidelines.12 In accord with these previous findings, our results suggest that educating physicians is essential to implement therapies with proven efficacy into clinical practice for secondary stroke prevention. Case-based learning would help to enhance the knowledge of guideline-based dyslipidemia management among neurologists, as shown by a cardiology study that demonstrated an improvement in physicians' knowledge of NCEP-ATP III guidelines after a validated case-based interactive educational program.13
In the present study, patients presenting with TIA were less likely to receive a GBSP, which has also been reported previously.8 In addition to the presentation with TIA, stroke mechanisms of cardioembolism, undetermined etiology due to negative or incomplete work-up, and other determined etiology were associated with a lower GBSP rate. However, many of these patients are likely to be at high risk of coronary event or nonstroke vascular death. A meta-analysis showed that the annual risks of nonstroke vascular death and myocardial infarction among stroke survivors were 2.1% and 2.2%, respectively.14 Another study found that the 5-year risk of cardiac death was twice that of fatal recurrent stroke.15 In the SPARCL trial, the relative risk reduction with statin treatment was greater for any coronary event and major coronary event than for recurrent stroke.5 Therefore, neurologists should also take into account events in vascular beds other than the cerebrovascular bed when performing the long-term management of stroke survivors.
This study has several limitations. The physicians were affiliated with and patients were enrolled from neurology training hospitals, which would limit the generalizability of the findings. The observational design of this study made it impossible to adjust for unmeasured confounders. The current GBSP rate defined by our algorithms does not necessarily indicate the appropriateness of statin therapy. Physicians may prescribe statin to some patients who had LDL-C <100 mg/dL but had a significant stenosis in cerebrovascular or other vascular beds. However, the mechanical algorithms used herein could not fully reflect these kinds of deliberate considerations by physicians. Finally, rather than a discharge statin prescription rate, the rate of target LDL-C goal achievement would be more clinically important, but it was not possible to assess the latter in the present study. Analysis of target LDL-C goal achievement in patients with ischemic stroke or TIA would be of great interest as a topic of future study. However, hospitalization due to stroke or TIA would be a good opportunity to initiate statin treatment and to increase patient adherence. Therefore, the status of discharge statin prescription per se is worthy of investigation.
Acknowledgements
This study was partially supported by a grant of the Korea Healthcare technology R & D project, Ministry of Health and Welfare, Republic of Korea (HI10C2020) and by Pfizer Pharmaceuticals Korea Ltd., but the sponsors did not participate in the study design, data analysis, or manuscript preparation.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: Part I. Epidemiology and risk factors: a report from the Korean Stroke Society and Clinical Research Center for Stroke. J Stroke. 2013;15:2–20. doi: 10.5853/jos.2013.15.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung KH, Lee SH, Kim BJ, Yu KH, Hong KS, Lee BC, et al. Secular trends in ischemic stroke characteristics in a rapidly developed country: results from the Korean Stroke Registry Study (secular trends in Korean stroke) Circ Cardiovasc Qual Outcomes. 2012;5:327–334. doi: 10.1161/CIRCOUTCOMES.111.963736. [DOI] [PubMed] [Google Scholar]
- 3.Jørgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Stroke recurrence: predictors, severity, and prognosis. The Copenhagen Stroke Study. Neurology. 1997;48:891–895. doi: 10.1212/wnl.48.4.891. [DOI] [PubMed] [Google Scholar]
- 4.Hong KS, Yegiaian S, Lee M, Lee J, Saver JL. Declining stroke and vascular event recurrence rates in secondary prevention trials over the past 50 years and consequences for current trial design. Circulation. 2011;123:2111–2119. doi: 10.1161/CIRCULATIONAHA.109.934786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amarenco P, Bogousslavsky J, Callahan A, 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–559. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 6.Amarenco P, Labreuche J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. Lancet Neurol. 2009;8:453–463. doi: 10.1016/S1474-4422(09)70058-4. [DOI] [PubMed] [Google Scholar]
- 7.Hwang JY, Jung CH, Lee WJ, Park CY, Kim SR, Yoon KH, et al. Low density lipoprotein cholesterol target goal attainment rate and physician perceptions about target goal achievement in Korean patients with diabetes. Diabetes Metab J. 2011;35:628–636. doi: 10.4093/dmj.2011.35.6.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ovbiagele B, Schwamm LH, Smith EE, Hernandez AF, Olson DM, Pan W, et al. Recent nationwide trends in discharge statin treatment of hospitalized patients with stroke. Stroke. 2010;41:1508–1513. doi: 10.1161/STROKEAHA.109.573618. [DOI] [PubMed] [Google Scholar]
- 9.Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37:577–617. doi: 10.1161/01.STR.0000199147.30016.74. [DOI] [PubMed] [Google Scholar]
- 10.Heidrich J, Behrens T, Raspe F, Keil U. Knowledge and perception of guidelines and secondary prevention of coronary heart disease among general practitioners and internists. Results from a physician survey in Germany. Eur J Cardiovasc Prev Rehabil. 2005;12:521–529. doi: 10.1097/00149831-200512000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Virani SS, Steinberg L, Murray T, Negi S, Nambi V, Woodard LD, et al. Barriers to non-HDL cholesterol goal attainment by providers. Am J Med. 2011;124:876–880.e2. doi: 10.1016/j.amjmed.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med. 2000;160:2281–2286. doi: 10.1001/archinte.160.15.2281. [DOI] [PubMed] [Google Scholar]
- 13.Sisson SD, Rice TN, Hughes MT. Physician knowledge of national cholesterol guidelines before and after an interactive curriculum. Am J Cardiol. 2007;99:1234–1235. doi: 10.1016/j.amjcard.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 14.Touzé E, Varenne O, Chatellier G, Peyrard S, Rothwell PM, Mas JL. Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke: a systematic review and meta-analysis. Stroke. 2005;36:2748–2755. doi: 10.1161/01.STR.0000190118.02275.33. [DOI] [PubMed] [Google Scholar]
- 15.Dhamoon MS, Sciacca RR, Rundek T, Sacco RL, Elkind MS. Recurrent stroke and cardiac risks after first ischemic stroke: the Northern Manhattan Study. Neurology. 2006;66:641–646. doi: 10.1212/01.wnl.0000201253.93811.f6. [DOI] [PubMed] [Google Scholar]