Abstract
Background and Purpose
Atherothrombotic cerebral infarction [atherothrombotic stroke (ATS)] shares common risk factors and pathophysiological mechanisms with coronary artery disease (CAD), and both diseases appear to have common susceptibility loci. The muscle RAS oncogene homolog gene (MRAS) has been identified as a susceptibility locus for CAD and is implicated in atherosclerosis. The aim of this study was to elucidate whether the single-nucleotide polymorphisms (SNPs) and haplotypes of MRAS are associated with increased risk of ATS in a population of Han Chinese.
Methods
A case-controlled association study was conducted in which only patients with ATS (identified as a major subtype in the Korean modification of the Trial of Org 10172 in Acute Stroke Treatment classification) were enrolled. Subgroup analyses were carried out to determine whether the effect of the MRAS polymorphism was specific to age and gender among the subjects.
Results
In total, 194 ATS and 186 control subjects were included in the present study. Two tagging SNPs were identified in MRAS (rs40593 and rs3755751). A multivariate regression analysis revealed a positive association between rs40593 and ATS under dominant and additive models after adjustment for covariates. Subgroup analyses revealed that there were no gender differences with respect to allele or genotype frequencies between the groups. The AG genotype for rs40593 (p=0.028), the CT genotype for rs3755751 (p=0.036), and G-allele carriers (AG plus GG) for rs40593 (p=0.015) exhibited a significant protective effect among those aged ≥45 years. For the haplotype analysis, ATS subjects aged ≥45 years had a higher frequency of the ACAC haplotype (76.0%) than the controls (68.1%; p<0.05); that haplotype was associated with an increased risk of ATS.
Conclusions
The obtained data suggest a positive association between MRAS and ATS among the Han Chinese. Further studies should be performed with larger sample and among different ethnic populations, and gene-gene or gene-environment interactions should be considered.
Keywords: ischemic stroke, atherothrombotic stroke, single-nucleotide polymorphism, haplotype, genetic variation
Introduction
Stroke is the second most common cause of death, and the major cause of disability worldwide.1,2 In mainland China it is estimated that about 1.5-2.0 million new cases occur each year,3 and cerebrovascular diseases (CVDs) were reportedly the leading cause of death in 2008.4 In developed countries 67.3-80.5% of strokes are reportedly ischemic in origin, while the proportion in China is 43.7-78.9%.3
Ischemic stroke (IS) is considered to be a heterogeneous, multifactorial disease that is caused by any or a combination of the traditional risk factors such as hypertension, diabetes, smoking, dyslipidemia, atrial fibrillation (AF), and obesity.5 However, these risk factors explain only approximately 60% of cases.6 Various studies involving families, twins, and animal models have suggested that genetic background contributes to a predisposition toward IS.5 IS is caused mainly by thromboembolic occlusion of the brain arteries secondary to atherosclerosis.7 Atherosclerotic stroke shares common risk factors and pathophysiological mechanisms with coronary artery disease (CAD),7-9 another well-known atherosclerotic disease, and they appear to have common susceptibility loci. For example, sequence variants on chromosome 9p21.3 were identified as susceptibility loci for CAD,10 and were also proven to be associated with IS, especially large-artery stroke (atherosclerotic stroke).11,12 A variant [single-nucleotide polymorphism (SNP) rs9818870] in the muscle RAS (M-ras) oncogene homolog gene (MRAS) on chromosome 3q22.3 was recently identified as a susceptibility locus for CAD in a genome-wide association study, with compelling statistical evidence.13 The M-ras protein (encoded by MRAS) was also found to play an important role in atherosclerosis.14 Thus, it is plausible that MRAS also plays a role in atherosclerotic stroke, as a result of a stronger genetic component in IS patients younger than 70 years of age and in the Han Chinese population, which accounts for 90% of the population in China.15 Therefore, the main focus of the present study was the possible association between MRAS and the risk of atherosclerotic stroke in a population of Han Chinese aged 19-70 years.
Methods
Study population
Study subjects were recruited from consecutive patients admitted with a first-ever IS to the Nanchong Central Hospital, which is affiliated with the North Sichuan Medical College, between August 2010 and December 2011. IS was defined according to the World Health Organization (WHO) definition16,17 and confirmed by a brain computed tomography and/or magnetic resonance imaging scan showing a recent brain infarct corresponding to the clinical presentation within 2 weeks of the event. Patients with nonsymptomatic cerebral infarction, hemorrhage after infarction, and intracranial hemorrhagic diseases were excluded from the study. IS is a heterogeneous phenotype composed of different entities, and hence the inclusion of all IS cases in the analyses may obscure genetic effects restricted to a certain IS subtype. Some studies have highlighted the need to evaluate the genetic effect on each IS subtype.18,19 The Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification is used extensively in genetic studies of IS; however, the Korean modification of the TOAST classification is more sensitive than the original TOAST classification for the diagnosis of atherosclerotic stroke.20 The present study included only subjects with an atherothrombotic cerebral infarction [atherothrombotic stroke (ATS)] diagnosed in accordance with the Korean modified TOAST classification of Han et al.20 in 2007.
All of the ATS subjects were Han Chinese patients with no history of CVDs, and with no consanguinity relationships among them. Strokes occurring in the course of systemic conditions such as immunological disorders, coagulopathies, thyroid disease, tuberculosis, or malignant tumor were excluded in order to assure the solely atherosclerotic etiology of the IS. ATS patients with liver/kidney disease, AF, thrombolytic therapy, or pregnancy were also excluded. The control subjects were randomly selected from inpatients with minor illness from the ophthalmology, gastroenterology, and otorhinolaryngology departments of the hospital, and nonfamily visitors to hospitalized patients, who were free of neurological diseases, as evidenced by clinical manifestations and physical examination, following the same exclusion criteria as the ATS subjects. The study was approved by the Ethics Committee of Nanchong Central Hospital, and all eligible subjects provided written informed consent to participate.
Baseline examination
A detailed medical history was obtained from each subject through an interview and physical examination. Demographic features, clinical features, biochemical parameters, and established risk factors for stroke were recorded. A blood sample was obtained from all subjects for genetic analysis.
A history of coronary heart disease (CHD; i.e., angina pectoris, unstable angina, myocardial infarction, or heart failure), as well as heart valve disease and arrhythmias was assessed by a questionnaire and relevant medical confirmation. Cigarette smoking was defined as having smoked at least one cigarette per day for 1 year or more. Former smokers who had stopped smoking more than 5 years previously were not included.21 The presence of alcohol consumption was defined as drinking alcohol at least 12 times during the past year.21 Hypertension was defined as present if subjects had previously been diagnosed according to the WHO/International Society of Hypertension guidelines (systolic or diastolic blood pressure ≥140 mm Hg or ≥90 mm Hg, respectively)22 and were routinely receiving antihypertensive therapy. Diabetes mellitus (DM) was characterized by recurrent or persistent hyperglycemia, and was diagnosed by the presence of 1) fasting plasma glucose ≥7.0 mM, 2) plasma glucose ≥11.1 mM at 2 hours after a 75.0-g oral glucose challenge, or 3) random plasma glucose ≥11.1 mM, or if a history of DM was reported (including patients with antidiabetic medication; WHO).23 Dyslipidemia was diagnosed using Chinese criteria published in 2007:24 1) a serum total cholesterol level of > or =5.18 mM (200 mg/dL), 2) a low high-density lipoprotein cholesterol of <1.04 mM (<40 mg/dL), 3) a low-density lipoprotein cholesterol level of ≥3.37 mM (130 mg/dL), and 4) a serum triglyceride concentration of ≥1.70 mM (150 mg/dL). The baseline body mass index (BMI) was calculated as the weight divided by the height squared, with a BMI of 24 kg/m2 taken as the cutoff point for being overweight.25,26
Selection of SNPs
Data were sourced from the National Center for Biotechnology Information Bulletin 36 (NCBI). Tagging SNPs were selected using the genotype data obtained from unrelated Han Chinese in Beijing in the HapMap database (HapMap Data Phase III/Rel#2, Feb09, on NCBI36 B36 assembly, dbSNP b126)27 with an r2 threshold of 0.8 and a minor allele frequency of 5%. The SNPs located in 5'- and/or 3'-flanking or untranslated regions (UTRs) were also selected for analysis.
Two tagging SNPs (rs40593 and rs6782181) were identified within a 32.67-kb region spanning MRAS (including 2.0 kb upstream and 0.5 kb downstream; chromosome three, positions 139, 574, 397-139, 607,065). An additional two SNPs were also included in the current study: rs9818870, which was located in the 3' UTR of MRAS in close proximity to a cluster of miRNA binding sites (an association with CAD has been noted previously),13 and rs3755751, which was located in the 5'-flanking region.
DNA isolation and genotyping
Venous blood samples were collected from all subjects in EDTA-treated evacuated tubes. Genomic DNA was extracted from blood samples according to standard procedures by using a TIANamp Genomic DNA kit (TIANamp Blood DNA Kit, DP318, TIANGEN Biotech, Beijing, China). All DNA fragments were subjected to electrophoresis on 2% agarose gels and visualized under ultraviolet light after staining with ethidium bromide.
The four MRAS SNPs were genotyped using the ABI multiplex SNaPshot method (Applied Biosystems, Foster City, CA, USA) with the technical support of Shanghai Generay Biotech (http://www.generay.com.cn/). The process used by the manufacturer is briefly described below.
The forward (F) and reverse (R) primers used for the polymerase chain reaction (PCR) and the extension reaction were as follows:
1. For rs40593: F, 5'-AAT AAA AGG CAG CAC AGC TGG-3'; R, 5'-GTA GCA GAA TCA TTC TCC AGC-3'; extension primer, 5'-TTT TTT TCC TCG GCA AGA TCA CCA GC-3'.
2. For rs6782181: F, 5'-GAA TTC ACA CGC ACA GTT CAG-3'; R, 5'-AGG CAA ATC CAT AAA GGC AGG-3'; extension primer, 5'-TTT TTT TTT TTG CAG GGT TGG GGA TGA ATA-3'.
3. For rs9818870: F, 5'-TGG GTT TCT CAG ATC TGT CTC-3'; R, 5'-GCT TAT AGA GGT GGT AGT CAG-3'; extension primer 5'-TTT TTT TTT GAC GTG TCA GTG TAT TC-3'.
4. For rs3755751: F, 5'-CCT CAA TGA CTT AGA ACC AGC-3'; R, 5'-TCT ACA GGG TCT TTG GAG CAG-3'; extension primer, 5'-TTT TTT TTT TTT TTT AGG AAG CCT GCA TGG GATT-3'.
Polymerase chain reaction was performed in a total volume of 15.0 µL containing 1.5 µL of 10× buffer, 1.8 µL of 25 mM MgCl2, 0.4 µL of each of dATP, dCTP, dTTP, and dGTP [R0192, Fermentas, Thermo Fisher Scientific (China) Co., Ltd, Beijing, China], 0.3 µL of Taq polymerase [EP0406, Fermentas, Thermo Fisher Scientific (China) Co., Ltd, Beijing, China], 1.0 µL of genomic DNA, and 0.1 µL (20 pmol) of each primer. The program used was an initial denaturation step of 95℃ for 3 minutes followed by the first 11 cycles of denaturation at 94℃ for 15 seconds, annealing at 60℃ for 15 seconds (the annealing temperature was decreased by 0.5℃ in each consecutive cycle), and elongation at 72℃ for 30 seconds, followed by the second 24 cycles of denaturation at 95℃ for 15 seconds, annealing at 54℃ for 15 seconds, and elongation at 72℃ for 30 seconds, and a final extension step at 72℃ for 3 minutes. To avoid the affect of primers and unincorporated dNTPs from the preliminary PCR reaction on the subsequent primer extension reaction, the PCR products were subsequently purified in 7.0-µL reaction volumes. Briefly, 3.0 µL of PCR products was incubated with 0.2 µL of Exo I [EN0582, Fermentas, Thermo Fisher Scientific (China) Co., Ltd, Beijing, China], 0.8 µL of FastAP thermosensitive alkaline phosphatase [FastAP, EF0652, Fermentas, Thermo Fisher Scientific (China) Co., Ltd, Beijing, China], and 0.7 µL of ExoI buffer at 37℃ for 15 minutes and then at 80℃ for 15 minutes.
The product was then processed according to the ABI SNaPshot protocol. The extension reaction was performed in a total volume of 6.0 µL, containing 2.0 µL of purified PCR product, 0.8 µL of SNaPshot multiplex mix containing Taq polymerase and fluorescently labeled dideoxy-NTPs (Applied Biosystems, Foster City, CA, USA), 2.0 µL of mixed extension primer, and 1.2 µL of H2O. The initial denaturation was performed at 96℃ for 1 minute, and then the samples were subjected to 28 cycles of denaturation at 96℃ for 10 seconds, annealing at 52℃ for 5 seconds, and elongation at 60℃ for 30 seconds. To remove the cycling unincorporated fluorescent dNTPs, 6.0 µL of the extension product was incubated with 0.5 µL of FastAP [EF 0652, Fermentas, Thermo Fisher Scientific (China) Co., Ltd, Beijing, China] at 37℃ for 15 minutes and then at 80℃ for 15 minutes. An 8.0-µL volume of deionized formamide was mixed with 1.0 µL of the purified extension product and electrophoresed on an ABI 3730XL genetic analyzer (Applied Biosystems). The parameters suggested in the SNaPshot protocol were used. The separated products were analyzed using GeneMapper Software v4.0 (Applied Biosystems, Foster City, CA, USA).
Statistical analysis
Continuous variables are expressed as mean±SD values. The normality of the sample distribution of each continuous variable was tested with the Kolmogorov-Smirnov test. Differences between continuous variables were evaluated by the independent-samples t-test or the Mann-Whitney U-test, depending on the shape of the distribution curves. Potential confounders were identified by performing univariate analyses. The chi-square test was employed to test for qualitative variables, genotypes/alleles frequencies, and Hardy-Weinberg equilibrium (HWE) of the polymorphisms.
Four genetic models (dominant, recessive, additive, and allelic comparison) were assumed while performing statistical analyses.28 Namely, for an SNP with minor allele a and major allele A, a dominant model means A/A versus both a/A and a/a combined, a recessive model means a/a versus a combined count of both a/A and A/A genotypes, a/A or a/a versus A/A for the additive model, and a versus A for allelic comparison. Multivariate logistic regression analysis with adjustment of traditional risk factors (e.g., age, sex, diabetes, hypertension, dyslipidemia, smoking, and alcohol consumption) was used to estimate the odds ratio (OR) and 95% confidence interval (CI) for the risk genotypes, and variables with p<0.10 on univariate analysis were included in a regression model. Subgroup analyses were also performed by stratifying the subjects according to sex and age (<45 years and ≥45 years).29 Haplotype construction was performed using the genetic statistical software SHEsis.30,31
All statistical analyses were performed with the SPSS 13.0 package, unless indicated otherwise. A probability value of p<0.05 (two tailed) was considered significant.
Results
General characteristics of the subjects
In total, 823 IS patients were admitted to Nanchong Central Hospital during the study period. Among them, 431 (52.4%) were classified with ATS under the criteria of the modified TOAST classification,20 39 (4.7%) with cardioembolism, 210 (25.5%) with small-artery disease (small-vessel disease), 18 (2.2%) with stroke of other determined etiology, and 125 (15.2%) with stroke of undetermined etiology. Of the 431 ATS subjects, 229 were excluded from the study because they had a history of CVD (n=107), were receiving thrombolytic therapy (n=17), suffered from liver or kidney disease (n=77), were pregnant (n=3), or had other severe systematic diseases (n=25). A control group of 188 unrelated individuals was recruited during the same period, of whom 28 were visitors to hospitalized patients, 48 were inpatients with cataract or conjunctivitis from the Department of Ophthalmology, 79 were inpatients with acute or chronic appendicitis from the Division of Gastroenterology, and 33 were patients from the Department of Otorhinolaryngology with acute or chronic rhinitis, pharyngitis, or laryngitis.
Ultimately, 202 subjects with ATS and 188 controls were recruited for the present study. However, genotyping was unsuccessful for eight of those in the ATS group and for two of the controls. Therefore, 194 ATS and 186 control subjects were included in the further analyses. The subjects were aged 60.59±8.18 years in the ATS group (the median was 62 years due to the nonnormal distribution of the data) and 56.44±11.43 years for the controls (median, 58 years). Women accounted for 35.6% of the ATS group (n=69) and 47.3% of the controls (n=88). As well as being more likely to be male and older, the ATS subjects had a higher prevalence of hypertension, diabetes, CHD, smoking, and drinking. The demographic and clinical characteristics of the ATS and control groups are presented in Table 1.
Table 1.
Characteristics of the atherothrombotic stroke (ATS) and control subjects included in this study. Unless stated otherwise, data are presented as n or mean±SD values
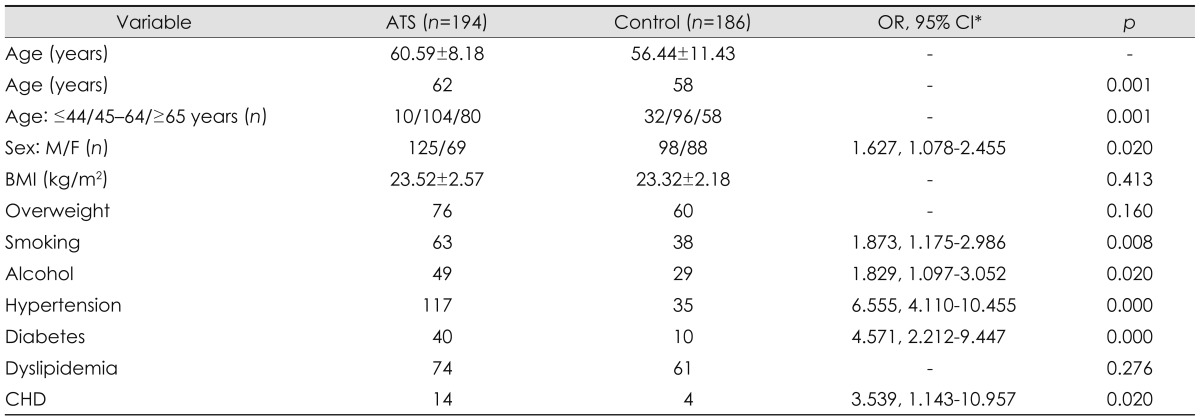
*OR, 95% CI listed only if p<0.05.
BMI: body mass index, CHD: coronary heart disease, F: female, M: male, OR: odds ratio, 95% CI: 95% confidence interval.
Individual SNP association analysis
The association between SNPs and ATS in general samples
The distribution of all SNP genotypes among the controls was consistent with the HWE model (p>0.05). There were no significant differences in four SNPs with respect to allele or genotype frequencies between the ATS and control groups in general samples for all genetic comparisons. These data are summarized in Table 2. However, the multivariate logistic regression analysis revealed a positive association between rs40593 and ATS under the dominant and additive models after adjustment for covariates [adjusted OR=1.673, 95% CI=1.031-2.715, and p=0.037 for the dominant model; and adjusted OR=0.585, 95% CI=0.356-0.962, and p=0.035 for the additive model (AG/AA), respectively] (Table 2). No association was found between the other three SNPs and ATS in all genetic models after adjustment for covariates.
Table 2.
Distribution of the alleles and genotypes for the four single-nucleotide polymorphisms (SNPs) in the ATS and control groups
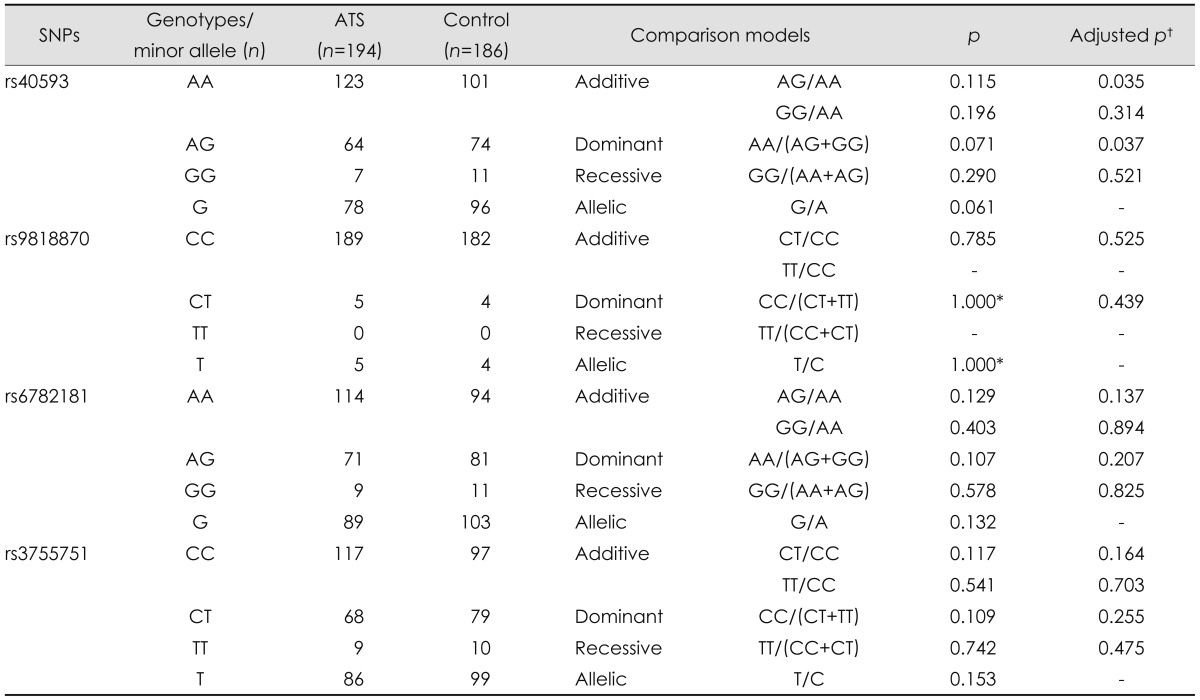
*Value with continuity correction, †Adjusted for age, gender, smoking, alcohol, hypertension, diabetes, and CHD.
ATS: atherothrombotic stroke, CHD: coronary heart disease.
Subgroup analyses
To reduce possible confounding effects of differences in age and sex distributions between the ATS and control groups, subgroup analyses were performed according to gender and age (<45 years and ≥45 years). In univariate analysis the minor allele G of SNP rs40593 was found to be significantly associated with ATS in males (OR=0.625, 95% CI=0.403-0969; p=0.035); however, no differences were detected for the other SNPs for all genetic comparisons. There was also no evidence of any significant differences between the ATS and control groups with regard to the distribution of alleles and genotypes for all SNPs in females (data not shown).
After adjustment for confounding variables such as age, dyslipidemia, CHD, alcohol, hypertension, and diabetes, the logistic regression analysis revealed no significant differences between the two groups with regard to genotypes frequencies for all SNPs and all genetic comparisons in either males or females.
When the subjects were divided into two groups according to age (<45 years or ≥45 years), only subjects in the older age group were included in analyses because there were only 10 ATS subjects and 32 control subjects in the younger age group. Three SNPs (rs6782181, rs40593, and rs3755751) were found to be significantly associated with ATS in the allelic comparison, and in additive and dominant models in individual SNP analyses. The minor G allele or G-allele carriers for rs6782181 and rs40593, as well as the minor T allele or T-allele carriers for rs3755751 played a protective role in IS risk (Table 3). After adjusting for covariants, the AG genotype for rs40593 (OR=0.557, 95% CI=0.331-0.938; p=0.028), the CT genotype for rs3755751 (OR=0.579, 95% CI=0.347-0.966; p=0.036), and the G-allele carriers (AG plus GG) for rs40593 (OR=0.535, 95% CI=0.324-0.886; p=0.015) still exhibited a significant protective effect; however, the association between T-allele genotypes and rs3755751 was only marginally significant (OR=1.637, 95% CI=0.999-2.681; p=0.05). In contrast, there was no significant association between rs6782181 and ATS (Table 3).
Table 3.
Distribution of alleles and genotypes for the four SNPs in ATS and control subjects aged ≥45 years
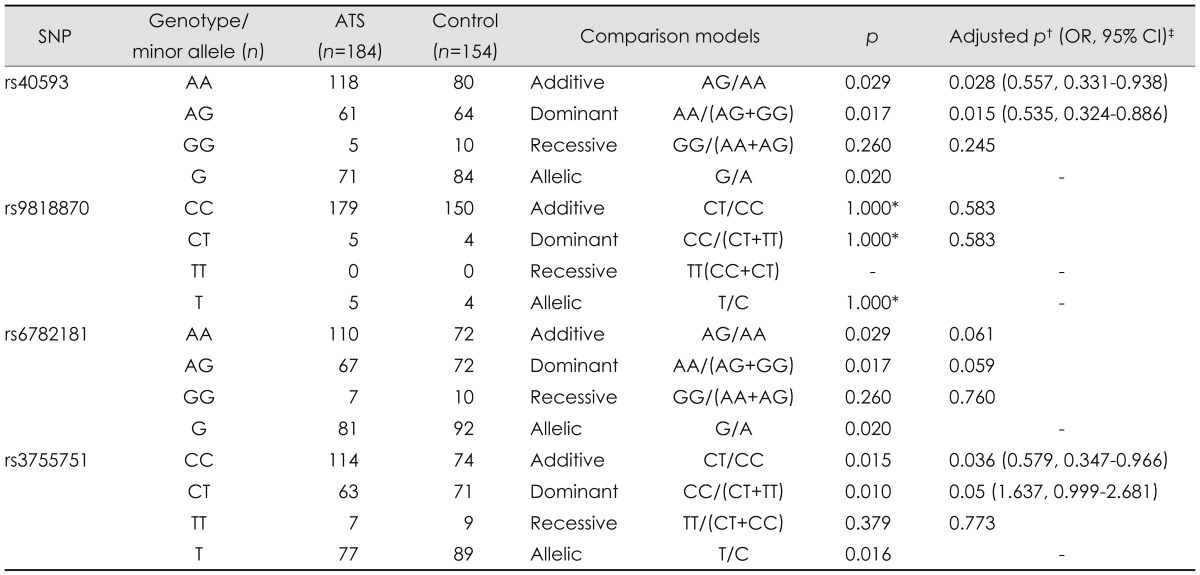
*Value with continuity correction, †Adjusted for gender, smoking, alcohol, hypertension, diabetes, and CHD, ‡OR, 95% CI listed only if p<0.05.
ATS: atherothrombotic stroke, CHD: coronary heart disease, SNP: single-nucleotide polymorphism.
Haplotype analysis
All four loci were analyzed for constructing haplotypes. Nine haplotypes were observed in the general population, female subjects, and subjects aged ≥45 years, and eight haplotypes were observed among the male subjects. No statistically significant differences were detected between ATS and control subjects with respect to haplotype distribution in either the general samples or in different gender groups.
Among those aged ≥45 years, the frequency of subjects carrying the ACAC haplotype (for markers rs40593-rs9818870-rs6782181-rs3755751), which was associated with an increased risk of ATS, was significantly higher in the ATS group (76.0%) than in the control group (68.1%; p<0.05). In contrast, the frequency of the GCGT haplotype (for markers rs40593-rs9818870-rs6782181-rs3755751) was significantly lower in the ATS group than in the controls (16.8% vs. 24.6%, p<0.05), demonstrating a significant protective effect against ATS (Table 4).
Table 4.
Estimated four-locus haplotype frequencies in ATS and control subjects aged ≥45 years
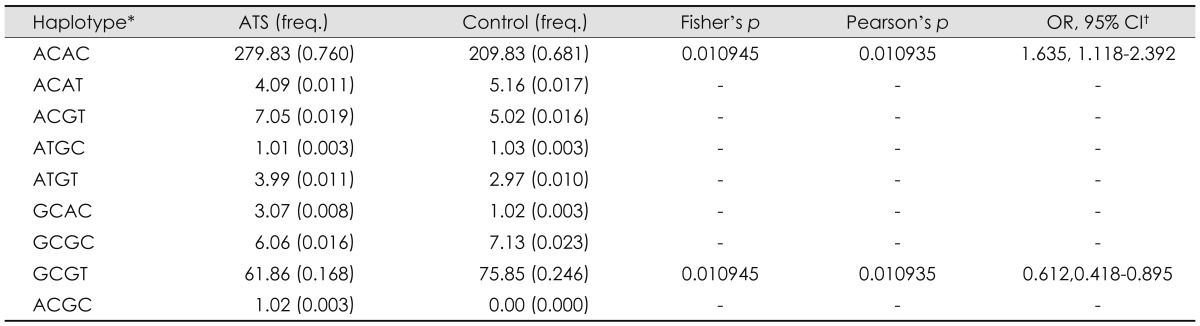
*The haplotype is listed in the order rs40593-rs9818870-rs6782181-rs3755751, †OR, 95% CI listed only if p<0.05, ‡ATS (freq.): it means the number of cases estimated to have ACAC haplotype, and this haplotype's frequency in Case; analogous meaning for other cells.
ATS: atherothrombotic stroke.
Discussion
The results of this study suggest that two SNPs (rs40593 and rs3755751) and haplotypes (ACAC and GCGT) at four loci are significantly associated with the risk of ATS. That is, the AA genotype of rs40592 significantly increases the ATS risk, with the association being particularly significant in subjects aged ≥45 years. On the other hand, among those aged ≥45 years, carriers of the CC genotype of rs3755751 were more prone to ATS than were carriers of the CT genotype, and the haplotypes constructed by the risk alleles (ACAC) exhibited a significantly elevated risk for ATS. In contrast, no evidence was found to support the hypothesis that the other MRAS SNPs play roles in ATS risk in the present population. To the best of our knowledge, no other studies have examined simultaneously the relationship between MRAS and ATS.
In humans, MRAS is located on chromosome 3q22.3, which comprises five exons and spans 33 kb (MIM608435). The M-ras protein belongs to the Ras superfamily of GTP-binding proteins. It is widely expressed in all tissues, including mouse and human aorta and heart tissues, which are potentially involved in atherosclerosis.13 Moreover, it has been demonstrated previously that activated M-ras potently induces the cell aggregation mediated by lymphocyte function-associated antigen 1.31 More importantly, there is evidence that M-ras plays a crucial role in adhesion signaling.32 It has been demonstrated that the initial stage of atherosclerosis requires interplay between various cell adhesion molecules and immune cells to trigger leukocyte and lymphocyte migration from the circulating blood into the arterial intima.33 Vascular adhesion molecules were also found to play a vital role in the atherosclerosis process, and are now recognized as critical factors in the initiation and progression of atherosclerotic disease.14 Therefore, MRAS may contribute to IS by promoting atherosclerosis.
The present study demonstrated the association between MRAS and ATS in a population of Han Chinese. However, the results should be interpreted with caution due to some limitations in both the data and methodology. First, the mean age was significantly lower in the control group than in the ATS group. Since stroke is a late-onset disease, the chances of misclassification as "stroke-free" was not excluded, which might have affected the results. The second possible limitation lies in the inclusion of a relatively small number of ATS and control subjects. In addition, performing multiple analyses may have increased the likelihood of spurious results. Nevertheless, corrections for multiple testing, which were considered appropriate for hypothesis-testing studies, were not applied. Since any genetic association study that includes only a small number of polymorphisms should generally be regarded as exploratory in character,34 such corrections were considered overly conservative for this exploratory study.34
This is the first report of an association between MRAS and ATS (the most important subtype of IS) in a population of Han Chinese. It is important to perform further genetic studies involving other ethnic populations, such as other Asian as well as Caucasian and African populations, in order to clarify the role of MRAS in IS. Moreover, since IS is a complex and multifactorial disease caused by a combination of vascular risk factors such as environmental and genetic factors, genegene and gene-environment interactions must also be considered in future studies.
Conclusion
The present study demonstrated a positive association between MRAS and ATS in a population of Han Chinese. Further functional studies are needed to define the mechanisms by which these loci translate into a higher risk of IS, and to explore whether this information can be used to improve the prevention, prediction, or treatment of this common disease. Future studies should be performed with large samples and among different ethnic populations, with gene-gene and gene-environment interactions being considered.
Acknowledgements
This article was supported by the Xinqiao Hospital of the Third Military Medical University Postdoctoral Fellowship Scheme. We thank Mr. Morgan Maclure for helpful comments on the manuscript.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 2.Donnan GA, Fisher M, Macleod M, Davis SM. Stroke. Lancet. 2008;371:1612–1623. doi: 10.1016/S0140-6736(08)60694-7. [DOI] [PubMed] [Google Scholar]
- 3.Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6:456–464. doi: 10.1016/S1474-4422(07)70004-2. [DOI] [PubMed] [Google Scholar]
- 4.Chen Z. Report for Third National Retrospective Sampling Mortality Survey. Beijing: Peking Union Medical College Press; 2008. [Google Scholar]
- 5.Dichgans M. Genetics of ischaemic stroke. Lancet Neurol. 2007;6:149–161. doi: 10.1016/S1474-4422(07)70028-5. [DOI] [PubMed] [Google Scholar]
- 6.Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 7.Humphries SE, Morgan L. Genetic risk factors for stroke and carotid atherosclerosis: insights into pathophysiology from candidate gene approaches. Lancet Neurol. 2004;3:227–235. doi: 10.1016/S1474-4422(04)00708-2. [DOI] [PubMed] [Google Scholar]
- 8.Adams RJ, Chimowitz MI, Alpert JS, Awad IA, Cerqueria MD, Fayad P, et al. Coronary risk evaluation in patients with transient ischemic attack and ischemic stroke: a scientific statement for healthcare professionals from the Stroke Council and the Council on Clinical Cardiology of the American Heart Association/American Stroke Association. Circulation. 2003;108:1278–1290. doi: 10.1161/01.CIR.0000090444.87006.CF. [DOI] [PubMed] [Google Scholar]
- 9.Pasternak RC, Criqui MH, Benjamin EJ, Fowkes FG, Isselbacher EM, McCullough PA, et al. Atherosclerotic Vascular Disease Conference: Writing Group I: epidemiology. Circulation. 2004;109:2605–2612. doi: 10.1161/01.CIR.0000128518.26834.93. [DOI] [PubMed] [Google Scholar]
- 10.Schunkert H, Götz A, Braund P, McGinnis R, Tregouet DA, Mangino M, et al. Repeated replication and a prospective meta-analysis of the association between chromosome 9p21.3 and coronary artery disease. Circulation. 2008;117:1675–1684. doi: 10.1161/CIRCULATIONAHA.107.730614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gschwendtner A, Bevan S, Cole JW, Plourde A, Matarin M, Ross-Adams H, et al. Sequence variants on chromosome 9p21.3 confer risk for atherosclerotic stroke. Ann Neurol. 2009;65:531–539. doi: 10.1002/ana.21590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson CD, Biffi A, Rost NS, Cortellini L, Furie KL, Rosand J. Chromosome 9p21 in ischemic stroke: population structure and meta-analysis. Stroke. 2010;41:1123–1131. doi: 10.1161/STROKEAHA.110.580589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erdmann J, Grosshennig A, Braund PS, König IR, Hengstenberg C, Hall AS, et al. New susceptibility locus for coronary artery disease on chromosome 3q22.3. Nat Genet. 2009;41:280–282. doi: 10.1038/ng.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galkina E, Ley K. Vascular adhesion molecules in atherosclerosis. Arterioscler Thromb Vasc Biol. 2007;27:2292–2301. doi: 10.1161/ATVBAHA.107.149179. [DOI] [PubMed] [Google Scholar]
- 15.Chen J, Zheng H, Bei JX, Sun L, Jia WH, Li T, et al. Genetic structure of the Han Chinese population revealed by genome-wide SNP variation. Am J Hum Genet. 2009;85:775–785. doi: 10.1016/j.ajhg.2009.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41:105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 17.Asplund K, Tuomilehto J, Stegmayr B, Wester PO, Tunstall-Pedoe H. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta Med Scand Suppl. 1988;728:26–39. doi: 10.1111/j.0954-6820.1988.tb05550.x. [DOI] [PubMed] [Google Scholar]
- 18.Bevan S, Dichgans M, Gschwendtner A, Kuhlenbäumer G, Ringelstein EB, Markus HS. Variation in the PDE4D gene and ischemic stroke risk: a systematic review and meta-analysis on 5200 cases and 6600 controls. Stroke. 2008;39:1966–1971. doi: 10.1161/STROKEAHA.107.509992. [DOI] [PubMed] [Google Scholar]
- 19.Rao R, Tah V, Casas JP, Hingorani A, Whittaker J, Smeeth L, et al. Ischaemic stroke subtypes and their genetic basis: a comprehensive meta-analysis of small and large vessel stroke. Eur Neurol. 2009;61:76–86. doi: 10.1159/000177939. [DOI] [PubMed] [Google Scholar]
- 20.Han SW, Kim SH, Lee JY, Chu CK, Yang JH, Shin HY, et al. A new subtype classification of ischemic stroke based on treatment and etiologic mechanism. Eur Neurol. 2007;57:96–102. doi: 10.1159/000098059. [DOI] [PubMed] [Google Scholar]
- 21.Kelly TN, Gu D, Chen J, Huang JF, Chen JC, Duan X, et al. Cigarette smoking and risk of stroke in the chinese adult population. Stroke. 2008;39:1688–1693. doi: 10.1161/STROKEAHA.107.505305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 23.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 24.Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. 2007;35:390–419. [PubMed] [Google Scholar]
- 25.Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases--report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. 2002;15:245–252. [PubMed] [Google Scholar]
- 26.Chen C, Lu FC Department of Disease Control Ministry of Health, PR China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36. [PubMed] [Google Scholar]
- 27.International HapMap Consortium. A haplotype map of the human genome. Nature. 2005;437:1299–1320. doi: 10.1038/nature04226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clarke GM, Anderson CA, Pettersson FH, Cardon LR, Morris AP, Zondervan KT. Basic statistical analysis in genetic case-control studies. Nat Protoc. 2011;6:121–133. doi: 10.1038/nprot.2010.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pezzini A. Genetic determinants of juvenile stroke. Thromb Res. 2012;129:330–335. doi: 10.1016/j.thromres.2011.10.035. [DOI] [PubMed] [Google Scholar]
- 30.Shi YY, He L. SHEsis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell Res. 2005;15:97–98. doi: 10.1038/sj.cr.7290272. [DOI] [PubMed] [Google Scholar]
- 31.Li Z, Zhang Z, He Z, Tang W, Li T, Zeng Z, et al. A partition-ligation-combination-subdivision EM algorithm for haplotype inference with multiallelic markers: update of the SHEsis (http://analysis.bio-x.cn) Cell Res. 2009;19:519–523. doi: 10.1038/cr.2009.33. [DOI] [PubMed] [Google Scholar]
- 32.Yoshikawa Y, Satoh T, Tamura T, Wei P, Bilasy SE, Edamatsu H, et al. The M-Ras-RA-GEF-2-Rap1 pathway mediates tumor necrosis factor-alpha dependent regulation of integrin activation in splenocytes. Mol Biol Cell. 2007;18:2949–2959. doi: 10.1091/mbc.E07-03-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chi Z, Melendez AJ. Role of cell adhesion molecules and immune-cell migration in the initiation, onset and development of atherosclerosis. Cell Adh Migr. 2007;1:171–175. doi: 10.4161/cam.1.4.5321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tobin MD, Braund PS, Burton PR, Thompson JR, Steeds R, Channer K, et al. Genotypes and haplotypes predisposing to myocardial infarction: a multilocus case-control study. Eur Heart J. 2004;25:459–467. doi: 10.1016/j.ehj.2003.11.014. [DOI] [PubMed] [Google Scholar]


